Abstract
Public health campaigns in several countries encourage population-wide reduced sodium (salt) intake, but excessive intake remains a major problem. Excessive sodium intake is independently related to adverse blood pressure and is a key factor in the epidemic of prehypertension/ hypertension. Identification of food sources of sodium in modern diets is critical to effective reduction of sodium intake worldwide. We used data from the INTERMAP Study to define major food sources of sodium in diverse East Asian and Western population samples. INTERMAP is an international, cross-sectional, epidemiologic study of 4, 680 individuals ages 40 to 59 years from Japan (four samples), People’s Republic of China (three rural samples), the United Kingdom (two samples), and the United States (eight samples); four in-depth, multipass 24-hour dietary recalls/person were used to identify foods accounting for most dietary sodium intake. In the People’s Republic of China sample, most (76%) dietary sodium was from salt added in home cooking, about 50% less in southern than northern samples. In Japan, most (63%) dietary sodium came from soy sauce (20%), commercially processed fish/seafood (15%), salted soups (15%), and preserved vegetables (13%). Processed foods, including breads/cereals/grains, contributed heavily to sodium intake in the United Kingdom (95%) and the United States (for methodological reasons, underestimated at 71%). To prevent and control prehypertension/hypertension and improve health, efforts to remove excess sodium from diets in rural China should focus on reducing salt in home cooking. To avoid excess sodium intake in Japan, the United Kingdom, and the United States, salt must be reduced in commercially processed foods.
Identification of modern sources of dietary sodium, consumed mostly as sodium chloride (salt), is critical to the reduction of sodium intake worldwide. Extensive concordant research evidence, from every research method, is the foundation for the repeated conclusion by independent expert groups that high dietary sodium intake is etiologically related to the worldwide epidemic of prehypertension, hypertension, and cardiovascular diseases (1-12). Evidence also indicates that reduced sodium intake lowers cardiovascular events (13,14). Furthermore, excessive dietary sodium intake has been linked to several other adverse medical conditions, including kidney stones (15), gastric cancer (16), asthma (17), and osteoporosis (18,19). All these findings have led to repeated recommendations by responsible agencies, national and international, for population-wide substantial reduction in salt intake (11,12,20).
Despite campaigns that encourage reduced sodium intake, excessive consumption remains a major public health problem in most populations. The World Health Organization (WHO) recommends <2,000 mg/day (20), but most of the world’s population consumes 2,300 to 4,600 mg sodium daily (21). Few studies have attempted to characterize the foods and food groups that are sources of sodium or to assess relative contributions from various sources (eg, inherent in foods, added during food processing, added as discretionary salt at home in cooking and at table, and salt in water and pharmaceuticals) (22-25). To our knowledge, no study has systematically compared dietary sources of salt in multiple countries.
Dietary sources of sodium must be identified and characterized to effectively implement population-based sodium reduction recommendations. With use of data from the INTERMAP Study on macro/micronutrients and blood pressure, we identified the major dietary sources of sodium in diverse population samples from Japan, People’s Republic of China, the United Kingdom, and the United States. This is the first study to use standardized methods for systematic concurrent measurement of food sources of salt intake in four countries.
PARTICIPANTS AND METHODS
This report is based on data from the INTERMAP Study, a cross-sectional basic epidemiologic investigation. The general aim of the INTERMAP research program as a whole is to advance knowledge on influences of multiple dietary factors—macro and micronutrients—on blood pressure of individuals, and on the role of these factors in the etiology of epidemic prehypertension and hypertension in adults of diverse geographic, ethnic, and socioeconomic backgrounds. Detailed study methods have been reported (26,27). Field surveys were done in 1996-1999. Quality-control measures for collection of dietary information were thorough; local, national, and international checks were conducted on the completeness and integrity of the data (26). A brief description of relevant study methods is provided here.
Participants
Participants were 4,680 women and men aged 40 to 59 years, recruited by stratified random sampling from 17 diverse populations—community-based or workplace-based—in Japan (four samples), People’s Republic of China (three rural samples), the United Kingdom (two samples), the United States (eight samples) (26,27). Persons were selected from four age–sex strata, women ages 40 to 49 years, men ages 40 to 49 years, women ages 50 to 59 years, and men ages 50 to 59 years. For any person not meeting protocol requirements, and thus excluded from all analyses, an alternative individual was selected from the same age–sex stratum. Mean participation rate was 49% (45% Japan, 83% People’s Republic of China, 22% United Kingdom, and 44% United States).
Data Collection
Each participant had four study visits: the first two on consecutive days, and on average 3 weeks later an additional two (26,27). Demographic data were obtained by interviewer-administered questionnaire. Two timed 24-hour urine collections were begun at Study Visit 1 and Study Visit 3, respectively, and completed at Study Visits 2 and 4. At each of the four study visits a multi-pass, in-depth 24-hour dietary recall was collected by a trained, certified interviewer. All foods and beverages consumed in the previous 24 hours, including dietary supplements, were recorded. These data enable identification of foods and food groups that account for individual dietary sodium intake.
In the United States, the dietary interviewer used the Nutrition Data System (NDS) (version 2.91, 1996, University of Minnesota Nutrition Coordinating Center [NCC], Minneapolis), in which guidance is given by a standardized computer program to maximize objectivity and completeness of the multipass probing as to foods consumed. Each food reported by the participant was entered into the computer immediately. The NDS contains nutrient composition information for 17, 000 foods, beverages, ingredients, and supplements. In Japan, People’s Republic of China, and the United Kingdom, dietary data were collected by interviewers using paper forms; data were coded and computerized after the interview. A random 10% of dietary recalls were recoded and re-entered, with staff blinded to original entries. Intake of sodium and other nutrients was calculated using country-specific food tables, enhanced and standardized for consistency across countries by the NCC. More specifically, all data on the nutrient composition of foods were derived from four data books—one per country, and were updated/enhanced/standardized by NCC senior staff working with the four INTERMAP senior national nutritionists and the senior international nutritionist. All foods were classified centrally in a standardized way by personnel at the INTERMAP International Coordinating Center in London, working with NCC senior staff and the senior INTERMAP national nutritionists in Japan, People’s Republic of China, and the United Kingdom so that every food was put into one of the 116 food subgroups in the NCC system used to classify every US food. Food classification was comparable across countries with the use of online computerization of 24-hour recall data in the United States, and postinterview, quality-controlled, standardized manual coding from paper forms in the three other countries. We focus on food sources of sodium for each of the four countries considered separately.
