Abstract
Background
Despite therapies proven effective for heart failure with systolic dysfunction, the condition continues to cause substantial hospitalization, disability, and death, especially among African-American and other nonwhite populations.
Objective
To compare the effects of a nurse-led intervention focused on specific management problems versus usual care among ethnically diverse patients with systolic dysfunction in ambulatory care practices.
Design
Randomized effectiveness trial conducted from September 2000 to September 2002.
Setting
The 4 hospitals in Harlem, New York.
Patients
406 adults (45.8% were non-Hispanic black adults, 32.5% were Hispanic adults, 46.3% were women, and 36.7% were ≥65 years of age) who met eligibility criteria: systolic dysfunction, English- or Spanish-language speakers, community-dwelling patients, and ambulatory care practice patients.
Intervention
During a 12-month intervention, bilingual nurses counseled patients on diet, medication adherence, and self-management of symptoms through an initial visit and regularly scheduled follow-up telephone calls and facilitated evidence-based changes to medications in discussions with patients’ clinicians.
Measurements
Hospitalizations (in 406 of 406 patients during follow-up) and self-reported functioning (in 286 of 406 patients during follow-up) at 12 months.
Results
At 12 months, nurse management patients had had fewer hospitalizations (143 hospitalizations vs. 180 hospitalizations; adjusted difference, −0.13 hospitalization/person-year [95% CI, −0.25 to −0.001 hospitalization/person-year]) than usual care patients. They also had better functioning: The Short Form-12 physical component score was 39.9 versus 36.3, respectively (difference, 3.6 [CI, 1.2 to 6.1]), and the Minnesota Living with Heart Failure Questionnaire score was 38.6 versus 47.3, respectively (difference, −8.8 [CI, −15.3 to −2.2]). Through 12 months, 22 deaths occurred in each group and percentages of patients who were hospitalized at least once were similar in each group (30.5% of nurse management patients vs. 36.5% of control patients; adjusted difference, −7.1 percentage points [CI, −16.9 to 2.6 percentage points]).
Limitations
Three nurses at 4 hospitals delivered interventions in this modest-sized trial, and 75% of the participants were from 1 site. It is not clear which aspects of the complex intervention accounted for the results.
Conclusions
Nurse management can improve functioning and modestly lower hospitalizations in ethnically diverse ambulatory care patients who have heart failure with systolic dysfunction. Sustaining improved functioning may require continuing nurse contact.
Heart failure disproportionately affects black and elderly people and is a leading cause of hospitalization among people 65 years of age or older (1, 2). Although effective therapies can improve functioning and survival in patients with systolic dysfunction, many patients may not be receiving the full benefit of existing knowledge (3–5).
Patients play a critical role in managing a chronic condition, such as heart failure. Patients may not realize that specific symptoms are related to heart failure or that adhering to medications and diet can reduce symptoms and life-threatening episodes (6). Evidence-based guidelines for systolic dysfunction recommend that physicians not only offer patients effective therapies but also teach them the importance of adherence and self-monitoring (3, 4). Clinicians have fallen short in prescribing angiotensin-converting enzyme inhibitors and β-blockers for patients with systolic dysfunction (5, 7, 8). When prescribed, the doses have often been lower than those proven to convey greater benefits (3, 9). Clinicians have also documented counseling only a fraction of patients with heart failure about self-management (10, 11). System-related factors may also influence patients’ ability to obtain quality care (12, 13).
Systematic reviews of clinical behavior change have suggested that interventions targeted to specific problems are more likely to be successful (14, 15). On the basis of shortfalls identified in patient self-management and clinical care in Harlem, New York, a predominately nonwhite area, we tailored a nurse management intervention to address documented problems and evaluated its effectiveness in a randomized, controlled trial. Our trial among primarily minority patients addresses important gaps in the literature. We targeted problems documented among patients with heart failure in Harlem, enrolled patients from ambulatory care practices, randomly assigned patients to either nurse management or usual care, and evaluated the patients’ subsequent health-related outcomes. We hypothesized that patients in the focused nurse management program would have fewer hospitalizations and report better functioning than patients in usual care.
Methods
Development of the Intervention
During interviews with patients with heart failure at Mount Sinai Hospital, New York, New York, patients reported inadequate understanding of heart failure and their role in managing it (6). Less than half of patients followed a very-low-salt diet, and only about one quarter weighed themselves daily. Regarding clinical management, medical records noted prescriptions for an angiotensin-converting enzyme inhibitor or hydralazine–dinitrate combination in 82% of 322 consecutive black patients with documented systolic dysfunction who were scheduled for visits at the general medicine clinic at Harlem Hospital from February 1995 through February 1997. The prescribed doses, however, equaled or exceeded those found to be efficacious in clinical trials in only 26% of these patients (3).
In designing a nurse management intervention to address these problems, we built on a Stanford University program that evaluated primarily privately insured patients at Kaiser Permanente in northern California (16, 17). We adapted their questionnaire on the frequency of foods eaten to incorporate those that are common among African-American and Hispanic people in Harlem.
Settings and Recruitment
All 4 hospitals in Harlem, the area’s major providers, collaborated in the trial: 1 large private academic medical center (1171 beds), 2 medium-sized municipal hospitals (286 beds and 363 beds), and 1 smaller private community hospital (200 beds). In 2000, these hospitals had 521, 267, 218, and 168 discharges for the heart failure diagnosis-related group (code 127), respectively. All are not-for-profit institutions.
The trial had the following inclusion criteria: adults 18 years of age or older; systolic dysfunction documented on a cardiac test (echocardiography, radionuclide ventriculography, myocardial stress sestamibi or thallium stress testing, or left-heart catheterization); English-language or Spanish-language speakers; community-dwelling at enrollment; and current patient in a general medicine, geriatrics, or cardiology clinic or office at a participating site. Exclusion criteria were medical conditions that prevented interaction with the nurse, including blindness, deafness, or cognitive impairment; medical conditions requiring individualized management that might differ from standard protocol, namely pregnancy, renal dialysis, or terminal illness; or procedures that corrected systolic dysfunction, such as heart transplantation. Of the 216 clinicians (209 physicians and 7 physicians’ assistants or nurse practitioners) in participating practices, 1 clinician declined permission to recruit his patients. The institutional review boards for each site approved the study.
