Abstract
Background
Despite a recent decline, Zimbabwe still has the fifth highest adult HIV prevalence in the world at 14.7%; 56% of the population are currently living in extreme poverty.
Design
Cross-sectional population-based survey of 18–22 year olds, conducted in 30 communities in south-eastern Zimbabwe in 2007.
Objective
To examine whether the risk of HIV infection among young rural Zimbabwean women is associated with socio-economic position and whether different socio-economic domains, including food sufficiency, might be associated with HIV risk in different ways.
Methods
Eligible participants completed a structured questionnaire and provided a finger-prick blood sample tested for antibodies to HIV and HSV-2. The relationship between poverty and HIV was explored for three socio-economic domains: ability to afford essential items; asset wealth; food sufficiency. Analyses were performed to examine whether these domains were associated with HIV infection or risk factors for infection among young women, and to explore which factors might mediate the relationship between poverty and HIV.
Results
2593 eligible females participated in the survey and were included in the analyses. Overall HIV prevalence among these young females was 7.7% (95% CI: 6.7–8.7); HSV-2 prevalence was 11.2% (95% CI: 9.9–12.4). Lower socio-economic position was associated with lower educational attainment, earlier marriage, increased risk of depression and anxiety disorders and increased reporting of higher risk sexual behaviours such as earlier sexual debut, more and older sexual partners and transactional sex. Young women reporting insufficient food were at increased risk of HIV infection and HSV-2.
Conclusions
This study provides evidence from Zimbabwe that among young poor women, economic need and food insufficiency are associated with the adoption of unsafe behaviours. Targeted structural interventions that aim to tackle social and economic constraints including insufficient food should be developed and evaluated alongside behaviour and biomedical interventions, as a component of HIV prevention programming and policy.
Introduction
Zimbabwe has seen a significant decline in HIV prevalence, driven in part by behaviour change [1–5]. Yet it still has one of the largest and most sustained HIV epidemics globally. In 2011 HIV prevalence among youth aged 15–24 years was 7.7% among females and 2.9% among males. [6].
The relationship between poverty and HIV infection in sub-Saharan Africa is complex and has been the subject of much debate over recent years [7–18]. A disproportionate number of those affected live in the poorer areas of the world, although HIV is not always concentrated among the poorest populations in these areas. [15, 19–24] The relationship between socio-economic position and HIV may also change over time with higher HIV prevalence shifting from the urban wealthy into impoverished and more rural populations. [10, 14, 25–28]
Socio-economic factors may act as a distal determinant of infection. Poor women are often economically dependent on men [11, 14, 29]. The need for economic support may partly drive earlier marriage and may make it difficult for young women to insist on safer sexual practices. Food insufficiency can also drive the adoption of high-risk behaviours.[18, 30, 31] It can also effect nutritional pathways which can affect both vertical and horizontal transmission of HIV.[18] The poorest women may have little choice but to adopt behaviours that put them at risk of infection, including transactional and intergenerational sex, earlier marriage, and relationships that expose them to violence and abuse. [7, 9, 11–14, 30–35] Poorer and less-educated women may be less knowledgeable about risks and therefore less able to adopt HIV risk-reducing behaviours. In many parts of rural Africa, this situation is fuelled by inadequate food supplies and malnutrition. [25, 30] This may be exacerbated further by high levels of rural-urban migration.
In 2007, 56% of Zimbabwe’s population were estimated to be living in extreme absolute poverty (on less than US$1 per day). [23] More recent estimates of the proportion living in absolute poverty are lacking but data from the 2012 Zimbabwe Census estimate that 72% of the population are living below the national poverty line.[36, 37] While rates of education and adult literacy remain relatively high compared to the rest of Africa these rates are now also falling, particularly among women. [23] Data from the UNDP Health Development Report for 2013 indicate that between 2006–2010 only 49% of females and 62% of males had at least secondary education and the mean years of schooling is now 7 years.[37] We present data from a population-based survey of 18–22 year olds living in South-Eastern Zimbabwe conducted in 2007 as the final survey of a cluster randomised trial of a community-based multi-component HIV prevention intervention for young rural Zimbabweans. [38, 39] At the time of the survey, Zimbabwe was experiencing extreme economic circumstances, the inflation rate was estimated to be over one million percent with market prices changing rapidly from day to day with multiple exchange rates in operation. The World Food programme estimated that around half of the population at that time were unable to meet their minimum food requirements and were needing assistance to survive.[40] In this context, we explore the relationship between socio-economic position and HIV status among young rural Zimbabwean women and whether different socio-economic domains (asset wealth; ability to afford essential items; and food sufficiency) are associated with HIV risk in different ways.
Methods
Study setting and trial design
The community-randomised trial was conducted in 30 rural communities in seven districts in three provinces in south-eastern Zimbabwe. The design of the trial, including sample size calculations, and details of the multi-component intervention are described elsewhere. [38, 39] The analysis reported here is restricted to female participants.
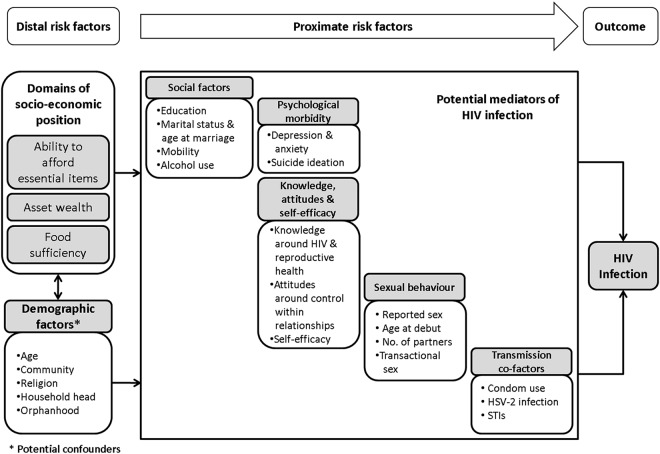
We hypothesised that poverty might be a cause of vulnerability to HIV among young rural Zimbabweans. We developed a conceptual framework postulating mechanisms by which different socio-economic factors might increase risk of HIV in the rural Zimbabwean context (see Fig. 1). The aim of the framework was to guide data collection and analysis in order to help disentangle the multiple risk factors that function at different levels among young rural Zimbabweans. [28, 41–53].
Fig 1. A conceptual framework for the association between domains of socio-economic position and HIV infection in young rural Zimbabwean women.
Procedures
Six enumeration areas of approximately 100 households were purposively selected in each of the 30 trial communities.[39] All 18–22 year olds who lived in the 180 selected enumeration areas were eligible for inclusion. Households were visited up to two times, after which time an individual was classified as unreachable. Participants provided written informed consent, and completed a self-administered paper-based questionnaire collecting information on factors shown in the framework.
Scales previously validated in South Africa were used to assess attitudes towards control within relationships. [54, 55] Psychological morbidity was assessed using the Shona Symptom Questionnaire (SSQ), a locally validated 14-item screening tool for those at risk of depressive and generalised anxiety disorders. [56] Potential socio-economic indicators were identified through reviewing a number of existing tools including Zimbabwe census questions and questions developed by UNICEF to assess poverty and socio-economic status.[57] In addition, focus group discussions and cognitive interviewing were conducted with community members to ensure that socio-economic indicators included on the questionnaire were contextually appropriate.[58] The final list of indicators incorporated standard UNICEF questions and questions that resulted from the qualitative research and were categorised under the three socio-economic domains identified in the conceptual framework. These were: 1) the ability of the household to afford essential items; 2) household ownership of ‘fixed’ and ‘sellable’ assets; and 3) food sufficiency. Table 1 lists the indicators included under each domain. [59, 60].
Table 1. Proportion of participants reporting individual wealth indicators.
