Abstract
One disadvantage of direct anticoagulant drug is the lack of an antidote, which may become relevant in patients with traumatic brain injury. A 77-years old man with atrial fibrillation and syncope received dabigatran despite recurrent falls. Due to a ground-level-fall, he suffered from subarachnoidal and intraparenchymal hemorrhages, subdural hematoma and brain edema with a midline shift. Despite osteoclastic trepanation and hematoma-evacuation he remained comatose and died seven days later without regaining consciousness. Most probably, decreased dabigatran clearance due to increased age might have contributed to the fatal course. We suggest withholding anticoagulant therapy in patients with unexplained falls. If anticoagulant therapy is deemed necessary, vitamin-K-antagonists with their potential for laboratory monitoring and reversal of anticoagulant activity should be preferred.
Keywords: Cerebral hemorrhage, Anticoagulation, Dabigatran, Atrial fibrillation
1. Introduction
Dabigatran, a direct thrombin inhibitor, is one of the direct anticoagulant drugs (DOACs) which are increasingly used in patients with atrial fibrillation (AF) for prevention of embolism. Dabigatran has been compared with the vitamin-K-antagonist (VKA) warfarin in the randomized evaluation of long-term anticoagulant therapy trial (RE-LY).[1] In that trial, the rates of ischemic strokes and intracranial haemorrhages were lower with dabigatran than with warfarin.[2] Patients with recurrent falls were excluded from RE-LY.[1] In real life, however, patients who are prone to falls are prescribed DOACs because physicians believe them to be “safer” than VKA. One of the disadvantages of the DOACs (Table 1), the lack of an antidote for prompt reversal of the anticoagulant effect, may become relevant in traumatic brain injury as illustrated by the following case.
Table 1. Advantages and disadvantages of the direct oral anticoagulant drugs.
| Advantage | Disadvantage |
| No need for repeated blood testing | No laboratory test for effectiveness of anticoagulation |
| Fixed doses | Elimination dependent on renal (dabigatran) and/or hepatic (factor Xa inhibitors) function |
| Less bleeding events than with warfarin in trials | No antidote |
| Less stroke/embolism than with warfarin in trials | Unknown potential for drug- and food interactions |
| Few known drug-drug interactions | Higher price than warfarin |
| No known food-drug interaction | Intricate application of dabigatran-capsule |
2. Case Report
TThe patient is a 77-years old man. He had had multiple sclerosis for 30 years, hypertension for 10 years, AF for 7 years, and dilated cardiomyopathy for 5 years. Because of his neurologic comorbidity associated with repeated falls, his physicians estimated the bleeding risk as high. He received no anticoagulant therapy until at age 73 years (in 2010) when he suffered from an ischemic stroke with right-sided hemiparesis and oral anticoagulation with phenprocoumon was started. Since 2011 he suffered from increasing cognitive impairment. In 2012, the mini-mental state examination yielded 18/30 points. A therapy with rivastigmin was not tolerated because of diaphoresis. In March 2012, he suffered from two episodes of speech disturbance, amaurosis fugax and right-sided weakness which were interpreted as prolonged reversible ischemic neurologic deficits. Because of unstable international normalised ratio (INR) values, the anticoagulant therapy was switched from phenprocoumon to dabigatran 300 mg/d. Since March 2012 recurrent syncopes occurred. Tachycardia-bradycardia syndrome was diagnosed, and he received a VVIR pacemaker in June 2012. Despite the pacemaker the syncopes recurred during one of which he nearly drowned. Neurologic investigation including electroencephalo-graph (EEG) in March 2014 disclosed no causes of syncopes. The treating physicians suspected a vagovasal etiology, but neither initiated further investigations nor considered changes in the anticoagulant therapy. He was on a chronic medication with nebivolol 5 mg/d, spironolactone 25 mg/d, venlafaxine 75 mg/d and dabigatran 300 mg/d at that time. His CHA2DS2VASc Score was 6.
