Abstract
Bath-induced paroxysmal events in infants and children can be triggered by various etiologies, including cardiological, neurological, and metabolic causes. It is important to ascertain the underlying cause for such events as this significantly affects the child's management and prognosis. We present the case of a 19-month-old boy who presented with recurrent episodes of apnea, cyanosis, and reduced level of consciousness in response to bathing. Through detailed history and investigation, the diagnosis of water reflex epilepsy was made. Treatment with carbamazepine and adjustment of the bathing technique have prevented further episodes from occurring, and the child's growth and development are progressing normally.
Conclusion
Water reflex epilepsy can mimic a range of other conditions, and a high index of suspicion is required to establish the diagnosis. Children with water reflex epilepsy can achieve a good quality of life with modified bathing and appropriate antiepileptic medication.
Abbreviations: ED, emergency department; EEG, electroencephalogram; PEPD, paroxysmal extreme pain disorder; MRI, magnetic resonance imaging; ECG, electrocardiogram
Keywords: Bath-induced, Paroxysmal events, Water reflex epilepsy
1. Introduction
Paroxysmal events related to bathing in children can be caused by a range of etiologies. Elucidating the diagnosis requires thorough history, examination, and focused investigation, which require background knowledge of the likely causes for childhood paroxysmal water-induced events.
2. Case report
A 19-month-old boy was brought to the emergency department (ED) after an episode of reduced consciousness while bathing. His parents reported that when lukewarm water was poured over his chest, he turned blue around the lips and began gasping for air. During this time, his eyes “rolled back”, and he did not interact with his parents. There were no clonic movements, and he did not respond to physical stimulation. He subsequently fell asleep for approximately 1 h and was brought to the ED. On arrival, he was alert and looked well. There were no focal findings on examination, his development was appropriate, and his laboratory studies were normal including a blood glucose level of 5.5 mmol/L. The boy's parents reported similar, less profound episodes occurring during bathing over the previous 2 weeks. They noted that, initially, his head would go back, his eyes would roll upwards, and he would become floppy and limp. These episodes occurred only during bathing and lasted 2–3 min, followed by a period of sleepiness. Detailed neurological exam was normal. He was admitted to the pediatric ward for investigation.
Between these episodes, he had been well, and he did not have any evidence of intercurrent illness. Contact with water other than bathing such as splashing water at nursery did not provoke symptoms. He had normal attainment of developmental milestones, and there was no significant past medical history. He had been born at term with no neonatal problems after an uneventful pregnancy. He was up-to-date with the UK vaccination schedule, and he had not received any vaccinations recently. He was an only child, and his parents were well with no family history of seizures or epilepsy.
2.1. Investigation and management
Electrocardiogram demonstrated sinus rhythm with a normal QT interval. Bathing in lukewarm water while his vital signs were monitored provoked hypotonia, tachycardia, and brief apnea with associated desaturation. He stared straight ahead and made mouthing movements. He was removed from the bath and given high-flow oxygen. He was subsequently sleepy for approximately 1 h. A further similar episode occurred later while he was sleeping, this time without provocation.
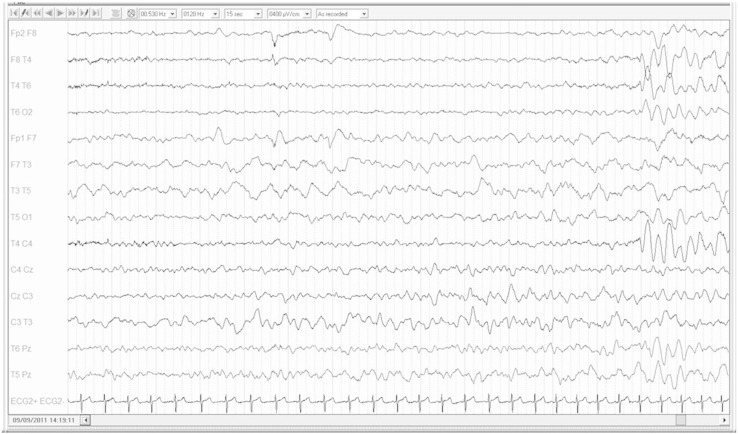
The first interictal EEG was normal using the standard 10–20 system. As he was clinically well between episodes and there was an avoidable trigger, he was discharged. Follow-up included a brain MRI, bathing EEG, and review in outpatient clinic. His parents were advised to sponge-wash him, which did not provoke the episodes. Prior to his bath, his background EEG showed 7- to 11-Hz (20–80 mV) activity mixed with some low amplitude irregular beta activity. The EEG during bathing, which provoked the same reaction as previously, demonstrated a build-up of left-sided temporal delta activity which soon involved the right side with the addition of suspicious sharp waves (Fig. 1). Widespread high amplitude irregular delta activity followed with slight left hemispheric dominance and occasional left-sided subtle sharp waves. Postictally, normal sleep phenomena were seen on the EEG with intermittent sleep spindles present.
Fig. 1.
Epileptiform activity provoked by bathing. During bathing, a slow build-up of irregular high amplitude (530 mV) delta activity over the left hemisphere was noted prior to any clinical change. Slow-wave activity subsequently spread to include the right hemisphere, becoming more generalized. There was concomitant hypotonia clinically. Electrode placement was the standard 10–20 system.