This analysis included 4, 680 (2,359 men and 2,321 women) of the 4,895 individuals initially surveyed. Based on the following, 215 individuals were excluded from the study and from all data analyses: 110 did not attend all four study visits; seven reported dietary data considered unreliable; 37 reported energy intake level from any 24-hour dietary recall that was <500 kcal/day or >5,000 kcal/day for women or >8,000 kcal/day for men; 37 lacked two complete urine samples; for 24, other data were incomplete, missing, or indicating a protocol violation.
All study procedures and protocols were approved by the institutional review board or ethics committee at each site. All participants gave written informed consent.
Statistical Considerations
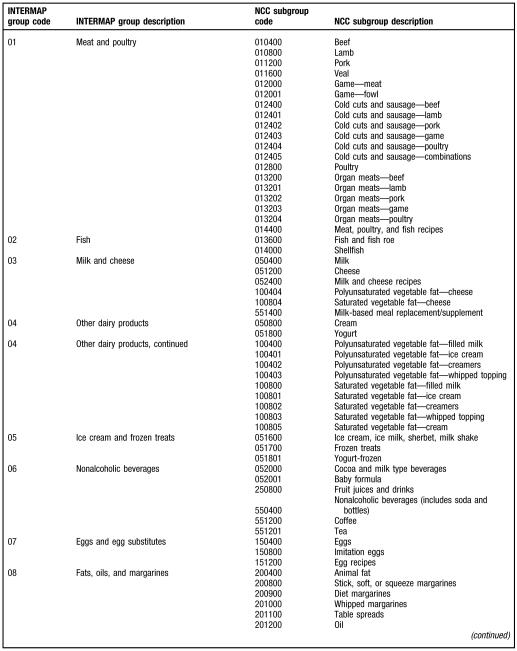
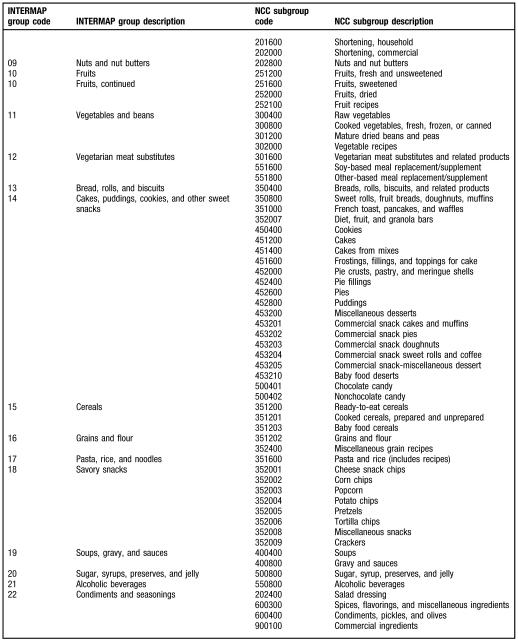
Data from each 24-hour recall interview were converted into macro- and micronutrient intake. Total sodium intake was calculated by summing estimates from all contributory food sources, including foods and beverages, ingested at home or away from home. Sodium content of each food item was determined using the enhanced national food database for each country. For each country, dietary sources (foods and food groups) that account for ≥80% of sodium intake were identified; food groups were those in the NCC classification (Figure).
In Japan, People’s Republic of China, and the United Kingdom, the coding system was designed to estimate nutrient intakes. Standardized classification into food groups, per the NCC classification, was undertaken by trained dietetics practitioners. For these countries, foods with multiple ingredients remained aggregated during data processing and analyses. For example, vegetables and meats were not disaggregated into their fresh and preserved components. Thus, vegetables include pickled, salted, and canned products; aggregated meats include salami, corned beef, liverwurst, ham, and sausage.
In Japan, the dietary source described as “salt” includes salt added during home cooking and at the table as well as in fast foods and foods eaten at restaurants. It excludes sodium in supplements. In some cases, the sodium contribution from a single food is presented separately from the sodium contribution of the entire food group because the contribution from that single food was high. Examples of this are: soy sauce, presented separately from sauces and condiments; miso soup, presented separately from all soups; fish, presented separately from seafood; and cured meats, presented separately from all meats. The dietary source category Miso Soup includes soups prepared from a variety of soy bean pastes (eg, Ama miso and Tanshokukara miso). Sodium from all other types of soups such as Japanese noodle soup and other soups with noodles (usually eaten as a snack) is in the category Other Soups. The dietary source category Fish includes fresh fish (eg, sashimi), fish salted by the respondent during preparation, and fish salted in commercial processing. Sodium from fish cakes, fish roe, and seafood was also calculated. The dietary source category Salted Fruits and Vegetables includes both vegetables and fruits salted (pickled) by the respondent and in commercial processing.
In the People’s Republic of China, the food group category Salt includes salt added during home cooking. It includes sodium chloride, but excludes monosodium glutamate (MSG), the tenderizers sodium bicarbonate and sodium carbonate, as well as salt in supplements. Salted Mustard, Turnip Greens, and Cabbage could not be disaggregated into fresh and preserved components; hence, this category includes pickled and canned products as well as salt added by the respondent during cooking or at the table.
In contrast to data from the People’s Republic of China, Japan, and the United Kingdom, some US foods with multiple ingredients such as fast foods and other processed foods were disaggregated during electronic data entry and computerization; for example, fried chicken leg became a chicken leg, salt, flour, and oil; baked potato became potato flesh, butter, and salt; egg and sausage biscuit became water, flour, shortening, whole egg, salt, chorizo sausage, and milk; jelly roll became water, baking powder, salt, whole egg, flour, jam, and sugar; and tortilla became water, flour, salt, shortening, and baking powder. Therefore, the US food group Salt Added during Cooking or Eating reflects salt added in home cooking and at the table, and salt in fast and processed foods. Because of this, the percentage of sodium from nondiscretionary processed foods is underestimated, whereas the amount of discretionary salt use is artificially inflated.