| Characteristic | N | n | % |
|---|---|---|---|
| Ability to afford essential items: | |||
| Cannot afford: | |||
| To cook with cooking oil at each meal | 2518 | 1444 | 57.4 |
| To eat meat/fish at least 4x per week | 2478 | 1823 | 73.6 |
| To drink tea at least once/day | 2480 | 977 | 39.4 |
| To use soap to wash our clothes | 2484 | 546 | 22.0 |
| For each household member to have pair of shoes | 2485 | 1292 | 52.0 |
| To pay hospital fees if household member sick | 2488 | 1386 | 55.7 |
| Been absent from school due to no money for fees | 2475 | 1382 | 55.8 |
| SEP determined by ability to afford essential items: | 2327 | ||
| SEP1 (wealthiest) | 751 | 32.3 | |
| SEP2 | 727 | 31.2 | |
| SEP3 (poorest) | 849 | 36.5 | |
| Ownership of fixed and sellable assets: | |||
| Sellable assets—household owns: | |||
| Oxcart | 2518 | 1111 | 44.1 |
| Bicycle | 2458 | 901 | 36.7 |
| Motorcycle | 2437 | 69 | 2.8 |
| Car | 2432 | 293 | 12.0 |
| Plough | 2475 | 1889 | 76.3 |
| Radio | 2442 | 1370 | 56.1 |
| Television | 2429 | 683 | 28.1 |
| Telephone | 2427 | 466 | 19.2 |
| Own any luxury item (motrocycle/car/tv/telephone) | 2332 | 874 | 37.5 |
| Fixed assets: | |||
| Type of toilet: | 2572 | ||
| Field or bush | 679 | 26.4 | |
| Blair (long drop) or Flush toilet | 1893 | 73.6 | |
| House built of: | 2576 | ||
| Traditional materials (poles and dagga) or mud | 1983 | 77.0 | |
| Cement or stones | 593 | 23.0 | |
| Kitchen Floor: | 2584 | ||
| Dirt | 786 | 30.4 | |
| Cement | 1798 | 69.6 | |
| SEP determined by ownership of fixed and sellable assets: | 2316 | ||
| SEP1 (wealthiest) | 708 | 30.6 | |
| SEP2 | 719 | 31.0 | |
| SEP3 (poorest) | 889 | 38.4 | |
| Food sufficiency and security: | |||
| Sometimes we go to bed hungry | 2472 | 480 | 19.4 |
| Cannot afford to eat at least 2 meals each day | 2480 | 460 | 18.6 |
| Adult skipped a meal in last week so food for others | 2582 | 476 | 18.4 |
| Gone day without food in last week because no food | 2586 | 378 | 14.6 |
| Overall reported one or more indicators of insufficient food | 2577 | 1050 | 40.8 |
All participants had a dried blood sample collected which was tested for HIV-1 antibody at the National Microbiology Reference Laboratory in Harare using a validated testing algorithm [61]. All specimens were tested using two ELISA tests (Vironostika HIV Microelisa System BioMerieux, Inc., Durham NC and AniLabsytems EIA kit, AniLabsystems Ltd, Vantaa, Finland), with western blot used in the case of discrepant results. Specimens were further tested for antibodies to HSV-2 using a type-specific HSV-2 assay (Focus HerpeSelect EIA, Focus Technologies, Cypress CA) with the index for diagnosing positive samples raised to >3.4 to minimise false positives. [62]
Data analysis
Continuous variables were categorised using recognised cut-off values or dichotomised at the median value. Attitudinal and knowledge outcomes were divided into 11 domains, described elsewhere.[39] Binary variables were created identifying those participants who answered all questions correctly in each domain. Participants were classified as orphans if they reported they had lost one or both parents before they were 19 years old. For the mental health SSQ a summed-score of all 14 items was calculated and participants who answered affirmatively to 8 or more of the items were defined as being at risk of common mental disorders. [56]
A variable was created for each socio-economic domain. For sellable assets and essential items, ownership of the asset or ability to afford the item conferred a score of 1; not owning or being able to afford the item was given a score of 0. For ordinal measures, responses were scored on a scale between 0 and 1. For example, type of toilet in the homestead conferred a value of 0 for having to use field or bush, 0.5 for only having access to a neighbour’s toilet, or 1 where the homestead had its own toilet. Indices were created by adding the variable scores in each domain (the essential items summed-score included 7 variables; and the asset ownership score included 11 variables); and then splitting the summed score into three approximately equally sized groups (terciles) from the whole population. As other researchers have found [3], our simple summed-score index was strongly correlated with an index compiled using principal components analysis to weight the items (r≥0.95). Given that weighting indicators appeared to offer little advantage, the simpler summed score approach was used for all analyses. Food sufficiency was determined based on responses to 4 question items (see Table 1). Food insufficiency was defined as an affirmative response to one or more of these questions.
We described the characteristics of the population by level of socio-economic position (SEP). We then examined HIV status by each risk factor identified in the conceptual framework while not including SEP. Age-adjusted odds ratios were calculated and then adjusted (Model 1) for those demographic factors associated with HIV (p≤0.1). Odds ratios were then further adjusted (Model 2) for those risk factors higher in the conceptual framework that were associated with HIV (p≤0.1).
Cox regression (stratified on community) and Kaplan-Meier survival estimates were used to explore time to first marriage and sexual debut by SEP. For other sexual behaviour risk factors and for HIV we used conditional logistic regression to explore associations with SEP, controlling for clustering by community and presenting likelihood ratio tests. Where there was evidence of an association between SEP and HIV after adjusting for age, risk factors that were significant from the first stage of analysis were added to the model using a stepped approach that allowed us to examine how any influence of that socio-economic domain might be explained (‘mediated’) by differences in the more proximate risk factors.
Finally we explored the relationship between SEP and sexual behaviour using the same approach as described above. We created a binary composite variable for sexual risk by combining several sexual risk behaviour variables. ‘High sexual risk’ females were those who reported two or more of the following characteristics: sexual debut at 17yrs or younger; 2 or more lifetime partners; any partner 6 or more years older; and not using a condom at last sex. All other women, including those who reported that they had never had sex, were classified as ‘low sexual risk’.
Ethical approval
The trial and all research related to the trial was approved by the Medical Research Council of Zimbabwe and the ethics committees of University College London Hospitals and the London School of Hygiene & Tropical Medicine.
Results
Of 4822 eligible individuals identified at households, 4672 (97%) participated in the survey and were included in the analyses, 2593 (56%) of whom were female. The median age of female participants was 19 years. Just over 70% had completed ≥3 years of secondary education. Using categorical variables for marital status and age at first marriage, almost half (45%; 1175) were either currently or previously married; just under 60% of married females were married before they were 18 years old; 18% were married aged 16 or younger. Rates of orphaning were high; 47% (1087/2509) reported having lost one or both parents; 24% had lost their father, 7% their mother, and 16% had lost both parents.
Distribution of socio-economic indicators
Table 1 shows the proportion of female participants reporting individual socioeconomic indicators. There was a high level of correlation between all binary and ordinal poverty indicators and evidence of increased food insufficiency with decreasing socio-economic position as determined by the other SEP indices (chi-square test for trend p<0.001). For example 62% of those in the poorest socio-economic position defined by ability to afford essential and everyday items, reported insufficient food compared to 19% of those in the wealthiest category and 37% in the middle group. Similar proportions of food insufficiency were seen among SEP terciles defined by asset ownership (20% reported food insufficiency in the wealthiest tercile vs. 39% in the mid tercile and 60% in the poorest asset ownership group.
Socio-economic position and potential risk factors for HIV infection
Table 2 presents characteristics and potential risk factors for female participants by socio-economic position. Older females were more likely to report being poor (by all definitions of SEP) than younger women. Poorer women were more likely to live in female-headed households and less likely to live in a household with an older or more educated household head. Orphaning was more common among those of lower SEP. Educational attainment was strongly associated with each socio-economic domain with poorer females significantly less likely to have had any secondary education. Poorer women were significantly more likely to be married (test-for-trend p-value<0.001) and to be married younger.