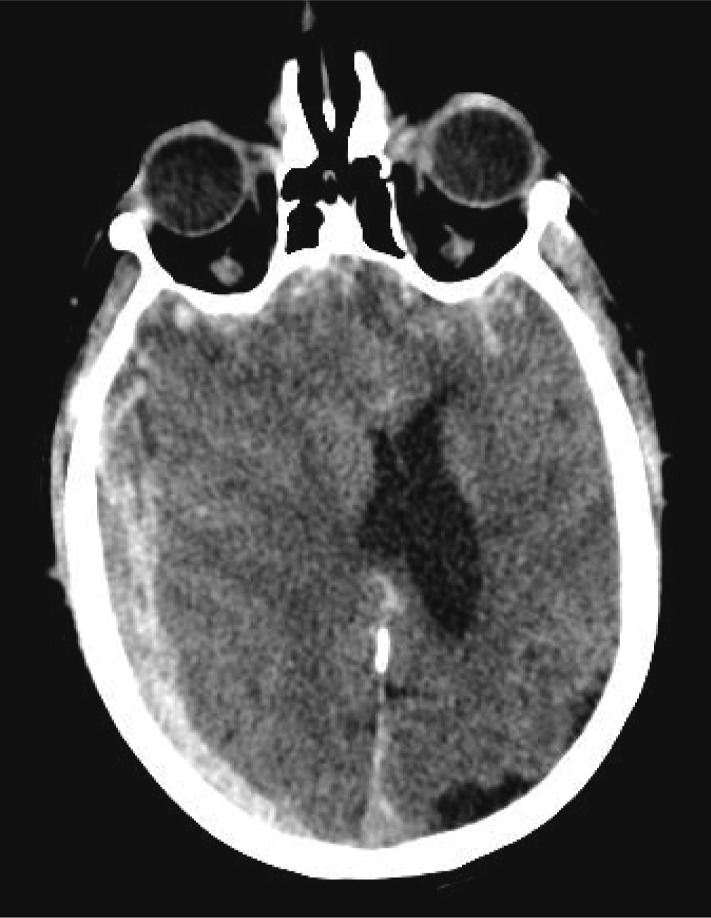
In June 2014, he fell from his chair without any prodromi and hit his head. He had taken his last dabigatran tablet 2 h before the accident. His wife called for the emergency service who found him soporous with a Glasgow coma scale (GCS) of 12. On admission, he started to vomit requiring intubation. Cerebral computed tomography (CCT) showed extensive subarachnoidal and intraparenchymal hemorrhages, subdural hematoma and brain edema with a midline shift (Figure 1). The results of the blood tests are listed in Table 2. The prolonged thrombin time indicated anticoagulant activity of dabigatran. Interrogation of the pacemaker showed AF and no dysfunction at the time of the fall. Due to the massive bleeding, the midline shift and the neurologic deterioration it was decided to perform surgery 4 h after the fall, 6 h after he had taken the last dabigatran dose. Osteoklastic trepanation and evacuation of the subdural hematoma were carried out, and a left-sided parenchymal probe was inserted. For correction of his anticoagulation therapy he received 3000 IU human prothrombin complex concentrate and 15 µg desmopressin pre-and intraoperatively. The postoperative CCT showed an increase in the size of the haemorrhage (Figure 2). The patient remained comatose with a GCS of 3 and died 7 days later without regaining consciousness.
Figure 1. Cerebral computed tomography two hours after the trauma showing extensive subarachnoidal and intraparenchymal hemorrhages, subdural hematoma and brain edema with a midline shift.
