Abstract
Objective
To describe levels of perceived lifetime discrimination among young adults and determine its role in understanding this racial/ethnic disparity.
Study design
Data were from the PSD study, a 10yr cohort study following 545 non-Hispanic black (46%) and white initial 5–12 graders. A parent reported highest parental education (PE) level. Perceived lifetime racial discrimination was assessed with the General Ethnic Discrimination Scale and depressive symptoms (DepSx) with the Center for Epidemiological Studies Depression Scale (CESD). Stepped linear and logistic regression analyses assessed the relationships of race/ethnicity, PE, and quintiles of discrimination to DepSx. Stratification by race/ethnicity explored differences in the role of discrimination in explaining the PE-DepSx relationship.
Results
Blacks from professionally educated families had the highest discrimination scores, 1.8 times higher than among their white peers (meanblack=42.1vs. meanwhite=22.8 p<.0001). Higher PE was associated with lower DepSx in all regression models. Race/ethnicity became predictive of DepSx only after adjusting for discrimination, which was strongly associated with DepSx. Stratified analysis suggested discrimination accounted for the relationship of PE to DepSx among whites. Among blacks, accounting for discrimination unmasked a buffering effect of PE.
Conclusions
Higher parent education is protective against depression for white youth. However, for black youth, higher parent education confers both risk and protective effects. The high discrimination among black youth from families with college or professionally-educated parents overwhelms the protective effect of higher parent education.
Keywords: Depression, discrimination, socioeconomic status, race/ethnicity, disparities, adolescence
Depression is an important morbidity, affecting approximately 35 million US adults over their lifetimes and 13.1 to 14.2 million adults annually.1 Young adulthood is a particularly vulnerable time, with 18–29 year olds being the most likely adult age group to experience depression over a 12 month period.1 For many, depression develops during adolescence, and evidence suggests that those diagnosed in their early years go on to experience more severe symptoms as adults.2–4 Thus, research which identifies risk factors for depression during adolescence may not only reduce the prevalence of depression among youth, but may also reduce the later life disease burden associated with this disorder.5
Like many psychological illnesses, the causes of depression are multifactorial, encompassing genetic, biological, behavioral, and social domains.6 One prominent social risk factor for depression is low social status, which can be defined both by socioeconomic status (SES) and by race/ethnicity.7–12 Although correlated with each other, how race and SES interrelate to affect depressive symptoms remains unclear. For example, a correlation between low SES and depression has been demonstrated in a variety of populations but, interestingly not consistently among non-Hispanic blacks.13 Data also suggest that racial and ethnic minorities experience major depressive disorder at lower rates than whites,14–16 despite the fact that these groups face higher levels of socioeconomic adversity.17 We noted higher levels of depressive symptoms among non-Hispanic black and low SES teens.18 However, when race/ethnicity and SES were considered simultaneously, the effect of black race on depressive symptoms was completely attenuated. Furthermore, in stratified analysis, the authors noted a SES gradient in depression only among non-Hispanic white adolescents, suggesting that higher SES was not protective for non-Hispanic black teens.
Some of these inconsistencies in how markers of social disadvantage relate to depression may be explained by perceived discrimination.19–21 Perceived discrimination, which has a significant negative effect on mental and physical health,21–24 is more common among individuals with disadvantaged social status,21 including racial and ethnic minorities.20,21,25–27 In turn, perceived racial discrimination correlates with low psychological well-being among racial and ethnic minority youth.19,28–30 Whether perceived discrimination accounts for some or all of the influence of low SES on depression in adolescence is unknown, as is whether the influence of discrimination is the same across racial/ethnic groups. Although Brody et al showed that high SES non-Hispanic black 5th graders had lower levels of perceived racial discrimination but reported greater increases in discrimination across early adolescence than their lower SES non-Hisapnic black peers,19 to our knowledge, no study has explored if and how perceived discrimination in childhood and adolescence affects the relationships between SES, race, and depression during the transition into adulthood.
The present study addresses this gap in the literature. We extend our work18 and use longitudinal data from the Princeton School District (PSD) Study, a study that followed a socioeconomically diverse, biracial community-based cohort over nine years into young adulthood. Using data from these young adults, we explore the role of perceived discrimination in the relationships among SES, race/ethnicity, and depression. Our objectives are to: (1) describe perceptions of lifetime discrimination in diverse cohort of young adults; (2) explore how these perceptions of lifetime discrimination differ by race/ethnicity and SES; and (3) determine whether perceived lifetime discrimination helps explain racial/ethnic differences in the SES gradient in depression.