We identified patients with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), and diagnosis-related group codes on outpatient or inpatient billings for heart failure, March 1999 through February 2001, who had at least 1 clinician visit to a participating practice and impaired systolic dysfunction. We defined impaired systolic dysfunction as a left ventricular ejection fraction less than 0.40 or moderately or severely reduced systolic dysfunction on echocardiography, radionuclide ventriculography, myocardial stress sestamibi or thallium stress testing, or left-heart catheterization. We obtained clinicians’ permission to recruit specific patients and sent each approved patient a letter from the site’s physician coordinator.
Bilingual recruiters telephoned eligible patients or approached them at scheduled clinician appointments. The recruiter confirmed each patient’s eligibility, obtained written informed consent to participate in the study, conducted the baseline survey, and telephoned the project manager for the treatment group assignment. The recruiter conveyed the assignment to the patient and, for each nurse management patient, scheduled the in-person appointment with a nurse. We provided telephone service for 3 patients who did not have it so we could telephone patients in both treatment groups every 3 months for data on end points and so nurse management patients could participate in the intervention.
Randomization and Treatment Groups
The project’s statistician used a computer-generated, random-number sequence without blocking or stratification to centrally determine randomization assignments and concealed treatment group assignments in sealed, opaque envelopes.
Usual care patients received federal consumer guidelines for managing systolic dysfunction but no other intervention (18). In the nurse management intervention, 1 of 3 trained registered nurses met once with each patient (Table 1). In counseling the patient, the nurse stressed the relationship among sodium intake; fluid buildup; and symptoms, such as shortness of breath. Nurses mailed patients the reports from the food-frequency questionnaire after each administration. The nurse also served as a bridge between the patient and the clinician (Table 1). A local clinical advisory committee implemented national evidence-based guidelines, and a committee of key clinicians from participating sites approved the protocol (3, 4). Nurses contacted patients’ clinicians to discuss specific medications and arranged any prescription changes and examinations ordered (Table 1). An internist monitored the nurses’ work, initially in weekly and then in biweekly meetings, and a cardiologist provided oversight and substituted for the internist at regular meetings, as necessary.
Table 1.
Components of Nurse Management*
| Initial, one-time, in-person appointment |
| 1. Educated patient about heart failure |
| Described physiology of heart failure |
| Provided educational booklet in English or Spanish |
| 2. Assessed and counseled patient about aspects of self-management |
| Monitoring symptoms and contacting clinician if symptoms worsen |
| Patient to weigh self daily and record weights |
| Nurse provided scale |
| Undertaking physical activity |
| Smoking cessation |
| Maintaining low-sodium diet |
| Administered food-frequency questionnaire to assess daily sodium intake, results given to patient |
| Identified foods that contributed to sodium in patient’s diet and proposed specific alternatives |
| Stressed importance of low-sodium diet and link to edema and shortness of breath |
| Eliminating or limiting alcohol intake |
| Adhering to medications |
| Assessed prescribed medications and any other remedies being used |
| Assessed adherence to prescribed medications |
| Counseled on medication adherence |
| 3. Referred patient to social services, if needed |
| Prescription drug or other insurance coverage |
| Home health services |
| Management of depression |
| 4. Reviewed nurse’s future role |
| Nurse to telephone patient regularly |
| Toll-free number to contact nurse during regular working hours |
| Patient to continue to contact usual clinician for care |
| Nurse to coordinate with patient’s clinician |
| Follow-up telephone calls |
| 1. Assessed how patient was feeling and extent of heart failure symptoms |
| 2. Recorded any hospitalizations or emergency department visits since last call |
| If any, telephone schedule reset to beginning |
| 3. Administered food frequency questionnaire at 2, 4, 8, 12, and 24 wk |
| Mailed to patient |
| 4. Reinforced importance of daily weighing, recording weights, monitoring symptoms, low-sodium diet, medication adherence, and smoking and alcohol cessation |
| Coordination with patient’s clinician |
| 1. Sent written note to clinician after each contact with patient |
| 2. Recommended changes in medications or doses indicated by the protocol |
| ACE inhibitor or substitute |
| ACE inhibitor titrated to doses proven effective, unless contraindicated† |
| Hydralazine–dinitrate combination substituted if renal failure or hyperkalemia |
| ARB substituted if intractable cough |
| β-Blockers for all NYHA class II and class III patients titrated to doses that are proven effective, unless contraindicated‡ |
| Patient self-management of diuretics |
| 3. Recommended any subsequent examinations indicated by the protocol |
| ACE inhibitor or ARB: Check creatinine, potassium, and blood pressure levels in 1–2 wk |
| β-Blocker: Check blood pressure and heart rate in 1–2 wk |
ACE = angiotensin-converting enzyme; ARB = angiotensin-receptor blocker; NYHA = New York Heart Association.
Contraindications to ACE inhibitor included moderate or severe aortic stenosis, symptomatic hypotension, bilateral renal artery stenosis, or hypersensitivity or angioedema.
Contraindications to β-blockers included bronchospasm requiring bronchodilators, bradyarrhythmia, symptomatic hypotension, or hypersensitivity.
One nurse who was bilingual in English and Spanish delivered the intervention primarily at the 2 municipal hospitals, a second bilingual nurse delivered the intervention primarily at the small community hospital, and the second and a third English-language–speaking nurse delivered the intervention primarily at the academic center. All 3 nurses covered each other, especially for the follow-up telephone calls.
Outcomes and Measurement
To measure hospitalizations, we used billing data from the 4 participating hospitals. At quarterly telephone surveys, interviewers who were blinded to treatment assignment asked patients about hospitalizations at nonparticipating hospitals; however, we present the analysis of billing data because they measure hospitalizations independent of possibly socially acceptable responses or survey nonresponse of the patients.
For functional status, we used the generic Short Form-12 (SF-12) physical component score and the condition-specific Minnesota Living with Heart Failure (MLHF) Questionnaire, with both scales administered at the quarterly interviews.