Table 2. Characteristics of female participants by socio-economic position (SEP) and SEP domain.
| Domain of socio-economic position (SEP) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ability to afford essential items | Asset wealth | Food sufficiency | |||||||||||
| Characteristic | SEP1 1 | SEP2 | SEP3 2 | p-value 3 | SEP1 1 | SEP2 | SEP3 2 | p-value 3 | Food sufficient | Food insufficient | p-value 3 | ||
| N | (%) 4 | (%) 4 | (%) 4 | (%) 4 | (%) 4 | (%) 4 | (%) 4 | (%) 4 | |||||
| 751 | 32.3 | 31.2 | 36.5 | 30.6 | 31.0 | 38.4 | 59.2 | 40.8 | |||||
| Demographic: | |||||||||||||
| Age: | |||||||||||||
| 18 years | 287 | 38.2 | 38.9 | 32.9 | 38.4 | 39.2 | 32.3 | 38.2 | 35.0 | ||||
| 19–20 years | 245 | 32.6 | 28.6 | 31.6 | 32.2 | 31.8 | 29.6 | 31.6 | 29.3 | ||||
| 21–22 years | 219 | 29.2 | 32.5 | 35.6 | p = 0.018 | 29.4 | 28.9 | 38.1 | p<0.001 | 30.3 | 35.7 | p = 0.014 | |
| Religion: | |||||||||||||
| Catholic | 164 | 21.9 | 17.9 | 14.5 | 21.4 | 17.5 | 15.4 | 19.5 | 16.4 | ||||
| Protestant | 218 | 29.2 | 26.8 | 22.2 | 32.3 | 25.6 | 19.8 | 26.7 | 25.0 | ||||
| Apostolic/pentecostal | 229 | 30.7 | 33.9 | 40.4 | 27.5 | 36.6 | 41.2 | 34.1 | 36.8 | ||||
| Other | 126 | 16.9 | 18.3 | 21.0 | 17.4 | 18.9 | 20.6 | 18.2 | 19.1 | ||||
| None | 10 | 1.3 | 3.1 | 1.8 | p<0.001 | 1.4 | 1.4 | 2.9 | p<0.001 | 1.5 | 2.8 | p = 0.031 | |
| Distance from tar road: | |||||||||||||
| <15km | 265 | 35.3 | 33.7 | 31.4 | 35.4 | 33.2 | 31.8 | 35.2 | 31.4 | ||||
| 15–30km | 306 | 40.7 | 36.6 | 37.3 | 39.1 | 36.0 | 38.4 | 38.3 | 37.4 | ||||
| >30km | 180 | 24.0 | 29.7 | 31.2 | p = 0.020 | 25.4 | 30.7 | 29.8 | p = 0.158 | 26.5 | 31.1 | p = 0.022 | |
| Household head: | |||||||||||||
| Female | 211 | 28.3 | 34.3 | 38.5 | p<0.001 | 28.7 | 34.6 | 36.8 | p<0.001 | 32.3 | 36.7 | p = 0.019 | |
| 40 years or older | 424 | 56.7 | 55.6 | 54.2 | p = 0.612 | 59.5 | 57.8 | 50.6 | p<0.001 | 58.9 | 46.2 | p<0.001 | |
| Some primary or secondary education | 658 | 97.6 | 93.2 | 89.8 | p<0.001 | 96.2 | 95.8 | 88.8 | p<0.001 | 95.1 | 90.2 | p<0.001 | |
| Orphanhood: | |||||||||||||
| Orphan (lost one or both parents) | 279 | 37.9 | 47.4 | 55.8 | p<0.001 | 39.6 | 47.6 | 52.5 | p<0.001 | 42.0 | 55.2 | p<0.001 | |
| Social Factors: | |||||||||||||
| Education: | |||||||||||||
| Secondary education (1 year or more) | 690 | 91.9 | 86.7 | 81.3 | p<0.001 | 94.8 | 89.0 | 77.9 | p<0.001 | 90.1 | 78.4 | p<0.001 | |
| Marital status: | |||||||||||||
| Currently/have been married | 276 | 36.9 | 47.2 | 49.5 | p<0.001 | 34.0 | 42.6 | 54.2 | p<0.001 | 39.6 | 54.1 | p<0.001 | |
| Median age at first marriage (years) | 21.5 | 20.5 | 20.5 | p<0.001 | 22.5 | 21.5 | 20.5 | p<0.001 | 21.5 | 20.5 | p<0.001 | ||
| Time in community: | |||||||||||||
| 5 years or more | 343 | 50.1 | 57.5 | 64.7 | 49.5 | 60.0 | 63.9 | 56.1 | 59.8 | ||||
| 1–4 years | 104 | 15.2 | 11.2 | 11.3 | 14.0 | 11.3 | 12.0 | 12.9 | 11.4 | ||||
| 1 year or more but not continuously | 65 | 9.5 | 11.5 | 9.2 | 10.5 | 10.0 | 8.4 | 10.4 | 9.8 | ||||
| Less than a year or visiting | 173 | 25.3 | 19.8 | 14.8 | p<0.001 | 26.0 | 18.7 | 15.7 | p<0.001 | 20.5 | 19.0 | p = 0.361 | |
| Alcohol consumption: | |||||||||||||
| Drunk alcohol in last 4 weeks | 165 | 22.2 | 23.7 | 25.9 | p = 0.218 | 22.2 | 21.0 | 27.5 | p = 0.010 | 22.3 | 29.0 | p<0.001 | |
| Psychological morbidity and suicide ideation: | |||||||||||||
| Reported 8 or more symptoms of depression & anxiety | 389 | 62.7 | 71.3 | 76.2 | p<0.001 | 67.4 | 69.3 | 73.2 | p = 0.068 | 65.6 | 78.4 | p<0.001 | |
| Suicidal ideation in last week | 218 | 30.2 | 33.6 | 38.3 | p<0.001 | 32.9 | 30.3 | 37.8 | p = 0.029 | 27.7 | 45.9 | p<0.001 | |
| Knowledge, attitudes & self-efficacy: | |||||||||||||
| Knowledge: | |||||||||||||
| HIV acquisition (3 questions) 5 | 139 | 18.5 | 18.8 | 18.6 | p = 0.986 | 18.2 | 19.5 | 18.3 | p = 0.793 | 17.7 | 19.4 | p = 0.256 | |
| STI acquisition (2 questions) 5 | 333 | 44.3 | 37.4 | 36.3 | p = 0.001 | 44.4 | 36.7 | 37.0 | p = 0.004 | 40.5 | 34.8 | p = 0.003 | |
| Pregnancy prevention (2 questions) 5 | 274 | 36.5 | 28.1 | 28.2 | p<0.001 | 34.8 | 31.6 | 27.4 | p = 0.001 | 32.8 | 24.3 | p<0.001 | |
| Attitudes around control over sex: | |||||||||||||
| Responded to ≥7 questions correctly (10 questions) | 405 | 58.7 | 49.3 | 53.4 | p = 0.062 | 62.7 | 50.8 | 49.2 | p<0.001 | 59.0 | 43.8 | p<0.001 | |
| Control around sexual refusal (3 questions) 5 | 205 | 28.0 | 21.7 | 25.8 | p = 0.351 | 24.9 | 27.8 | 23.4 | p = 0.425 | 26.9 | 21.9 | p = 0.005 | |
| Control around sexual partners (4 questions) 5 | 263 | 37.0 | 30.2 | 31.3 | p = 0.020 | 37.7 | 32.4 | 29.8 | p = 0.001 | 36.8 | 24.3 | p<0.001 | |
| Control around safe sex (2 questions) 5 | 278 | 38.0 | 33.1 | 33.2 | p = 0.051 | 41.2 | 33.1 | 32.2 | p<0.001 | 37.8 | 29.4 | p<0.001 | |
| Self-efficacy: | |||||||||||||
| Condom self-efficacy (3 questions) 5 | 464 | 62.4 | 63.5 | 65.0 | p = 0.570 | 66.9 | 62.2 | 62.4 | p = 0.104 | 63.7 | 62.4 | p = 0.508 | |
| Sexual refusal self-efficacy (2 questions) 5 | 535 | 72.1 | 68.5 | 70.4 | p = 0.324 | 75.2 | 70.2 | 67.3 | p<0.001 | 73.0 | 61.2 | p<0.001 | |
| HIV testing self-efficacy (3 questions) 5 | 535 | 71.7 | 69.4 | 70.2 | p = 0.620 | 74.2 | 70.6 | 68.4 | p = 0.011 | 72.6 | 64.3 | p<0.001 | |
| Sexual risk factors 5 : | |||||||||||||
| Reported (vaginal) sex | 327 | 44.7 | 53.8 | 58.2 | p<0.001 | 45.2 | 48.0 | 61.5 | p<0.001 | 47.4 | 61.2 | p<0.001 | |
| Sexual debut younger than 18 years | 125 | 17.1 | 24.9 | 26.9 | p<0.001 | 15.7 | 22.4 | 28.0 | p<0.001 | 18.2 | 31.8 | p<0.001 | |
| Median age at sexual debut (years) | 20.5 | 19.5 | 19.5 | p<0.001 | 20.5 | 20.5 | 19.5 | p<0.001 | 20.5 | 19.5 | p<0.001 | ||
| 2 or more lifetime partners | 72 | 9.8 | 10.2 | 13.5 | p = 0.021 | 10.0 | 9.8 | 13.1 | p = 0.060 | 9.3 | 14.0 | p = 0.001 | |
| Had a sexual partner who was >5 years older | 137 | 18.7 | 22.6 | 26.2 | p<0.001 | 20.9 | 19.7 | 26.9 | p = 0.004 | 20.0 | 28.0 | p<0.001 | |
| Had sex for material/financial support | 70 | 9.6 | 9.4 | 12.5 | p = 0.081 | 7.9 | 8.3 | 13.2 | p<0.001 | 7.9 | 16.8 | p<0.001 | |
| Transmission co-factors: | |||||||||||||
| Use condoms inconsistently or never use 5 | 324 | 44.3 | 52.4 | 58.2 | p<0.001 | 44.3 | 47.7 | 61.0 | p<0.001 | 46.8 | 60.7 | p<0.001 | |
| No condom used at last sex 5 | 244 | 33.6 | 41.9 | 44.8 | p<0.001 | 33.3 | 37.3 | 48.8 | p<0.001 | 36.2 | 47.0 | p<0.001 | |
| Reported one or more symptoms of STD | 217 | 29.0 | 33.0 | 38.1 | p<0.001 | 29.3 | 31.1 | 38.8 | p<0.001 | 30.6 | 40.8 | p<0.001 | |
| HSV-2 positive | 74 | 10.1 | 11.1 | 11.3 | p = 0.713 | 5.6 | 8.8 | 12.8 | p = 0.004 | 9.1 | 14.3 | p<0.001 | |
1 Wealthiest category (SEP1);
2 Poorest category (SEP3);
3 P-value from Chi-square test, Mantel-Haenszel test-for-trend (given in italics where chi-square p≤0.05) or Cox proportional hazard depending on type of data;
4 Column percentages (%);
5 Reference category includes those who have never had sex.
The proportion of participants at risk of common mental disorders increased as socio-economic position decreased; 46% of females who had insufficient food reported considering suicide at some point in the previous week, compared to 28% of those who had not had to go without food. However, there was no evidence of association between SEP and knowledge of HIV acquisition for any of the socio-economic domains. Attitudes around control within relationships were strongly associated with food sufficiency status with food insufficient women reporting less control. The lowest levels of self-efficacy were also seen among this group of women.
Risk factors for HIV infection
Overall HIV prevalence was 7.7% (95%CI: 6.7–8.7) and there was increasing HIV risk with increasing age (Table 3). After adjusting for age the only demographic factor significantly associated with HIV infection was the age of the household head. Of the social factors (see Fig. 1), education, marital status, age of first marriage and alcohol consumption were all strongly associated with HIV infection even after adjusting for age and age of household head. Having some secondary education was associated with lower HIV prevalence, whereas ever being married was associated with a higher prevalence of HIV infection. Alcohol consumption in the last 4 weeks was also significantly associated with higher prevalence of HIV. After further adjusting for all demographic and social variables in Model 2, there was weak evidence that education was associated with reduced risk of HIV infection but there continued to be strong evidence of increased risk associated with marital status.