METHODS
Data were drawn from Phase 2 of the PSD Study, a longitudinal cohort study of adolescents from a single Midwestern suburban public school district. A detailed description of Phase 1 of the PSD Study (2001–2005) is available elsewhere.31,32 Phase 2, which included two additional waves of data collection in Years 8 and 10, began in May 2008 and enrolled 822 of the 1,207 eligible non-Hispanic black and non-Hispanic white Phase 1 participants (68.1%). Because perceived discrimination was assessed in Year 10, subjects for the current study were drawn from the Year 10 cohort (N=565). Furthermore, because race/ethnicity is a key variable, we restricted eligibility to the 545 Year 10 participants who self-identified as non-Hispanic black and non-Hispanic white (hereafter referred to as “black” and “white,” respectively). Self-identified race/ethnicity was collected in Phase 2, whereas in Phase 1, race/ethnicity had been determined by parental report. Approval for all data collection and procedures for the PSD study and these analyses was received from the Institutional Review Boards at the participating institutions. Continued analyses are approved by the Partners Human Subjects Research Committee.
SES measures were obtained at baseline through a parental survey. All other measures were obtained from a survey completed by the adolescent/young adult PSD Study participant at a study visit. SES is made up of multiple dimensions, including education, income, and occupation.33 The PSD Study included assessment of both parent education and household income in Year 1. In this study, although we include household income in our analyses, we focus on parent education as our sentinel measure of SES because parent education is usually stable across adolescence, and household income can fluctuate from year to year. This is particularly relevant because Phase 2 of the PSD Study began during the second year of the Great Recession in the US. In the baseline parent survey, the parent reported his/her current education level as well as his/her spouse/current partner’s education level. For analyses, responses were collapsed into four categories reflecting the highest level of parental education: E1= ≤ high school or GED; E2= some college or vocational training; E3= college graduate; and E4= professional degree. The parent also reported current household pre-tax income from all sources by selecting a response from nine ordered options (<$5000 to ≥$100,000). Ranges of these response options varied, so the midpoints of each range were used in analyses and $150,000 was used for the ≥$100,000 category. Household income was imputed in cases of missing data using multiple imputation based upon parent education and race.31
Perceived racial discrimination was measured at Year 10 using the Perceived Lifetime Discrimination subscale of the General Ethnic Discrimination Scale (GED).34 The GED, which was developed to be consistent with a stress-coping paradigm, assesses the frequency and appraised severity of 18 discriminatory experiences (e.g., “How often have you been treated unfairly by strangers…”). These 18 items were adapted from the Schedule of Racist Events, a scale designed for use in black samples.35 In contrast, the GED was designed for use with any ethnic group in university and community settings and has been shown to have high reliability (≥0.91) and to adequately differentiate across racial/ethnic groups.34 The GED has three unidimensional subscales – recent (past year) discrimination, lifetime discrimination, and appraised discrimination.34 In this study, we used the perceived lifetime discrimination subscale, which asked participants to indicate how often the experiences occurred in their “entire life.” Because these participants were young adults, perceived lifetime racial discrimination represents a measure of discrimination during childhood and adolescence. Hereafter, we refer to perceived lifetime racial discrimination as “discrimination.” Of note, when the PSD Study began in 2001, little was known about perceived discrimination in children and adolescents and there were no validated measures for use in 7–12th graders.23 Sex and race/ethnicity were identified by self report. Age was calculated as the date of survey completion minus the participant’s date of birth.
Depressive symptoms were measured at baseline (adolescence) and Year 10 (young adulthood) by the 20-item Center for Epidemiological Studies Depression Scale (CESD). The CESD was developed to measure symptoms of depression within the community among both adolescents and young adults.35 It is a valid and reliable measure with good internal consistency and test-retest reliability that distinguishes well between psychiatric inpatients and those in the general population and between people who report they need help for emotional problems and those who report they do not.36 Although not indicative of a diagnosis of clinical depression, scores of 16 or higher are have been shown to identify major depressive disorder in adults36 and scores of 22 for males and 24 for females suggest major depressive disorder in adolescence.37 We refer to scores above these cut points as “high depressive symptoms” or “HDS.”
Statistical analyses
Analyses were conducted in SAS version 9.3 (Cary, NC). We first performed univariate analyses to describe the distribution of the factors of interest. We then evaluated the relationships of race/ethnicity and SES to discrimination and examined bivariate associations of covariates to depressive symptoms in young adulthood. Next, multivariable analyses were used to assess the impact of SES, race/ethnicity, and discrimination to depressive symptoms in young adulthood. Because these 545 individuals came from 469 families, 11.5% of which had two siblings and 2.3% of which had three siblings in the study, multivariable models were run using generalized estimating equations via PROC GENMOD to account for this family clustering. Due to the non-normal distribution of the GED scale, we categorized the scale into quintiles for the multivariable analyses.