We measured deaths recorded in the National Death Index plus deaths reported by patients’ families for patients with no subsequent billings. Since both nurse management and usual care involved only services delivered in routine practice, the study did not monitor adverse effects. As required by the academic center’s institutional review board, we informed the institutional review board about hospitalizations and deaths of that hospital’s patients reported to the nurses or quarterly interviewers. No death or hospitalization was deemed to be caused by the intervention.
Statistical Analysis
We calculated that a sample size of 400 patients would have 80% power to detect a 23% difference in the probability of hospitalization between treatment groups over 12 months. This calculation assumed a baseline hospitalization rate of 69% and an α level of 0.05 (2-sided). We surveyed the first 254 recruited patients—127 patients assigned to nurse management and 127 patients assigned to usual care—twice at 3-month intervals after the intervention ended to assess whether the intervention had a sustained effect on functioning.
Hospitalizations
We calculated the number of cumulative hospitalizations per person-year in the treatment and control groups through 12 and 18 months. A person-year equaled the number of days that each person survived during the period divided by 365 days. We estimated the adjusted hospitalization rates by using Poisson regression. Exogenous variables included treatment assignment; indicators for recruitment site; baseline values for patient age, race (white, black, or other), ethnicity (Hispanic or non-Hispanic), gender, education (<high school, high school graduate, or >high school), New York Heart Association (NYHA) class, and preference for Spanish-language interview; and baseline indicators for diabetes, chronic pulmonary disease, and ischemic heart disease. We used person-years of survival as an exposure variable so that the number or timing of deaths would not affect the estimate of differences in hospitalization rates by treatment group. The study was not powered to detect differences in deaths.
Functioning
For each functioning scale, we report the difference between treatment groups in mean change from baseline to 12 months. Observations were missing either because the patient did not complete all items of the questionnaire (item nonresponse) or because the patient could not be reached to complete the survey (survey nonresponse).
To address item nonresponse, we used a prediction-matching algorithm to impute the missing SF-12 items (114 of 2032 observations) and MLHF items (343 of 2032 observations) (19, 20). We used the ice command in STATA, version 9.1 (Stata Corp., College Station, Texas), to implement this algorithm. We estimated predicted values for each missing item from observed items and the baseline patient characteristics listed earlier. We replaced missing items with nonmissing items from patients with similar predicted values, and we recomputed the composite SF-12 and MLHF scores from the observed and imputed items.
To address survey nonresponse, we conducted tests for missing data bias suggested by Hogan and colleagues (21), and these tests gave little evidence of informative missingness. We also used linear mixed models, which are robust to data missing at random, to estimate treatment effectiveness (22). The dependent variables for these models were changes from baseline in SF-12 and MLHF scores in each time period through 12 months. Fixed effects included treatment assignment, a quadratic time trend, an interaction between the time terms and treatment assignment, and the covariates listed earlier. The mixed models included patient-level random components for the intercept, time, and treatment-by-time interaction. We report the difference in expected values from these models at 12 months for the nurse management and usual care groups as the adjusted effects of the intervention on changes in functioning from baseline to 12 months. To assess whether the effects of the intervention persisted for the 254 participants who were followed for 2 additional periods, we estimated similar equations, but the dependent variables were changes in SF-12 and MLHF scores from their 12-month values, not from baseline values. Abstractors who did not know patients’ treatment assignments obtained data on baseline medical conditions and documented components of heart failure management from medical records.
Role of the Funding Source
The Agency for Healthcare Research and Quality funded this study. The funding source had no role in the design, data collection, analysis, or interpretation of the study or in the decision to submit the manuscript for publication. All authors had access to the data files.
Results
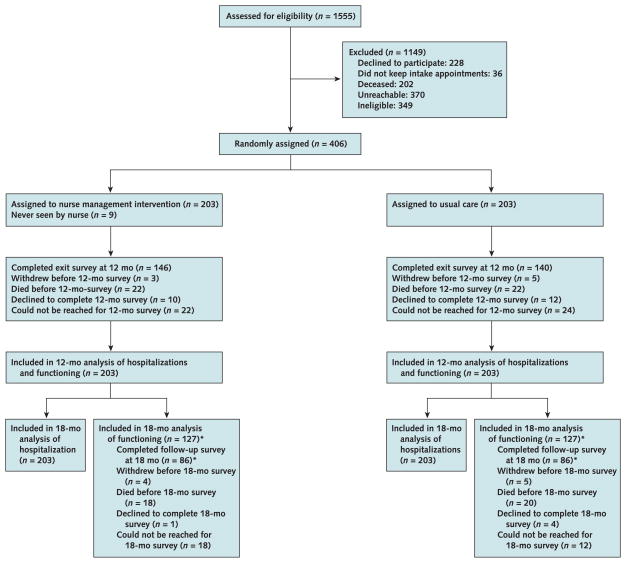
The 406 patients recruited and randomly assigned to nurse management (n = 203) or usual care (control group) (n = 203) constituted 64% of those who were reached, alive, and eligible (Figure 1). Table 2 contains patients’ baseline characteristics. The 127 nurse management and 127 usual care patients who were followed for 6 months after the intervention were similar at baseline. According to billing data before enrollment, 4 usual care patients and 1 nurse management patient had received an implantable cardioverter defibrillator and no patient in either group had received cardiac resynchronization therapy.
Figure 1. Study flow diagram.
* Of the 203 patients assigned to each trial group at baseline, as part of the original randomization process, the first 127 patients in each group were randomly assigned to receive a follow-up survey at 15 months and at 18 months.
Table 2.