Sodium intake values for each individual were averaged across the four study visits. Country-specific relative contribution (% of total sodium intake) was estimated for every individual food, then for major food groups, and also for salt added to foods in cooking and at table (discretionary salt use).
RESULTS
Mean age of participants was 49 years (Table 1). Mean body mass index was lowest in the People’s Republic of China (23.1) and highest in the United States (28.9). Mean systolic blood pressure ranged from 117 mm Hg in Japan to 121 mm Hg in the People’s Republic China. Prevalence of hypertension ranged from 13% (Japan) to 27% (United States). Mean 24-hour urinary sodium excretion ranged from 3,702 mg (United Kingdom) to 5,633 mg (People’s Republic China); mean dietary sodium intake ranged from 3, 407 mg/person/day (United Kingdom) to 4, 662 mg /person/day (Japan) (Table 1). Mean levels were similar for the urinary and dietary sodium estimates for Japan, United Kingdom, and United States; for the People’s Republic China, dietary estimates were lower than urinary.
Table 1.
Characteristics (mean value±standard deviation [SD] or number and percent) of INTERMAP Study participants by country (Japan, People’s Republic of China [PRC], the United Kingdom [UK], and the United States [US]), sex, and overall
| Variable | Japan (n=1,145) |
PRC (n=839) |
UK (n=501) |
US (n=2,195) |
Men (n=2,359) |
Women (n=2,321) |
All (n=4,680) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mean ± SD | ||||||||||||||
| Age (y) | 49.4±5.3 | 49.0±5.8 | 49.1±5.6 | 49.1±5.4 | 49.2±5.5 | 49.1±5.4 | 49.2±5.5 | |||||||
| Height (m) | 1.61±0.09 | 1.59±0.08 | 1.69±0.09 | 1.68±0.10 | 1.72±0.08 | 1.58±0.07 | 1.65±0.10 | |||||||
| Weight (kg) | 61.2±10.2 | 58.9±10.0 | 78.2±15.3 | 82.3±19.6 | 78.4±18.6 | 66.5±17.3 | 72.5±19.0 | |||||||
| Body mass index | 23.4±2.9 | 23.1±3.4 | 27.5±4.6 | 28.9±5.9 | 26.4±5.0 | 26.3±5.9 | 26.4±5.5 | |||||||
| Systolic blood pressure (mm Hg) |
117.2±13.8 | 121.3±17.4 | 120.4±14.6 | 118.6±13.9 | 120.8±13.9 | 117.0±15.3 | 118.9±14.7 | |||||||
| Diastolic blood pressure (mm Hg) |
73.6±10.3 | 73.2±10.2 | 77.3±9.9 | 73.4±9.7 | 76.2±10.0 | 71.5±9.5 | 73.8±10.0 | |||||||
| 24-h urinary sodium (mg) |
4,561±1,293 | 5,233±2,308 | 3,339±1,130 | 3,739±1,365 | 4,554±1,720 | 3,770±1,510 | 4,165±1,666 | |||||||
| 24-h dietary sodium (mg) |
4,651±1,279 | 3,990±1,943 | 3,406±1,162 | 3,660±1,343 | 4,465±1,571 | 3,394±1,211 | 3,934±1,502 | |||||||
| Hypertension (yes)a |
n
153 |
% 13.4 |
n
145 |
% 17.3 |
n
116 |
% 23.2 |
n
595 |
% 27.1 |
n
544 |
% 23.1 |
n
465 |
% 20.0 |
n
1,009 |
% 21.6 |
Systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or taking medication for high blood pressure.
For Japan, 340 foods contributed more than 1 mg/person/day sodium. Important dietary sources were soy sauce (20%); soups (16.4%), particularly miso soups (9.7%) made from soy bean paste; salted fish, seafood, fish roe (15%); salted (pickled) vegetables and fruits (9.8%), particularly salted Japanese radish (4.3%); 9.5% came from salt added to foods during home cooking and at the table, and from salt in fast foods and foods eaten at restaurants (Table 2).
Table 2.
Dietary sources of sodium for participants from Japan, People’s Republic of China, United Kingdom, and United States
| Country | Dietary source: Foods and food groups |
mg/d/person | % sodium |
|---|---|---|---|
|
Japan
(n=1,145) |
mean=4,651 | ||
| Soy sauce | 932 | 20.0 | |
| Salted vegetables and fruits (eg, radish, apricots) |
458 | 9.8 | |
| Miso soup | 450 | 9.7 | |
| Fish (fresh and salted) | 443 | 9.5 | |
| Salt (from restaurants, fast foods, and home) |
441 | 9.5 | |
| Other soups (eg, Japanese noodle soup) |
311 | 6.7 | |
| Breads and noodles | 215 | 4.6 | |
| Sauces and condiments (not including soy) |
203 | 4.4 | |
| Fish cake | 131 | 2.8 | |
| Cured meats (eg, ham, sausage, bacon) |
103 | 2.2 | |
| Seafood (eg, squid, prawns, eel, oyster, crab) |
78 | 1.7 | |
| Roux (curry, consommé) | 64 | 1.4 | |
| Eggs | 53 | 1.1 | |
| Fish roe | 45 | 1.0 | |
| Total=84.4 | |||
| China (n=839) | mean=3,990 | ||
| Salt (added in home cooking) | 3,024.0 | 75.8 | |
| Soy sauce | 255.5 | 6.4 | |
| Mustard, turnip greens, and cabbage |
143.4 | 3.6 | |
| Sodium bicarbonate and sodium carbonate (tenderizers) |
98.1 | 2.5 | |
| Noodles | 88.8 | 2.2 | |
| Breads (eg, mantou, stuffed with bean) |
63.931.7 | 1.6 | |
| Salted eggs | 24.5 | 0.8 | |
| Monosodium glutamate | 0.6 | ||
| Total=93.5 | |||
| Southern China (n=278) (Guangxi) |
mean=2,491 | ||
| Salt (added in home cooking) | 1,836 | 73.7 | |
| Soy sauce | 246 | 9.9 | |
| Mustard, turnip greens, and cabbage |
175 | 7.0 | |
| Monosodium glutamate | 49 | 2.0 | |
| Pork | 24 | 1.0 | |
| Lettuce | 21 | 0.8 | |
| Sweet potato | 18 | 0.7 | |
| Noodles | 10 | 0.3 | |
| Peanuts | 9 | 0.3 | |
| Salted eggs | 8 | 0.3 | |
| Breads (eg, mantou) | 2 | 0.1 | |
| Sodium bicarbonate (tenderizer) | 1 | <0.1 | |
| Total=95.8 | |||
| Northern China (n=561) (Beijing and Shanxi) |
mean=4,733 | ||
| 3,614 | 76.4 | ||
| Salt (added in home cooking) | 260 | ||
| Soy sauce | 147 | 5.5 | |
| Sodium bicarbonate and sodium carbonate |
142 | 3.1 | |
| Mustard, turnip greens, and cabbage |
133 | 3.0 | |
| Breads (eg, mantou) | 131 | 2.8 | |