Depressive symptoms were first modeled as a continuous variable, using CESD scores as the outcome, in order to assess symptomatology. Because CESD scores were not normally distributed, we explored using square-root transformed and log-transformed CESD scores, in addition to raw CESD scores in regression modeling. Analyses of all three yielded similar results (data available upon request). For ease of interpretation, we present the results from models using the non-transformed, raw CESD scores. To explore associations with the more pathological end of the symptomatology spectrum, we also performed regression analyses with the dichotomized HDS variable as the outcome. These analyses used the logit link function to estimate the odds of reporting HDS.
Three models were run for both the continuous and the dichotomized outcomes. The first model examined the associations of parent education and race/ethnicity to depressive symptoms. The second model added discrimination (quintiles). Model 3 included baseline depressive symptoms for the continuous outcome and baseline HDS for the dichotomized outcome. Because prior work had suggested effect modification by race/ethnicity,18 the multivariable analyses were also stratified by race/ethnicity. Testing to assess if discrimination mediated the relationship of parent education to depressive symptoms was performed only on the race/ethnicity stratified models. The mediation testing used bootstrapping procedures (N=1,000) and was operationalized in an SAS macro developed by Preacher and Hayes for estimating direct and indirect effects.38 Parent education was used as an ordinal variable in these mediation analyses. All multivariable models adjusted for sex, age, and household income. For Model 3, which adjusted for baseline depressive symptoms, baseline age and length of follow up were included instead of Year 10 age, which was used in Models 1–2.
RESULTS
Sample characteristics are presented in Table I. The median discrimination score was 26 and 11.9% of the sample reported HDS in adolescence. With regard to racial disparities, blacks had lower parental education levels, lower family household income levels, and higher discrimination scores than whites. Black adolescents also reported more depressive symptoms than white adolescents, but there was no racial/ethnic difference in the baseline prevalence of HDS.
Table 1.
Description of the study sample and associations of race/ethnicity to covariates
| Total (N=545) |
Black (N=249) |
White (N=296) |
p-value | |
|---|---|---|---|---|
| % | % | % | ||
| Sex | 0.88 | |||
| Male | 41.8 | 42.2 | 41.6 | |
| Female | 58.2 | 57.8 | 58.4 | |
| Highest Parent Education | <.0001 | |||
| High school, GED, or less | 18.5 | 26.1 | 12.2 | |
| Some College | 27.5 | 35.7 | 20.6 | |
| College Graduate | 30.8 | 28.9 | 32.4 | |
| Professional Degree | 23.1 | 9.2 | 34.8 | |
| High Depressive Symptoms in Adolescence | 11.9 | 13.3 | 10.8 | 0.38 |
| Med (IQR) | Med (IQR) | Med (IQR) | ||
| Age, years | ||||
| Baseline (Adolescence) | 14.3 (13.1–16.0) | 14.2 (13.1–15.8) | 14.4 (13.2–16.1) | 0.30 |
| Year 10 (Young Adulthood) | 23.5 (21.6–25.3) | 23.3 (21.5–25.1) | 23.6 (21.9–25.5) | 0.11 |
| Length of Follow-up, years | 9.0 (8.7–9.4) | 9.4 (9.0–9.4) | 9.1 (8.7–9.5) | 0.02 |
| Household Income ($1000) | 62.5 (30.0–87.5) | 30.0 (20.5–62.5) | 87.5 (62.5–150.0) | <.0001 |
| CESD Score in Adolescence | 13.0 (7.0–18.0) | 13.0 (8.0–18.0) | 12.0 (7.0–17.0) | 0.02 |
| Discrimination | 26.0 (20.0–36.0) | 35.0 (26.0–42.0) | 22.0 (19.0–28.0) | <.0001 |
Note. CESD, Center for Epidemiological Studies Depression Scale; Med, median; IQR, inner quartile range. High depressive symptoms were defined by CESD scores ≥22 for males and ≥24 for females in adolescence and ≥16 in young adulthood. Percentages may not sum to 100 due to rounding.
