Abstract
Mistaking psychogenic nonepileptic paroxysmal episodes (PNEPEs) for epileptic seizures (ES) is potentially dangerous, and certain features should alert physicians to a possible PNEPE diagnosis. Psychogenic nonepileptic paroxysmal episodes due to factitious seizures carry particularly high risks of morbidity or mortality from nonindicated emergency treatment and, often, high costs in wasted medical treatment expenditures. We report a case of a 28-year-old man with PNEPEs that were misdiagnosed as ES. The patient had been on four antiseizure medications (ASMs) with therapeutic serum levels and had had multiple intubations in the past for uncontrolled episodes. He had no episodes for two days of continuous video-EEG monitoring. He then disconnected his EEG cables and had an episode of generalized stiffening and cyanosis, followed by jerking and profuse bleeding from the mouth. The manifestations were unusually similar to those of ES, except that he was clearly startled by spraying water on his face, while he was stiff in all extremities and unresponsive. There were indications that he had sucked blood from his central venous catheter to expel through his mouth during his PNEPEs while consciously holding his breath. Normal video-EEG monitoring; the patient's volitional and deceptive acts to fabricate the appearance of illness, despite pain and personal endangerment; and the absence of reward other than remaining in a sick role were all consistent with a diagnosis of factitious disorder.
Keywords: Epilepsy, Psychogenic nonepileptic paroxysmal episodes, Pseudoseizures, Factitious disorder, Video-EEG
1. Introduction
The majority of reported psychogenic nonepileptic paroxysmal episodes (PNEPEs) consist of individuals with conversion disorder [1], [2]. Psychogenic nonepileptic paroxysmal episodes due to factitious disorder may be underrecognized and can be even more difficult to differentiate from epilepsy than conversion disorder. This increases the risk of misdiagnosis, which leads to inappropriate treatment, increased mortality risk, and unnecessary health-care costs [1], [3].
2. Case report
A 28-year-old man was transferred to our institution for video-EEG (vEEG) monitoring. His past medical history included depression, bipolar disorder, self-reported epilepsy, protein C deficiency, a central venous catheter (CVC), and chronic pain syndrome. Upon arrival, his neurological examination was normal despite several paroxysmal episodes, and his serum levels of multiple antiseizure medications (ASMs) were therapeutic. His complete laboratory workup and brain MRI were normal except for low hemoglobin.
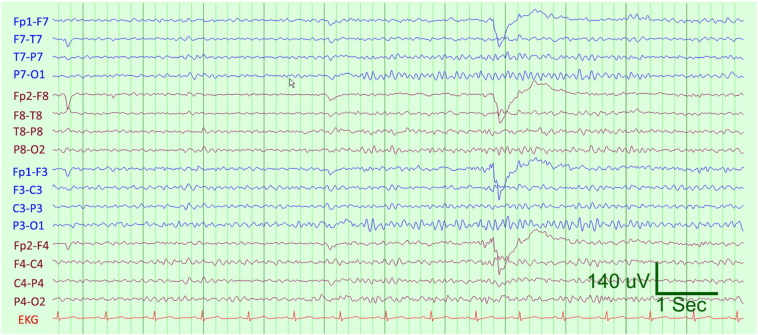
Continuous video-EEG monitoring for 48 h captured no episodes and showed normal EEG (Fig. 1). An episode occurred after he disconnected his own EEG leads, which consisted of cyanosis and irregular, arrhythmic, intermittent stiffening and jerking of both legs with forceful flexion of the toes and left arm, while the right arm was extended and internally rotated with unusual twisted finger positioning. He did not respond to painful stimuli. With subsequent events, blood spewed profusely from his mouth. His eyes were forcefully closed, but his pupils were normal in size and reactive. However, the patient was clearly startled by spraying water on his face.
Fig. 1.
Eleven-second sample of patient's normal EEG.
The patient was counseled about PNEPEs and was provided with appropriate psychiatric evaluation. However, he escaped from the hospital. Later, he returned and was intubated after multiple PNEPEs. Again, blood spewed from his mouth, but subsequent upper GI endoscopies and ENT examinations were unrevealing.
There were indications that he may have sucked blood out of his own CVC to expel through his mouth during his PNEPEs. His blood cultures were positive for Streptococcus viridans, and bleeding episodes ceased after removal of the catheter. Finally, the patient was transferred to the psychiatry ward and subsequently discharged. That same day, he was intubated at a third outside hospital following another PNEPE. The patient was recognized by staff as having been previously treated under an alias and was discharged the following day.