| Noodles | 49 | 2.8 | |
| Salted eggs | 32 | 1.0 | |
| Peanuts | 12 | 0.7 | |
| Monosodium glutamate | 0.3 | ||
| Total=95.5 | |||
|
United Kingdom
(n=501) |
mean=3,406 | ||
| Breads, grains, cereals | 1,178.2 | 34.6 | |
| Red meats, poultry, eggs | 696.3 | 20.4 | |
| Vegetables and vegetarian products |
280.1 | 8.2 | |
| Dairy | 267.0 | 7.8 | |
| Spices, flavorings, gravies, sauces, salt (added in home cooking) |
170.1 | 5.0 | |
| Soups | 169.0 | 5.0 | |
| Table spreads | 134.3 | 3.9 | |
| 125.9 | 3.7 | ||
| Total=88.6 | |||
|
United States
(n=2,195) |
mean=3,660 | ||
| Salt (from restaurants, fast foods, and home) |
1,062.9 | 29.0 | |
| Breads, grains, cereals | 713.0 | 19.5 | |
| Red meats, poultry, eggs | 439.5 | 12.0 | |
| Dairy products | 300.4 | 8.2 | |
| Gravies, seasonings, sauces, salad dressings |
262.0 | 7.2 | |
| Soy and teriyaki sauces | 166.4 | 4.5 | |
| Vegetables and textured vegetable protein |
119.4 | 3.3 | |
| Soups | 104.8 | 2.9 | |
| Pickles and olives | 54.7 | 1.5 | |
| Baking powder and soda | 52.7 | 1.4 | |
| Margarines | 45.9 | 1.3 | |
| Total=90.8 |
For the People’s Republic China, 105 foods contributed more than 1 mg/person/day sodium. Mean sodium intake was 3, 991 mg/person/day; most (75.8%) was from salt added during home cooking and at the table (Table 2). Other sources were soy sauce (6.4%); noodles and breads (3.8%); and mustard, turnip greens, and cabbage—not completely disaggregated into fresh and preserved. Sodium from MSG was 0.6% of the total. In contrast to the three other countries, for the People’s Republic China there were sizable regional differences between southern (ie, Guangxi) and northern (ie, Beijing and Shanxi) samples (Table 2). Mean northern sodium intake was 4,733 mg/person/day, notably higher than southern 2,491 mg/person/day. The main reason for this difference was the smaller discretionary salt use at home south than north, less by about 50%.
For the United Kingdom, breads, cereals, and grains—virtually all purchased commercially processed food products—were important sources (34.6%) of sodium intake, as were commercially processed red meats, poultry, and eggs (20.4%); soups (3.9%); and salted vegetables and vegetarian products (8.2%). The contribution of salt added in home cooking or at the table to overall intake was 5%.
For the United States, major food sources of sodium were breads, cereals, and grains (19.5 %), virtually exclusively store bought; that is, commercially processed; commercially processed red meats, poultry, and eggs (12.0 %); gravies, seasonings, sauces, and salad dressings (11.7%); and dairy products (8.2%). As a result of disaggregation of fast foods and other processed foods during the computerization process (see the Participants and Methods section), the category Salt Added to Foods is overestimated at 29.0%.
DISCUSSION
INTERMAP is the first study to use standardized methods for systematic concurrent measurement of salt intake in four countries. For every person, total sodium intake was estimated from both two timed 24-hour urinary excretion and four 24-hour dietary recalls. There was general concordance of mean findings by country, except for the People’s Republic of China where the dietary estimate was lower than the urinary. Our primary findings on foods/food groups supplying dietary sodium are that commercially processed foods such as breads, grains, cereals, soups, sauces, and cured meats account for the great majority of sodium consumed in Japan, the United Kingdom, and the United States. Discretionary sodium intake; that is, salt added to foods during home preparation or at the table, was a modest contributor to overall intake. In contrast, in the three rural People’s Republic of China samples, discretionary sodium use accounted for most sodium intake. Only a small proportion of sodium in foods is intrinsic (eg, sodium in milk), and the majority is added by manufacturers, while cooking, or at the table. Where some of the important food sources of sodium identified here are inherently sodium-free (eg, vegetables in Japan, red meat in United States), sodium is added to these products by manufacturers. We also found that average sodium intake for all four countries was well above the current WHO recommendation of <2,000 mg/day (20). Similar to our findings, previously published reports show sodium intake in Japan to be above recommended levels (28-30). A comparison of sodium intake data across the INTERMAP Study, the INTERSALT Study in the mid-1980s, and investigations in the 1950s reveals that Japanese sodium intake has declined from the 1950s to the 1980s (21). However, data from INTERSALT (1980s) and INTERMAP (1990s) show only small differences in intakes; excessive consumption continues. To lower sodium intake in the Japanese population, reductions must be made in commercially processed products such as sauces (particularly soy sauce) and soups (particularly miso soup); salted fish consumption must also be reduced. Fish is heavily used in traditional Japanese cooking. It is commonly cooked in high amounts of soy sauce and sugar, or salted and fermented. Use of fish in Western-style dishes is still low. Sauces, soups, and fish accounted for more than 50% of total sodium intake in the Japanese samples.