Race and SES differences in discrimination
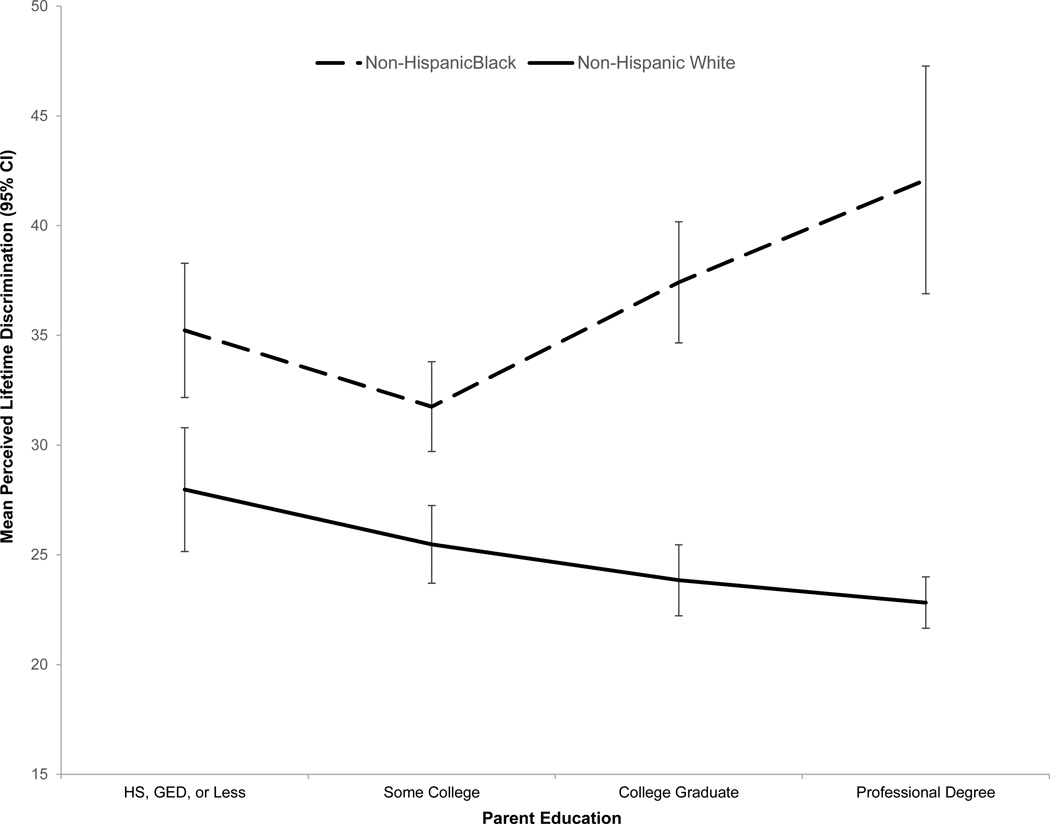
The relationships among parent education, race/ethnicity, and discrimination were complex and suggested a race/ethnicity by parent education interaction (Figure). Discrimination scores were higher among blacks than whites across all levels of parental education. However, even though there was a simple inverse gradient between parent education and discrimination among whites, among blacks this relationship was j-shaped, with elevated discrimination scores at both low and high levels of parental education (p<.0001). In fact, discrimination was highest amongst blacks from the highest educated families. For young adults whose parent(s) had at least a professional degree, mean discrimination scores were 1.8 times higher (mean=42.1, SD=12.0) than their white peers from similarly educated families (mean=22.8, SD=5.9) and 1.2 times higher than black youth from families with the lowest level of parent education (mean=35.2, SD=12.3).
Figure. The Relationship of Perceived Lifetime Discrimination and Parental Education by Race/Ethnicity.
Mean perceived lifetime discrimination and 95% confidence intervals for each level of parent education are shown by race/ethnicity. The solid line represents non-Hispanic whites and the dashed line non-Hispanic blacks.
Determinants of depressive symptoms in young adulthood
Table II presents bivariate relationships between sex, race/ethnicity, SES, and discrimination to depressive symptoms in young adulthood, both as the continuous CESD score and dichotomized as HDS. Overall, the median CESD score in young adulthood was 9, well below the cut point of 16 for HDS. However, more than one quarter (25.9%) had HDS. As expected, on average, CESD scores declined from adolescence to young adulthood (Wilcoxon signed rank p<0.001). Those with HDS in adolescence were more likely to have HDS in young adulthood (55.4% baseline HDS versus 25.4% baseline non-HDS; McNemar’s p<0.001).. CESD scores were higher among young women, blacks, and those with lower parent education and household income levels. These same associations were found when assessing the dichotomized HDS outcome. Of note, CESD and discrimination scores were positively correlated (r=0.30; p<.0001) and discrimination scores were higher among those with HDS than those without.
Table 2.
