Abstract
Background
Despite the recognized health benefits, few older women participate in strength-training exercises.
Methods
The purpose of this study was to examine factors related to older women’s adherence to strength training after participation in the StrongWomen Program, a nationally disseminated community program. Adherence was defined as ≥4 months of twice-weekly strength training. Surveys were sent to 970 program participants from 23 states and to participants’ corresponding program leaders. Five-hundred fifty-seven participants responded (57%).
Results
Of respondents who completed surveys (527), 79% (415) adhered to strength training; adherers reported a mean of 14.1 ± 9.1 months of strength training. Logistic-regression analysis revealed that exercise adherence was positively associated with age (p = .001), higher lifetime physical activity levels (p = .045), better perceived health (p = .003), leader’s sports participation (p = .028), and leader’s prior experience leading programs (p = .006).
Conclusion
These data lend insight to factors that may be related to exercise adherence among midlife and older women.
Keywords: community program, aging, physical activity
Physical inactivity and poor nutrition are leading contributors to chronic disease and premature death (Cress & Buchner, 2005; Gerberding, 2006; Morgan, 2003). Laboratory and home-based studies have demonstrated that strength training—also referred to as resistance training or weight lifting—confers numerous health benefits, particularly for women as they age (Baker et al., 2001; Cussler et al., 2003; Nelson et al., 1994; Nichols, Nelson, Peterson, & Sartoris, 1995). Functionally, strength training is an activity in which muscles move dynamically against weight (or other resistance) with small but consistent increases in the amount of weight being lifted over time. Done regularly, these exercises improve glucose control and body composition, build bone and muscle, and help preserve strength, independence, and vitality with age (Baker et al., 2001; Beniamini, Rubenstein, Faigenbaum, Lichtenstein, & Crim, 1999; Conroy & Earle, 1994; Cussler et al., 2003; Fiatarone et al., 1990; Lemmer et al., 2001; Menkes et al., 1993; Nelson et al., 1994; Sims, Hill, Davidson, Gunn, & Huang, 2006; Tracy et al., 1999).
As a result of the established body of research related to physical activity and older adults, there has been an ongoing movement to raise awareness and provide detailed recommendations that encourage participation from local, state, and national government and organizations (American College of Sports Medicine, 1998; Nelson et al., 2007; U.S. Department of Health and Human Services [USDHHS], 2008). Most recently, the USDHHS’s 2008 Physical Activity Guidelines for Americans recommended that “at least 2 days a week, older adults should do muscle-strengthening activities that involve all the major muscle groups” (USDHHS, 2008).
Despite compelling scientific research and widespread public health recommendations, among women 45–64 years and 65–74 years old, only 18% and 11%, respectively, perform physical activities that enhance and maintain muscle strength and endurance two or more times per week (Kruger, Carlson, & Buchner, 2007). Two critical areas of focus to address this need are developing effective strategies for increasing access to and participation in strength-building activities by older adults and understanding the individual, social, community, and demographic factors that might potentially be acted on to enhance adherence to this health-promoting behavior long term (Boyette, Sharon, & Brandon, 1997; Chiang, Seman, Belza, & Tsai, 2008; McAuley, Courneya, Rudolph, & Lox, 1994; Nelson et al., 2007).
Although personal involvement and commitment to any exercise program are essential, studies indicate that initiating individual behavior change is more likely with social or environmental change and support (Boyette et al., 1997; Dollahite, Hosig, Adeletti White, Rodibaugh, & Holmes, 1998; Elder et al., 2007; Kawachi, 1999; Leung, Yen, & Minkler, 2004; McNeill, Wyrwich, Brownson, Clark, & Kreuter, 2006; Sallis et al., 2006). The EnhanceFitness (EF) program is one example of an evidence-based group exercise class for older adults. It has been implemented at 277 community sites as of 2008 (Project Enhance and Senior Services, 2008). Scientists who developed the EF program and who conduct ongoing research with EF program participants have found that social support from both peers and leaders (interpersonal level) and past physical activity experiences (individual level) were important factors related to exercise adherence among a group of ethnically diverse older adults (mean age 76 years; Belza et al., 2006; Chiang et al., 2008). Thus, the structure of community-based programs to address these factors combined with their increased affordability and accessibility may provide more feasible opportunities for supporting long-term behavior change than other common options (e.g., fitness-center membership; Boyette et al., 1997; Centers for Disease Control and Prevention, 1997, 1999, 2005, 2006; Dollahite et al., 1998; Findorff, Hatch Stock, Gross, & Wyman, 2007; Kawachi, 1999; Kowal & Fortier, 2007; Kruger, Carlson, & Kohl, 2007; Leung et al., 2004; McNeill et al., 2006; Seguin et al., 2008; Sims et al., 2006; Wellman, Kamp, Kirk-Sanchez, & Johnson, 2007; Yajima, Takano, Nakamura, & Watanabe, 2001).
Research demonstrates that using multiple levels of influence, including individual, interpersonal, and community elements, encourages and supports long-term adherence to behavior change compared with single-level approaches. In addition, single-level approaches may be unrealistic for promoting population-wide change because of resource constraints and limited long-term motivation, leadership and peer support, and, thus, adherence (Beauchamp, Welch, & Hulley, 2007; Burton, Turrell, & Oldenburg, 2003; Elder et al., 2007; Kowal & Fortier, 2007; Paluck, Allerdings, Kealy, & Dorgan, 2006; Sallis et al., 2006; Wilcox, Castro, King, Housemann, & Brownson, 2000). From a behavioral-theory perspective, community-based health-promotion programs are advantageous because they bring groups of individuals from a common locale together, which enhances the interpersonal component of social support from peers, as well as guidance, motivation, and encouragement from the community leader (Belza et al., 2006; Chiang et al., 2008; Elder et al., 2007; Findorff et al., 2007; Izquierdo-Porrera, Powell, Reiner, & Fontaine, 2002; Leung et al., 2004; McNeill et al., 2006; Sallis et al., 2006; Wellman et al., 2007; Wilcox et al., 2006).
The purpose of this study was to use a detailed survey to explore the relationships between socioeconomic, personal/behavioral, programmatic, leadership, and community-level social and demographic characteristics as they relate to older women’s adherence to strength training after participation in a community-based program.