In the INTERMAP rural People’s Republic of China samples, we found extensive use of salting in home cooking and at the table (75.8% of total intake). Soy sauce accounted for 6.5% of total intake. These findings are consistent with other published data showing estimates of 63% (24) or >75% (31) of salt in the diet coming from discretionary salt. The tenderizers sodium bicarbonate and sodium carbonate, and the flavor enhancer MSG contributed 3.1%. Sodium from vegetables such as mustard, turnip greens, and cabbage (3.6%) could not be parsed into fresh or preserved vegetables, but inspection of individual food diaries by site nutritionists indicated that pickled, salted, and canned goods were primarily responsible for high sodium from vegetables. Our observation that the southern People’s Republic of China sample had lower dietary intake of sodium than northern People’s Republic of China samples has been reported in other studies (32). Lower average blood pressure and lower prevalence of high blood pressure has also been observed in southern People’s Republic of China samples compared to northern samples; lower sodium intake has been shown to be an important contributor to this more favorable blood pressure pattern (33). To reduce sodium intake in the Chinese rural farming population, discretionary sodium used for salting vegetables, eggs, and meats needs to be limited. The much lower intake in southern People’s Republic of China than northern indicates this is feasible, and useful healthwise (33). Cultural and economic considerations must be addressed in sodium reduction efforts; for example, in rural People’s Republic of China, salt is still used traditionally for preservation and storage of foods. However, widespread acquisition of home refrigerators is making these practices obsolete and dispensable.
Our results for the United Kingdom and United States are similar to prior studies showing that excessive salt intake in modern diets in these countries is a result mainly of salting in commercial food processing (22,23,34). Previously published data show that in the United Kingdom, 83% of dietary sodium comes from processed foods (23), and 77% in the United States (22). Our data collection and analysis techniques for the US samples resulted in underestimation of the percent of sodium coming from nondiscretionary sources. NDS computerization procedures disaggregated salt from processed foods in a way that made it impossible to fully determine salt from discretionary and nondiscretionary sources. This conclusion is supported by previously published data showing that discretionary salt is a relatively minor percentage of overall sodium intake in both the United States and United Kingdom (23,34,35). Data also show that approximately one quarter of cooking salt actually enters the consumed food; in the case of vegetables, 20% to 36% of salt added during cooking is recovered in the vegetables while the rest is discarded in cooking water (36). Unlike canned and pickled products, fresh vegetables, as such, do not contribute to excess sodium intake in the United States unless salt, or a salt-containing sauce, is added in cooking or at table. To enable the UK and the US populations to lower sodium intake sizably, significant reductions must be made in the sodium content of commercially processed foods that are the major purveyors of sodium into the individual diet. These include breads, grains, cereals, processed meats, poultry, eggs, spices, and sauces.
Our findings regarding food sources of sodium intake are relevant to the first decade of the 21st century. Evidence suggests that little improvement has been made in sodium content of current food sources in Japan, the People’s Republic of China, the United Kingdom, or the United States since the date of our original data collection. Food industry efforts are still few and far between, and little reduction has occurred in the sodium content of processed foods. Population intake of sodium remains way above recommended levels. In most respects our results are broadly comparable to data from recent national surveys in Japan, the People’s Republic of China, the United Kingdom, and the United States.
For Japan, Shimbo and colleagues in 1996 (37) reported findings concordant with our results; that is, primary food sources of sodium are soy sauce and salted vegetables, soups, and fish. Current Japanese Standard Food Tables that show levels of sodium in foods indicate the sodium content of salted vegetables/fruits, soups, salted fish, breads, and noodles is higher than that of other foods (38). Furthermore, an investigation by Kimira and colleagues (39) found that urinary sodium excretion was related significantly to intake of seasonings, vegetables, and noodles. Concordantly, data on trends from 1975 to 2005 shows intake of these foods remains high, consistent with an observed 2005 level of 4,331 mg/day dietary sodium (40).
Similar to our findings for People’s Republic of China rural samples, recently published data from national surveys show primary food sources of sodium to be salt and soy sauce; these two food sources made up 82% of total sodium intake (31,41,42). In addition, in 2009 a pilot study with 44 individuals, aged 50 to 70 years was conducted in Yunnan Province collecting one 24-hour urine sample. Mean 24-hour urine sodium excretion was 4,770±1,902 mg; comparable to findings in our study (personal communication, Liancheng Zhao, MD, June 29, 2009).
In the United Kingdom, the Food Standards Agency has set a target to reduce mean adult salt intake to 6,000 mg/day by 2012. Accordingly, voluntary efforts have been encouraged to reduce sodium in the food supply through the reformulation of food products. To our knowledge, there are no recent data on food sources of sodium in the United Kingdom. Efforts to monitor progress toward the foregoing target include analysis of 24-hour urinary sodium excretion, and there are ongoing discussions between the Food Standards Agency and United Kingdom’s major retailers about evaluating progress on gradual salt reduction in foods (43,44). Survey data from the World Action on Salt and Health suggest that food industry efforts can be improved and little reduction has occurred in the sodium content of processed foods (44). Urinary sodium data from a 2008 UK national survey indicate that mean UK salt intake is 8,600 mg/day, similar to the UK mean of 9,000 mg/day in 2005-2006, but significantly lower than estimate of 9,500 mg/day in 2000-2001; however, still in excess of recommended intake (21,44,45).
The latest estimates of US sodium intakes are from the 2005-2006 National Health and Nutrition Examination Survey (46). Similar to our findings, the total average daily sodium intake for individuals was 3,436 mg. There are reports of efforts on the part of a limited number of food companies to gradually reduce the sodium content of some processed foods (47-49). Available data indicate that only a small percentage of adults regularly buy reduced-sodium products—20% in 1988, 19% in 1995, and 15% in 2002 (50,51). Recent surveys by the Center for Science in the Public Interest (52) indicate that food industry efforts have resulted in only small reductions in the sodium content of processed foods. There are no data suggesting that primary food sources of sodium in the US diet have shifted as a result of any of these efforts to date. In fact, data from National Health and Nutrition Examination Surveys in 2001-2002 (53), 2003-2004, and 2005-2006 show that top contributors of sodium are similar to our findings for 1996-1999: breads, grains and cereals, meats, poultry and eggs, dairy products, sauces and seasonings, and soups (personal communication, Ronette Briefel, DrPH, RD, July 24, 2009). The continuing high prevalence of salt in commercially processed foods creates a major challenge for efforts to remove excess sodium from the diet. Because of this, restaurants and other food industry sectors play a major role in determining levels of salt in foods, thereby affecting health. For most individuals—including those concerned about limiting salt intake—complete avoidance of prepackaged and processed foods is difficult to achieve, inconvenient, or not desirable. Even with conscious avoidance of foods known to be high in sodium, and no use of salt in cooking or at the table, it is difficult to meet current sodium recommendations, especially when an individual’s diet includes fast foods and other prepackaged and processed foods. Separate analyses of INTERMAP data show that for individuals who attempted to lower salt intake in each of the four countries, including hypertensive persons, mean reduction actually achieved was small; and salt intake remained considerably above recommended levels (personal communication, Nagako Okuda, MD, November 12, 2008).