Associations of sex, race/ethnicity, SES, and discrimination to depressive symptoms
| CESD Scores | High Depressive Symptoms | ||||
|---|---|---|---|---|---|
| p-value | Yes | No | p-value | ||
| Med (IQR) | % | % | |||
| Total | 9.0 (5.0–17.0) | 25.9 | 74.1 | ||
| Mean (SD) | |||||
| Sex | 0.003 | 0.004 | |||
| Male | 10.9 (8.6) | 32.3 | 45.7 | ||
| Female | 13.3 (9.8) | 67.7 | 54.3 | ||
| Race/ethnicity | 0.03 | 0.04 | |||
| Black | 13.2 (9.2) | 52.5 | 42.9 | ||
| White | 11.5 (9.5) | 47.5 | 57.1 | ||
| Highest Parent Education | <.0001 | 0.003 | |||
| High school, GED, or less | 15.1 (9.7) | 25.3 | 15.8 | ||
| Some college | 13.2 (9.3) | 31.0 | 26.1 | ||
| College graduate | 12.2 (9.7) | 29.1 | 31.5 | ||
| Professional degree | 9.0 (7.8) | 14.6 | 26.6 | ||
| Spearman Rho | Med (IQR) | Med (IQR) | |||
| Household Income ($1000) | −0.17 | <.0001 | 62.5 (30.0–87.5) | 62.5 (30.0–87.8) | 0.68 |
| Discrimination | 0.30 | <.0001 | 34.0 (22.0–41.0) | 25.0 (19.0–33.0) | <.0001 |
Note. CESD, Center for Epidemiological Studies Depression Scale; Med, median; IQR, inner quartile range. High depressive symptoms were defined by CESD score ≥16. Percentages may not sum to 100 due to rounding.
Multivariable analyses are presented in Table III. In the whole sample, lower parent education, but not race/ethnicity was associated with both higher CESD scores and increased odds of HDS in Model 1. Inclusion of discrimination in Model 2 showed it to be a strong determinant of depressive symptoms, one that did not affect the relationship between parental education and depressive symptoms. However, inclusion of discrimination in the model caused race/ethnicity to become a significant determinant of CESD scores but not HDS. In Model 2, black race/ethnicity was associated with lower depressive symptoms (β= −2.45, SE=0.91). These associations were largely unaffected by adjusting for CESD scores in adolescence (Model 3), which was, itself, a strong independent predictor of both higher CESD scores (β=0.31, SE=0.04) and HDS (AOR 3.11; 95% CI: 1.77–5.46) in young adulthood.
Table 3.
Results from a series of multivariable general linear and logistic models assessing if race/ethnicity, parent education, and discrimination predict depressive symptoms
| Outcome = CESD Scores | Outcome = High Depressive Symptoms | |||||
|---|---|---|---|---|---|---|
| Model 1 Beta (SE) |
Model 2 Beta (SE) |
Model 3 Beta (SE) |
Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
|
| Whole Sample (N=545) | ||||||
| Black Race/ethnicity | 0.35 (0.89) | −2.45 (0.91)** | −2.22 (0.86)** | 1.19 (0.77 – 1.83) | 0.69 (0.43 – 1.12) | 0.72 (0.44–1.16) |
| Highest Parent Education | ||||||
| High School, GED, or Less | 5.97 (1.53)*** | 5.49 (1.50)*** | 5.48 (1.45)*** | 2.76 (1.32–5.76)*** | 2.58 (1.22–5.45)** | 3.08 (1..43–6.65)** |
| Some College | 3.78 (1.32)** | 3.85 (1.26)** | 3.80 (1.18)** | 1.92 (0.97–3.81) | 2.00 (1.01–3.99)* | 2.33 (1.16–4.67)** |
| College Graduate | 2.98 (1.18)** | 2.78 (1.13)** | 2.48 (1.10)* | 1.54 (0.84–2.81) | 1.49 (0.81–2.74) | 1.55 (0.83–2.90) |
| Discrimination (quintiles) | 1.95 (0.29)*** | 1.59 (0.29)*** | 1.50 (1.28–1.77)*** | 1.45 (1.24–1.71)*** | ||
| CESD in Adolescence | 0.31 (0.04)*** | 3.11 (1.77–5.46)*** | ||||
| Blacks (N=249) | ||||||
| Highest Parent Education | ||||||
| High school, GED, or less | 7.03 (2.65)** | 8.59 (2.53)*** | 9.61 (2.36)*** | 3.97 (1.03–15.23)* | 5.73 (1.44–22.72)** | 8.40 (1.98–35.59)** |
| Some college | 4.39 (2.36) | 6.38 (2.31)** | 7.31 (2.09)*** | 2.72 (0.75–9.91) | 4.26 (1.12–16.23)* | 6.44 (1.64–25.22)** |