Baseline Characteristics*
| Characteristic | All Patients (n = 406) | Usual Care Group (n = 203) | Nurse Management Group (n = 203) |
|---|---|---|---|
| Mean (SD) age, y | 59.4 (13.7) | 59.3 (13.7) | 59.6 (13.8) |
|
| |||
| Ethnicity, % | |||
|
| |||
| Non-Hispanic black | 45.8 | 44.3 | 47.3 |
|
| |||
| Hispanic | 32.5 | 35.5 | 29.6 |
|
| |||
| Non-Hispanic white | 15.3 | 15.3 | 15.3 |
|
| |||
| Other race or ethnicity | 6.4 | 4.9 | 7.9 |
|
| |||
| Women, % | 46.3 | 47.8 | 44.8 |
|
| |||
| Spanish-language speaker, % | 22.7 | 25.1 | 20.2 |
|
| |||
| HIgh school education, % | 46.1 | 49.8 | 42.4 |
|
| |||
| Inadequate health literacy, %† | 29.8 | 28.1 | 31.5 |
|
| |||
| Insured, % | 95.6 | 95.1 | 96.1 |
|
| |||
| Married (living with spouse), % | 27.7 | 29.2 | 26.1 |
|
| |||
| Widowed, % | 16.8 | 13.9 | 19.7 |
|
| |||
| Living alone, % | 31.5 | 34.0 | 29.1 |
|
| |||
| NYHA class, % | |||
|
| |||
| I | 18.5 | 19.2 | 17.7 |
|
| |||
| II | 22.4 | 20.2 | 24.6 |
|
| |||
| III | 14.0 | 11.8 | 16.3 |
|
| |||
| IV | 45.1 | 48.8 | 41.4 |
| Symptoms, % | |||
|
| |||
| Edema | 50.7 | 50.7 | 50.7 |
|
| |||
| Orthopnea | 51.7 | 54.7 | 48.8 |
|
| |||
| Paroxysmal nocturnal dyspnea | 28.8 | 31.5 | 26.1 |
|
| |||
| Comorbid conditions, % | |||
|
| |||
| Alcoholism | 9.4 | 10.8 | 7.9 |
|
| |||
| Angina | 13.1 | 13.3 | 12.8 |
|
| |||
| Cerebrovascular disease | 12.8 | 12.8 | 12.8 |
|
| |||
| Chronic pulmonary disease | 31.0 | 28.6 | 33.5 |
|
| |||
| Diabetes | 38.2 | 39.9 | 36.5 |
|
| |||
| Drug abuse | 5.9 | 5.9 | 5.9 |
|
| |||
| Hypertension | 70.7 | 71.4 | 70.0 |
|
| |||
| Ischemic heart disease | 44.8 | 47.8 | 41.9 |
|
| |||
| Psychiatric disorder | 9.9 | 12.8 | 6.9 |
|
| |||
| Depression | 14.0 | 15.3 | 12.8 |
|
| |||
| Dementia | 1.7 | 1.5 | 2.0 |
|
| |||
| Moderate or severe renal disease | 13.5 | 13.3 | 13.8 |
|
| |||
| Mean (SD) creatinine level | |||
| μmol/L | 133 (141) | 141 (133) | 133 (159) |
| mg/dL | 1.5 (1.6) | 1.6 (1.5) | 1.5 (1.8) |
|
| |||
| Mean (SD) Charlson index score‡ | 3.1 (1.9) | 3.2 (1.9) | 3.0 (1.9) |
|
| |||
| Mean (SD) SF-12 physical component score | 39.2 (9.1) | 38.8 (9.0) | 39.5 (9.2) |
|
| |||
| Mean (SD) MLHF Questionnaire score | 41.2 (25.6) | 41.2 (25.2) | 41.2 (26.0) |
|
| |||
| Mean hospitalizations per person in 3 mo before enrollment, n | 0.2 | 0.2 | 0.2 |
|
| |||
| Medications prescribed at baseline, % | |||
|
| |||
| Vasodilators§ | 80.5 | 80.3 | 80.8 |
|
| |||
| β-Blockers | 52.0 | 55.2 | 48.8 |
|
| |||
| Diuretics | 69.5 | 70.4 | 68.5 |
We compared outcomes on an intention-to-treat basis. Nurse management patients had fewer cumulative hospitalizations and fewer hospitalizations/person-year by the end of the 12-month trial (Table 3). From 12 to 18 months, the nurse management group continued to have a lower hospitalization rate (adjusted difference, −0.10 hospitalization/person-year [CI, −0.19 to −0.02 hospitalization/person-year]). Over 18 months, the nurse management group had 55 fewer cumulative hospitalizations (adjusted difference, −0.23 hospitalization/person-year [CI, −0.39 to −0.07 hospitalization/person-year]) (data not shown). Including patient-reported hospitalizations at nonparticipating hospitals, the adjusted rate difference over 18 months was −0.21 hospitalization/person-year (CI, −0.38 to −0.05 hospitalization/person-year) (data not shown). The probability of being hospitalized at least once over 12 months did not differ by treatment group (Table 3).
Table 3.
All-Cause Hospitalizations and Functioning of Nurse Management and Usual Care Patients*
| Variable | Usual Care Group | Nurse Management Group | Difference (95% CI) | Adjusted Difference (95% CI) |
|---|---|---|---|---|
| All-cause hospitalizations | ||||
| Cumulative over 12 mo | ||||
|
| ||||
| Total hospitalizations, n | 180 | 143 | −37 | |
|
| ||||
| Hospitalizations/person-year† | 0.93 | 0.74 | −0.19 (−0.38 to −0.01) | −0.13 (−0.25 to −0.001) |
|
| ||||
| Persons hospitalized, n | 74 | 62 | −12 | |
|
| ||||
| Persons hospitalized, %‡ | 36.5 | 30.5 | −5.9 (−15.1 to 3.3) | −7.1 (−16.9 to 2.6) |
| Cumulative from 12 mo to 18 mo | ||||
|
| ||||
| Total hospitalizations | 74 | 56 | −18 | |
|
| ||||
| Hospitalizations/person-year† | 0.83 | 0.63 | −0.20 (−0.46 to 0.05) | −0.10 (−0.19 to −0.02) |
|
| ||||
| Persons hospitalized, n | 42 | 39 | −3 | |
|
| ||||
| Persons hospitalized, %‡ | 23.1 | 21.5 | −1.5 (−10.1 to 7.0) | −4.0 (−12.5 to 4.4) |
| Functioning | ||||
| Change from baseline to 12 mo | ||||
|
| ||||
| Mean change in SF-12 physical component score§ | −2.7 (140) | 0.5 (146) | 3.2 (1.0 to 5.3) | 3.1 (0.7 to 5.5) |
|
| ||||
| Mean change in MLHF score§ | 5.4 (140) | −1.9 (146) | −7.3 (−12.1 to −2.6) | −7.0 (−12.4 to −1.7) |
| Change from 12 mo to 18 mo | ||||
|
| ||||
| Mean change in SF-12 physical component score§ | −0.5 (80) | −2.1 (81) | −1.6 (−4.7 to 1.4) | −1.7 (−4.2 to 0.9) |
|
| ||||
| Mean change in MLHF score§ | −4.6 (80) | 0.0 (80) | 4.6 (−1.3 to 10.6) | 4.7 (−0.1 to 9.5) |
MLHF = Minnesota Living with Heart Failure; SF-12 = Short Form-12.