Table 3. Risk factors for HIV infection excluding socio-economic position.
| Characteristic | Proportion HIV positive | Age-adjusted OR a [95% CI] | Age-adjusted Model 11, a | Age-adjusted Model 2 (n = 2022)2, a | |||||
|---|---|---|---|---|---|---|---|---|---|
| n/N | % | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | ||
| Demographic: | |||||||||
| Age: | p<0.001 | p<0.001 | |||||||
| 18 years | 21/953 | 2.2 | 1.00 | 1.00 | |||||
| 19–20 years | 62/794 | 7.8 | 3.74 | [2.25–6.21] | 4.09 | [2.38–7.03] | |||
| 21–22 years | 116/841 | 13.8 | 7.13 | [4.41–11.51] | 7.57 | [4.52–12.66] | |||
| Age of household head: | p = 0.004 | p = 0.003 | |||||||
| Under 40 years old | 115/1191 | 9.7 | 1.00 | ||||||
| 40 years or older | 81/1374 | 5.9 | 0.64 | [0.47–0.86] | 0.62 | [0.45–0.85] | |||
| Social Factors: | |||||||||
| Education: | p = 0.002 | p = 0.012 | p = 0.066 | ||||||
| None/primary | 42/380 | 11.0 | 1.00 | 1.00 | 1.00 | ||||
| Secondary or higher education | 154/2194 | 7.0 | 0.54 | [0.37–0.78] | 0.60 | [0.40–0.88] | 0.63 | [0.39–1.02] | |
| Marital status: | p<0.001 | p<0.001 | p<0.001 | ||||||
| Never | 39/1403 | 2.8 | 1.00 | 1.00 | 1.00 | ||||
| Currently/have been married | 160/1176 | 13.6 | 3.86 | [2.62–5.69] | 3.86 | [2.58–5.77] | 2.82 | [1.75–4.53] | |
| Age first married: | p = 0.017 | p = 0.041 | p = 0.433 | ||||||
| 17 or older/never married | 143/2168 | 6.6 | 1.00 | 1.00 | 1.00 | ||||
| 16 or younger | 23/169 | 13.9 | 1.88 | [1.15–3.06] | 1.73 | [1.04–2.85] | 1.27 | [0.70–2.30] | |
| Alcohol drunk in last 4 weeks: | p = 0.001 | p = 0.002 | p = 0.219 | ||||||
| Never drunk alcohol/no alcohol last 4 wks | 127/1916 | 6.6 | 1.00 | 1.00 | 1.00 | ||||
| Drunk alcohol in last 4 weeks | 68/638 | 10.7 | 1.76 | [1.27–2.43] | 1.72 | [1.24–2.39] | 1.30 | [0.86–1.98] | |
| Psychological Morbidity: | |||||||||
| Suicide ideation in last week: | p = 0.022 | p = 0.059 | p = 0.075 | ||||||
| Never considered suicide | 101/1546 | 6.5 | 1.00 | 1.00 | 1.00 | ||||
| Sometimes/always feel like committing suicide | 78/835 | 9.3 | 1.46 | [1.06–2.00] | 1.37 | [0.99–1.89] | 1.21 | [0.82–1.78] | |
| Knowledge, attitudes & self-efficacy: | |||||||||
| Knowledge: | |||||||||
| Around pregnancy prevention (2 questions): | p = 0.025 | p = 0.032 | p = 0.006 | ||||||
| Low | 150/1829 | 8.2 | 1.00 | 1.00 | 1.00 | ||||
| Both question responses ‘correct’ | 48/756 | 6.4 | 0.68 | [0.48–0.96] | 0.69 | [0.48–0.98] | 0.61 | [0.40–0.94] | |
| Attitudes around control over sex | |||||||||
| Control around sexual partners (4 questions): | p = 0.090 | p = 0.051 | p = 0.038 | ||||||
| Low | 107/1612 | 6.6 | 1.00 | 1.00 | 1.00 | ||||
| All 4 question responses ‘correct’ | 68/751 | 9.0 | 1.33 | [0.96–1.85] | 1.40 | [1.00–1.95] | 1.46 | [0.98–2.18] | |
| Self-efficacy: | |||||||||
| Condom self-efficacy (3 questions) | p = 0.004 | p = 0.003 | p = 0.049 | ||||||
| Poor | 45/941 | 4.8 | 1.00 | 1.00 | 1.00 | ||||
| All 3 question responses ‘correct’ | 152/1612 | 9.4 | 1.65 | [1.16–2.36] | 1.71 | [1.19–2.45] | 1.38 | [0.89–2.14] | |
| Sexual Risk Factors: | |||||||||
| Reported vaginal sex: | p<0.001 | p<0.001 | p = 0.487 | ||||||
| Never had sex/never had vaginal sex | 28/1175 | 2.4 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 165/1326 | 12.4 | 3.87 | [2.51–5.97] | 3.99 | [2.54–6.28] | 1.31 | [0.61–2.83] | |
| Sexual debut (vaginal sex): | p<0.001 | p<0.001 | p = 0.447 | ||||||
| Never had sex/18 or older | 121/1910 | 6.3 | 1.00 | 1.00 | 1.00 | ||||
| Younger than 17 years | 72/591 | 12.2 | 2.07 | [1.50–2.85] | 2.02 | [1.45–2.81] | 1.19 | [0.76–1.86] | |
| Number of partners: | p<0.001 | p<0.001 | p = 0.383 | ||||||
| Never had sex/Only 1 lifetime partner | 141/2223 | 6.3 | 1.00 | 1.00 | 1.00 | ||||
| Two or more lifetime partners | 52/278 | 18.7 | 2.34 | [1.63–3.38] | 2.37 | [1.64–3.43] | 1.25 | [0.76–2.08] | |
| Age of partners: | p<0.001 | p<0.001 | p = 0.060 | ||||||
| Never had sex/partners same age (+/-5 yrs) or younger | 101/1924 | 5.2 | 1.00 | 1.00 | 1.00 | ||||
| Any partner 6–10 yrs older | 56/373 | 15.0 | 2.45 | [1.70–3.52] | 2.51 | [1.73–3.63] | 1.48 | [0.92–2.37] | |
| Any partner >10 yrs older | 36/204 | 17.6 | 3.09 | [1.99–4.80] | 3.21 | [2.06–5.01] | 1.89 | [1.07–3.33] | |
| Transactional sex: | |||||||||
| Had sex with partner for material/other support: | p<0.001 | p<0.001 | p = 0.170 | ||||||
| Never had sex/never had transactional sex | 148/2214 | 6.7 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 45/287 | 15.7 | 2.34 | [1.60–3.42] | 2.26 | [1.54–3.32] | 1.45 | [0.86–2.46] | |
| Transmission co-factors: | |||||||||
| Condom use: | |||||||||
| Used condom at last sex with last partner: | p = 0.005 | p = 0.012 | p = 0.046 | ||||||
| Never had sex/used a condom at last sex | 75/1475 | 5.1 | 1.00 | 1.00 | 1.00 | ||||
| Did not use a condom at last sex | 117/1011 | 11.6 | 1.59 | [1.14–2.21] | 1.55 | [1.10–2.17] | 0.58 | [0.34–0.98] | |
| Reported condom use with any partner: | p<0.001 | p<0.001 | p = 0.312 | ||||||
| Never had sex/always used a condom with all partners | 29/1189 | 2.4 | 1.00 | 1.00 | 1.00 | ||||
| Only sometimes/never used condoms with any partner | 164/1312 | 12.5 | 3.80 | [2.48–5.83] | 3.90 | [2.50–6.09] | 1.47 | [0.70–3.10] | |
| Sexually transmitted infections: | |||||||||
| Reported any symptom of STI: | p = 0.001 | p = 0.004 | p = 0.387 | ||||||
| No | 103/1671 | 6.2 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 92/891 | 10.3 | 1.65 | [1.22–2.24] | 1.58 | [1.16–2.16] | 1.20 | [0.80–1.80] | |
| Biomarker for HSV-2 infection: | p<0.001 | p<0.001 | p<0.001 | ||||||
| Negative | 75/2226 | 3.4 | 1.00 | 1.00 | 1.00 | ||||
| Positive | 99/279 | 35.5 | 12.83 | [8.91–18.47] | 12.24 | [8.43–17.77] | 8.60 | [5.57–13.27] | |
1 Adjusted for age and age of household head.
2 Adjusted for age and age of household head and other variables higher in conceptual framework (Fig. 2) that remain associated (at p≤0.1) with HIV after adjustment.
a Likelihood ratio p-value.
After adjustment for potential confounders and those social factors associated with HIV infection there was little evidence that psychological morbidity was associated with HIV. Only three of the knowledge and attitudinal outcomes were associated with HIV infection, although the direction of effect differed depending on the item (see Table 3). After adjusting for age and other potential confounding factors (Model 1) there was strong evidence of an association between reported sexual behaviours and increased risk of HIV infection. However, after further adjusting for those factors higher in the conceptual framework that were associated with HIV (Model 2), there remained only a borderline significant association with age of sexual partners. Not using a condom during last sexual encounter was initially associated with a higher prevalence of HIV (see age-adjusted and adjusted OR in Model 1); however controlling for other factors in Model 2 led to a change in the direction of effect with lack of condom use at last sex appearing now to be associated with a reduced risk of HIV suggesting an association with one of the other proximate risk factors or some unmeasured factor. HSV-2 infection was strongly associated with HIV infection.
Socio-economic position and HIV infection
The prevalence of HIV varied little between SEP categories for the SEP domains defined by ability to afford essential items and ownership of fixed and sellable assets (Table 4). However, there was evidence of an association between food sufficiency and HIV infection (aOR 1.6). Further adjusting for social factors associated with HIV (Model 3) led to a fall in the OR to 1.4, suggesting that differences in these social factors between women with sufficient and insufficient food partly explained the difference seen in HIV prevalence. The OR fell further as the model was adjusted for knowledge, attitudes and self-efficacy variables (Model 4), for sexual risk factors (Model 5) and finally for transmission co-factors (Model 6), with the final adjusted OR being 1.27 (95% CI: 0.84–1.94). Each fall in OR suggests that these proximate factors mediated the relationship between food sufficiency and HIV among these female participants.