| College graduate | 3.89 (2.19) | 1.87 (2.09)* | 4.75 (1.90)** | 2.56 (0.76–8.64) | 3.31 (0.97–11.30) | 4.13 (1.18–14.42)* |
| Discrimination (quintiles) | 2.15 (0.45)*** | 2.25 (0.54)*** | 1.54 (1.19–1.99)*** | 1.61 (1.19–2.16)** | ||
| CESD in Adolescence | 0.33 (0.07)*** | 3.50 (1.42–8.62)** | ||||
| Whites (N=296) | ||||||
| Highest Parent Education | ||||||
| High school, GED, or less | 4.67 (2.05)* | 3.43 (2.09) | 3.11 (1.97) | 2.28 (0.84–6.18) | 1.74 (0.62–4.88) | 2.03 (0.73–5.64) |
| Some college | 3.70 (1.63)* | 3.15 (1.56) | 3.04 (1.48) | 1.81 (0.78–4.21) | 1.62 (0.70–3.75) | 1.84 (0.79–4.26) |
| College graduate | 2.01 (1.43) | 1.93 (1.37) | 1.84 (1.33) | 1.08 (0.51–2.26) | 1.00 (0.47–2.13) | 1.06 (0.49–2.30) |
| Discrimination (quintiles) | 1.79 (0.41)*** | 1.50 (0.39)*** | 1.50 (1.20–1.87)*** | 1.45 (1.16–1.81)*** | ||
| CESD in Adolescence | 0.29 (0.06)*** | 2.99 (1.34–6.69)*** | ||||
Note. CESD, Center for Epidemiological Studies Depression Scale; SE, standard error; OR, odds ratio; CI, confidence interval. The reference category for highest parental education is professional degree. Models 1 and 2 additionally adjust for sex, age, and household income. Model 3 adjusts for sex, household income, baseline age, and length of follow up. CESD in adolescence is operationalized using baseline CESD scores for the CESD Score outcome model and baseline CESD dichotomized at ≥22 for males and ≥24 for females for the model predicting high depressive symptoms.
p≤.001;
p≤.01;
p≤.05.
Based on our a priori hypothesis, we also performed parallel race/ethnicity stratified multivariable analyses to explore racial/ethnic differences in the role of discrimination in explaining parent education’s impact on depressive symptoms in young adulthood (Table III). Among blacks, an inverse gradient between parent education and CESD was revealed with the adjustment for discrimination (Model 2), and for whites, adjusting for discrimination caused parent education to become non-significant, suggesting mediation. Mediation testing revealed that discrimination accounted for 32.3% of the effect of parental education on CESD scores among whites (Table IV; available at www.jpeds.com). Among both blacks and whites, discrimination was strongly associated with depressive symptoms, whether measured as continuous CESD scores or HDS. The magnitude of effect seemed stronger for blacks than whites. Each additional quintile increase in the discrimination scale resulted in 61% and 45% greater odds of HDS and a 2.25 (SE=0.54) and 1.50 (SE=0.39) point increase in CESD scores for blacks and whites, respectively.
DISCUSSION
In this study we found that perceived lifetime racial discrimination was associated with depressive symptoms regardless of race/ethnicity. We also found that the relationship of parent education to perceived discrimination differed by race/ethnicity. The relationship was a simple inverse gradient for whites but for blacks, the relationship was j-shaped. Black young adults from highly educated families reported the highest levels of discrimination in this cohort, 1.8 times higher than their white counterparts and 1.2 times higher than discrimination reported by blacks from families with low parent education. Furthermore, we demonstrated that the markedly increased levels of discrimination reported by black young adults from the most educated families overwhelmed the protective effect of higher parent education on depressive symptoms. Thus, even though higher parent education was protective against depression for white young adults, among blacks, higher parent education conferred both risk and protective effects.