Table 2. Laboratory findings.
| Parameter (normal range) | D1 15: 00 | D1 19: 35 | D2 07: 51 | D3 06: 44 | D3 18: 21 | D4 06: 43 | D6 07: 24 |
| BUN, 8–23 mg/dL | 17 | NM | 11 | 10 | NM | NM | NM |
| Creatinine, < 1.1 mg/dL | 0.93 | NM | 0.96 | 0.84 | NM | 0.71 | NM |
| *Cr clearance, > 90 mL/min | 85 | NM | 82 | 94 | NM | 111 | NM |
| Potassium, 3.5–5.5 mmol/L | 4.2 | NM | 4.1 | 4.3 | NM | 3.9 | NM |
| Sodium, 135–150 mmol/L | 136 | NM | 138 | 139 | NM | 138 | NM |
| Haemoglobin, 14–17 g/dL | 14.5 | 11.2 | 11.9 | 11.4 | 11.4 | 10.7 | NM |
| Thrombocytes, 150–450/nL | 249 | 202 | 209 | 174 | 180 | 172 | NM |
| INR | 1.09 | NM | NM | NM | NM | NM | NM |
| PT, 70% –130% | 64 | 63 | 73.0 | 65.0 | 63 | 62 | 76 |
| aPTT < 33 s | 52 | 54.1 | 39.1 | 37.3 | 36.2 | 36.9 | 38.4 |
| TT, 14–21 s | 186 | NM | 100.5 | NM | NM | NM | NM |
| Fibrinogen, 1.50-4.50 g/dL | 3.26 | NM | 3.59 | NM | NM | NM | NM |
| ASAT, 0–35 U/L | 34 | NM | 39 | 31 | NM | 23 | NM |
| ALAT, 0–35 U/L | 18 | NM | 20 | 18 | NM | 15 | 52 |
| Gamma GT, 0–40 U/L | 41 | NM | 33 | 33 | NM | 38 | 83 |
| Bilirubin, 0.0–1.1 mg/dL | 0.92 | NM | 2.54 | 3.26 | NM | 3.39 | 2.3 |
| Total protein, 64–83 g/L | NM | NM | 49 | NM | NM | NM | NM |
*According to the Cockcroft-Gault formula. ALAT: alanine aminotransferase; aPTT: activated partial thromboplastin time; ASAT: aspartate aminotransferase; BUN: blood urea nitrogen; Cr: Creatinine; GT: glutamyltransferase; INR: international normalised ratio; PT: prothrombin time; TT: thrombin time; NM: not measured.
Figure 2. Postoperative cerebral computed tomography 26 h after the trauma showing an increase in the size of the hemorrhage of the brain edema.

3. Discussion
Head trauma in the presented patient was severe and it is questionable if the outcome would have been different if he had not been anticoagulated. There are indications that the pathophysiology of traumatic intracranial hemorrhages differs from spontaneous intracranial hemorrhage due to extensive endothelial activation exacerbating prothrombotic and proinflammatory signaling pathways in traumatic intracranial hemorrhage.[3]
The influence of dabigatran on traumatic brain injury has only been investigated in animal models, so far.[4] Little is known about patients who suffered from traumatic brain injury in the DOAC-investigating trials. There are indications from RE-LY that traumatic intracerebral haemorrhages under dabigatran may have a higher mortality then under warfarin.[2] In this trial, 22 traumatic intracranial haemorrhages occurred under dabigatran (intracerebral n = 4, subdural n = 15, subarachnoid n = 3), and 6 of them (27%) were fatal. In the patients randomized to warfarin, 46 traumatic intracranial haemorrhages occurred (intracerebral n = 4, subdural n = 16, subarachnoid n = 4), and only 5 of them (11%) were fatal. No details were reported how these patients were treated and if they underwent surgery.[2]
In addition to RE-LY, there are case reports which indicate that the therapy of fall-associated brain injuries in patients under dabigatran is difficult since there is no specific antidote available, as listed in Table 3.[5]–[12] From these cases it can be inferred that patients with chronic subdural hematoma under dabigatran have a better prognosis than patients with acute subdural hematoma which is similar to patients under VKA- or antiplatelet-therapy.[13]
Table 3. Traumatic cerebral bleedings reported under dabigatran.