Table 4. Socio-economic position as a risk factor for HIV infection among females by socio-economic domain.
| Characteristic | Proportion HIV positive | Age-adjusted OR [95% CI[ | Adjusted OR Model 3 1 | Adjusted OR Model 4 2 | Adjusted OR Model 5 3 | Adjusted OR Model 6 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n/N | % | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Domains of socio-economic position (SEP) | ||||||||||||
| SEP defined by ability to afford essential items: | p = 0.926 | |||||||||||
| SEP 1 (Wealthiest) | 52/748 | 6.9 | 1.00 | |||||||||
| SEP 2 | 51/727 | 7.0 | 0.92 | [0.57–1.47] | ||||||||
| SEP 3 (Poorest) | 68/847 | 8.0 | 0.99 | [0.64–1.53] | ||||||||
| SEP defined by ownership of fixed & sellable assets: | p = 0.839 | |||||||||||
| SEP 1 (Wealthiest) | 47/707 | 6.6 | 1.00 | |||||||||
| SEP 2 | 44/717 | 6.1 | 0.95 | [0.58–1.55] | ||||||||
| SEP 3 (Poorest) | 76/887 | 8.6 | 1.09 | [0.69–1.70] | ||||||||
| Food sufficiency & security: | p = 0.009 | p = 0.079 | p = 0.082 | p = 0.113 | p = 0.261 | |||||||
| Food sufficient | 92/1524 | 6.0 | 1.00 | |||||||||
| Food insufficient 5 | 104/1049 | 9.9 | 1.64 | [1.13–2.36] | 1.40 | [0.96–2.04] | 1.41 | [0.96–2.08] | 1.37 | [0.93–2.03] | 1.27 | [0.84–1.94] |
1 Adjusted for age, age of household head, education, marital status & alcohol consumption.
2 Adjusted for variables in model 3 & knowledge around pregnancy prevention, attitudes around sexual partners & condom self-efficacy.
3 Adjusted for variables in model 4 & age of sexual partners.
4 Adjusted for variables in model 5 & condom use at last sex & HSV-2 infection.
5 Food insufficiency—reported adult skipping meals and/or going day without food; going to bed hungry; <2 meals per day.
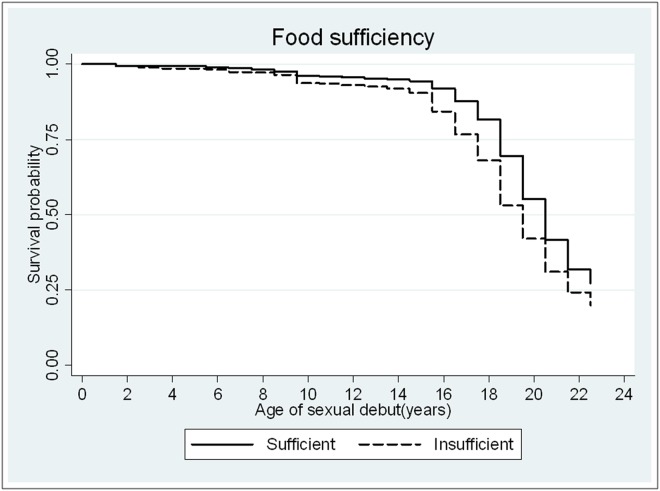
Determinants of risky sexual behaviour
There was strong evidence of association between SEP and most aspects of reported sexual behaviour, in all three socio-economic domains (Table 3). Poorer women were more likely to report ever having had (vaginal) sex; to have experienced earlier sexual debut; to have had more partners and partners who were 6 or more years older and to report having had sex for material or financial support. Women who reported having insufficient food reported earlier sexual debut (age adjusted HR = 1.49; 95% CI: 1.33–1.66—see Fig. 2) and were more likely to report sex for material or financial support (age-adjusted OR = 2.30; 95% CI: 1.78–2.98).
Fig 2. Survival time to age at sexual debut by food sufficiency status.
Rates of reported condom use were generally low, only 59.6% of all women reported using a condom at last sex (vaginal, anal, consensual or non-consensual). Poorer women were significantly less likely to report condom use than women in the wealthier SEP categories for all 3 socio-economic domains. There was evidence of increasing prevalence of reported symptoms of STIs with declining SEP. Women who had insufficient food were more likely to be HSV-2 positive (aOR 1.7 95% CI: 1.30–2.20).
There was also a significant association seen between SEP and reporting two or more high-risk sexual behaviours among these young women (Table 5), even after adjusting for age, with those women categorised in the poorest categories of each socio-economic domain more likely to report high-risk behaviours than those in the wealthiest categories. For example, women reporting insufficient food were more likely to report two or more high-risk behaviours than women with sufficient food supply (aOR 1.6; 95% CI: 1.3–2.0). These associations remained significant after adjusting for potential confounding factors although there was a slight fall in the ORs for the association in each case (Model 1). After adjusting for those social factors that were associated with reporting risky sexual behaviour (Model 2), the OR for the association between SEP and risky behaviour fell for all three socio-economic domains suggesting that the influence of asset wealth on higher risk behaviours was explained in part through differences in educational attainment, marital status and alcohol consumption between these SEP groups. Adjusting these estimates further by incorporating psychological, knowledge, attitudinal and self-efficacy variables in the model (Model 3) led to little change in the OR for risky behaviour associated with food sufficiency.
Table 5. Socio-economic position as a risk factor for reporting risky sexual behaviour by socio-economic domain.
| Prevalence of ‘high risk’ behaviour 1 | Age-adjusted OR | Adjusted OR Model 1 2 | Adjusted OR Model 2 3 | Adjusted OR Model 3 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Domains of Socio-economic position (SEP): | ||||||||||
| SEP defined by ability to afford essential items: | p = 0.009 | p = 0.030 | p = 0.547 | p = 0.594 | ||||||
| SEP 1 (Wealthiest) | 198 | 26.4 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| SEP 2 | 238 | 32.7 | 1.38 | [1.04–1.81] | 1.35 | [1.02–1.78] | 1.05 | [0.77–1.43] | 1.04 | [0.76–1.43] |
| SEP 3 (Poorest) | 313 | 36.9 | 1.49 | [1.14–1.94] | 1.40 | [1.07–1.84] | 1.18 | [0.87–1.60] | 1.16 | [0.86–1.59] |
| SEP defined by ownership of fixed & sellable assets: | p = 0.014 | p = 0.042 | p = 0.467 | p = 0.584 | ||||||
| SEP 1 (Wealthiest) | 192 | 27.1 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| SEP 2 | 217 | 30.2 | 1.07 | [0.81–1.41] | 1.04 | [0.79–1.38] | 0.82 | [0.60–1.13] | 0.84 | [0.61–1.16] |
| SEP 3 (Poorest) | 332 | 37.4 | 1.43 | [1.10–1.87] | 1.36 | [1.04–1.78] | 0.88 | [0.64–1.20] | 0.90 | [0.66–1.23] |
| Food sufficiency & security: | p<0.001 | p<0.001 | p = 0.044 | p = 0.072 | ||||||
| Food sufficient | 424 | 27.8 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Food insufficient 5 | 419 | 39.9 | 1.60 | [1.29–1.98] | 1.51 | [1.21–1.88] | 1.29 | [1.01–1.66] | 1.26 | [0.98–1.63] |
1 ‘High risk’ behaviour defined as 2 or more risky behaviours: sexual debut ≤17yrs; ≥2 lifetime partners; any partner ≥6 years older; not using a condom at last sex.
2 Adjusted for age, age of household head & orphanhood.
3 Adjusted for variables in model 1 & education, marital status & alcohol consumption.
4 Adjusted for variables in model 2, risk of depression & anxiety, suicide ideation, attitudes around sexual refusal and sexual partners and condom self-efficacy.
5 Food insufficiency—reported adult skipping meals and/or going day without food; going to bed hungry; <2 meals per day.
Discussion
Among young rural Zimbabwean women, indicators of lower socio-economic position were associated with lower educational attainment, earlier marriage, higher rates of symptoms of depression and anxiety and suicidal ideation. Food insufficiency was associated with lower levels of HIV knowledge, less strong attitudes around sexual control and poorer self-efficacy. Lower SEP was also associated with high-risk sexual behaviours. In particular, insufficient food was strongly associated with increased reporting of these behaviours and was also strongly associated with lack of condom use, reporting ever had symptoms of STIs and HSV-2 infection. The more robust relationship between food insufficiency and sexual risk than the other SEP domains investigated here, may reflect the temporal nature of those domains which could have been influenced by the Zimbabwean economy and HIV epidemic within Zimbabwe.[58] It is not possible from this study to determine how socio-economic position has changed over time and it is possible that food insufficiency is more of a reflection of current wealth whereas asset ownership may reflect economic wealth in the recent past. Likewise with the domain ‘ability to afford essential items’, whilst several of the items used to assess this e.g. ability to afford cooking oil and tea, likely reflect the level of current disposable income, owning shoes and absenteeism from school due to lack of fees are more likely to indicate poverty over a longer period of time. It may also be that being poor itself does not drive high-risk behaviours, but being poor to the point of having insufficient food and being hungry, or having hungry children in a household, instigates a need among these women to do whatever is required to survive including disregarding their own safety and health. The relationship between food insufficiency and high risk sexual behaviours was further supported by some evidence of an association between food insufficiency and HIV prevalence among these women. This relationship appeared to be explained in part through differences in social factors such as marriage, education and alcohol use, and in more proximate risk factors such as psychological morbidity, knowledge, attitudes, self-efficacy and sexual behaviour.
This study had a number of strengths, including a high response rate and large sample size. We also included data on a range of lifestyle and economic indicators, sexual behaviour and biomarkers for both HIV and HSV-2. This enabled us to explore a number of hypothesised relationships outlined in the conceptual framework, whilst incorporating different aspects of poverty and other factors (e.g. psychological morbidity).