Our findings align with studies documenting the protective effect of high SES10,12 and the harmful effect of discrimination22 on mental health and well-being, and also provide new insight into the linkages among SES, race/ethnicity, and health. To date, the evidence for the presence and direction of racial/ethnic disparities in depressive symptoms during adolescence, particularly black-white differences, has been mixed, as has evidence for the relationships of SES markers to depression in adolescence and young adulthood. Higher levels of discrimination have been found among individuals with disadvantaged social status,21 including racial and ethnic minorities,21,25,26,29,30,39 and have also been shown to have an inverse relationship with mental health.22 However, to our knowledge, no prior study has documented the high levels of discrimination among black young adults from highly educated families that we demonstrated here. In addition, despite the well-established inverse relationship between SES and depression,10 research has not found a consistent inverse relationship between SES and depression among racial/ethnic minorities.40 Being in a lower status racial/ethnic group is often collinear with lower SES and one might expect that racial/ethnic minorities suffer double disadvantage to health due to the interactive effects of low SES and race. However, evidence shows that higher SES confers less health benefit to blacks than whites. This “diminishing returns” hypothesis41 has been supported in previous research on depression among racial/ethnic minorities.16,18,42 Our study implicates discrimination as a key contributor to these findings. Our data suggest that among blacks, the inverse association between higher SES and lower depressive symptoms may be masked by the simultaneous association of higher SES with discrimination. The implication is that higher SES does not afford the same protective mental health benefit for blacks as whites due to the deleterious effects of discrimination.
Perceived discrimination has been conceptualized as a social stressor that negatively affects health through both psychological and behavioral responses.22,43 Across racial and ethnic groups, experiences of discrimination may decrease an individual’s self-control resources, leading to maladaptive health behaviors, such as smoking, and alcohol and substance use that ultimately increase the risk for poor health outcomes.22 High SES minorities may be especially sensitive to poor mental health outcomes because they feel socially ostracized and/or lack strong social support networks to buffer the negative impacts of discrimination. With higher levels of SES, racial-ethnic minority groups members may be more stigmatized or more aware of the social and economic inequalities they face despite their economic achievements,41 which in turn fosters depressive symptoms. Chronic awareness of social stigma may also increase an individual’s vigilance regarding discriminatory experiences and, in turn, the number of times discrimination is perceived.22,41,44 Regardless of the mechanism, our findings highlight the need to consider the role of perceived discrimination when examining the intersections of race/ethnicity and SES with health.
Our results suggest that preventing the causes and effects of perceived discrimination should be a priority in reducing rates adolescent depression. Research and practice efforts should recognize that although blacks are 40% less likely than whites to experience depression during their lifetime,45 the strikingly high rate of discrimination among upper SES black young adults suggest that they are a particularly vulnerable group. Strategies targeting social support, coping skills (e.g., confrontation, positive reappraisal), and adverse health behaviors have been shown to be effective in forestalling the negative consequences of discrimination on health22 and may be particularly important for high SES black youth. Future research is needed to examine these mechanisms and their impact on reducing depression in this subgroup.
We acknowledge several limitations to this study. First, our sample was limited to non-Hispanic blacks and whites and did not include other racial/ethnic groups. This reflected the sociodemographics of the area when the cohort was incepted. We also were not able to determine whether those who identified as “black or African American” were US born African-Americans or were from other countries such as the West Indies/Caribbean or were immigrant Africans. SES was assessed at baseline, so we cannot determine if parent education changed during the follow up period. Finally, the relatively small sample may have limited our ability to detect significant effects, particularly in stratified analyses. Future work should replicate our findings in a larger sample.
Despite these limitations, this study has several key strengths. The depression and discrimination measures are well-validated instruments with strong construct validity across racial/ethnic groups. At the time of this study, the GED was the only discrimination scale developed for use among multiple minority groups,34 which strengthens this investigation of the role of discrimination in racial/ethnic health disparities. Further, our data come from a diverse community-based cohort. We also accounted for age and length of follow up, a notable contribution over previous cross-sectional reports.
In conclusion, our results suggest that the high level of discrimination associated with high parent education among black youth may be a mechanism underlying the ‘diminishing returns’ hypothesis. Targeting the causes and effects of discrimination may help ensure that blacks benefit from same health advantages of high SES as their white peers and should be a priority for researchers, clinicians, and policy makers serving young adults. Future research investigating other cultural and social factors that racial/ethnic minorities experience throughout the lifecourse is needed to inform the development of programs and policies that address the unique social stressors that blacks encounter across all levels of SES. Interventions developed to address perceived discrimination may be one promising avenue to reduce mental health disparities and mitigate effects of inequality on mental health.
Supplementary Material
Acknowledgments
Supported by the National Institutes of Health (HD041527 and DK59183) and the William T Grant Foundation (grant #2151). The authors have no conflicts to declare.