Adjusted estimates are differences in events per person-year between treatment and control groups estimated by Poisson regression with explanatory variables listed below and survival time as the exposure variable.
Adjusted estimates are differences in probability of the event between treatment and control groups estimated by logistic regression. Explanatory variables included baseline values for race; Hispanic ethnicity; gender; language; education; New York Heart Association class; and indicators for diabetes, chronic pulmonary disease, ischemic heart disease, and recruitment site.
Values in parentheses are the numbers of patients who responded. Adjusted estimates are expected values from mixed models. Independent variables include the explanatory variables listed above, as well as linear time and its square, treatment, and treatment–time interactions.
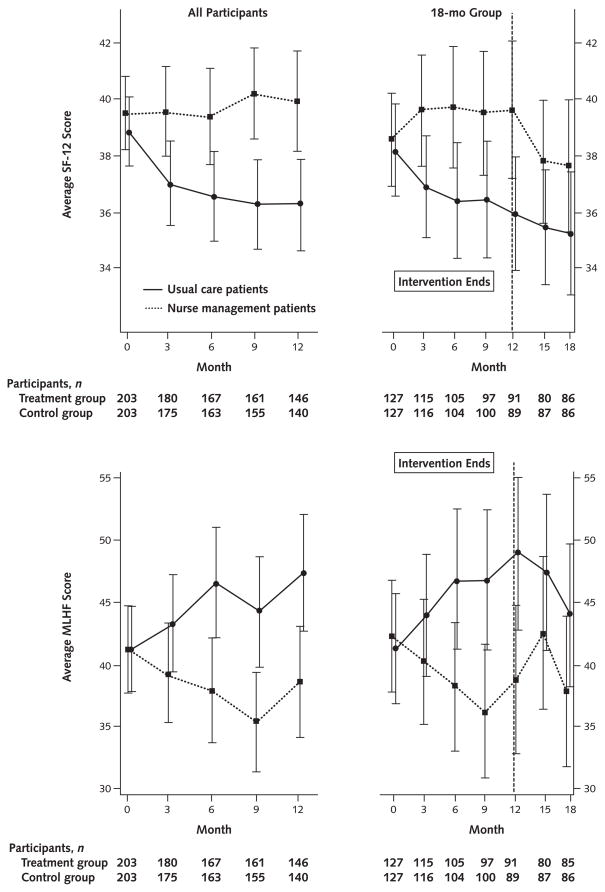
From the first follow-up interview at 3 months through the 12-month intervention, nurse management patients reported better functioning than usual care patients on both scales, with statistically significant differences (Figure 2). At 12 months, the proportion of missing SF-12 scores due to survey nonresponse did not differ between the 2 groups (20.2% usual care patients and 17.2% nurse management patients; P = 0.45). We found superior functioning in the nurse management group in both adjusted and unadjusted analyses. Compared with usual care patients, nurse management patients reported better functioning on both the SF-12 physical component scale (39.9 vs. 36.3; difference, 3.6 [CI, 1.2 to 6.1]) and the MLHF Questionnaire (38.6 vs. 47.3; difference, −8.8 [CI, −15.3 to −2.2]) (data not shown).
Figure 2.
Short Form-12 (SF-12) physical component score (top) and the Minnesota Living with Heart Failure (MLHF) Questionnaire functioning score (bottom) for all patients over the 12-month intervention period and for the subset of patients who were followed for 18 months, by usual care versus nurse management.
To place these differences in a clinically meaningful context, we compared SF-12 scores at baseline and 12 months with baseline NYHA class (25). The difference in functioning between the nurse management and usual care groups at 12 months was similar to the difference between NYHA class II and class III patients at baseline. At baseline, the SF-12 scores averaged 47.6 for NYHA class I patients, 41.3 for class II patients, 36.3 for class III patients, and 35.6 for class IV patients. From baseline to 12 months, the average unadjusted score for nurse management patients increased from 39.5 to 39.9, which was close to an NYHA class II patient’s baseline score. At the same time, the average score for usual care patients decreased from 38.8 to 36.3, which was similar to an NYHA class III patient’s baseline score. Thus, at the end of the intervention, these differences were consistent with the average nurse management patient’s score remaining similar to that of NYHA class II, denoting a slight limitation in physical activity, while the average usual care patient’s score decreased to that of NYHA class III, denoting a marked limitation in physical activity (3).
After the intervention, nurse management patients’ functioning worsened. From 12 months, nurse management patients’ SF-12 physical component scores decreased at rates that were similar to those of the usual care group (Table 3 and Figure 2).
In secondary analyses, we found fewer total hospitalizations billed for the heart failure diagnosis-related group in the nurse management group through 12 months but no differences in percentage of persons hospitalized for heart failure or in emergency department visits (Table 4). Clinicians documented counseling for salt reduction in their medical records more frequently for nurse management patients (adjusted difference, 10.1 percentage points [CI, 0.2 to 20.0 percentage points]), but rates of documenting other elements of the intervention were similar between the 2 groups (Table 4). Changes in the percentage of patients who were prescribed key medications did not differ between the 2 groups (Table 4). According to billing data for the 12 months, 1 patient in the usual care group and 0 patients in the nurse management group received an implantable cardioverter defibrillator and no patient in either group received cardiac resynchronization therapy. Each group had 22 deaths through 12 months, and nurse management patients had 3 fewer deaths at 18 months: 23 deaths versus 26 deaths (risk ratio, 0.88 [CI, 0.48 to 1.61]).
Table 4.