A key limitation of the study was that the data were cross-sectional. It was therefore not possible to infer the temporality of the associations seen here. Where associations were seen, we could not assess whether poverty increased risk of HIV infection, or, whether risk poverty arose as a consequence of HIV infection. A further potential limitation relates to the validity of reported sexual behaviour data, an issue affecting all sexual behaviour research among young people in Africa. [49, 63–69] While we implemented best-practice approaches to the collection of these data, limitations in their validity may remain. Measuring income and/or expenditure is generally considered the gold standard measure of socio-economic position, while we measured assets, ability to pay and food security. While our approach again has limitations, at the time of the survey market prices fluctuated radically and rapidly, inflation was in excess of one million percent and there were multiple exchange rates in operation, making any kind of monetary monitoring almost impossible. [70] While the proportion of participants reporting food insufficiency seems high, World Food Programme estimates of the number of people requiring food aid in Zimbabwe at that time also suggest high levels of food insecurity. [40] Despite inflation stabilising, the position regarding food security has not changed significantly since the study was conducted. Recent estimates suggest that only 49% of Zimbabweans were food secure in 2012. [71] The World Food programme predictions of the number of people who will be food insecure in the next year continue to increase with an estimated 2.2 million people (one in four of the rural population), expected to need food assistance in the next year. [72]
While there were associations between asset wealth and sexual behaviour, in contrast with some previous studies [10, 26, 73], we found no association between either asset wealth or ability to afford essential items and HIV prevalence among this population. As discussed earlier, the populations most at risk tend to change over time. [14, 25] Between 1998 and 2003 HIV incidence was associated with asset wealth among young men in Manicaland, but there was no association between wealth index and incidence among young women. [3] Some studies have used alternative indicators of socio-economic position to those used here such as household income, education and occupation. [14, 74]. We found educational attainment to be strongly correlated with socio-economic position, and it was associated with lower prevalence of HIV and less reporting of risky sexual behaviours. These results concur with results from other studies that have demonstrated a protective effect of education on sexual behaviour and/or on HIV prevalence. [3, 27, 28, 32, 75–78]
The study data did suggest an association between food insecurity, our third domain of socioeconomic position, and HIV prevalence. Few studies have explored how food insufficiency contributes to the spread of HIV although the likelihood and plausibility of the association have frequently been discussed. [12, 15, 18, 29, 30, 33, 34, 79] A study in Botswana and Swaziland found similar results to those reported here with food insufficiency among women significantly associated with increased HIV risk behaviour although no biomarkers of risk were collected in that study. [30] Qualitative research conducted in southern Zambia by Bryceson et al. demonstrated how participants believe that hunger is a driver of the HIV epidemic, particularly for women. [80] More recently Tsai et al. reported on a study of sexually active women in Brazil which demonstrated that severe food insecurity was associated with reduced odds of condom use and an increase in potential symptoms of STIs. Of note, severe food insecurity was associated with increased risk taking even after controlling for household wealth and did not appear to be mediated either by gender power inequity or poor nutrition. The authors concluded that lack of food security appeared to have a direct association with sexual risk taking which would appear to support the relationship seen in this study between food insufficiency and HIV risk behaviours. Furthermore, a project conducted in Malawi, giving cash transfers to young women showed a reduction in risk of HIV infection among these women associated with the relatively small increase in economic security.[81, 82] The influence of food security as a driver for adopting risky sexual behaviours among these young Zimbabwean women is important particularly in light of the current level of food aid that appears to be needed within the country. [40, 72] The importance of food insecurity is increasingly being recognised as a variable of central importance in HIV prevention efforts and the integration of nutrition and HIV/AIDS programming activities is more and more frequently discussed and proposed. [18, 81–85]
The extreme economic circumstances that Zimbabwe endured at the time of this study may influence the comparability of the results to other populations. However, the turmoil experienced by Zimbabwe over recent years is not unique in Africa. Given the paucity of research that explores the link between poverty and HIV during times of rapid economic contraction, this study provides an important and relevant addition to this field of research. The overall decline in HIV infection within Zimbabwe during a time when the levels of poverty, particularly food insufficiency, and unemployment were undeniably increasing, challenges the idea that poverty was driving the overall epidemic trajectory in Zimbabwe over this period [4, 86, 87]. However, the evidence presented here suggests that the poorest young women, particularly those who did not have access to sufficient food, had riskier sexual behaviour and were at increased risk of HIV and HSV-2.
The increased prevalence of high-risk behaviours and HIV in those young women of lower socio-economic position is a cause for concern. Programme planners need to ensure that those made vulnerable through increasing poverty and food insufficiency are successfully and appropriately targeted. There are many practical and ethical difficulties in determining how to deliver food to those most at risk amidst widespread food insecurity. Interventions to tackle poverty and keep young people in school will not be successful without a high level of governmental support. [12] The challenge now is how to rebalance these social and economic inequalities, particularly among young rural women. Structural interventions that include cash transfers, vocational skills training and microfinance interventions are increasingly being considered as important components of the HIV prevention armoury but further exploration in a range of contexts is required, and the reality is that no single or simple intervention will be sufficient. [8, 18, 33, 82, 88–91]
In summary, this study provides further evidence that young poor rural women in Zimbabwe, particularly those who do not have access to sufficient food and those with lower educational attainment, were at increased risk of HIV infection in 2007 and are likely to remain so given that many of these risk factors continue to be prevalent within the country. It is evident that poverty is associated with many factors that drive and influence HIV risk behaviours. However, the notion that ‘HIV is a disease caused by poverty’ is, as others have concluded, too simplistic. [7, 11, 13] These data suggest that targeted structural interventions that tackle social and economic constraints are likely to be a critical component of combination HIV prevention programming and policy.
Data Availability
The data have been made fully available and published for public access on Figshare along with papers that describe the methods for the trial and the final results and the final survey questionnaire (accession numbers http://dx.doi.org/10.6084/m9.figshare.1241574; http://dx.doi.org/10.6084/m9.figshare.1243193; http://dx.doi.org/10.6084/m9.figshare.1243192; http://dx.doi.org/10.6084/m9.figshare.1241575).
Funding Statement
This study was funded through the National Institute of Mental Health (RO1 MH66570). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Gregson S, Garnett GP, Nyamukapa CA, Hallett TB, Lewis JJ, et al. (2006) HIV decline associated with behavior change in eastern Zimbabwe. Science 311: 664–666. 10.1126/science.1121054 [DOI] [PubMed] [Google Scholar]
- 2. Hallett TB, Aberle-Grasse J, Bello G, Boulos LM, Cayemittes MP, et al. (2006) Declines in HIV prevalence can be associated with changing sexual behaviour in Uganda, urban Kenya, Zimbabwe, and urban Haiti. Sex Transm Infect 82 Suppl 1: i1–8. 10.1136/sti.2005.016014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lopman B, Lewis J, Nyamukapa C, Mushati P, Chandiwana S, et al. (2007) HIV incidence and poverty in Manicaland, Zimbabwe: is HIV becoming a disease of the poor? AIDS 21 Suppl 7: S57–66. 10.1097/01.aids.0000300536.82354.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mahomva A, Greby S, Dube S, Mugurungi O, Hargrove J, et al. (2006) HIV prevalence and trends from data in Zimbabwe, 1997–2004. Sex Transm Infect 82 Suppl 1: i42–47. 10.1136/sti.2005.019174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UNAIDS (2007) AIDS epidemic update: December 2007. Available: http://data.unaids.org/pub/EPISlides/2007/2007_epiupdate_en.pdf
- 6. Zimbabwe National Statistics Agency (ZIMSTAT) and ICF International. (2012) Zimbabwe Demographic and Health Survey 2010–11. Calverton, Maryland: Available: http://dhsprogram.com/pubs/pdf/FR254/FR254.pdf. [Google Scholar]
- 7. Gillespie S, Kadiyala S, Greener R (2007) Is poverty or wealth driving HIV transmission? AIDS 21 Suppl 7: S5–S16. 10.1097/01.aids.0000300531.74730.72 [DOI] [PubMed] [Google Scholar]
- 8. Barnett T, Weston M (2008) Wealth, health, HIV and the economics of hope. AIDS 22 Suppl 2: S27–34. 10.1097/01.aids.0000327434.28538.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Krishnan S, Dunbar MS, Minnis AM, Medlin CA, Gerdts CE, et al. (2008) Poverty, gender inequities, and women’s risk of human immunodeficiency virus/AIDS. Ann N Y Acad Sci 1136: 101–110. 10.1196/annals.1425.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mishra V, Assche SBV, Greener R, Vaessen M, Hong R, et al. (2007) HIV infection does not disproportionately affect the poorer in sub-Saharan Africa. AIDS 21 Suppl 7: S17–S28. 10.1097/01.aids.0000300532.51860.2a [DOI] [PubMed] [Google Scholar]
- 11. Piot P, Greener R, Russell S (2007) Squaring the circle: AIDS, poverty, and human development. PLOS Med 4: 1571–1575. 10.1371/journal.pmed.0040314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rollins N (2007) Food insecurity—a risk factor for HIV infection. PLOS Med 4: 1576–1577. 10.1371/journal.pmed.0040301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shelton JD, Cassell MM, Adetunji J (2005) Is poverty or wealth at the root of HIV? Lancet 366: 1057–1058. 10.1016/S0140-6736(05)67401-6 [DOI] [PubMed] [Google Scholar]
- 14. Wojcicki JM (2005) Socioeconomic status as a risk factor for HIV infection in women in East, Central and Southern Africa: a systematic review. J Biosoc Sci 37: 1–36. 10.1017/S0021932004006534 [DOI] [PubMed] [Google Scholar]
- 15. Gillespie S, Greener R, Whiteside A, Whitworth J (2007) Investigating the empirical evidence for understanding vulnerability and the associations between poverty, HIV infection and AIDS impact. AIDS 21 Suppl 7: S1–4. 10.1097/01.aids.0000300530.67107.45 [DOI] [PubMed] [Google Scholar]
- 16. O’Farrell N (2001) Poverty and HIV in sub-Saharan Africa. Lancet 357: 636–637. 10.1016/S0140-6736(05)71428-8 [DOI] [PubMed] [Google Scholar]
- 17. Tsai AC, Bangsberg DR, Weiser SD (2013) Harnessing poverty alleviation to reduce the stigma of HIV in sub-Saharan Africa. PLOS Med 10: e1001557 10.1371/journal.pmed.1001557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, et al. (2011) Conceptual framework for understanding the bidirectional links between food insecurity and HIV AIDS. Am J Clin Nutr 94: 1729S–1739S]. 10.3945/ajcn.111.012070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dinkelman T, Lam D, Leibbrandt M (2007) Household and community income, economic shocks and risky sexual behavior of young adults: evidence from the Cape Area Panel Study 2002 and 2005. AIDS 21 Suppl 7: S49–56. 10.1097/01.aids.0000300535.05226.a9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fenton L (2004) Preventing HIV/AIDS through poverty reduction: the only sustainable solution? Lancet 364: 1186–1187. 10.1016/S0140-6736(04)17109-2 [DOI] [PubMed] [Google Scholar]
- 21. Mishra V, Bignami S, Greener R, Vaessen M, Hong R, et al. (2007) DHS Working Papers: A study of the association of HIV infection with wealth in sub-Saharan Africa. 2007 No. 31 Available: http://dhsprogram.com/pubs/pdf/WP31/WP31.pdf. [Google Scholar]
- 22.UNAIDS (2008) Report on the global AIDS epidemic 2008. Available: http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/dataimport/pub/globalreport/2008/jc1510_2008globalreport_en.pdf
- 23.UNDP (2007) Human Development Report 2007/2008. Fighting climate change: Human solidarity in a divided world. Available: http://hdr.undp.org/sites/default/files/reports/268/hdr_20072008_en_complete.pdf
- 24. Wilson D, Halperin DT (2008) “Know your epidemic, know your response”: a useful approach, if we get it right. Lancet 372: 423–426. 10.1016/S0140-6736(08)60883-1 [DOI] [PubMed] [Google Scholar]
- 25. Dodoo FN, Zulu EM, Ezeh AC (2007) Urban-rural differences in the socioeconomic deprivation--sexual behavior link in Kenya. Soc Sci Med 64: 1019–1031. 10.1016/j.socscimed.2006.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johnson K, Way A (2006) Risk factors for HIV infection in a national adult population: evidence from the 2003 Kenya Demographic and Health Survey. J Acquir Immune Defic Syndr 42: 627–636. 10.1097/01.qai.0000225870.87456.ae [DOI] [PubMed] [Google Scholar]
- 27. Hargreaves JR, Bonell CP, Boler T, Boccia D, Birdthistle I, et al. (2008) Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS 22: 403–414. 10.1097/QAD.0b013e3282f2aac3 [DOI] [PubMed] [Google Scholar]
- 28. Hargreaves JR, Glynn JR (2002) Educational attainment and HIV-1 infection in developing countries: a systematic review. Trop Med Int Health 7: 489–498. 10.1046/j.1365-3156.2002.00889.x [DOI] [PubMed] [Google Scholar]
- 29.Cohen D. (1998) Poverty and HIV/AIDS in sub-Saharan Africa. pp. 1–12.