To support individual efforts, a public health approach addressing population-wide sodium reduction has been recommended (54). A recent WHO report calls for a combined strategy of consumer education, changes in the food environment, and worldwide reformulation of processed and prepared foods to achieve the lowest possible sodium content (20).
Limitations of our study include complexity of identifying and quantifying dietary sodium intake given variability in salt used in food preparation, home cooking, and commercial processing; however, efforts to cope with this in INTERMAP were extensive, and data indicate reasonable concordance for individuals of overall sodium intake as measured from the four 24-hour dietary recalls and from the two timed 24-hour urine collections (26). Further, use of local population samples (ie, not sampling of each country’s general population) and the response rates is a limitation; however, data on nutrient and food patterns of these samples by country and sex are concordant with data in the literature from multiple sources, including on food sources of sodium. It is reasonable to infer that our findings on food sources of sodium intake for the four countries reflect their situation in the closing years of the 20th century, and remain meaningful up to the present, with the qualification that discretionary salt was overestimated for US participants due to the NDS disaggregation of some mixed dishes. Despite such difficulties, this study has several strengths. These include diverse population-based samples; standardized collection of high-quality nutrition data based on four in-depth, multipass 24-hour dietary recalls per participant; state-of-the-art, updated, and standardized tables for each of the four countries on the nutrient composition of all reported foods; two timed 24-hour urine collections per person to estimate sodium intake; and multiple quality-control procedures. This study’s main limitation is the use of a computerization system that disaggregated some data leading to overestimation of the role of discretionary salt use in overall sodium intake for the US samples.
CONCLUSIONS
Excess sodium intake has been linked to increased risk of cardiovascular diseases and such adverse conditions as prehypertension/hypertension, renal stones, gastric cancer, asthma, and osteoporosis. To prevent and control prehypertension/hypertension and improve health, efforts to remove excess salt from diets must be enhanced. Our findings of much lower salt intake in southern than northern Chinese, with associated lower blood pressure, indicate this is feasible and efficacious; the emphasis at present needs in rural China to be on reducing discretionary salt use, but with modernization it is reasonable to anticipate that the challenge in China will become similar to that in the three other countries. Whereas the data presented here can be useful for dietetics practitioners in Japan, the People’s Republic of China, the United States, and the United Kingdom to educate individuals on the principal food sources of sodium, reduction of salt in commercially processed foods is essential for public health progress to achieve population-wide substantial reductions in salt intake.
Figure.
INTERMAP Study food groups (N=22) and National Coordinating Center (NCC) food subgroups (N=113).
ACKNOWLEDGEMENTS
The authors thank all INTERMAP staff at local, national, and international centers for their invaluable efforts (a partial listing can be found in reference 27).
FUNDING/SUPPORT: The INTERMAP Study was supported by grant no. 2RO1-HL50490 from the United States National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD; by the Chicago Health Research Foundation; and by national agencies in China, Japan (the Ministry of Education, Science, Sports and Culture Grant-in Aid for Scientific Research (A), no. 090357003), and the United Kingdom.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST: No potential conflict of interest was reported by the authors.
Contributor Information
CHERYL A. M. ANDERSON, assistant professor of epidemiology, Johns Hopkins University Bloomberg School of Public Health, and Welch Center for Prevention, Epidemiology, and Clinical Research, Baltimore, MD.
LAWRENCE J. APPEL, professor of medicine, epidemiology, and international health (human nutrition), Johns Hopkins Medical Institutions, and Welch Center for Prevention, Epidemiology, and Clinical Research, Baltimore, MD.
NAGAKO OKUDA, assistant professor, Department of Health Science, Shiga University of Medical Science, Otsu, Shiga, Japan.
IAN J. BROWN, research associate, Department of Epidemiology and Public Health, School of Medicine, Imperial College London, UK.
QUEENIE CHAN, senior research officer, Department of Epidemiology and Public Health, School of Medicine, Imperial College London, UK.
LIANCHENG ZHAO, associate professor, Department of Epidemiology, Fu Wai Hospital and Cardiovascular Institute, Chinese Academy of Medical Sciences, Beijing, China.
HIROTSUGU UESHIMA, professor, and K. Miura is an associate professor, Department of Health Science, Shiga University of Medical Science, Otsu, Shiga, Japan.
HUGO KESTELOOT, professor, Division of Epidemiology, Katholieke Universiteit Leuven, Leuven, Belgium.
KATSUYUKI MIURA, associate professor, Department of Health Science, Shiga University of Medical Science, Otsu, Shiga, Japan.
J. DAVID CURB, professor of geriatric medicine and internal medicine, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu.
KATSUSHI YOSHITA, leader, Project for the National Health and Nutrition Survey, Nutritional Epidemiology Program, National Institute of Health and Nutrition, Tokyo, Japan.
PAUL ELLIOTT, professor, Department of Epidemiology and Public Health, School of Medicine, Imperial College London, UK.
MONICA E. YAMAMOTO, assistant professor, Department of Epidemiology, University of Pittsburgh, Pittsburgh, PA.
JEREMIAH STAMLER, professor emeritus, Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL.