3. Discussion
Psychogenic nonepileptic paroxysmal episodes account for about 30% of referrals for refractory seizures [4]. Thus, it is paramount to analyze the clinical features of the episodes as video-EEG monitoring has limited availability [1], [2]. Features suggestive of PNEPE often refer to episodes occurring as part of a conversion disorder. These include preserved awareness and eye flutter, among others, contrasting with features consistent with ES that include postictal confusion, incontinence, seizures during sleep, tongue biting, and cyanosis [2], [3], [4]. Our subject bled from the mouth and became cyanotic during the episode, posing a particular diagnostic difficulty.
Our case demonstrates a rarer psychiatric diagnosis of Recurrent Factitious Disorder Imposed on Self 300.19 (F68.10), which is the repeated falsification of one's own physical or psychological signs or symptoms or induction of injury or disease. Although the behaviors are volitional, the patient may show little insight, and there is often uncertainty regarding conscious intent [5]. This is further complicated by deception and fabrication. Proposed motivations for volitional acts of deception have included the following: need of attention, desire to be cared for, maladaptive reaction to separation, and pleasure of deceiving others. In the Munchausen syndrome subtype, a person uses aliases and travels to further deceive. Factitious disorder is distinguished from malingering in which deceptive behavior is produced in order to gain an external reward.
In the few patients who have been studied, a childhood history of personal or parental illness, abandonment, and institutionalization is common [6]. There is no established psychiatric treatment for patients with the Munchausen subtype of factitious disorder [7]. Patients most commonly refuse or bring similar deception into psychiatric treatment. Treatment is often guided by the ethical injunction: first, do no harm.
Patients with factitious PNEPEs represent a clinical problem that is sporadic and high risk for the patient and produces extreme wastes in health care. A proposal would be to establish a national registry with collection of clinical data of patients with factitious PNEPEs. In this case, the hospitalizations cost $243,469.54, underscoring the importance of early detection, diagnosis, and case management. A multidisciplinary collaboration should be sought to establish a treatment plan with appropriate consultation with hospital administrators, attorneys, and ethics committee. Such a strategy could provide the rationale for research funding needed to adequately study factitious PNEPEs.
Author contributions
-
1.
Alissa Romano, DO — wrote and edited the manuscript.
-
2.
Saeed Alqahtani, MD — reviewed documents of the case and edited the manuscript.
-
3.
James L. Griffith, MD — reviewed and edited the manuscript.
-
4.
Mohamad Z. Koubeissi, MD — reviewed and edited the manuscript.
Conflict of interest
There are no financial disclosures to report as this was not part of any sponsored study.
References
- 1.Lafrance W.C., Baker G.A., Duncan R., Goldstein L.H., Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia. 2013;54:2005–2018. doi: 10.1111/epi.12356. [DOI] [PubMed] [Google Scholar]
- 2.Syed T.U., LaFrance W.C., Jr., Kahriman E.S., Hasan S.N., Rajasekaran V., Gulati D. Can semiology predict psychogenic nonepileptic seizures? A prospective study. Ann Neurol. 03/26/2011;69:997–1004. doi: 10.1002/ana.22345. [DOI] [PubMed] [Google Scholar]
- 3.Reuber M., Baker G.A., Gill R., Smith D.F., Chadwick D.W. Failure to recognize psychogenic nonepileptic seizures may cause death. Neurology. 2004;62:834–835. doi: 10.1212/01.wnl.0000113755.11398.90. [DOI] [PubMed] [Google Scholar]
- 4.Benbadis S.R. Nonepileptic behavioral disorders: diagnosis and treatment. Continuum (Minneap Minn) 2013;19:715–729. doi: 10.1212/01.CON.0000431399.69594.de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association . American Psychiatric Association; Arlington, Va.: 2013. Desk reference to the diagnostic criteria from DSM-5. [Google Scholar]
- 6.Ford C.V. The Munchausen syndrome: a report of four new cases and a review of psychodynamic considerations. Int J Psychiatry Med. 1973;4:31–45. doi: 10.2190/qe7c-d4jy-w3lq-y34c. [DOI] [PubMed] [Google Scholar]
- 7.Eastwood S., Bisson J.I. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77:209–218. doi: 10.1159/000126072. [DOI] [PubMed] [Google Scholar]