- 30. Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, et al. (2007) Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLOS Medicine 4: 1589–1597. 10.1371/journal.pmed.0040260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miller CL, Bangsberg DR, Tuller DM, Senkungu J, Kawuma A, et al. (2010) Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS and Behavior 15: 1512–1519. 10.1007/s10461-010-9693-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pettifor AE, Levandowski BA, MacPhail C, Padian NS, Cohen MS, et al. (2008) Keep them in school: the importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol 37: 1266–1273. 10.1093/ije/dyn131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kim J, Pronyk P, Barnett T, Watts C (2008) Exploring the role of economic empowerment in HIV prevention. AIDS 22 Suppl 4: S57–71. 10.1097/01.aids.0000341777.78876.40 [DOI] [PubMed] [Google Scholar]
- 34. Brook DW, Morojele NK, Zhang C, Brook JS (2006) South African adolescents: pathways to risky sexual behavior. AIDS Educ Prev 18: 259–272. 10.1521/aeap.2006.18.3.259 [DOI] [PubMed] [Google Scholar]
- 35. Kaufman CE, Clark S, Manzini N, May J (2004) Communities, opportunities, and adolescents’ sexual behavior in KwaZulu-Natal, South Africa. Stud Fam Plann 35: 261–274. 10.1111/j.0039-3665.2004.00030.x [DOI] [PubMed] [Google Scholar]
- 36.Zimbabwe National Statistics Agency (ZIMSTAT) (2012) Zimbabwe Population Census 2012: National Report. Available: http://www.zimstat.co.zw/dmdocuments/Census/CensusResults2012/National_Report.pdf
- 37.UNDP (2013) Human Development Report 2013 The Rise of the South: Human Progress in a Diverse World. http://hdr.undp.org/sites/default/files/reports/14/hdr2013_en_complete.pdf
- 38. Cowan FM, Pascoe SJ, Langhaug LF, Dirawo J, Chidiya S, et al. (2008) The Regai Dzive Shiri Project: a cluster randomised controlled trial to determine the effectiveness of a multi-component community-based HIV prevention intervention for rural youth in Zimbabwe—study design and baseline results. Trop Med Int Health 13: 1235–1244. 10.1111/j.1365-3156.2008.02137.x [DOI] [PubMed] [Google Scholar]
- 39. Cowan F, Pascoe SJS, LF L, Mavhu W, Chidiya S, et al. (2010) The Regai Dzive Shiri Project: results of a randomised trial of an HIV prevention intervention for Zimbabwean youth. AIDS 24: 2541–2542. 10.1097/QAD.0b013e32833e77c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Food and Agricultural Organization of the United Nations (FAO)/World Food Programme (WFP) (2009) FAO/WFP crop and food security assessment mission to Zimbabwe. Special Report. 22 June 2009. Available: http://documents.wfp.org/stellent/groups/public/documents/ena/wfp204531.pdf
- 41. Auvert B, Buve A, Ferry B, Carael M, Morison L, et al. (2001) Ecological and individual level analysis of risk factors for HIV infection in four urban populations in sub-Saharan Africa with different levels of HIV infection. AIDS 15 Suppl 4: S15–30. 10.1097/00002030-200108004-00003 [DOI] [PubMed] [Google Scholar]
- 42. Auvert B, Buve A, Lagarde E, Kahindo M, Chege J, et al. (2001) Male circumcision and HIV infection in four cities in sub-Saharan Africa. AIDS 15: S31–S40. 10.1097/00002030-200108004-00004 [DOI] [PubMed] [Google Scholar]
- 43. Booysen Fle R, Summerton J (2002) Poverty, risky sexual behaviour, and vulnerability to HIV infection: evidence from South Africa. J Health Popul Nutr 20: 285–288. [PubMed] [Google Scholar]
- 44. Coffee MP, Garnett GP, Mlilo M, Voeten HA, Chandiwana S, et al. (2005) Patterns of movement and risk of HIV infection in rural Zimbabwe. J Infect Dis 191 Suppl 1: S159–167. 10.1086/425270 [DOI] [PubMed] [Google Scholar]
- 45. Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, et al. (2004) Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med 59: 1581–1592. 10.1016/j.socscimed.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 46. Freeman EE, Glynn JR (2004) Factors affecting HIV concordancy in married couples in four African cities. AIDS 18: 1715–1721. 10.1097/01.aids.0000139075.13906.2f [DOI] [PubMed] [Google Scholar]
- 47. Glynn JR, Carael M, Auvert B, Kahindo M, Chege J, et al. (2001) Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS 15 Suppl 4: S51–60. 10.1097/00002030-200108004-00006 [DOI] [PubMed] [Google Scholar]
- 48. Gregson S, Mason PR, Garnett GP, Zhuwau T, Nyamukapa CA, et al. (2001) A rural HIV epidemic in Zimbabwe? Findings from a population-based survey. Int J STD AIDS 12: 189–196. 10.1258/0956462011917009 [DOI] [PubMed] [Google Scholar]
- 49. Gregson S, Nyamukapa CA, Garnett GP, Mason PR, Zhuwau T, et al. (2002) Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. Lancet 359: 1896–1903. 10.1016/S0140-6736(02)08780-9 [DOI] [PubMed] [Google Scholar]
- 50. Morison L, Weiss HA, Buve A, Carael M, Abega SC, et al. (2001) Commercial sex and the spread of HIV in four cities in sub-Saharan Africa. AIDS 15 Suppl 4: S61–69. 10.1097/00002030-200108004-00007 [DOI] [PubMed] [Google Scholar]
- 51. Nunn AJ, Wagner HU, Kamali A, Kengeya-Kayondo JF, Mulder DW (1995) Migration and HIV-1 seroprevalence in a rural Ugandan population. AIDS 9: 503–506. 10.1097/00002030-199505000-00013 [DOI] [PubMed] [Google Scholar]
- 52. Patel V, Kleinman A (2003) Poverty and common mental disorders in developing countries. Bull World Health Organ 81: 609–615. [PMC free article] [PubMed] [Google Scholar]
- 53. Todd J, Changalucha J, Ross DA, Mosha F, Obasi AIN, et al. (2004) The sexual health of pupils in years 4 to 6 of primary schools in rural Tanzania. Sex Transm Infect 80: 35–42. 10.1136/sti.2003.005413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, et al. (2004) Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet 363: 1415–1421. 10.1016/S0140-6736(04)16098-4 [DOI] [PubMed] [Google Scholar]
- 55. Jewkes RK, Levin JB, Penn-Kekana LA (2003) Gender inequalities, intimate partner violence and HIV preventive practices: findings of a South African cross-sectional study. Soc Sci Med 56: 125–134. 10.1016/S0277-9536(02)00012-6 [DOI] [PubMed] [Google Scholar]
- 56. Patel V, Simunyu E, Gwanzura F, Lewis G, Mann A (1997) The Shona Symptom Questionnaire: the development of an indigenous measure of common mental disorders in Harare. Acta Psychiatr Scand 95: 469–475. 10.1111/j.1600-0447.1997.tb10134.x [DOI] [PubMed] [Google Scholar]
- 57. United Nations Children’s Fund (UNICEF) (2005) Guide to monitoring and evaluation of the national response for children orphaned and made vulnerable by HIV/AIDS. New York: https://www.globalhivmeinfo.org/DigitalLibrary/Digital%20Library/OVC_ME_Guide.pdf. [Google Scholar]
- 58. Pascoe SJS, Hargreaves JR, Langhaug LF, Hayes RJ, Cowan FM (2013) ‘How Poor Are You?’—A Comparison of Four Questionnaire Delivery Modes for Assessing Socio-Economic Position in Rural Zimbabwe. PLOS ONE 8: e74977 10.1371/journal.pone.0074977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Central Statistical Office (CSO) [Zimbabwe] and Macro International Inc. (2007) Zimbabwe Demographic and Health Survey 2005–06. Calverton, Maryland: CSO and Macro International Inc. Available: http://dhsprogram.com/pubs/pdf/FR186/FR186.pdf
- 60. UNICEF (2003) The State of the World’s Children 2004: Girls, education and development. New York: Available: http://www.unicef.org/sowc04/files/SOWC_O4_eng.pdf. [Google Scholar]
- 61.US Department of Health and Human Services, Public Health Services and Centers for Disease Control and Prevention (2000) Serologic assays for human immunodeficiency virus antibody in dried blood specimens collected on filter paper.
