Abstract
A woman with temporal lobe epilepsy manifesting with repeated episodes of sudden diarrhea and loss of consciousness is reported. A 63-year-old, right-handed female presented with chief complaints of sudden diarrhea and loss of consciousness for almost three decades. The first attack occurred in her 30s, and similar attacks repeated several times in a year. Her attacks comprised abrupt abdominal discomfort, diarrhea, sudden emergence of old memories relating to when she had played with her brother in her childhood, and loss of consciousness during defecation. She had no convulsion or automatism and fully recovered in a few minutes. Every time she was transferred to emergency hospital by ambulance, she had examinations such as blood test, head computed tomography, electrocardiogram, abdominal ultrasound, and electroencephalography (EEG), but no specific diagnosis was made. On admission to our hospital, vital signs, neurological examination, and blood tests did not show abnormal findings. During long-term video-EEG monitoring for 40 h, she had no habitual event. Interictal EEG showed intermittent irregular delta waves and sharp regional transients in the left anterio-midtemporal area. Sharp transients were not as outstanding from background activities as to be defined as epileptiform discharges, but they were reproducible in morphology and distribution and appeared not only in sleep but also in wakefulness. Brain magnetic resonance imaging was unremarkable. Single-photon emission computed tomography showed a decrease of blood flow in the left frontal and temporal lobes. Wechsler Adult Intelligence Scale—III showed a decline of verbal comprehension. We concluded that the patient was suffering from partial epilepsy originating from the left temporal lobe. Carbamazepine markedly improved her seizures. Temporal lobe epilepsy can manifest with diverse autonomic symptoms and signs. Abdominal sensations often herald the onset of epileptic seizures. Among them is an uncommon syndrome called abdominal epilepsy in which gastrointestinal complaints are the primary or the sole manifestation of epileptic seizures. In patients who present with diarrhea and other autonomic symptoms otherwise unexplained, a possible diagnosis of epilepsy should be considered.
Keywords: Recurrent diarrhea, Semiology, Temporal lobe epilepsy
1. Introduction
Abdominal sensations often herald the onset of epileptic seizures. Among them is an uncommon syndrome called abdominal epilepsy in which gastrointestinal complaints are the primary or the sole manifestation of epileptic seizures [1], [2], [3], [4]. Here, we present a case with recurrent diarrhea as a primary manifestation of temporal lobe epilepsy.
2. Case report
A 63-year-old, right-handed woman, who had been suffering from repeated episodes of sudden loss of consciousness for almost three decades, was referred to our epilepsy clinic for further evaluation after experiencing three episodes in the last six months. She had the first episode in her 30s, several days after delivery of twins; she suddenly experienced abdominal discomfort, developed diarrhea, and lost consciousness during defecation. Subsequently, she had similar episodes several times a year, occasionally along with palpitations. On arrival at the hospital emergency department after every episode, examinations including blood tests, head CT, conventional and Holter electrocardiogram, abdominal ultrasound, and electroencephalogram (EEG) were performed, but no specific diagnosis was made.
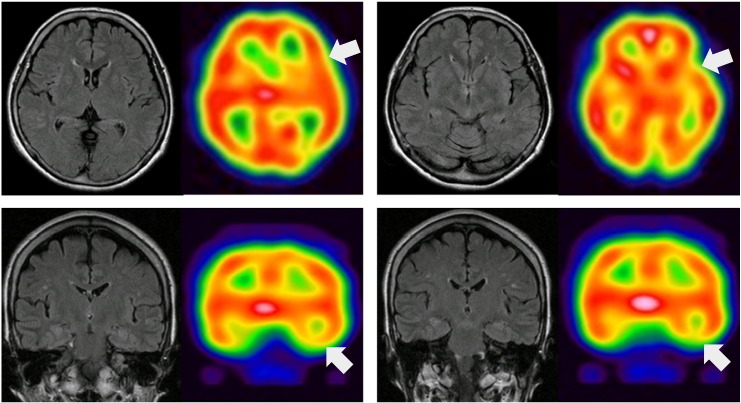
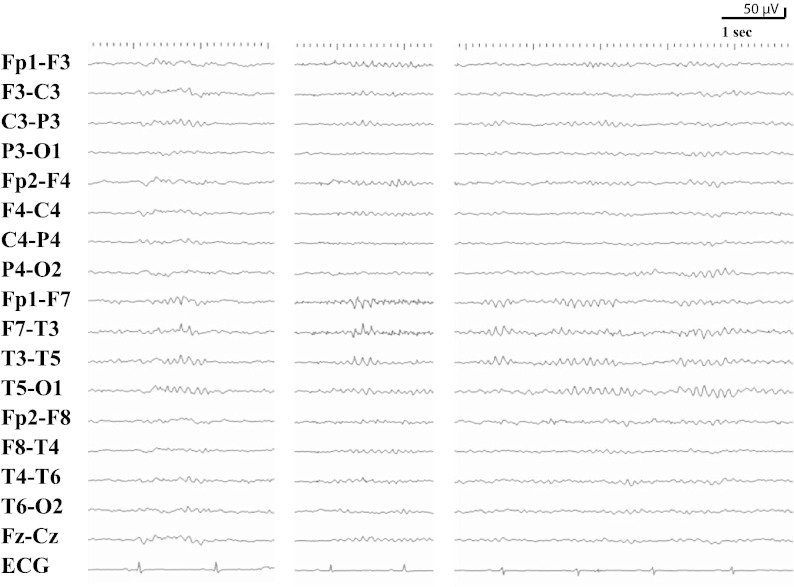
A thorough neurological examination did not show abnormal findings. Complete blood cell count, electrolytes, and liver and renal function were within normal limits. Brain magnetic resonance imaging was unremarkable; however, interictal brain SPECT (123I) showed a decrease of blood flow in the left frontal and temporal lobes (Fig. 1). During long-term video-EEG monitoring for 40 h, she did not exhibit habitual episodes. Interictal EEG showed intermittent irregular delta waves and sharp regional transients in the left anterio-midtemporal area (Fig. 2); these sharp transients were not as clearly distinct from background activities as to be defined as epileptiform discharges, but they were reproducible in morphology and distribution and appeared not only in sleep but also in wakefulness. The scores of the Wechsler Adult Intelligence Scale — Third Edition showed normal intellectual performance (full scale IQ: 104, verbal IQ: 101, performance IQ: 106); however, secondary indices showed decreased verbal comprehension as compared with the other categories (verbal comprehension: 92, working memory: 102, perceptual organization: 97, processing speed: 113). There was no sign of depression or other psychiatric problems.