Secondary Outcomes from Baseline to 12 Months*
| Variable | Usual Care Group | Nurse Management Group | Difference (95% CI) | Adjusted Difference (95% CI) |
|---|---|---|---|---|
| Hospitalizations for HF, cumulative | ||||
|
| ||||
| Persons hospitalized for HF, n | 29 | 18 | −11 | |
|
| ||||
| Persons hospitalized, %† | 14.3 | 8.9 | −5.4 (−11.6 to 0.8) | −5.2 (−11.1 to 0.7) |
|
| ||||
| Total hospitalizations for HF, n‡ | 54 | 28 | ||
|
| ||||
| Hospitalizations/person-year | 0.28 | 0.14 | −0.14 (−0.23 to −0.04) | −0.10 (−0.17 to −0.03) |
| ED visits, cumulative | ||||
|
| ||||
| Persons with any ED visit, n† | 75 | 66 | −9 | |
|
| ||||
| Persons with an ED visit, % | 36.9 | 32.5 | −4.4 (−13.7 to 4.8) | −5.7 (−15.0 to 3.7) |
|
| ||||
| Total ED visits, n‡ | 157 | 147 | −10 | |
|
| ||||
| ED visits/person-year | 0.81 | 0.76 | −0.05 (−0.23 to 0.12) | −0.06 (−0.19 to 0.07) |
| Nurse management components documented, cumulative, % (n)† | ||||
|
| ||||
| Counseled to reduce salt intake | 38.4 (78) | 47.8 (97) | 9.4 (−0.2 to 19.0) | 10.1 (0.2 to 20.0) |
|
| ||||
| Counseled to monitor weight daily | 55.7 (113) | 55.7 (113) | 0.0 (−9.7 to 9.7) | 0.3 (−10.2 to 11.0) |
|
| ||||
| Counseled to exercise | 27.6 (56) | 26.1 (53) | −1.5 (−10.1 to 7.1) | −1.0 (−11.3 to 9.2) |
|
| ||||
| Counseled against smoking | 12.8 (26) | 9.9 (20) | −3.0 (−9.1 to 3.2) | −2.7 (−7.7 to 2.3) |
|
| ||||
| Counseled to reduce alcohol consumption | 4.9 (10) | 4.4 (9) | −0.5 (−4.6 to 3.6) | −0.6 (−4.0 to 2.9) |
|
| ||||
| Referred to nutritionist | 5.4 (11) | 3.4 (7) | −2.0 (−6.0 to 2.0) | −2.4 (−6.7 to 1.8) |
| Medications prescribed (at 12 mo), %† | ||||
|
| ||||
| Vasodilators§ | 82.3 | 86.2 | 3.9 (−3.1 to 11.0) | 3.2 (−3.7 to 10.1) |
|
| ||||
| β-Blockers | 61.6 | 58.1 | −3.4 (−13.0 to 6.1) | −3.9 (−13.5 to 5.8) |
|
| ||||
| Diuretics | 74.4 | 74.9 | −0.5 (−9.0 to 8.0) | −0.5 (−9.0 to 7.9) |
ED = emergency department; HF = heart failure.
Adjusted estimates are differences in probability of the event between treatment and control groups estimated by logistic regression with site indicators as explanatory variables.
Adjusted estimates are differences in events per person-year between treatment and control groups estimated by Poisson regression with site indicators as explanatory variables and survival time as the exposure variable.
Angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, or hydralazine–dinitrate combination.
Discussion
A nurse management strategy to address documented shortfalls in patient self-management and clinical care was associated with fewer hospitalizations and improved functioning. These results have important clinical significance. At the end of the intervention, the average nurse management patient reported maintained functioning, with a slight limitation in physical activity, but the average usual care patient reported worse functioning and marked limitation in physical activity.
Our study contributes to knowledge about nurse management for patients with systolic dysfunction in 2 important ways. First, the results indicate that nurse management can be effective in minority communities, which is an important finding because these communities have a disproportionate burden from heart failure (2). We enrolled predominately non-Hispanic black and Hispanic patients and enlisted the ambulatory care practices that provide front-line heart failure care in these communities. The intervention incorporated culturally sensitive elements, including bilingual nurses and counseling based on local diets. The diversity of the hospitals, practices, and patients and the almost universal participation of clinicians enhanced the generalizability of the results to these populations.
Second, we showed that patients with systolic dysfunction who are treated in ambulatory care practices can benefit from nurse management. Trials of disease management and comprehensive discharge planning with postdischarge support for patients with heart failure, which are programs often led by nurses, have generally reported fewer readmissions among intervention patients than among control patients (16, 26–28). Except for 1 study, these studies identified patients while hospitalized, and several studies followed these patients for only 3 months after discharge (26, 27).
Of the 7 U.S. studies with quality-of-life measures, only 2 studies found better outcomes among intervention patients that were statistically significant (27, 29, 30). Despite greater disease burden among minority populations, these studies enrolled few minority patients. For example, nonwhite patients made up an average of only 14% of older patients with heart failure in trials of comprehensive discharge planning (28). Compared with patients in other heart failure studies that measured quality of life, our study patients were younger; this is consistent with heart failure epidemiology among black patients, who made up a higher percentage of our enrollment (29–36). The low educational levels in our patients were similar to those reported in other studies (30, 34, 36). Our study enrolled patients with more severe heart failure than those in the studies by Galbreath and colleagues (26) and Rich and colleagues (30); 59% of our patients were in NYHA classes III and IV, compared with 24% of patients in the former study (26), and our patients’ mean NYHA class was 2.9 (SD, 1.2), compared with 2.4 (SD, 1.0) in the latter study (30). Only our study limited enrollment to patients with documented systolic dysfunction. Galbreath and colleagues (26) concluded that the intervention in their study did not benefit patients with diastolic dysfunction.
The effectiveness of an intervention to improve the quality of care, such as our nurse management program, depends on the strength of the scientific evidence underlying the intervention and the room for improvement in patients’ care at baseline. Considerable shortfalls in self-management and clinical care existed in our communities and provided opportunities for improvement. The trial patients had documented systolic dysfunction and substantial risk for worsening and hospitalization. At enrollment, 59% were in NYHA class III and class IV, 41% had been hospitalized during the previous year, and 81% were ingesting more than 2 g of sodium daily (the maximum recommended) (3). The nurse management intervention implemented evidence-based guidelines to address these problems.