Methods
Design
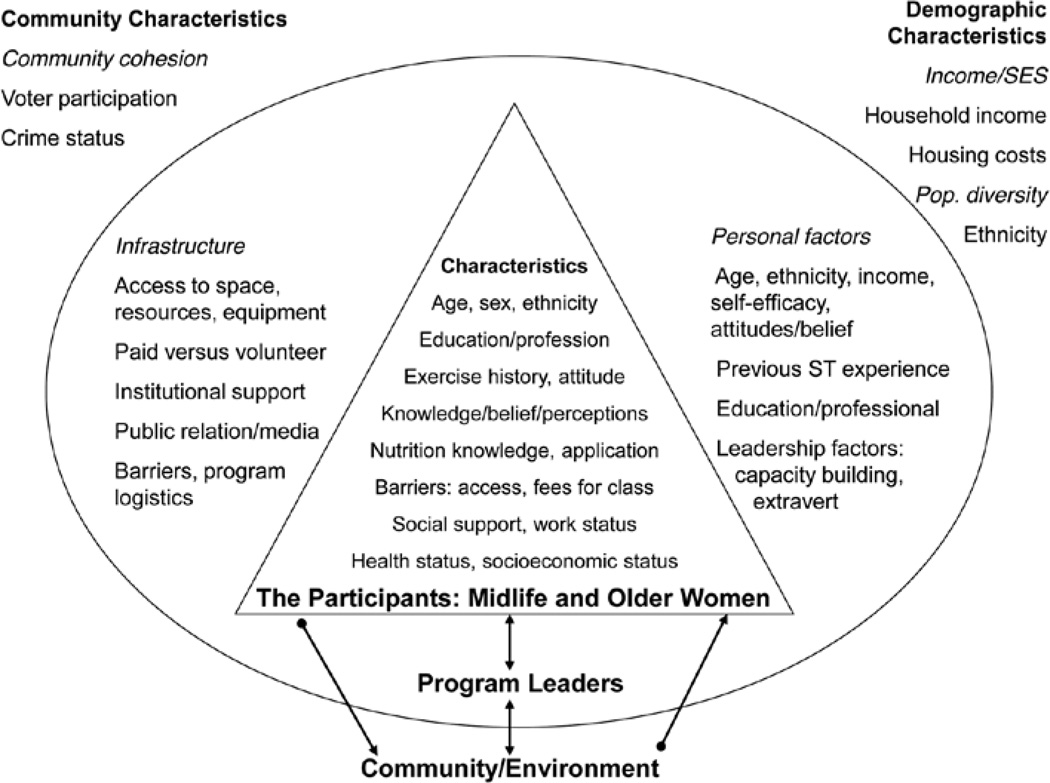
This was a cross-sectional design that used a convenience sample of participants in a nationally disseminated, evidence-informed, community-based strength-training program, the StrongWomen Program (SWP; Seguin et al., 2008). The primary hypothesis for this study stated that adherence (≥4 months of strength training) would be associated with personal factors (income, education, exercise experience, ethnicity, health status, and perceived support) and program characteristics (leader characteristics and behavior modeling). The SWP was developed and disseminated to enable women age 40 or older to maintain their strength, function, and independence. Although the SWP is targeted to and largely attended by women, some program leaders allow men to join the program, as well. Therefore, male participants were included in this research. Program leaders are trained at the StrongWomen Workshop and provided a training manual, The StrongWomen Tool Kit. SWP participants are recruited through local community agencies such as senior centers and county cooperative extension offices, and classes typically meet twice weekly for 12 weeks. An extensive review of the SWP—including the training workshop, curriculum, and programmatic details—has been previously published (Seguin et al., 2008). Figure 1 shows the socioecological framework of variables for this research (Bronfenbrenner, 1979).
Figure 1.
Socioecological framework describing the leader, participant, and community characteristics examined in this study and how they may be related to implementation (leaders) and adherence (participants). The community-level characteristics also help describe the larger contextual landscape of the dissemination environment.
Study Population
To recruit participants, 854 SWP leaders were contacted by e-mail and asked to provide names of current and past program participants. The e-mail was sent to all trained leaders, although it was only applicable to those who had implemented the program. The e-mail explained that our research group was interested in obtaining contact information (full name, complete mailing address, and e-mail address, if available) of at least 20 of their previous and current program participants, preferably an equal split between the two groups. The e-mail provided detailed information about the nature of the survey we would be inviting participants to complete, as well as a protocol for collecting the contact information and an attached spreadsheet for submission of the contact information. All materials for this study (i.e., cover letter/cover e-mail, study information, protocol, survey, etc.) were approved by the Tufts University Human Investigation Review Board (IRB approval #7049).
Survey Design and Development
Survey development involved reviewing and synthesizing findings from program participant interviews and evaluations previously conducted during program site visits (Seguin et al., 2008; Seguin, Hyatt, Kennedy, Irish, & Nelson, 2005). Those data were used to compile a working draft concept and content table, which framed the survey outline. Drafts of the survey were reviewed and pilot tested internally among the research team and selected colleagues, in both an Internet-based and a paper-based format. After modifications, the survey was pilot tested in both formats with 26 program participants from eight states; these individuals were subsequently excluded from final survey participation. Based on pilot feedback, revisions were made to the survey and related materials.
Survey Data Collection
Fifty-seven program leaders provided 970 names and contact information for participants who were then invited to complete the survey beginning in June 2006. All program participants with e-mail addresses received the e-mail invitation, which included a link to the informed consent and survey. Those for whom an e-mail address was not provided, as well as those who responded to the e-mail invitation asking for a printed version, were mailed the paper-based version, which included a written informed consent. After the initial e-mail and paper releases, all nonrespondents received both the e-mail-based and paper-based invitations on two subsequent dates separated by approximately 3 weeks. All respondents were required to sign an informed consent to participate—either using the online consent format or by signing the paper-based survey informed consent. After survey submission, respondents were mailed a thank you letter.
All survey data were collected over a 3-month period. Paper-survey data were entered into SPSS Data Builder 14.0. Internet- survey data were downloaded to a Microsoft Excel spreadsheet, converted to the SPSS 14.0 format, and merged with paper-survey data. All data analysis was conducted using SPSS 14.0 (SPSS, Inc., Chicago, IL).