References
- 1.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks: US population data. Arch Intern Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. [DOI] [PubMed] [Google Scholar]
- 2.Stamler J. The INTERSALT study: Background, methods, findings, and implications. Am J Clin Nutr. 1997;65:626S–642S. doi: 10.1093/ajcn/65.2.626S. suppl. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki S, Zhang XH, Kesteloot H. Dietary sodium, potassium, saturated fat, alcohol, and stroke mortality. Stroke. 1995;26:783–789. doi: 10.1161/01.str.26.5.783. [DOI] [PubMed] [Google Scholar]
- 4.Khaw KT, Barrett-Connor E. The association between blood pressure, age, and dietary sodium and potassium: A population study. Circulation. 1988;77:53–61. doi: 10.1161/01.cir.77.1.53. [DOI] [PubMed] [Google Scholar]
- 5.Perry IJ, Beevers DG. Salt intake and stroke: A possible direct effect. J Hum Hypertens. 1992;6:23–25. [PubMed] [Google Scholar]
- 6.Cutler JA, Roccella EJ. Salt reduction for preventing hypertension and cardiovascular disease: A population approach should include children. Hypertension. 2006;48:818–819. doi: 10.1161/01.HYP.0000245673.93844.6d. [DOI] [PubMed] [Google Scholar]
- 7.He J, Ogden LG, Vupputuri S, Bazzano LA, Loria C, Whelton PK. Dietary sodium intake and subsequent risk of cardiovascular disease in overweight adults. JAMA. 1999;282:2027–2034. doi: 10.1001/jama.282.21.2027. [DOI] [PubMed] [Google Scholar]
- 8.Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, Nissinen A. Urinary sodium excretion and cardiovascular mortality in Finland: A prospective study. Lancet. 2001;357:848–851. doi: 10.1016/S0140-6736(00)04199-4. [DOI] [PubMed] [Google Scholar]
- 9.Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: Results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE) Arch Intern Med. 2001;161:685–693. doi: 10.1001/archinte.161.5.685. [DOI] [PubMed] [Google Scholar]
- 10.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH, DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 11.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM, American Heart Association Dietary approaches to prevent and treat hypertension. A scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 12.American Heart Association Nutrition Committee. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 13.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the Trials of Hypertension Prevention (TOHP) BMJ. 2007;334:885. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang HY, Hu YW, Yue CS, Wen YW, Yeh WT, Hsu LS, Tsai SY, Pan WH. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr. 2006;83:1289–1296. doi: 10.1093/ajcn/83.6.1289. [DOI] [PubMed] [Google Scholar]
- 15.Cirillo M, Laurenzi M, Panarelli W, Stamler J. on behalf of the Gubbio Population Study Research Group. Kidney Intl. 1994;46:1133–1139. doi: 10.1038/ki.1994.376. [DOI] [PubMed] [Google Scholar]
- 16.Tsugane S, Sasazuki S, Kobayashi M, Sasaki S. Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer. 2004;90:128–134. doi: 10.1038/sj.bjc.6601511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey OJ, Locke C, Cookson JB. Effect of alterations of dietary sodium on the severity of asthma in men. Thorax. 1993;48:714–718. doi: 10.1136/thx.48.7.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Devine A, Criddle AR, Dick IM, Kerr DA, Prince RL. A longitudinal study of the effect of sodium and calcium intakes on regional bone density in post-menopausal women. Am J Clin Nutr. 1995;62:740–745. doi: 10.1093/ajcn/62.4.740. [DOI] [PubMed] [Google Scholar]
- 19.Martini LA, Cuppari L, Colugnati FAB, Sigulem DM, Szejnfeld VL, Schor N, Heilberg IP. High sodium chloride intake is associated with low bone density in calcium stone-forming patients. Clin Neprol. 2000;54:85–93. [PubMed] [Google Scholar]
- 20.World Health Organization Forum Reducing salt intake in populations: Report of a WHO forum and technical meeting. World Health Organization Web site. www.who.int/dietphysicalactivity/SaltReport-VC-April07.pdf. Accessed September 1, 2009.
- 21.Brown IJ, Tzoulaki I, Candelas V, Elliott P. Salt intakes around the world: Implications for public health. Int J Epidemiol. 2009;38:791–813. doi: 10.1093/ije/dyp139. [DOI] [PubMed] [Google Scholar]
- 22.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10:383–393. doi: 10.1080/07315724.1991.10718167. [DOI] [PubMed] [Google Scholar]
- 23.Sanchez-Castillo CP, Warrender S, Whitehead TP, James WP. An assessment of the sources of dietary salt in a British population. Clin Sci (Lond) 1987;72:95–102. doi: 10.1042/cs0720095. [DOI] [PubMed] [Google Scholar]
- 24.Tian HG, Hu G, Dong QN, Yang XL, Nan Y, Pietinen P, Nissinen A. Dietary sodium and potassium, socioeconomic status and blood pressure in a Chinese population. Appetite. 1996;26:235–246. doi: 10.1006/appe.1996.0018. [DOI] [PubMed] [Google Scholar]
- 25.Kesteloot H. Relationship between dietary cations and blood pressure. Ann Nutr Metab. 1991;35(suppl 1):109–118. doi: 10.1159/000177690. [DOI] [PubMed] [Google Scholar]
- 26.Dennis B, Stamler J, Buzzard M, Conway R, Elliott P, Moag-Stahlberg A, Okayama A, Okuda N, Robertson C, Robinson F, Schakel S, Stevens M, Van Heel N, Zhao L, Zhou BF, INTERMAP Research Group The dietary data—Process and quality control. J Hum Hypertens. 2003;17:609–622. doi: 10.1038/sj.jhh.1001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stamler J, Elliott P, Dennis B, Dyer AR, Kesteloot H, Liu K, Ueshima H, Zhou BF, INTERMAP Research Group Background, aims, design, methods, and descriptive statistics (nondietary) J Hum Hypertens. 2003;17:591–608. doi: 10.1038/sj.jhh.1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakagawa H, Morikawa Y, Okayama A, Fujita Y, Yoshida Y, Mikawa K, Sakata K, Ishizaki M, Miura K, Naruse Y, Kagamimori S, Hashimoto T, Ueshima H. Trends in blood pressure and urinary sodium and potassium excretion in Japan: Reinvestigation in the 8th year after the INTERSALT study. J Hum Hypertens. 1999;13:735–741. doi: 10.1038/sj.jhh.1000915. [DOI] [PubMed] [Google Scholar]