Fig. 1.
Brain magnetic resonance imaging (FLAIR) and interictal brain SPECT (123I). Note the decrease of blood flow in the left frontal and temporal lobes (arrows).
Fig. 2.
Interictal EEG showing regional sharp transients in the left anterio-midtemporal region. These sharp transients were not as clearly distinct from background activities as to be defined as epileptiform discharges, but they were reproducible in morphology and distribution and appeared not only in sleep but also in wakefulness.
Considering that the EEG finding was subtle but in concordance with the clinical semiology of autonomic symptoms followed by loss of consciousness and that the interictal SPECT and neuropsychology findings were compatible with dysfunction of the left hemisphere, we diagnosed the patient with partial epilepsy originating from the left temporal lobe. Further inquiry into subjective symptoms revealed that, immediately before losing consciousness, she frequently had sudden emergence of old memories of her childhood relating to when she had played with her brother. After starting carbamazepine and adjusting dosage at 300 mg/day to maintain therapeutic plasma concentration, she did not experience an episode over the follow up period of greater than six months.
3. Discussion
Temporal lobe epilepsy can manifest with diverse autonomic symptoms and signs, and abdominal sensations often herald the onset of epileptic seizures. Among them is an uncommon syndrome called abdominal epilepsy in which gastrointestinal complaints, usually abdominal pain and nausea, are the primary or the sole manifestation of epileptic seizures [1], [2], [3], [4]. The present case demonstrated that, though extremely rare, recurrent diarrhea can be a cardinal manifestation of temporal lobe epilepsy. In patients who present with diarrhea and other autonomic symptoms otherwise unexplained, epilepsy should be listed in the possible diagnoses by careful history taking.
Diagnosing epilepsy is not straightforward, especially in patients who do not exhibit convulsions or other typical motor manifestations. Commencement of antiepileptic therapy can be delayed by decades as in the current patient until a possible diagnosis of epilepsy is made on the basis of careful patient history taking, including a detailed description of the subjective and objective events by patients and witnesses. Electroencephalogram is the cardinal method for diagnosis when significant epileptiform discharges are detected. In contrast, EEG is normal in about 50% of individuals clinically diagnosed with a seizure, i.e., normal EEG does not exclude the presence of epileptic disorder [5]. Therefore, even subtle EEG findings should be taken into account when they are reproducible and in concordance with clinical manifestations.
4. Conclusion
Recurrent diarrhea can be a manifestation of temporal lobe epilepsy. Careful and detailed patient history taking with sufficient knowledge of seizure semiology and EEG evaluation, while considering both its capabilities and limitations, will enable proper diagnosis and therapy of abdominal epilepsy in patients with paroxysmal gastrointestinal symptoms that are otherwise unexplained.
Conflict of interest
The authors have no conflict of interests to disclose.
References
- 1.Zinkin N.T., Peppercorn M.A. Abdominal epilepsy. Best Pract Res Clin Gastroenterol. 2005;19:263–274. doi: 10.1016/j.bpg.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Peppercorn M.A., Herzog A.G. The spectrum of abdominal epilepsy in adults. Am J Gastroenterol. 1989;84:1294–1296. [PubMed] [Google Scholar]
- 3.Freeman R., Schachter S.C. Autonomic epilepsy. Semin Neurol. 1995;15:158–166. doi: 10.1055/s-2008-1041019. [DOI] [PubMed] [Google Scholar]
- 4.Dutta S.R., Hazarika I., Chakravarty B.P. Abdominal epilepsy, an uncommon cause of recurrent abdominal pain: a brief report. Gut. 2007;56:439–441. doi: 10.1136/gut.2006.094250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krumholz A., Wiebe S., Gronseth G., Shinnar S., Levisohn P., Ting T. Quality Standards Subcommittee of the American Academy of Neurology; American Epilepsy Society. Practice parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69:1996–2007. doi: 10.1212/01.wnl.0000285084.93652.43. [DOI] [PubMed] [Google Scholar]