Our study differed on these 2 points from the Stan-ford University program in Kaiser Permanente, on which we modeled our program. A similar intervention among recently discharged Kaiser Permanente patients with heart failure did not reduce rehospitalizations (16, 37). Kaiser Permanente’s long orientation to preventing hospitalization may have left little room for improvement (38). The Stanford University program also identified patients with heart failure from clinical symptoms recorded in charts, and probably half of these patients did not have systolic dysfunction (16). As DeBusk and colleagues (16) commented, evidence-based guidelines for patients with heart failure and preserved left ventricular function are much less well developed. Guidelines have recommended that clinicians initially test to assess a patient’s left ventricular function (3, 39). In the absence of controlled trials on preserved left ventricular function, guidelines call for controlling underlying conditions and targeting symptom reduction (39). When efficacy studies have established elements of medical management that are associated with improved health outcomes for patients with diastolic dysfunction, it will be important to assess the effectiveness of a nurse-led intervention to improve that management.
Recent reviews have concluded that multidisciplinary heart failure management strategies that successfully reduced hospitalizations have incorporated follow-up by a specialized multidisciplinary team (27, 40). Like those programs, our intervention incorporated improving patient self-care and follow-up monitoring by specially trained staff. Instead of providing access to specialized clinics, our nurses coordinated care with patients’ usual clinicians, who were often general internists. One dimension of our program and many other successful programs was that the nurse met personally with the patient at the patient’s usual practice setting. This contact may have led the patient to bond with the nurse and rely on her for social support as the patient sought to improve self-management skills. Counseling about salt reduction was the only component of the intervention documented to differ between treatment groups. Although salt reduction may have played a role in avoiding hospitalizations, support from the nurse may have led patients to better adherence with the counseling. Consistent with this phenomenon, the benefits of nurse management to patients’ functioning seemed to accrue only while the nurse was in contact with the patient. Within months of the last contact, nurse management patients’ functioning began decreasing at a rate similar to that of patients who had received no counseling at all.
Study limitations include that only 3 nurses delivered the intervention, the sites were in 1 area with primarily non-Hispanic black and Hispanic patients, and 75% of patients came from 1 site. We also have not identified which patient and intervention characteristics accounted for improved outcomes during the intervention and their decline afterward. Few differences existed between study and control groups in the frequency with which various counseling measures were documented in patients’ medical records. Entries in patients’ medical records may not have reflected the nature, frequency, and extent of the counseling that occurred. To improve future multifaceted programs, it would be valuable to analyze precisely which components are associated with improved outcomes and which are not. To better target programs, it would also be valuable to determine whether certain patients are more or less likely to benefit from the intervention. Information on the program’s cost-effectiveness is also needed to guide the advisability of large-scale implementation.
Only 4.4% of our trial’s patients reported having no health insurance coverage (Table 2). This figure is similar to estimates from the National Hospital Ambulatory Medical Care Survey, 2000–2004 (unpublished data). Of the visits for patients with heart failure in the hospital outpatient clinics covered by this national probability sample, the expected source of payment for 6.8% was self-pay, no charge, or charity care (the closest approximation to lack of insurance). To the extent that patients with this chronic condition have more visits than average or that self-pay patients have insurance, the percentage of patients in the national sample who actually lack coverage would be lower.
In summary, a nurse management program following an evidence-based protocol can improve functioning and modestly reduce hospitalizations among predominately minority, low-educated ambulatory care patients who have systolic dysfunction. Continued contact with a nurse seemed to be needed to maintain the intervention’s effect.
Context
People with chronic conditions may need tailored, practical help for managing their conditions.
Contribution
This 12-month trial of assistance with managing systolic-dysfunction heart failure randomly assigned 406 ethnically diverse adults from Harlem, New York, to usual care or nurse management. Nurses counseled nurse management patients about sodium intake, fluid buildup, medication adherence, and self-management of symptoms; served as a bridge between patients and physicians; and regularly called patients to discuss problems. Compared with usual care patients, nurse management patients had fewer hospitalizations and better functioning.
Implications
Nurse management can improve some outcomes in ethnically diverse patients with systolic-dysfunction heart failure in ambulatory practices.
—The Editors
Acknowledgments
The authors thank the nurses who performed the intervention (Wanda Garcia, Adaga Catano, and Gema Richards), the project managers for the study (Aimee Quijano and Leah Tuzzio), the abstractors of cardiac test results (Meredith Reh and Van Hong Nguyen), the survey expert at Gfk NOP (previously RoperASW) for guidance in survey design and patient interviewing (Tim Nanneman), and the analyst who prepared the graphics (Jodi Casabianca). They also thank the key clinicians who supported planning and implementation at the participating hospitals—Aubrey Clarke at Harlem Hospital Center; Elliott Perla at Metropolitan Hospital Center; Valentin Fuster, Thomas McGinn, Elizabeth Clark, Marrick Kukin, and Catherine Halliday at Mount Sinai Medical Center; and Linda Williams at North General Hospital—and Nancy Houston Miller, who shared the materials developed for Stanford University’s Kaiser Permanente study and helped train the nurses.
Grant Support: By the Agency for Healthcare Research and Quality (R01 HS 10402).
Footnotes
Clinical Trials.gov identifier: NCT00211874.
Potential Financial Conflicts of Interest: None disclosed.