| References | Age/sex | Trauma | Type of bleeding | Reversal of dabigatran | Surgery | Discharge |
| [5] | 85/F | MHT | SDH, MS | HD attempt failed | Burr hole drainage | Neurologically intact |
| [6] | 94/M | GLF | SDH, MS | FEIBA, HD | Burr hole drainage | Mild hemiparesis |
| [7] | 80/M | GLF | SDH | Vitamin K | ND | Neurologically intact |
| [8] | NR | GLF | IP | NR | Craniotomy | Dead |
| [9] | 83/M | GLF | IP, tSAH, SDH | rFVII | ND | Dead |
| [10] | 88/F | GLF | tSAH, SDH | PCC, rFVII, HD | ND | Recovered |
| [11] | 87/F | NS | CSDH | ND | Burr hole evacuation | Fully recovered |
| [11] | 80/F | GLF | CSDH | PCC | Burr hole evacuation | Fully recovered |
| [11] | 86/M | GLF | CSDH | ND | Burr hole evacuation | Fully recovered |
| [11] | 74/M | GLF | CSDH | ND | Burr hole evacuation | Fully recovered |
| [11] | 87/F* | GLF | tSAH | ND | ND | NI |
| [11] | 87/F* | GLF | IP | ND | ND | NI |
| [12] | 79/F | GLF | IP, MS | ND | ND | Dead |
| [12] | 72/M | GLF | tSAH | FFP | ND | Neurologically intact |
| [15] | NR | NS | IP | FFP, HD platelets | Done, not specified | Dead |
| Present case | 77/M | GLF | IP, MS, tSAH, SDH | PCC, desmopressin | Trepanation, hematoma evacuation | Dead |
*This patient suffered from two falls. CSDH: chronic subdural hematoma; FEIBA: factor VIII inhibitor bypass agent; FFP: fresh frozen plasma; GLF: ground-level fall; HD: hemodialysis; IP: intraparenchymal; MHT: mild head trauma; MS: midline shift; ND: not done; NR: not reported; NS: trauma type not specified; PCC: prothrombin complex concentrate; RfVII: recombinant factor VII; SDH: subdural hematoma; tSAH: traumatic subarachnoid hemorrhage.
Parra, et al.[14] reported five patients with closed head injury secondary to ground-level falls under dabigatran. All patients had repeated CCTs after reversal of anticoagulation, and in four patients, new or expanded haemorrhages were seen. Two of these five patients died. During the same time, 15 patients under warfarin (n =12 with AF) and 25 without anticoagulation (n = 0 with AF) were treated after closed head injury and none of these patients died.[3] Alonso, et al.[15] reported about intracranial haemorrhages in AF patients treated with dabigatran or warfarin by analysing healthcare utilization claims in the Truven Health Marketscan Research Database. They reported that 45 of the 101 dabigatran-treated patients suffered from traumatic haemorrhages but traumatic and nontraumatic intracerebral haemorrhages were not compared regarding haemorrhage subtype, therapy or mortality. Among 11 patients with life-threatening dabigatran-related bleeding events, reported by Ross, et al., [16] four patients had traumatic intracerebral haemorrhages and one of them died.
Neurosurgeons are frequently involved in the management of anticoagulation-related intracerebral hemorrhages. Strategies to reverse VKA comprise fresh frozen plasma, prothrombin complex concentrates, vitamin K, and recombinant activated factor VII. However, reversal of anticoagulation may not always result in good clinical outcome which is probably related to the severity of the initial hemorrhage.[17] As compared with VKA, pharmacologic strategies to reverse dabigatran or other DOACs are lacking and experience is limited mostly to case reports as listed in Table 3. Multiple measures are taken, like in our patient, to reverse the anticoagulant effect of dabigatran. This polypragmatic approach is of limited therapeutic success. Since dabigatran has a low protein binding, elimination by haemodialysis or hemofiltration is a possible therapy, however in trauma-patients this measure is difficult to perform and only applied rarely.[6],[10],[16] In our patient, haemodialysis was not carried out because of the rapid progression of the neurologic deterioration necessitating urgent surgery.
