Abstract
The duration of untreated psychosis (DUP) is a key determinant in the severity of symptoms in patients with schizophrenia. DUP is a modifiable factor that if reduced can improve patient outcome and treatment response. We sought to decrease DUP in rural Argentina by instituting annual training of local health agents to better identify signs of mental illness and offer earlier intervention. DUP was estimated using Schedules of Clinical Assessment in Neuropsychiatry (SCAN). Ongoing training was correlated with a reduction in DUP. Reducing DUP through better screening can decrease the psychosocial burden of disease and improve the trajectory of psychosis.
1. Introduction
The duration of untreated psychosis (DUP) is the amount of time that elapses between the appearance of psychotic symptoms and the initiation of an adequate pharmacological treatment. Even though the onset of psychotic phenomena is often elusive, a variety of methods have been developed to ascertain it objectively. Albeit with the limitations attendant to its accurate determination, DUP predicts the initial clinical course of schizophrenia. Indeed, longer DUP probably has a neurotoxic effect that may result in reduced cortical thickness (Guo et al., 2013) and cognitive impairment (Rapp et al., 2013). Furthermore, longer DUPs are related with shorter periods of symptom remission, longer hospitalizations, less treatment adherence, increased risk of depression and suicide, substance abuse, and higher costs of treatment (Yung et al., 2007). DUP can be influenced by the insidious onset of symptomatology, the lack of public awareness, and the stigma associated with mental illness. Thus, DUP is a modifiable factor whose reduction can improve patient outcomes and increase the effectiveness of pharmacological treatment (McGlashan, 1999;Penttilä et al., 2013). Hence, the prolongation of DUP is a serious public health issue with complex socio-cultural and pathophysiological implications. Here we describe the impact of yearly training of primary care Health Agents (HA) in the province of Jujuy, Argentina, on DUP in all cases of never treated psychosis detected during a 7 years surveillance program as part of the Investigation of Movement Abnormalities and Genetic of Schizophrenia study (IMAGES).
The Ministry of Health of the Province of Jujuy has a primary care infrastructure heavily dependent on the use of HA, who are members of each community, typically with high school level education, familiar with the culture, the language, and the attitudes towards self-care in their environment. For HA assignment, the province is divided in 21 districts covering its three geographical regions, namely the valley, the jungle, and the highlands. Within each district, HA are assigned to monitor, educate, and facilitate access to care for a small number of households, resulting in complete or near complete coverage of the population. Each household is visited at the least two times per year, and HA are charged with the epidemiological surveillance of communicable diseases, health education for primary prevention, vaccination campaigns, prenatal and pediatric well-care, and of engaging and referral of community members in the health system. Prior to the onset of the study reported here, HA had never received training in mental health.
2. Methods
2.1. Targeted Training of HA
Beginning in 2004, we carried out annual training of all HA in the province in three sessions, one for each geographical region (valleys, jungle, and highlands). The province has a population of 672.260 according to the 2010 census, with 373.705 belonging to First Nations. The total number of agents on year 1 of the study was 650, and on year 7, 821. Turnover is minimal, so most of the HA had training in all years, and all of them had at least two trainings. Each training session lasted 3 hours and included lectures and printed materials focused on general knowledge about the signs and symptoms of severe mental illness (psychosis, mood or affective symptoms, disabling anxiety, alcohol and substance abuse), basic knowledge about risk factors, and practical instructions on risk management and referral for specialty care. HA fund of knowledge regarding mental health/illness was evaluated by administration of a brief questionnaire immediately before and after sessions to enhance their engagement in the process, but the primary outcome of the training was considered the number of appropriate referrals to the Mental Health system. Prior to 2004, HA did not receive any training whatsoever on mental health or psychiatric diseases. Assessment of training outcomes was achieved by administration of a brief questionnaire to evaluate HA knowledge of mental illness immediately before and after each session. Of note, the primary purpose of the treatment was not necessarily to increase the HA fund of knowledge regarding mental illness, but rather to increase awareness and promote early referrals to specialty care.