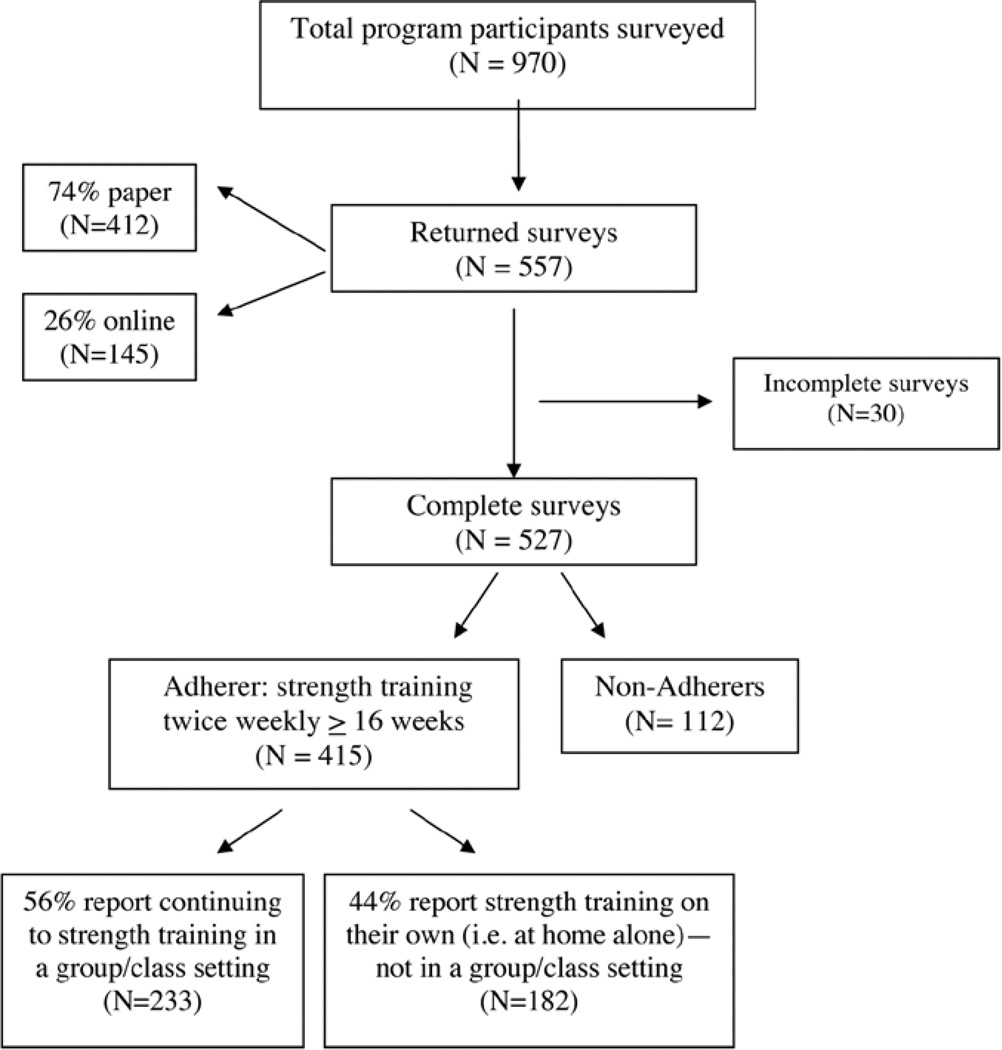
Of the 970 participants surveyed, 557 returned the survey, yielding a 57% response rate. Incomplete surveys (defined as nonresponse to the primary outcome, strength-training adherence) were not included in the analysis (n = 30). Of the 557 submitted surveys, 412 were paper (74%) and 145 were online (26%). Using chi-square to compare categorical variables and t tests to compare continuous variables (i.e., those shown in Tables 1–4 of this manuscript), no statistically significant differences were found between the online and mail respondents. Therefore all data were analyzed and are shown together.
Table 1.
Participants’ Socioeconomic Characteristics
| Nonadherers, n = 112 |
Adherers, n = 415 |
p | |
|---|---|---|---|
| Age, years, M (SD) | 59 (12) | 63 (11) | <.001 |
| Sex, % female | 99 | 98 | .697 |
| Race, % White | 93 | 94 | .663 |
| Household size, % | (.005) | ||
| 1 | 15 | 26 | .013 |
| 2 | 64 | 58 | .263 |
| 3 | 11 | 7 | .120 |
| 4+ | 10 | 9 | .507 |
| Currently married/living with domestic partner, % | 78 | 66 | .010 |
| Education level, % | (.158) | ||
| some high school | 0 | 2 | .355 |
| high school graduate | 24 | 20 | .356 |
| some college | 29 | 32 | .381 |
| college graduate | 47 | 46 | .182 |
| Household income, % | (.600) | ||
| <$20,000 | 7 | 11 | .443 |
| $20,000–49,999 | 36 | 32 | .447 |
| $50,000–74,999 | 26 | 27 | .945 |
| $75,000–100,000 | 20 | 15 | .369 |
| >$100,000 | 11 | 15 | .322 |
| Work status, % | (.025) | ||
| full-time | 32 | 31 | .764 |
| part-time | 24 | 13 | .008 |
| volunteer only | 15 | 25 | .045 |
| no work | 29 | 31 | .550 |
Note. Because of the nature of survey data, sample size varies by question. Sample size range for nonadherers, n = 95–112, and adherers, n = 360–415. The overall p value for each variable is shown in parentheses.
Table 4.
Participant Communities: Individual, Community, and National Demographic Comparisons, M (SD)
| Individual level (all respondents) |
Community level (respondents’ reported ZIP code) |
National level (ZIP code data, 2004 U.S. Census) |
|
|---|---|---|---|
| Education levela | 3.42 (1.09) | 2.71 (0.47) | 2.48 (0.44) |
| Household incomeb | 2.86 (1.20) | 2.39 (0.61) | 2.20 (0.57) |
| Race (% White) | 93.47 (24.70) | 85.9 (12.10) | 75.1 (22.90) |
| Voter participation | — | 61.05 (10.60) | 58.85 (9.88) |
| Violent crimes per 100,000 people | — | 1,060 (693) | 1,070 (837) |
Note. Individual data as reported on survey; community level by reported corresponding ZIP code and national means. All values for each category at all levels are different (p ≤ .01). References: Federal Bureau of Investigation, 2004; Australian Electoral Commission, 2004; U.S. Census Bureau, 2004.
Education scores correspond to the 5 education categories described in the Methods section.
Income scores correspond to the 5 income categories described in the Methods section.