- 62. Ashley Morrow R, Krantz E, Friedrich D, Wald A (2006) Clinical correlates of index values in the focus HerpeSelect ELISA for antibodies to herpes simplex virus type 2 (HSV-2). J Clin Virol 36: 141–145. 10.1016/j.jcv.2006.02.006 [DOI] [PubMed] [Google Scholar]
- 63.Auerbach JD, Hayes R, Kandathil SM (2006) Overview of effective and promising interventions to prevent HIV infection. UNAIDS Interagency Task Team on Young People Preventing HIV/AIDS in young people: a systematic review of the evidence from developing countries pp. 42–78.
- 64. Gregson S, Todd J, Zaba B (2009) Sexual behaviour change in countries with generalised HIV epidemics? Evidence from population-based cohort studies in sub-Saharan Africa. Sex Transm Infect 85 Suppl 1: i1–2. 10.1136/sti.2009.036053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cowan F, Pascoe S, Langhaug LF, Jaffar S, Hayes R (2005) Baseline data from the Regai Dzive Shiri Project: a community randomised trial of an adolescent reproductive health trial in rural Zimbabwe. 16th International Society for Sexually Transmitted Diseases Research (ISSTDR). Amsterdam, The Netherlands: 10–13 July, 2005. [Google Scholar]
- 66. Hewett PC, Mensch BS, Erulkar AS (2004) Consistency in the reporting of sexual behaviour by adolescent girls in Kenya: a comparison of interviewing methods. Sex Transm Infect 80 (Suppl 2): 43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mensch BS, Hewett PC, Erulkar AS (2003) The reporting of sensitive behavior by adolescents: a methodological experiment in Kenya. Demography 40: 247–268. 10.1353/dem.2003.0017 [DOI] [PubMed] [Google Scholar]
- 68. Ministry of Health and Child Welfare (Zimbabwe), Zimbabwe National Family Planning Council, National AIDS Council (Zimbabwe), US Centers for Disease Control and Prevention (2004) The Zimbabwe Young Adult Survey (YAS) 2001–2002. Harare, Zimbabwe: Ministry of Health and Child Welfare and U.S. Centres for Disease Control and Prevention. [Google Scholar]
- 69. Plummer ML, Ross DA, Wight D, Changalucha J, Mshana G, et al. (2004) “A bit more truthful”: the validity of adolescent sexual behaviour data collected in rural northern Tanzania using five methods. Sex Transm Infect 80 (Suppl 2): 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Internal Displacement Monitoring Centre (2008) The many faces of displacement: IDPs in Zimbabwe. [Google Scholar]
- 71. McCoy S, Ricculli ML, Buzdugan R, Mushavi A, Mahomva A, et al. (2013) Food insecurity is a barrier to service uptake in the PMTCT cascade in Zimbabwe. 7th IAS Conference on HIV Pathogenesis, Treatment, and Prevention. Kuala Lumpur, Malaysia: June 30-July 3, 2013(Session MOAD02). [Google Scholar]
- 72.World Food Programme (2013) Hunger Looms as Zimbabwe faces highest levels of food insecurity in years. Available: https://www.wfp.org/news/news-release/hunger-looms-zimbabwe-faces-highest-levels-food-insecurity-years. Accessed 2014 Oct 16.
- 73. Madise N, Zulu EM, Ciera J (2007) Is poverty a driver for risky sexual behaviour? Evidence from national surveys of adolescents in four African countries. African Journal of Reproductive Health 11: 83–98. 10.2307/25549733 [DOI] [PubMed] [Google Scholar]
- 74. Bachmann MO, Booysen FL (2006) Economic causes and effects of AIDS in South African households. AIDS 20: 1861–1867. 10.1097/01.aids.0000244205.03382.84 [DOI] [PubMed] [Google Scholar]
- 75. Barnighausen T, Hosegood V, Timaeus IM, Newell ML (2007) The socioeconomic determinants of HIV incidence: evidence from a longitudinal, population-based study in rural South Africa. AIDS 21 Suppl 7: S29–38. 10.1097/01.aids.0000300533.59483.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. de Walque D, Nakiyingi-Miiro JS, Busingye J, Whitworth JA (2005) Changing association between schooling levels and HIV-1 infection over 11 years in a rural population cohort in south-west Uganda. Trop Med Int Health 10: 993–1001. 10.1111/j.1365-3156.2005.01475.x [DOI] [PubMed] [Google Scholar]
- 77. Glynn JR, Carael M, Buve A, Anagonou S, Zekeng L, et al. (2004) Does increased general schooling protect against HIV infection? A study in four African cities. Trop Med Int Health 9: 4–14. 10.1046/j.1365-3156.2003.01168.x [DOI] [PubMed] [Google Scholar]
- 78. Hargreaves JR, Morison LA, Kim JC, Bonell CP, Porter JD, et al. (2008) The association between school attendance, HIV infection and sexual behaviour among young people in rural South Africa. J Epidemiol Community Health 62: 113–119. 10.1136/jech.2006.053827 [DOI] [PubMed] [Google Scholar]
- 79. Gillespie S (2006) AIDS, poverty and hunger: challenges and responses. Washington DC: International Food Policy Research Institute. [Google Scholar]
- 80. Bryceson DF, Fonseca J (2006) An enduring or dying peasantry? Interactive impact of famine and HIV/AIDS in rural Malawi. In: Gillespie S, editor. AIDS, Poverty, and Hunger: Challenges and Responses. Washington, D.C.: International Food Policy Research Institute; pp. 97–108. [Google Scholar]
- 81. Baird SG, Garfein RS; MacIntosh CT; Ozler B. (2012) Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet 379: 1320–1329. 10.1016/S0140-6736(11)61709-1 [DOI] [PubMed] [Google Scholar]
- 82. Tsai AC, Hung KJ, Weiser SD (2012) Is food insecurity associated with HIV risk? Cross-sectional evidence from sexually active women in Brazil. PLOS Med 9 e1001203 10.1371/journal.pmed.1001203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. The World Bank (2007) HIV/AIDS, nutrition and food security: what we can do. A synthesis of international guidance. Washington DC. [Google Scholar]
- 84.UNAIDS (2008) HIV, food security, and nutrition. Policy Brief Expanded version May 2008. Available: http://www.unaids.org/en/media/unaids/contentassets/dataimport/pub/manual/2008/jc1565_policy_brief_nutrition_long_en.pdf
- 85. Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, et al. (2012) Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS 26: 67–75. 10.1097/QAD.0b013e32834cad37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shelton JD (2007) Ten myths and one truth about generalised HIV epidemics. Lancet 370: 1809–1811. 10.1016/S0140-6736(07)61755-3 [DOI] [PubMed] [Google Scholar]
- 87.UNAIDS (2005) Evidence for HIV decline in Zimbabwe: a comprehensive review of the epidemiological data. Available: http://data.unaids.org/Publications/IRC-pub06/zimbabwe_epi_report_nov05_en.pdf
- 88. Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, et al. (2006) Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet 368: 1973–1983. 10.1016/S0140-6736(06)69744-4 [DOI] [PubMed] [Google Scholar]
- 89. Kim JC, Watts CH, Hargreaves JR, Ndhlovu LX, Phetla G, et al. (2007) Understanding the impact of a microfinance-based intervention on women’s empowerment and the reduction of intimate partner violence in South Africa. Am J Public Health 97: 1794–1802. 10.2105/AJPH.2006.095521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Pronyk PM, Kim JC, Abramsky T, Phetla G, Hargreaves JR, et al. (2008) A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS 22: 1659–1665. 10.1097/QAD.0b013e328307a040 [DOI] [PubMed] [Google Scholar]
- 91.International Planned Parenthood Foundation (IPPF), United Nations Population Fund (UNFPA), and Young Positives (2007) Change, choice and power: Young women, livelihoods and HIV prevention. Literature review and case study analysis. Available: http://www.unfpa.org/sites/default/files/resource-pdf/change.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data have been made fully available and published for public access on Figshare along with papers that describe the methods for the trial and the final results and the final survey questionnaire (accession numbers http://dx.doi.org/10.6084/m9.figshare.1241574; http://dx.doi.org/10.6084/m9.figshare.1243193; http://dx.doi.org/10.6084/m9.figshare.1243192; http://dx.doi.org/10.6084/m9.figshare.1241575).