2.2. Diagnostic Ascertainment and Assessment of DUP
All protocols used in this study were approved by the Ethics Committee of the Province of Jujuy and by the Morsani College of Medicine IRB at University of South Florida. As part of the IMAGES study, HA were instructed to notify the Direction of Mental Health upon detection of any cases of severe mental illness. A determination was made on first contact of the acuity of the symptoms, and appropriate actions were taken to ensure the safety of the patient and his/her family (including dispatch of an ambulance for hospitalization if necessary and feasible for the person’s location). Once safety was ensured, investigators of the IMAGES study were immediately sent to evaluate the new patient in his/her place of residence (or in the Hospital Nestor Sequeiros if admitted). At this point two possible routes would be followed. If the person and his/her family were interested in participating in research, they were enrolled in the IMAGES study after written informed consent was obtained. Alternatively, if they were not interested, appropriate care was provided free of cost under the universal coverage provincial system. Assessment consisted of semi-structured interviews with the World Health Organization’s SCAN (Schedules of Clinical Assessment in Neuropsychiatry), and if criteria for a diagnosis of schizophrenia were met, a neuropsychological assessment, neurological exam, and transcranial ultrasound were collected. Inclusion criteria for the study were a diagnosis of DSM-IV schizophrenia (by two independent SCAN raters), age 18 to 65 years, absence of comorbid neurological or psychiatric disorders or substance abuse, and ability to provide informed consent.
2.3. Schedules of Clinical Assessment in Neuropsychiatry (WHO SCAN)
SCAN consists of a series of phenomenological assessment tools, a glossary of psychopathology, and software tools for administering the interviews, and algorithms to render a diagnosis in either ICD or DSM diagnostic systems (Wing et al., 1990). In a study using trained clinicians and videotaped interviews, the agreement per interviewer with regard to the reference diagnoses ranged from 87% (diagnostic group) to 94% (diagnostic caseness), and agreement on the syndrome level (without duration and interference criteria of DSM-IV) was excellent (Rijnders et al., 2000). Using the same methodology (blind scoring of videotaped interviews), we found very high inter-rater reliability for part 1, part 2, and the psychosis sections of SCAN (table 1). SCAN has being field tested in 20 centers in 11 countries, including ours (http://whoscan.org).
Table 1.
Interrater reliability of SCAN Part 1 (somatoform, anxiety, mood and substance use disorders), SCAN Part 2 (psychotic disorders), and individual sections for hallucinations (section 17), experiences of thought interference and replacement of will (section 18), delusions (section 19), motor and behavioral symptoms (section 22) and speech abnormalities (section 24). Three raters independently score videos of the same interviews (n=30). Cohen’s kappa scores are provided.
| Kappa | STD | |
|---|---|---|
| SCAN PART 1 | 0.54 | 0.17 |
| SCAN PART 2 | 0.76 | 0.28 |
| SCAN Section 17 | 1.00 | 0.00 |
| SCAN Section 18 | 0.68 | 0.30 |
| SCAN Section 19 | 0.80 | 0.45 |
| SCAN Section 22 | 0.56 | 0.38 |
| SCAN Section 24 | 0.82 | 0.21 |
2.4. Estimation of DUP
SCAN provides semistructured items to record the age of onset of prodromal symptoms, the age of onset of first psychotic symptoms, the age of the first recognition of the illness and the age at which treatment began. These dates were estimated using direct questioning of the subject, collateral information from family members and any alternate sources of information, such as health or school records when available. We estimated onset of DUP as the time from which psychotic symptoms have occurred. In addition, we completed the SOS (Symptom Onset in Schizophrenia Inventory), which rates the presence and dates of onset of general prodromal, positive, negative, and disorganized symptoms, as well as a clinician, family, and patient global rating of onset of illness (Perkins et al., 2000).