Outcome Measurements
Strength-Training Adherence
The dichotomous variable (adherence) was defined a priori as having completed at least 16 weeks of twice-weekly strength training. To be classified as an adherer, individuals must have answered yes to currently strength training regularly (regardless of specifics, i.e., location/venue, individually or with a group) and reported 4 months or longer of regularly strength training twice weekly.
All survey respondents were asked their frequency of strength training (times per week, with 0 to 7 as the choices) and the duration that strength-training practice had been regularly maintained (e.g., 6 months)—whether as part of a formal program or classes or on their own at home or in a fitness center. Thus, a “yes” response to participation in the SWP or to strength training elsewhere qualified that respondent as an adherer if he or she reported at least 16 weeks of strength training. Adherence was the primary outcome of interest and the dependent variable (0 = no, nonadherer; 1 = yes, adherer) for the logistic-regression analysis.
Socioeconomic Factors
Socioeconomic characteristics included the following: age, sex, race, marital status, educational attainment (e.g., bachelor level), income, and work status. Questions were adapted from the U.S. Census Bureau American Community Survey and the Behavioral Risk Factor Surveillance System Survey Questionnaire (U.S. Census Bureau, 2004; Centers for Disease Control and Prevention, 2006).
Program-Related Personal Factors
The program-related personal characteristics of respondents collected included current and previous activity level and types, previous sports participation, and change in eating habits, nutrition knowledge, and activity level since program participation was initiated. Respondents were asked to classify their health status as one of five choices: excellent, very good, good, fair, or poor. In addition, they were asked to describe the frequency of activity-limiting pain over the previous 4 weeks, adapted from the MOS SF-36, by selecting one of five choices: never/hardly ever, a few times, fairly often, very often, or almost every day/every day (Stewart, Hays, & Ware, 1988). Physical activity and nutrition topic areas were derived from the National Health Interview Survey, and specific questions were developed, pilot tested, and administered for this survey (Centers for Disease Control and Prevention, 2004).
Programmatic and Leadership Variables
Respondents were asked about factors that motivated them to join a group strength-training program, reasons for discontinued participation (if applicable), and a range of questions related to their program logistics, including satisfaction with space, class length, content, social aspects, class attendance, host organization, and leader punctuality. A separate survey was also conducted simultaneously with program leaders, which included questions related to leaders’ activity habits and previous experience leading community programs. Leader data were merged and matched to their corresponding participants’ data for inclusion in the analysis. (Complete findings from the leader survey are in press.)
Demographic Comparisons
To assess socioeconomic status, survey respondents indicated their educational attainment, household income level, and race. To provide additional context and understanding of the community and social environment, these variables were also collected at the respondent ZIP code level. National-level corresponding data from the 2004 U.S. Census were also obtained to identify possible differences between participant communities and the country as a whole (U.S. Census Bureau, 2004). Means were compared for education, income, and race between the individual and community levels, between the individual and national levels, and between the community and national levels. In addition, voter participation rates and crime rates were collected at the community level and national level as indicators for community participation and community cohesion, respectively. Statistical means for the variables were compared with STATA 10 Software (StataCorp, LP, College Station, TX) at the community and national levels (Federal Bureau of Investigation, 2004; Australian Electoral Commission, 2004).
Statistical Analyses
Chi-square was used to compare adherers with nonadherers on categorical variables, and t tests for continuous variables. The a priori hypothesized model to examine factors related to adherence was specified as adherence = age + educational attainment + income + self-reported health status + lifetime physical activity participation + leader’s participation in sports + leader’s previous experience leading programs + race. It is important to note that the construction of alternative models informed by the univariate results occurred during the analyses of these data. The process involved a phased approach testing for collinearity among variables and using stepwise logistic regression. The variables were first tested for collinearity within their respective categories (socioeconomic, program-related personal, programmatic, and leadership). When this occurred, variables were examined using step-wise logistic regression, and variables were chosen based on higher Cox and Snell R2 values. SPSS 14.0 was used to execute this analysis.
Results
Of the 527 respondents who completed the survey, 415 (79%) were classified as adherers and 112 (21%) were classified as nonadherers. See Figure 2.
Figure 2.
Participant survey response.
Socioeconomic Factors
Sex, race, educational attainment, and income were not different between nonadherers and adherers. Nonadherers were significantly younger and more likely to be married or living with a domestic partner than adherers (p < .001 and p = .010, respectively). In addition, household size and part-time and volunteer work status were significantly different between nonadherers and adherers (p = .013, p = .008, and p = .045, respectively). Data are shown in Table 1.
Program-Related Personal Factors
Adherers reported significantly greater current and lifetime physical activity levels (both p < .001) and better overall health status and less frequency of activity-limiting pain (p < .001 and p = .003, respectively). Adherers also reported improved eating habits, nutrition knowledge, and physical activity levels after program participation compared with nonadherers (p = .010, p = .005, and p < .001, respectively). Data are presented in Table 2.
Table 2.
Program-Related Personal Factors
| Nonadherers (%), n = 112 |
Adherers (%), n = 415 |
p | |
|---|---|---|---|
| Current physical activity | (<.001) | ||
| not active | 13 | 3 | <.001 |
| somewhat active | 63 | 39 | <.001 |
| active | 24 | 58 | <.001 |
| Lifetime physical activity | (.002) | ||
| not active | 6 | 5 | .174 |
| somewhat active | 54 | 40 | .003 |
| active | 40 | 55 | <.001 |
| Prior sports participation | 45 | 45 | .878 |
| In general, my health is … | (.002) | ||
| poor | 0 | 0 | 1.000 |
| fair | 8 | 7 | .683 |
| good | 47 | 32 | .005 |
| very good | 40 | 43 | .700 |
| excellent | 5 | 18 | <.001 |
| Pain limited activities during the previous 4 weeks | (.026) | ||
| never/hardly ever | 55 | 57 | .808 |
| a few times | 25 | 32 | .091 |
| fairly often | 10 | 6 | .078 |
| very often | 1 | 2 | 1.000 |
| almost every day/daily | 9 | 3 | .007 |
| My eating habits improved since participation. | 37 | 52 | .010 |
| I feel more knowledgeable about healthy eating. | 49 | 65 | .005 |
| Change in activity level since program participation | (<.001) | ||
| less active | 26 | 1 | <.001 |
| more active | 74 | 99 | <.001 |
Note. Because of the nature of survey data, sample size varies by question. Sample size range for nonadherers, n = 85–112, and adherers, n = 312–415. The overall p value for each variable is shown in parentheses.