At present, there is no specific antidote available for dabigatran. Idarucizumab, an investigational fully humanized antibody fragment, is under investigation. Data from a, so far unpublished, phase I study showed that idarucizumab was able to achieve immediate, complete and sustained reversal of dabigatran-induced anticoagulation in healthy humans. According to the manufacturer, a global phase III study, RE-VERSE AD™, is under way in patients taking dabigatran who have uncontrolled bleeding or require emergency surgery or procedures.
Frail elderly people, like our patient, were not represented in DOAC-investigating trials due to various exclusion criteria, and only a third of patients in these trials were > 75 years. From RE-LY, a subgroup analysis showed that in patients ≥ 75 years extracranial bleeding risk was higher (4.1%/4.7% per year) under 220/300 mg/d dabigatran vs. 3.4%/year under warfarin.[18] One factor for the increased bleeding risk in elderly patients might be the decreased clearance of dabigatran: dabigatran concentration is increased 1.3-fold in patients aged 65–75 years and 1.7-fold in those ≥ 75 years; these increases correspond to a decreased clearance of 0.66% for each year of age greater than the median age of 68 years.[19]
The risk of falls is the most frequent reason for not prescribing VKAs to elderly patients.[20] In patients aged ≥ 81 years, the risk of non-accidental falls was 2.5 times higher in patients with AF compared to those without.[21] A history of falls is the strongest risk factor for subsequent bleeding events, strokes and all-cause mortality in elderly AF-patients under anticoagulation.[22,[23] The use of DOACs will neither solve the problem of falls nor of fall-associated traumatic bleeding, as illustrated by the presented case.
In conclusion, we suggest withholding anticoagulant therapy in patients with unexplained falls as long as no therapy for their falls has been established. If anticoagulant therapy is deemed necessary, VKA should be preferred over DOACs, as long as no antidotes for DOACs and reliable tests for laboratory monitoring are available.
Acknowledgments
Written informed consent was obtained from the widow of the patient for publication of this case report and any accompanying images. The author(s) declare that they have no competing interests.
References
- 1.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 2.Hart RG, Diener HC, Yang S, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43:1511–1517. doi: 10.1161/STROKEAHA.112.650614. [DOI] [PubMed] [Google Scholar]
- 3.Lok J, Leung W, Murphy S, et al. Intracranial hemorrhage: mechanisms of secondary brain injury. Acta Neurochir. 2011;111(Suppl):S63–S69. doi: 10.1007/978-3-7091-0693-8_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schaefer JH, Leung W, Wu L, et al. Translational insights into traumatic brain injury occurring during dabigatran or warfarin anticoagulation. J Cereb Blood Flow Metab. 2014;34:870–875. doi: 10.1038/jcbfm.2014.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Awad AJ, Walcott BP, Stapleton CJ, et al. Dabigatran, intracranial hemorrhage, and the neurosurgeon. Neurosurg Focus. 2013;34:E7. doi: 10.3171/2013.2.FOCUS1323. [DOI] [PubMed] [Google Scholar]
- 6.Chang DN, Dager WE, Chin AI. Removal of dabigatran by hemodialysis. Am J Kidney Dis. 2013;61:487–489. doi: 10.1053/j.ajkd.2012.08.047. [DOI] [PubMed] [Google Scholar]
- 7.Chen BC, Viny AD, Garlich FM, et al. Hemorrhagic complications associated with dabigatran use. Clin Toxicol (Phila) 2012;50:854–857. doi: 10.3109/15563650.2012.721888. [DOI] [PubMed] [Google Scholar]
- 8.Cotton BA, McCarthy JJ, Holcomb JB. Acutely injured patients on dabigatran. N Engl J Med. 2011;365:2039–2040. doi: 10.1056/NEJMc1111095. [DOI] [PubMed] [Google Scholar]