2.5. Statistics
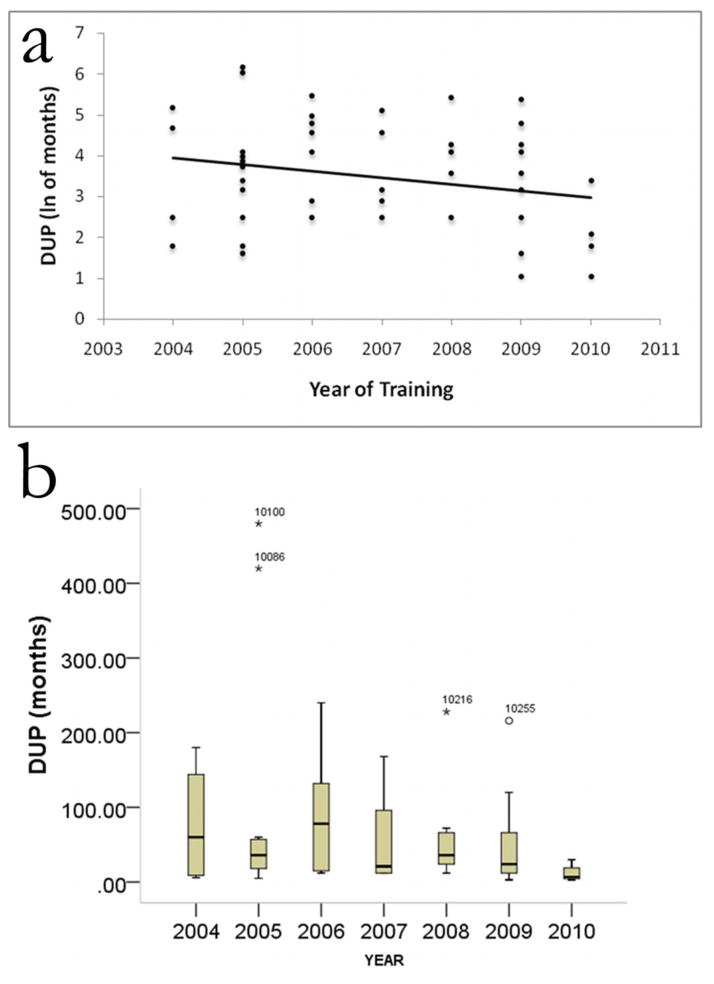
Interrater reliability for SCAN was calculated for scores of individual items, sections and parts of the interview. Results are reported for Part 1, Part 2 and pertinent sections evaluating psychotic symptoms. DUP measures were not normally distributed. A spread vs. level plot of DUP over year revealed a slope of 0.699 and a power of transformation of 0.301. Therefore, for linear correlation and analysis of variance DUP was elevated to power 0.301. Outlier analysis based on two standard deviations was also performed and the results are provided in figure 1b. Exclusion of outliers (Figure 1b) did not change the conclusions of the previous analysis.
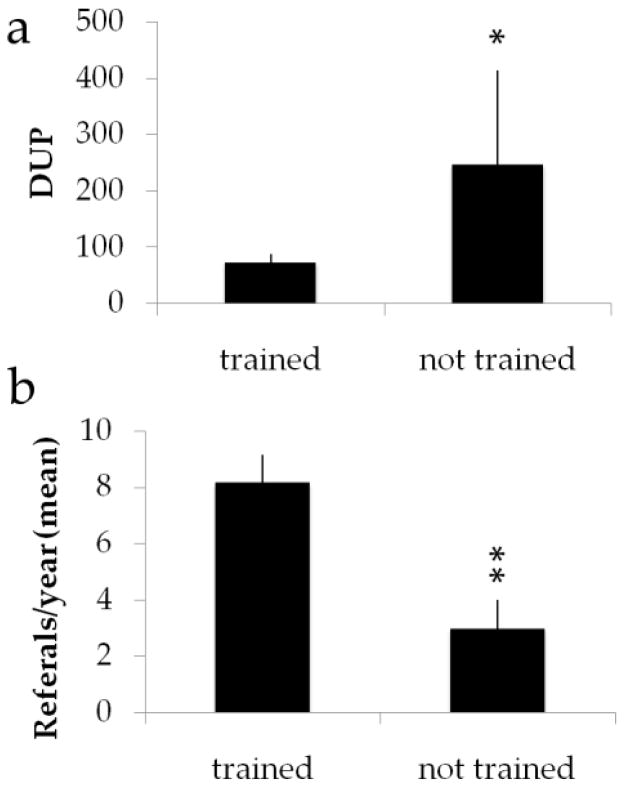
Figure 1.
Average DUP (panel a) and average number of referrals to specialty care (panel b) for years with and without training. Error bars represent SD.