Programmatic and Leadership Variables
Respondents answered a variety of questions related to their program participation. A greater percentage of nonadherers reported mental or emotional reasons for joining the program than adherers (p = .048), although a greater percentage of adherers reported social reasons for joining than nonadherers (p = .034). Several reasons reported for stopping strength training in a group setting were different between nonadherers and adherers. Nonadherers were more likely to report boredom, a health condition, and lack of time as reasons (p = .017, p = .001, and p < .001, respectively), and adherers were more likely to report that they prefer to strength train at home as their reason for no longer strength training in a group (p < .001). In terms of leader and class specifics, adherers reported greater satisfaction with class space and higher attendance (p = .001 and p = .047, respectively). Data are shown in Table 3.
Table 3.
Programmatic Variables
| Nonadherers (%), n = 112 |
Adherers (%), n = 415 |
p | |
|---|---|---|---|
| Motivation and Barriers | |||
| Top 3 reasons you joined program | |||
| physical | 93 | 92 | .931 |
| medical | 80 | 82 | .320 |
| mental/emotional | 41 | 31 | .048 |
| social | 21 | 30 | .034 |
| referral | 18 | 21 | .397 |
| Top 3 reasons you stopped strength training in a group (if applicable)a | |||
| lack of time/too busy | 44 | 20 | .001 |
| class no longer offered | 33 | 32 | .949 |
| health condition | 21 | 7 | .001 |
| scheduling conflicts | 20 | 21 | .667 |
| location | 14 | 14 | .927 |
| boredom | 13 | 4 | .017 |
| prefer to do it at home | 8 | 29 | <.001 |
| doctor advised against it | 4 | 1 | <.211 |
| didn’t like strength training | 4 | 0 | .076 |
| Class Specifics | |||
| I was satisfied with the space. | 91 | 98 | .001 |
| Class length was good/right for me. | 97 | 99 | .164 |
| Content was what I expected. | 100 | 98 | .604 |
| Content was what I wanted. | 96 | 97 | .512 |
| Social factors encourage me. | 80 | 78 | .807 |
| I rarely, if ever, skipped class. | 92 | 95 | .047 |
| My class was through extension. | 42 | 50 | .177 |
| Class always began on time. | 97 | 99 | .228 |
Note. Because of the nature of survey data, sample size varies by question. Sample size range for nonadherers, n = 104–112, and adherers, n = 360–415.
Sample size for nonadherers, n = 104, adherers, n = 157.
Adherers reported 14.1 ± 9.1 mean ± SD total months of strength training. Data from the leader survey revealed that compared with nonadherers, adherers’ leaders were more likely to report previous experience leading programs (56% vs. 73%, p < .001) and more likely to report sports participation (12% vs. 22%, p = .02). In addition, among 182 respondent adherers who reported no longer participating in the group setting but continuing to strength train on their own, physical and medical reasons were the top reported reasons for continuing to strength train. Data are not shown.
Demographic Comparison
Individual-, community-, and national-level comparisons for education, income, and race, as well as community- and national-level voter participation and crime rates for participant communities, are shown in Tables 4. At the individual level, respondents had higher levels of education, higher household income, and less racial diversity than their respective communities (all p < .001), and their respective communities had higher levels of education, higher household income, less racial diversity than the national levels (all p < .001). In addition, respondents’ respective communities had higher voter participation rates and lower crime rates than the country overall (both p < .001).
Factors Related to Exercise Adherence: Logistic-Regression Analysis
To examine the impact of these measures on adherence to the strength-training program, a logistic-regression model was estimated. The logistic model presented in Table 5 was specified as adherence = age + educational attainment + self-reported health status + lifetime physical activity participation + leader’s participation in sports + leader’s previous experience leading programs + race. During the construction of alternative models (see Methods) in which collinearity was examined within the respective variable categories (socioeconomic, professional, etc.), education and income were highly correlated and thus could not be included in any regression models together. Using separate step-wise logistic-regression tests, educational attainment remained in the model and income did not. Thus, education was chosen over income for inclusion.
Table 5.
Logistic Regression: Factors Related to Strength-Training Adherence, N = 491
| Odds ratio |
95% CI | p | |
|---|---|---|---|
| Age (years) | 1.036 | 1.014 to 1.058 | .001 |
| Educational attainment | 1.110 | 0.893 to 1.380 | .349 |
| Self-reported health status | 1.545 | 1.162 to 2.054 | .003 |
| Lifetime physical activity participation | 1.494 | 1.010 to 2.209 | .045 |
| Leader’s participation in sports | 2.320 | 1.096 to 4.907 | .028 |
| Leader’s previous experience leading programs | 1.956 | 1.217 to 3.143 | .006 |
| Race | 0.679 | −0.251 to 1.839 | .446 |
| Constant | 0.020 | .000 |
Note. CI = confidence interval. Because of the nature of survey data, sample size varies by question.
As age increased, participants were more likely to adhere to strength training (OR = 1.036, 95% CI = 1.014–1.058). For example, for every added decade of life, participants were approximately 10 times as likely to adhere to strength training. Participants whose leader participated in sports and had previous program leadership experience were approximately twice as likely to adhere to strength training (OR = 2.320, CI = 1.096–4.907, and OR = 1.956, CI = 1.217–3.143, respectively). In addition, participants who reported better health status and higher levels of lifetime physical activity were more likely to adhere to strength training (OR = 1.545, CI = 1.162–2.054, and OR = 1.494, CI = 1.010–2.209). Included in the model but not related to adherence were participant educational attainment and race (p = .359 and p = .446, respectively). The overall model was significant (p < .001) with a −2 log likelihood of 462.8 and a Cox and Snell R2 value of .086, suggesting that this model may explain approximately 8.6% of the variability in adherence status.
Discussion
Findings from this study revealed that participant age, lifetime physical activity level, and perceived overall health were positively associated with adherence. In addition, leaders’ physical activity participation and previous experience leading programs were positively associated with participants’ strength-training adherence. These factors’ relationship with exercise adherence is consistent with previous findings from studies with women and older adults (Boyette et al., 1997; Izquierdo-Porrera et al., 2002; McAuley et al., 1994).