- 9.Garber ST, Sivakumar W, Schmidt RH. Neurosurgical complications of direct thrombin inhibitors--catastrophic hemorrhage after mild traumatic brain injury in a patient receiving dabigatran. J Neurosurg. 2012;116:1093–1096. doi: 10.3171/2012.2.JNS112132. [DOI] [PubMed] [Google Scholar]
- 10.Joseph B, Ditillo M, Pandit V, et al. Dabigatran therapy. Minor trauma injuries are no longer minor. Am Surg. 2014;80:116–118. [PubMed] [Google Scholar]
- 11.Komori M, Yasaka M, Kokuba K, et al. Intracranial hemorrhage during dabigatran treatment. Circ J. 2014;78:1335–1341. doi: 10.1253/circj.cj-13-1534. [DOI] [PubMed] [Google Scholar]
- 12.Wassef SN, Abel TJ, Grossbach A, et al. Traumatic intracranial hemorrhage in patients taking dabigatran: report of 3 cases and review of the literature. Neurosurgery. 2013;73:E368–E373. doi: 10.1227/01.neu.0000430763.95349.5f. [DOI] [PubMed] [Google Scholar]
- 13.Baraniskin A, Steffens C, Harders A, et al. Impact of pre-hospital antithrombotic medication on the outcome of chronic and acute subdural hematoma. J Neurol Surg A Cent Eur Neurosurg. 2014;75:31–36. doi: 10.1055/s-0032-1325629. [DOI] [PubMed] [Google Scholar]
- 14.Parra MW, Zucker L, Johnson ES, et al. Dabigatran bleed risk with closed head injuries: are we prepared? J Neurosurg. 2013;119:760–765. doi: 10.3171/2013.3.JNS12503. [DOI] [PubMed] [Google Scholar]
- 15.Alonso A, Bengtson LG, MacLehose RF, et al. Intracranial hemorrhage mortality in atrial fibrillation patients treated with dabigatran or warfarin. Stroke. 2014;45:2286–2291. doi: 10.1161/STROKEAHA.114.006016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross B, Miller MA, Ditch K, et al. Clinical experience of life-threateningdabigatran-related bleeding at a large, tertiary care, academic medical center: a case series. J Med Toxicol. 2014;10:223–228. doi: 10.1007/s13181-013-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dowlatshahi D, Butcher KS, Asdaghi N, et al. Poor prognosis in warfarin-associated intracranial hemorrhage despite anticoagulation reversal. Stroke. 2012;43:1812–1817. doi: 10.1161/STROKEAHA.112.652065. [DOI] [PubMed] [Google Scholar]
- 18.Eikelboom JW, Wallentin L, Connolly SJ, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011;123:2363–2372. doi: 10.1161/CIRCULATIONAHA.110.004747. [DOI] [PubMed] [Google Scholar]
- 19.Hunchuck JE, Lake JD. Dabigatran for stroke prevention in all patients with atrial fibrillation? Pharmacotherapy. 2011;31:725–728. doi: 10.1592/phco.31.8.725. [DOI] [PubMed] [Google Scholar]
- 20.Rosenman MB, Baker L, Jing Y, et al. Why is warfarin underused for stroke prevention in atrial fibrillation? A detailed review of electronic medical records. Curr Med Res Opin. 2012;28:1407–1414. doi: 10.1185/03007995.2012.708653. [DOI] [PubMed] [Google Scholar]
- 21.Sanders NA, Ganguly JA, Jetter TL, et al. Atrial fibrillation: an independent risk factor for nonaccidental falls in older patients. Pacing Clin Electrophysiol. 2012;35:973–979. doi: 10.1111/j.1540-8159.2012.03443.x. [DOI] [PubMed] [Google Scholar]
- 22.Banerjee A, Clementy N, Haguenoer K, et al. Prior history of falls and risk of outcomes in atrial fibrillation: The Loire Valley Atrial Fibrillation Project. Am J Med. 2014;127:972–978. doi: 10.1016/j.amjmed.2014.05.035. [DOI] [PubMed] [Google Scholar]
- 23.Poli D, Antonucci E, Testa S, et al. Bleeding risk in very old patients on vitamin K antagonist treatment: results of a prospective collaborative study on elderly patients followed by Italian Centres for Anticoagulation. Circulation. 2011;124:824–829. doi: 10.1161/CIRCULATIONAHA.110.007864. [DOI] [PubMed] [Google Scholar]