References
- 1.Kozak LJ, Hall MJ, Owings MF. Trends in avoidable hospitalizations, 1980–1998. Health Aff (Millwood) 2001;20:225–32. doi: 10.1377/hlthaff.20.2.225. [DOI] [PubMed] [Google Scholar]
- 2.Heart Disease and Stroke Statistics—2005 Update. Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 3.Konstam MA, Dracup K, Baker DW, Bottorff MB, Brooks NH, Dacey RA, et al. Heart Failure: Evaluation and Care of Patients with Left-Ventricular Systolic Dysfunction. Clinical Practice Guideline no. 11. Rockville, MD: Agency for Health Care Policy and Research; Jun, 1994. AHCPR publication no. 94-0612. [Google Scholar]
- 4.Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Am J Cardiol. 1999;83:1A–38A. [PubMed] [Google Scholar]
- 5.Stafford RS, Davidson SM, Davidson H, Miracle-McMahill H, Crawford SL, Blumenthal D. Chronic disease medication use in managed care and indemnity insurance plans. Health Serv Res. 2003;38:595–612. doi: 10.1111/1475-6773.00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horowitz CR, Rein SB, Leventhal H. A story of maladies, misconceptions and mishaps: effective management of heart failure. Soc Sci Med. 2004;58:631–43. doi: 10.1016/s0277-9536(03)00232-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heart failure treatment with angiotensin-converting enzyme inhibitors in hospitalized Medicare patients in 10 large states. The Large State Peer Review Organization Consortium. Arch Intern Med. 1997;157:1103–8. [PubMed] [Google Scholar]
- 8.Philbin EF, Lynch LJ, Rocco TA, Lindenmuth NW, Ulrich K, McCall M, et al. Does QI work? The Management to Improve Survival in Congestive Heart Failure (MISCHF) study. Jt Comm J Qual Improv. 1996;22:721–33. doi: 10.1016/s1070-3241(16)30278-4. [DOI] [PubMed] [Google Scholar]
- 9.Ansari M, Shlipak MG, Heidenreich PA, Van Ostaeyen D, Pohl EC, Browner WS, et al. Improving guideline adherence: a randomized trial evaluating strategies to increase beta-blocker use in heart failure. Circulation. 2003;107:2799–804. doi: 10.1161/01.CIR.0000070952.08969.5B. [DOI] [PubMed] [Google Scholar]
- 10.Island Peer Review Organization Health Care Quality Improvement Program no. 96-02. Lake Success, NY: Island Peer Review Organization; Feb, 1996. A Quality Improvement Study: Congestive Heart Failure Patient Education. [Google Scholar]
- 11.Retchin SM, Brown B. Elderly patients with congestive heart failure under prepaid care. Am J Med. 1991;90:236–42. [PubMed] [Google Scholar]
- 12.Billings J. Findings from the Ambulatory Care Access Project. New York: United Hospital Fund; 1993. [Google Scholar]
- 13.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–73. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 14.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153:1423–31. [PMC free article] [PubMed] [Google Scholar]
- 15.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 16.DeBusk RF, Miller NH, Parker KM, Bandura A, Kraemer HC, Cher DJ, et al. Care management for low-risk patients with heart failure: a randomized, controlled trial. Ann Intern Med. 2004;141:606–13. doi: 10.7326/0003-4819-141-8-200410190-00008. [DOI] [PubMed] [Google Scholar]
- 17.West JA, Miller NH, Parker KM, Senneca D, Ghandour G, Clark M, et al. A comprehensive management system for heart failure improves clinical outcomes and reduces medical resource utilization. Am J Cardiol. 1997;79:58–63. doi: 10.1016/s0002-9149(96)00676-5. [DOI] [PubMed] [Google Scholar]
- 18.Living with Heart Disease: Is It Heart Failure? Consumer guideline no. 11. Rockville, MD: Agency for Health Care Policy and Research; Jun, 1994. AHCPR publication no. 94-0614. [Google Scholar]
- 19.Liu H, Hays RD, Adams JL, Chen WP, Tisnado D, Mangione CM, et al. Imputation of SF-12 health scores for respondents with partially missing data. Health Serv Res. 2005;40:905–21. doi: 10.1111/j.1475-6773.2005.00391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–94. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 21.Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med. 2004;23:1455–97. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- 22.Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of Longitudinal Data. 2. Oxford, United Kingdom: Oxford Univ Pr; 2002. [Google Scholar]
- 23.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 24.Charlson M, Peterson J, Szatrowski TP, MacKenzie R, Gold J. Long-term prognosis after peri-operative cardiac complications. J Clin Epidemiol. 1994;47:1389–400. doi: 10.1016/0895-4356(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 25.Bennett SJ, Oldridge NB, Eckert GJ, Embree JL, Browning S, Hou N, et al. Comparison of quality of life measures in heart failure. Nurs Res. 2003;52:207–16. doi: 10.1097/00006199-200307000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Galbreath AD, Krasuski RA, Smith B, Stajduhar KC, Kwan MD, Ellis R, et al. Long-term healthcare and cost outcomes of disease management in a large, randomized, community-based population with heart failure. Circulation. 2004;110:3518–26. doi: 10.1161/01.CIR.0000148957.62328.89. [DOI] [PubMed] [Google Scholar]
- 27.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–9. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 28.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:1358–67. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 29.Kasper EK, Gerstenblith G, Hefter G, Van Anden E, Brinker JA, Thiemann DR, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002;39:471–80. doi: 10.1016/s0735-1097(01)01761-2. [DOI] [PubMed] [Google Scholar]
- 30.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–5. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 31.Gillum RF. Heart failure in the United States 1970–1985 [Editorial] Am Heart J. 1987;113:1043–5. doi: 10.1016/0002-8703(87)90077-9. [DOI] [PubMed] [Google Scholar]
- 32.Benatar D, Bondmass M, Ghitelman J, Avitall B. Outcomes of chronic heart failure. Arch Intern Med. 2003;163:347–52. doi: 10.1001/archinte.163.3.347. [DOI] [PubMed] [Google Scholar]
- 33.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 34.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 35.Pugh LC, Havens DS, Xie S, Robinson JM, Blaha C. Case management for elderly persons with heart failure: the quality of life and cost outcomes. MED-SURG Nursing. 2001;10:71–8. [Google Scholar]
- 36.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 37.Wagner EH. Deconstructing heart failure disease management [Editorial] Ann Intern Med. 2004;141:644–6. doi: 10.7326/0003-4819-141-8-200410190-00015. [DOI] [PubMed] [Google Scholar]
- 38.Miller RH, Luft HS. HMO plan performance update: an analysis of the literature, 1997–2001. Health Aff (Millwood) 2002;21:63–86. doi: 10.1377/hlthaff.21.4.63. [DOI] [PubMed] [Google Scholar]
- 39.Hunt SA. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2005;46:e1–82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 40.Fonarow GC. Heart failure disease management programs: not a class effect [Editorial] Circulation. 2004;110:3506–8. doi: 10.1161/01.CIR.0000151101.17629.20. [DOI] [PubMed] [Google Scholar]