At the individual level, women who adhered to strength training reported higher levels of current and previous exercise participation, as well as better perceived health and less activity-limiting pain, than nonadherers. These factors’ relationship with exercise adherence is consistent with previous findings, especially from studies with women and older adults (Boyette et al., 1997; Izquierdo-Porrera et al., 2002; Kowal & Fortier, 2007; McAuley et al., 1994; Walcott-McQuigg, Zerwic, Dan, & Kelley, 2001). Although this was simply a comparison by groups, these findings, particularly those related to perceived health status and frequency of activity-limiting pain, offer some information about the perceived and real barriers that may need to be addressed to improve adherence. One may also consider how it might be synergistic to combine SWP with a program that addresses these barriers, such as a chronic-disease self-management program (Farrell et al., 2004).
Studies examining behavioral interventions have identified factors associated with catalyzing and sustaining change, such as facilitating an environment that supports and reinforces the behavior. In the SWP, that “environment” encompasses a myriad of factors that may include individual program-relevant knowledge, attitudes, experiences, and beliefs; enhancing interpersonal and community engagement; positive behavior modeling and skill mastery by program leaders; and/or policy changes (Addy et al., 2004; Estabrooks, Lee, & Gyurcsik, 2003; French & Stables, 2003; Hooker, Wilson, Griffin, & Ainsworth, 2005; Kowal & Fortier, 2007; McNeill et al., 2006; Sallis et al., 2003; Sallis et al., 2006). In this study, several of those aspects of environmental support, as well as community characteristics, were incorporated and examined. The socioecological framework of variables considered the potential influence of community leaders’ experiences, characteristics, and skills on participant experience and behavior change (Chelladurai, 1980; Kennerly, 1989; Li-Chun, L, Bi-Ying, Wan-En, & Shu-Feng, 2004). These data, along with prior research, demonstrate that the relationship between participants and leadership in the learning environment—behavior modeling (leader’s physical activity habits) and skill mastery (previous experience leading programs)—were important elements of adherence (Elder et al., 1986; Farquhar et al., 1990; Li-Chun, I-Chuan, Bi-Ying, Wan-En, & Shu-Feng, 2004; McNeill et al., 2006). In addition, the community-level data from this research help provide context and understanding of the demographics and social environment among this population and may inform future research aiming to examine the effects of these factors on community-based behavior-change interventions and dissemination efforts.
Although program participation was a required precursor to survey participation, individuals could be classified as adherers as long they continued to strength train, regardless of venue. As such, the finding that 182 survey respondents were no longer participating in the program and yet continued to strength train regularly is an encouraging finding. What this indicates is that exposure to this health-promoting behavior in the context of a community-based program executed by trained leaders who themselves are physically active was a potent enough exposure to support adherence in this population to the behavior of interest—strength training.
There are notable limitations inherent in the design and sample of this survey. Response and selection bias are perhaps the most considerable. Participant contact information was solicited from leaders. Although we asked leaders to include an even representation of both current and previous participants, that was not possible for those who had either recently started leading a program or who had high retention. In addition, there was an extra step in the process of gaining permission from previous participants to provide their contact information to us, which may have been a barrier to gaining equal representation from both groups. For current participants, leaders asked for permission in class, whereas for previous participants, they had to call and gain permission over the phone. There may have also been bias among leaders, however unconscious, to select “successful” program participants—i.e., those they thought had had a positive program experience. However, this was the only possible approach to acquiring contact information. In addition, because only 58% of those surveyed responded and 79% of those individuals were classified as adherers, it is not possible to determine whether the factors identified here would be the same in the group of nonresponders. It is also important to note that although a great variety of categories of variables was included in these surveys, it is possible that key variables of influence were omitted.
Conclusion
This cross-sectional study used a convenience sample of community-based program participants. Despite the limitations of this design and sample, these data make an important contribution to the literature related to exercise adherence in older women, particularly as relates to the influence of leadership in community-based settings. The national sample is also a notable characteristic of this program and the related findings.
Leadership at the community level was an important component of the SWP implementation strategy, and these data support its relevance in exercise adherence in this population, both in terms of behavior modeling—as demonstrated by the positive association between adherence and leaders’ physical activity habits (sport participation)—and in terms of skill mastery by program leaders—as demonstrated by the positive association between adherence and leaders’ previous experience leading programs (Elder et al., 1986; Farquhar et al., 1990; Li-Chun et al., 2004; McNeill et al., 2006). Strategies that focus on leader recruitment, selection, and targeted training (i.e., skill mastery and behavior modeling) and participant-level factors (i.e., improving participants’ perceived health status or pain limitations) may be considered to guide future research and programmatic approaches.
References
- Addy CL, Wilson DK, Kirkland KA, Ainsworth BE, Sharpe P, Kimsey D. Associations of perceived social and physical environmental supports with physical activity and walking behavior. American Journal of Public Health. 2004;94(3):440–443. doi: 10.2105/ajph.94.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Sports Medicine. ACSM position stand on osteoporosis and exercise. Medicine and Science in Sports and Exercise. 27(4):i–vii. [PubMed] [Google Scholar]
- American College of Sports Medicine. American College of Sports Medicine position stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Medicine and Science in Sports and Exercise. 1998;30(6):975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- Australian Electoral Commission. The official 2004 federal election results. 2004 Retrieved from http://results.aec.gov.au/12246/results/default.htm.