3. Results
Average DUP was calculated for all cases of untreated psychosis (n=53; 17F/36M) detected in the Province on consecutive years of the study (from 2004 to 2010). Average age of participants was: 30.7 ± 11.1 (reported as mean ±s.d. unless otherwise stated) and average years of education: 8.8 ± 2.8. The rate of detection of new cases was relatively stable (4 patients on year 1, and 5 patients on the last year). Most notably, when the mean DUP for years 2004–2010 (following yearly training) (Mean±SEM: 68.9±97.6) is compared to years 2011–2014 (when trainings were not performed but intakes continued) (Mean±SEM: 366.0±640.5), and the difference was highly significant (Figure 1a, F=10.785; p=0.002). Furthermore, the average number of new referrals to the Mental Health service was also significantly increased in years of training (Figure 1b). In this regard, we found a strong correlation between recognition of symptoms and risk factors on the surveys and index of referral to the Direction of Mental Health (Spearman r =−0.154, p<0.000, n=4,140).
Average DUP steadily decline on consecutive years of training from 76.5± 63.3 weeks in year 1, to 11.7±12.3 weeks on year 6. In our sample, DUP was not normally distributed. Thus, we used a power transformation of the DUP values for subsequent analysis (see methods). A general linear model with years of training as the main predictor (with geographical region modeled as a random effect) found a significant relationship between HA training and DUP (F=3.2, p=0.026; Spearman r=−0.234, p=0.046, one-tailed, Figure 2a). The results were unchanged by exclusion of outliers (with very long DUP values, Figure 2b).
Figure 2.
Reduction in Duration of Untreated Psychosis over time. Panel a shows normalized DUP (by logarithm transformation) (Spearman r=−0.234, p=0.046, one-sided). Panel b shows median values and excluded outliers for each of the years of training.
4. Discussion
We found that consecutive years of training of health agents aimed at raising awareness of symptoms of mental health disorders, when coupled with an effective system to refer cases to specialty care, correlates with reductions in DUP in new cases detected in a rural environment. It has been pointed out that reducing DUP through early detection may be possible from a service systems perspective (McGlashan, 1999), and our data support this notion. Reducing DUP, in addition to obtaining a better response to symptomatic medications, may improve long-term prognosis by attenuating ongoing neurotoxicity (McGlashan, 1999;Guo et al., 2013;Penttilä et al., 2013). At least two independent reviews have provided evidence for a negative influence of longer DUP on short-term outcomes of schizophrenia (Marshall et al., 2005;Perkins, 2006;Harrigan et al., 2003). Since most predictors of outcome in first-episode psychosis are not modifiable and DUP remained a significant predictor of outcome after adjusting for the effects of many other variables, DUP could prove to be a target for secondary preventive efforts in early psychosis (Harrigan et al., 2003). Indeed, consistent with our data, community education and intervention in a Norwegian early detection study of psychosis resulted in decreased average DUP (Johannessen et al., 2001;Larsen et al., 2001). In spite of the available evidence, primary and secondary prevention of schizophrenia, a disorder entailing many years of life in disability, is still being neglected. The determinants of DUP are complex, and include social factors such as accessibility to health care services and social stigma, pathological factors such as the nature, intensity and the velocity of accumulation of symptoms, the toleration of the patient’s environment to deviant behavior, and the patient’s unique insight and distress. Since many of these factors can be approached by interventions, secondary prevention of schizophrenia focused on identification and intervention early in the course of the illness appears feasible (Häfner, 2002). Furthermore, it has been pointed out that most of the social consequences of schizophrenia become evident before the first treatment contact, underscoring the urgency for early intervention and preventative action (Häfner, 2002). The data reported here demonstrates that a simple fact-based training of physician extenders aimed at increasing disease awareness, coupled with facilitation of referrals to specialized care, can result in reductions in DUP over time.
Acknowledgments
Role of the Funding Source. The funding agencies had no participation whatsoever in the design, analysis, interpretation, or communication of the data and in no way influenced the contents of this manuscript.
This work was funded in part by grants NIMH K08MH077220, NIH FIC 7R21TW007882-05, NIH FIC 3R21TW007882-04S1 and by the Roskamp Endowment fund and two NARSAD (Brain and Behavior Foundation) grants to GdeE. GdE is Constance and Stephen Lieber Investigator, Sidney R. Baer Junior Investigator and Roskamp Chair of Biological Psychiatry. The authors wish to thank the Agentes Sanitarios of the Province of Jujuy for their generous and untiring collaboration with the study.