A diagnosis of water reflex epilepsy was made based on the clinical history, witnessed events, and the EEG findings. His MRI was normal, excluding an underlying structural abnormality. Because of occasional unprovoked seizures, he was commenced on carbamazepine 20 mg twice daily with a regime increasing up to 160 mg twice daily. At subsequent follow-up, he was developing normally and able to bathe without seizure activity.
3. Discussion
There are various bath-induced paroxysmal disorders that can present during infancy and early childhood. Initially, the primary question to consider is whether the episodes are consistent with epileptiform events. Water seemed an obvious trigger for these episodes, and reflex epilepsy has been described in response to water, although less commonly than photosensitive reflex epilepsy. The inability to physically interrupt the episodes and the apparent postictal period suggested seizure activity in this case. As space-occupying lesions can cause epileptogenic foci, underlying structural abnormalities (e.g., grey matter heterotopia, polymicrogyria, intracranial tumors) must be considered. Hot water epilepsy, a variant of bathing epilepsy, has been described as seizure activity precipitated by bathing in water with a temperature > 37 °C and in which seizures may not be provoked if water temperature is reduced [1], [2]. In this case, the water was lukewarm, and it did not appear to be temperature-related, consistent with water reflex or bathing epilepsy.
Nonepileptic paroxysmal disorders can present with similar episodes in response to a trigger such as water but must be differentiated as the underlying cause and management differs. Reflex anoxic seizures can occur in response to bathing if it is distressing and can be difficult to distinguish clinically from water reflex epilepsy as both can cause hypotonia, apnea, unresponsiveness, pallor, and postictal drowsiness. Reflex anoxic seizures can occur in other distressing situations as well. In this case, cardiac monitoring during an episode identified that the child became tachycardic rather than bradycardic/asystolic as seen when vagal overactivity occurs in reflex anoxic seizures. An EEG during an episode is important because while anoxic seizures can cause EEG changes including slowing and flattening, no epileptiform abnormalities are seen, in contrast to this case. Breath-holding can also cause episodes of cyanosis and loss of consciousness which can mimic seizure activity clinically. The history preceding the event is an important differentiator as it is usually precipitated by the child being upset or angry which was absent in this case. Cardiac syncope must also be considered, especially prolonged QT syndrome, and an ECG is an important first line investigation and, if strongly suspected, 24-hour ECG is recommended. The much rarer channelopathy of paroxysmal extreme pain disorder (PEPD) should also be considered. Paroxysmal extreme pain disorder is a rare autosomal dominant condition which typically presents in the neonatal period, arising due to a sodium channelopathy causing tonic events and autonomic signs such as flushing and perception of pain (not present in this case) in response to bathing [3]. Alternating hemiplegia of childhood can also present with paroxysmal episodes while bathing and is also associated with epilepsy [4]. There were no reported or witnessed episodes of hemiplegia or weakness in this case. Events due to hyperekplexia, a form of exaggerated startle response which can result in syncope, can be precipitated by bathing, causing episodes of tonic stiffening. The boy in this case, however, demonstrated hypotonicity during the episodes, and he did not have an exaggerated startle response. There are thought to be multiple etiological factors underlying these conditions, and ion channel mutations are thought to play a significant role in bath-induced paroxysmal disorders [5].
4. Conclusion
There is a wide differential diagnosis for reduced conscious level triggered by bathing including neurological, cardiological, and metabolic causes. Clinical history and witness accounts are crucial to target investigations and establish the diagnosis. Practical advice must be offered to parents as the implications of water reflex epilepsy should not be underestimated. Where seizure activity is limited to provoked episodes only, changing bathing practices such as sponging or changing water temperature can help to reduce or avoid events. For children who are also having unprovoked seizures as in this case, antiepileptic medication in addition can increase seizure-free periods. Although many children will grow out of reflex water epilepsy, some can go on to have nonreflex epilepsies, and parents should be warned of this.
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
C.J. Stutchfield, Email: cstutch@gmail.com.
N.R. Loh, Email: n.loh@nhs.net.
References
- 1.De Keyzer K., Corthouts I., Van Coster R., Verhelst H. Hot water epilepsy: a new Caucasian case. Eur J Pediatr. 2005;164:184–185. doi: 10.1007/s00431-004-1595-6. [DOI] [PubMed] [Google Scholar]
- 2.Gokcil Z., Ipekdal H., Ulas U., Odabasi Z. Hot water epilepsy: seizure type, water temperature, EEG findings and treatment. Neurologist. 2010;16(2):109–112. doi: 10.1097/NRL.0b013e3181bd603c. [DOI] [PubMed] [Google Scholar]
- 3.Fertleman C.R., Ferrie C.D., AIcardi J., Bednarek N.A., Eeg-Olofsson O., Elmslie F.V. Paroxysmal extreme pain disorder (previously familial rectal pain syndrome) JAMA Neurol. 2007;69(6):586–595. doi: 10.1212/01.wnl.0000268065.16865.5f. [DOI] [PubMed] [Google Scholar]
- 4.Mikati M.A., Kramer U., Zupanc M.L., Shanahan R.J. Alternating hemiplegia of childhood: clinical manifestations and long-term outcome. J Pediatr Neurol. 2000;23:134–141. doi: 10.1016/s0887-8994(00)00157-0. [DOI] [PubMed] [Google Scholar]
- 5.Nechay A., Stephenson J.B.P. Bath-induced paroxysmal disorders in infancy. Eur J Paediatr Neurol. 2009;13:203–208. doi: 10.1016/j.ejpn.2008.04.004. [DOI] [PubMed] [Google Scholar]