- 29.Sasaki N. High blood pressure and the salt intake of the Japanese. Jpn Heart J. 1962;3:313–324. doi: 10.1536/ihj.3.313. [DOI] [PubMed] [Google Scholar]
- 30.Dahl LK. Salt and hypertension. Am J Clin Nutr. 1972;25:231–244. doi: 10.1093/ajcn/25.2.231. [DOI] [PubMed] [Google Scholar]
- 31.Zhai FY, Yang XG. China National Health and Nutrition Survey—Report Two: Food and Nutrients Intake in 2002 [in Chinese] People’s Medical Publishing House; Beijing, China: 2006. p. 254. [Google Scholar]
- 32.Kesteloot H, Huang DX, Li YL, Geboers J, Joossens JV. The relationship between cations and blood pressure in the People’s Republic of China. Hypertension. 1987;9:654–659. doi: 10.1161/01.hyp.9.6.654. [DOI] [PubMed] [Google Scholar]
- 33.Zhao L, Stamler J, Yan LL, Zhou B, Wu Y, Liu K, Daviglus ML, Dennis BH, Elliott P, Ueshima H, Yang J, Zhu L, Guo D, INTERMAP Research Group Blood pressure differences between northern and southern Chinese: Role of dietary factors: The international study on macronutrients and blood pressure. Hypertension. 2004;43:1332–1337. doi: 10.1161/01.HYP.0000128243.06502.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bull NL, Buss DH. Contributions of foods to sodium intakes. Proc Nutr Soc. 1980;39:30A. [PubMed] [Google Scholar]
- 35.Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P, INTERMAP Research Group Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: The INTERMAP study. J Hum Hypertens. 2003;17:623–630. doi: 10.1038/sj.jhh.1001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.James WP, Ralph A, Sanchez-Castillo CP. The dominance of salt in manufactured food in the sodium intake of affluent societies. Lancet. 1987;1:426–429. doi: 10.1016/s0140-6736(87)90127-9. [DOI] [PubMed] [Google Scholar]
- 37.Shimbo S, Hatai I, Saito T, Yokota M, Imai Y, Watanabe T, Moon CS, Zhang ZW, Ikeda M. Shift in sodium chloride sources in past 10 years of salt reduction campaign in Japan. Tohoku J Exp Med. 1996;180:249–259. doi: 10.1620/tjem.180.249. [DOI] [PubMed] [Google Scholar]
- 38.The Resources Council, Science and Technology Agency, Japan . Standard Tables of Food Composition in Japan, 5th revised edition [in Japanese] Printing Bureau, Ministry of Finance; Tokyo, Japan: 2000. [Google Scholar]
- 39.Kimira M, Kudo Y, Takachi R, Haba R, Watanabe S. Associations between dietary intake and urinary excretion of sodium, potassium, phosphorus, magnesium, and calcium. Japan J Hygiene. 2004;59:23–30. doi: 10.1265/jjh.59.23. [DOI] [PubMed] [Google Scholar]
- 40.Ministry of Health, Labour, and Welfare . The National Health and Nutrition Survey in Japan, 2005 [in Japanese] Daiichi Shuppan; Tokyo, Japan: 2008. [Google Scholar]
- 41.Zhai FY, Yang XG. China National Health and Nutrition Survey—Report Two: Food and Nutrients Intake in 2002 [in Chinese] Beijing, China: People’s Medical Publishing House: 2006. p. 100. [Google Scholar]
- 42.Guansheng MA, Qin Z, Yanping LI. The salt consumption of residents in China [in Chinese] Chinese J Prev Control Chronic Non-Commun Dis. 2008;16:331–333. [Google Scholar]
- 43.An Assessment of Dietary Sodium Levels among Adults (Aged 19-64) in the General UK Population in 2008, Based on the Analysis of Sodium in 24-Hour Urine Excretion. National Centre for Social Research; London, UK: 2008. p. 3. [Google Scholar]
- 44.Survey of over 260 food products around the world from KFC, McDonalds, Kellogg’s, Nestle, Burger King, and Subway. World Action on Salt and Health Web site. http://www.worldactiononsalt.com/media/international_products_survey_2009.xls. Accessed September 1, 2009.
- 45.He FJ, McGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- 46.Nutrient intakes from food: Mean amounts consumed per individual, one day, 2005-2006. US Dept of Agriculture, Agricultural Research Service Web site. www.ars.usda.gov/ba/bhnrc/fsrg. Accessed September 1, 2009.
- 47.Halliday J. Reduced sodium ingredients contribute to salt effort. http://www.foodnavigator.com/Product-Categories/Proteins-non-dairy/Reduced-sodium-ingredients-contribute-to-salt-effort. Accessed September 1, 2009.
- 48.Product development. http://www.nestle.com/SharedValueCSR/Products AndConsumers/NutritionHealthandWellness/ProductDevelopment.htm. Nestle Web site. Accessed September 1, 2009.
- 49.Roodenburg AJC, Feunekes GIJ, Leenen R, Ramsay G. Food products and dietary guidelines: How to align? Trends in Food Science and Technology. 2008;19:165–170. [Google Scholar]
- 50.Frazao E, editor. America’s Eating Habits: Changes and Consequences. US Department of Agriculture; Washington, DC: 1999. Agriculture Information Bulletin No. 750. [Google Scholar]
- 51.Health and Diet Survey: Dietary Guidelines Supplement—Report of Findings (2004 & 2005) US Food and Drug Administration; Washington, DC: 2008. [Google Scholar]
- 52.Jacobson M, editor. Sodium Levels in Processed Foods. 2nd Center for Science in the Public Interest; Washington, DC: 2008. [Google Scholar]
- 53.Moshfegh A, Goldman J, Cleveland L. What We Eat in America, NHANES 2001-2002: Usual Nutrient Intakes from Food Compared to Dietary Reference Intakes. US Department of Agriculture, Agricultural Research Service; Washington, DC: 2005. [Google Scholar]
- 54.Appel LJ. At the tipping point: Accomplishing population-wide sodium reduction in the United States. J Clin Hypertens (Greenwich) 2008;10:7–11. doi: 10.1111/j.1524-6175.2007.07227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]