Footnotes
Contributors.
EP, MC, SS, GGA, GG and MB were responsible for training of health agents, ascertainment of diagnosis, evaluation of DUP and editing of the manuscript. DK, JM and LS were responsible for data analysis, writing and editing of the manuscript. JIE and GAdE were responsible for experimental design, training and certification of evaluators on the use of SCAN, training of health agents, assessment of outcome of training sessions, data analysis and writing and editing the final version of the manuscript.
Conflict of interest. None of the authors has any conflict of interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Guo X, Li J, Wei Q, Fan X, Kennedy DN, Shen Y, Chen H, Zhao J. Duration of untreated psychosis is associated with temporal and occipitotemporal gray matter volume decrease in treatment naïve schizophrenia. PloS One. 2013;8:e83679. doi: 10.1371/journal.pone.0083679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häfner H. Prevention and early intervention in schizophrenia: facts and visions. Seishin Shinkeigaku Zasshi. 2002;104:1033–1054. [PubMed] [Google Scholar]
- Harrigan SM, McGorry PD, Krstev H. Does treatment delay in first-episode psychosis really matter? Psychol Med. 2003;33:97–110. doi: 10.1017/s003329170200675x. [DOI] [PubMed] [Google Scholar]
- Johannessen JO, McGlashan TH, Larsen TK, Horneland M, Joa I, Mardal S, Kvebaek R, Friis S, Melle I, Opjordsmoen S, Simonsen E, Ulrik H, Vaglum P. Early detection strategies for untreated first-episode psychosis. Schizophr Res. 2001;51:39–46. doi: 10.1016/s0920-9964(01)00237-7. [DOI] [PubMed] [Google Scholar]
- Larsen TK, Friis S, Haahr U, Joa I, Johannessen JO, Melle I, Opjordsmoen S, Simonsen E, Vaglum P. Early detection and intervention in first-episode schizophrenia: a critical review. Acta Psychiatr Scand. 2001;103:323–334. doi: 10.1034/j.1600-0447.2001.00131.x. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62:975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999;46:899–907. doi: 10.1016/s0006-3223(99)00084-0. [DOI] [PubMed] [Google Scholar]
- Penttilä M, Miettunen J, Koponen H, Kyllönen M, Veijola J, Isohanni M, Jääskeläinen E. Association between the duration of untreated psychosis and short- and long-term outcome in schizophrenia within the Northern Finland 1966 Birth Cohort. Schizophr Res. 2013;143:3–10. doi: 10.1016/j.schres.2012.10.029. [DOI] [PubMed] [Google Scholar]
- Perkins DO. Review: longer duration of untreated psychosis is associated with worse outcome in people with first episode psychosis. Evid Based Ment Health. 2006;9:36. doi: 10.1136/ebmh.9.2.36. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J, Lieberman JA. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophr Res. 2000;44:1–10. doi: 10.1016/s0920-9964(99)00161-9. [DOI] [PubMed] [Google Scholar]
- Rapp C, Studerus E, Bugra H, Aston J, Tamagni C, Walter A, Pflueger M, Borgwardt S, Riecher-Rössler A. Duration of untreated psychosis and cognitive functioning. Schizophr Res. 2013;145:43–49. doi: 10.1016/j.schres.2012.12.016. [DOI] [PubMed] [Google Scholar]
- Rijnders CA, van den Berg JF, Hodiamont PP, Nienhuis FJ, Furer JW, Mulder J, Giel R. Psychometric properties of the schedules for clinical assessment in neuropsychiatry (SCAN-2.1) Soc Psychiatry Psychiatr Epidemiol. 2000;35:348–352. doi: 10.1007/s001270050249. [DOI] [PubMed] [Google Scholar]
- Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, Jablenski A, Regier D, Sartorius N. SCAN Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–593. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
- Yung AR, Killackey E, Hetrick SE, Parker AG, Schultze-Lutter F, Klosterkoetter J, Purcell R, Mcgorry PD. The prevention of schizophrenia. Int Rev Psychiatry Abingdon Engl. 2007;19:633–646. doi: 10.1080/09540260701797803. [DOI] [PubMed] [Google Scholar]