- Baker KR, Nelson ME, Felson DT, Layne JE, Sarno R, Roubenoff R. The efficacy of home based progressive strength training in older adults with knee osteoarthritis: A randomized controlled trial. The Journal of Rheumatology. 2001;28(7):1655–1665. [PubMed] [Google Scholar]
- Beauchamp MR, Welch AS, Hulley AJ. Transformational and transactional leadership and exercise-related self-efficacy: An exploratory study. Journal of Health Psychology. 2007;12(1):83–88. doi: 10.1177/1359105307071742. [DOI] [PubMed] [Google Scholar]
- Belza B, Shumway-Cook A, Phelan E, Williams B, Snyder S, LoGerfo J. The effects of a community-based exercise program on function and health in older adults: The EnhanceFitness Program. Journal of Applied Gerontology. 2006;25(4):291–306. [Google Scholar]
- Beniamini Y, Rubenstein J, Faigenbaum A, Lichtenstein A, Crim M. High-intensity strength training of patients enrolled in an outpatient cardiac rehabilitation program. Journal of Cardiopulmonary Rehabilitation. 1999;19:8–17. doi: 10.1097/00008483-199901000-00001. [DOI] [PubMed] [Google Scholar]
- Boyette LW, Sharon BF, Brandon LJ. Exercise adherence for a strength training program in older adults. The Journal of Nutrition, Health & Aging. 1997;1(2):93–97. [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Burton NW, Turrell G, Oldenburg B. Participation in recreational physical activity: why do socioeconomic groups differ? Health Education & Behavior. 2003;30(2):225–244. doi: 10.1177/1090198102251036. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Unrealized prevention opportunities: Reducing the health and economic burden of chronic disease. Atlanta, GA: U.S. Department of Health and Human Services & Centers for Disease Control and Prevention; 1997. [Google Scholar]
- Centers for Disease Control and Prevention. Promoting physical activity: A guide for community action. Champaign, IL: Human Kinetics; 1999. [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System survey questionnaire. Atlanta, GA: U.S. Department of Health and Human Services & Centers for Disease Control and Prevention; 2004. [Google Scholar]
- Centers for Disease Control and Prevention. Preventing obesity and chronic diseases through good nutrition and physical activity. Atlanta, GA: U.S. Department of Health and Human Services & Centers for Disease Control and Prevention; 2005. [Google Scholar]
- Centers for Disease Control and Prevention. DATA2010–The Healthy People 2010 database. Focus area 22: Physical activity and fitness. Atlanta, GA: U.S. Department of Health and Human Services & Centers for Disease Control and Prevention; 2006. [Google Scholar]
- Chelladurai P. Leadership in sports organizations. Canadian Journal of Applied Sport Sciences. 1980;5(4):226–231. [PubMed] [Google Scholar]
- Chiang KC, Seman L, Belza B, Tsai JH. “It is our exercise family”: Experiences of ethnic older adults in a group-based exercise program. Preventing Chronic Disease. 2008;5(1):A05. [PMC free article] [PubMed] [Google Scholar]
- Conroy BP, Earle RW. Bone, muscle, and connective tissue adaptations to physical activity. In: Baechle TR, editor. Essentials of strength training and conditioning. Champaign, IL: Human Kinetics; 1994. pp. 57–73. [Google Scholar]
- Cress M, Buchner D. Best practices for physical activity programs and behavior counseling in older adult populations. Journal of Aging and Physical Activity. 2005;13(1):61–74. doi: 10.1123/japa.13.1.61. [DOI] [PubMed] [Google Scholar]
- Cussler EC, Lohman TG, Going SB, Houtkooper LB, Metcalfe LL, Flint-Wagner HG, Teixeira PJ. Weight lifted in strength training predicts bone change in postmenopausal women. Medicine and Science in Sports and Exercise. 2003;35(1):10–17. doi: 10.1097/00005768-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Dollahite J, Hosig K, Adeletti White K, Rodibaugh R, Holmes T. Impact of a school-based community intervention program on nutrition knowledge and food choices in elementary school children in the rural Arkansas Delta. Journal of Nutrition Education. 1998;30(5):289–293. [Google Scholar]
- Elder JP, Lytle L, Sallis JF, Young DR, Steckler A, Simons-Morton D, Ribisl K. A description of the social-ecological framework used in the trial of activity for adolescent girls (TAAG) Health Education Research. 2007;22(2):155–165. doi: 10.1093/her/cyl059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, McGraw SA, Abrams DB, Ferreira A, Lasater TM, Longpre H, Carleton RA. Organizational and community approaches to community-wide prevention of heart disease: The first two years of the Pawtucket Heart Health Program. Preventive Medicine. 1986;15(2):107–117. doi: 10.1016/0091-7435(86)90081-2. [DOI] [PubMed] [Google Scholar]
- Estabrooks PA, Lee RE, Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine. 2003;25(2):100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- Farquhar JW, Fortmann SP, Flora JA, Taylor CB, Haskell WL, Williams PT, Wood PD. Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. Journal of the American Medical Association. 1990;264(3):359–365. [PubMed] [Google Scholar]
- Farrell K, Wicks MN, Martin JC. Chronic disease self-management improved with enhanced self-efficacy. Clinical Nursing Research. 2004;13(4):289–308. doi: 10.1177/1054773804267878. [DOI] [PubMed] [Google Scholar]
- Federal Bureau of Investigation. Crime in the United States 2004. 2004 Retrieved from http://www.fbi.gov/ucr/cius_04/documents/CIUS2004.pdf.
- Fiatarone M, Marks E, Ryan N, Meredith C, Lipsitz L, Evans W. High-intensity strength training in nonagenarians. Effects on skeletal muscle. Journal of the American Medical Association. 1990;263(22):3029–3034. [PubMed] [Google Scholar]
- Findorff MJ, Hatch Stock H, Gross CR, Wyman JF. Does the transtheoretical model (TTM) explain exercise behavior in a community-based sample of older women? Journal of Aging and Health. 2007;19(6):985–1003. doi: 10.1177/0898264307308341. [DOI] [PubMed] [Google Scholar]
- French SA, Stables G. Environmental interventions to promote vegetable and fruit consumption among youth in school settings. Preventive Medicine. 2003;37:593–610. doi: 10.1016/j.ypmed.2003.09.007. [DOI] [PubMed] [Google Scholar]
- Gerberding G. Healthy aging: Preventing disease and improving quality of life among older Americans 2006. Atlanta, GA: Coordinating Center for Health Promotion & Centers for Disease Control and Prevention; 2006. [Google Scholar]
- Hooker S, Wilson D, Griffin S, Ainsworth B. Perceptions of environmental supports for physical activity in African American and White adults in a rural county in South Carolina. Preventing Chronic Disease. 2005;2(4):A11. [PMC free article] [PubMed] [Google Scholar]
- Izquierdo-Porrera AM, Powell CC, Reiner J, Fontaine KR. Correlates of exercise adherence in an African American church community. Cultural Diversity & Ethnic Minority Psychology. 2002;8(4):389–394. doi: 10.1037/1099-9809.8.4.390. [DOI] [PubMed] [Google Scholar]
- Kawachi I. Social capital and community effects on population and individual health. Annals of the New York Academy of Sciences. 1999;896:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kennerly SM. Leadership behavior and organizational characteristics: implications for faculty satisfaction. The Journal of Nursing Education. 1989;28(5):198–202. doi: 10.3928/0148-4834-19890501-04. [DOI] [PubMed] [Google Scholar]
- Kowal J, Fortier MS. Physical activity behavior change in middle-aged and older women: The role of barriers and of environmental characteristics. Journal of Behavioral Medicine. 2007;30(3):233–242. doi: 10.1007/s10865-007-9102-y. [DOI] [PubMed] [Google Scholar]
- Kruger J, Carlson SA, Buchner D. How active are older Americans? Preventing Chronic Disease. 2007;4(3):A53. [PMC free article] [PubMed] [Google Scholar]
- Kruger J, Carlson SA, Kohl HW., 3rd Fitness facilities for adults: Differences in perceived access and usage. American Journal of Preventive Medicine. 2007;32(6):500–505. doi: 10.1016/j.amepre.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Lemmer JT, Ivey FM, Ryan AS, Martel GF, Hurlbut DE, Metter JE, Hurley BF. Effect of strength training on resting metabolic rate and physical activity: Age and gender comparisons. Medicine and Science in Sports and Exercise. 2001;33(4):532–541. doi: 10.1097/00005768-200104000-00005. [DOI] [PubMed] [Google Scholar]
- Leung MW, Yen IH, Minkler M. Community based participatory research: A promising approach for increasing epidemiology’s relevance in the 21st century. International Journal of Epidemiology. 2004;33(3):499–506. doi: 10.1093/ije/dyh010. [DOI] [PubMed] [Google Scholar]
- Li-Chun C, I-Chuan L, Bi-Ying H, Wan-En C, Shu-Feng L. A preliminary survey of the health behaviors of community leaders. The Journal of Nursing Research. 2004;12(2):92–102. doi: 10.1097/01.jnr.0000387493.16804.ea. [DOI] [PubMed] [Google Scholar]
- McAuley E, Courneya D, Rudolph D, Lox C. Enhancing exercise adherence in middle-aged males and females. Preventive Medicine. 1994;23:498–506. doi: 10.1006/pmed.1994.1068. [DOI] [PubMed] [Google Scholar]
- McNeill LH, Wyrwich KW, Brownson RC, Clark EM, Kreuter MW. Individual, social environmental, and physical environmental influences on physical activity among Black and White adults: A structural equation analysis. Annals of Behavioral Medicine. 2006;31(1):36–44. doi: 10.1207/s15324796abm3101_7. [DOI] [PubMed] [Google Scholar]
- Menkes A, Mazel S, Redmond R, Koffler K, Libanati C, Gundberg C, Hurley BF. Strength training increases regional bone mineral density and bone remodeling in middle-aged and older men. Journal of Applied Physiology. 1993;74(5):2478–2484. doi: 10.1152/jappl.1993.74.5.2478. [DOI] [PubMed] [Google Scholar]
- Morgan D. Facts and figures about the baby boom. Generations (San Francisco, Calif.) 2003;XXII:10–15. [Google Scholar]
- Nelson ME, Fiatarone M, Morganti C, Trice I, Greenberg R, Evans W. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. Journal of the American Medical Association. 1994;272:1909–1914. doi: 10.1001/jama.1994.03520240037038. [DOI] [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC American Heart Association. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Nichols JF, Nelson KP, Peterson KK, Sartoris DJ. Bone mineral density responses to high-intensity strength training in active older women. Journal of Aging and Physical Activity. 1995;3(36):26–38. [Google Scholar]
- Paluck EC, Allerdings M, Kealy K, Dorgan H. Health promotion needs of women living in rural areas: An exploratory study. Canadian Journal of Rural Medicine. 2006;11(2):111–116. [PubMed] [Google Scholar]
- Project Enhance and Senior Services. Empower: Annual report 2008. Seattle, WA: Author; 2009. [Google Scholar]
- Sallis JF, McKenzie TL, Conway TL, Elder JP, Prochaska JJ, Brown M, Alcaraz JE. Environmental interventions for eating and physical activity: A randomized controlled trial in middle schools. American Journal of Preventive Medicine. 2003;24(3):209–217. doi: 10.1016/s0749-3797(02)00646-3. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annual Review of Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- Seguin R, Economos C, Hyatt R, Palombo R, Reed P, Nelson M. Design and national dissemination of the Strong Women community strength training program. Preventing Chronic Disease. 2008;5(1):A06. Retrieved from http://www.cdc.gov/pcd/issues/2008/jan/2006_0165.htm. [PMC free article] [PubMed] [Google Scholar]
- Seguin R, Hyatt R, Kennedy M, Irish S, Nelson M. The Strongwomen Program: Evaluation of a community-based exercise program and its leaders. Medicine and Science in Sport and Exercise. 2005;37(5 Suppl):S246. [Google Scholar]
- Sims J, Hill K, Davidson S, Gunn J, Huang N. Exploring the feasibility of a community-based strength training program for older people with depressive symptoms and its impact on depressive symptoms. BMC Geriatrics. 2006;6:18. doi: 10.1186/1471-2318-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart A, Hays R, Ware J. The MOS short-form general health survey: Reliability and validity in a patient population. Medical Care. 1988;26(7):724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- Tracy BL, Ivey FM, Hurlbut D, Martel GF, Lemmer JT, Siegel EL, Hurley BF. Muscle quality. II. Effects of strength training in 65- to 75-yr-old men and women. J Appl Physiol. 1999;86(1):195–201. doi: 10.1152/jappl.1999.86.1.195. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. American community survey. Washington, DC: Author; 2004. [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical activity guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008. Retrieved from http://www.health.gov/paguidelines/pdf/paguide.pdf. [Google Scholar]
- Walcott-McQuigg JA, Zerwic JJ, Dan A, Kelley MA. An ecological approach to physical activity in African American women. Medscape Women’s Health. 2001;6(6):3. [PubMed] [Google Scholar]
- Wellman NS, Kamp B, Kirk-Sanchez NJ, Johnson PM. Eat better & move more: A community-based program designed to improve diets and increase physical activity among older Americans. American Journal of Public Health. 2007;97(4):710–717. doi: 10.2105/AJPH.2006.090522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox S, Castro C, King AC, Housemann R, Brownson RC. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. Journal of Epidemiology and Community Health. 2000;54(9):667–672. doi: 10.1136/jech.54.9.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox S, Dowda M, Griffin SF, Rheaume C, Ory MG, Leviton L, Mockenhaupt R. Results of the first year of Active for Life: Translation of 2 evidence-based physical activity programs for older adults into community settings. American Journal of Public Health. 2006;96(7):1201–1209. doi: 10.2105/AJPH.2005.074690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yajima S, Takano T, Nakamura K, Watanabe M. Effectiveness of a community leaders’ programme to promote healthy lifestyles in Tokyo, Japan. Health Promotion International. 2001;16(3):235–243. doi: 10.1093/heapro/16.3.235. [DOI] [PubMed] [Google Scholar]