Abbreviations
- SES
socioeconomic status
- PE
parent education
- CESD
Center for Epidemiological Studies Depression Scale
- IQR
inner quartile range
- US
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. J Amer Acad Child Adolesc Psych. 1999;38:56–63. doi: 10.1097/00004583-199901000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, et al. Children with prepubertal-onset major depressive disorder and anxiety grown up. Arch Gen Psych. 1999;56:794–801. doi: 10.1001/archpsyc.56.9.794. [DOI] [PubMed] [Google Scholar]
- 4.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Amer Acad Child Adolesc Psych. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psych. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 6.Petersen AC, Compas BE, Brooks-Gunn J, Stemmler M, Ey S, Grant KE. Depression in adolescence. The American Psychologist. 1993;48:155–168. doi: 10.1037//0003-066x.48.2.155. [DOI] [PubMed] [Google Scholar]
- 7.Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med. 2004;158:760–765. doi: 10.1001/archpedi.158.8.760. [DOI] [PubMed] [Google Scholar]
- 8.Gore S, Aseltine RH, Jr, Colton ME. Social structure, life stress and depressive symptoms in a high school-aged population. J Health Soc Behav. 1992;33:97–113. [PubMed] [Google Scholar]
- 9.Rao U, Chen LA. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues in clinical neuroscience. 2009;11:45–62. doi: 10.31887/DCNS.2009.11.1/urao. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents' health. Am J Pub Health. 1999;89:1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kennard BD, Stewart SM, Hughes JL, Patel PG, Emslie GJ. Cognitions and depressive symptoms among ethnic minority adolescents. Cultural diversity & ethnic minority psychology. 2006;12:578–591. doi: 10.1037/1099-9809.12.3.578. [DOI] [PubMed] [Google Scholar]
- 12.Goodman E, Slap GB, Huang B. The public health impact of socioeconomic status on adolescent depression and obesity. Am J Pub Health. 2003;93:1844–1850. doi: 10.2105/ajph.93.11.1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gavin AR, Walton E, Chae DH, Alegria M, Jackson JS, Takeuchi D. The associations between socioeconomic status and major depressive disorder among Blacks, Latinos, Asians and non-Hispanic Whites: findings from the Collaborative Psychiatric Epidemiology Studies. Psychological Medicine. 2010;40:51–61. doi: 10.1017/S0033291709006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, et al. Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psych. 2002;59:893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- 15.Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. American journal of public health. 2005;95:998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawachi I, Daniels N, Robinson DE. Health disparities by race and class: why both matter. Health Affairs. 2005;24:343–352. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- 18.Jackson B, Goodman E. Low social status markers: Do they predict depressive symptoms in adolescence? Race and Social Problems. 2011;3:119–128. doi: 10.1007/s12552-011-9047-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brody GH, Chen YF, Murry VM, Ge X, Simons RL, Gibbons FX, et al. Perceived discrimination and the adjustment of African American youths: a five-year longitudinal analysis with contextual moderation effects. Child Dev. 2006;77:1170–1189. doi: 10.1111/j.1467-8624.2006.00927.x. [DOI] [PubMed] [Google Scholar]
- 20.Garcia Coll C, Lamberty G, Jenkins R, McAdoo HP, Crnic K, Wasik BH, et al. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996;67:1891–1914. [PubMed] [Google Scholar]
- 21.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 22.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psych Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pachter LM, Coll CG. Racism and child health: a review of the literature and future directions. J Dev Bahav Pediatr. 2009;30:255–263. doi: 10.1097/DBP.0b013e3181a7ed5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older blacks and whites. Journal Aging and Health. 2004;16:315–337. doi: 10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]
- 26.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Pachter LM, Bernstein BA, Szalacha LA, Garcia Coll C. Perceived racism and discrimination in children and youths: an exploratory study. Health & Social Work. 2010;35:61–69. doi: 10.1093/hsw/35.1.61. [DOI] [PubMed] [Google Scholar]
- 28.Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: patterns and psychological correlates. Developmental psychology. 2006;42:218–236. doi: 10.1037/0012-1649.42.2.218. [DOI] [PubMed] [Google Scholar]
- 29.English D, Lambert SF, Ialongo NS. Longitudinal associations between experienced racial discrimination and depressive symptoms in African American adolescents. Developmental psychology. 2014;50:1190–1196. doi: 10.1037/a0034703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith-Bynum MA, Lambert SF, English D, Ialongo NS. Associations between trajectories of perceived racial discrimination and psychological symptoms among African American adolescents. Development and Psychopathology. 2014:1–17. doi: 10.1017/S0954579414000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obesity Research. 2003;11:1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- 32.Dolan LM, Bean J, D'Alessio D, Cohen RM, Morrison JA, Goodman E, et al. Frequency of abnormal carbohydrate metabolism and diabetes in a population-based screening of adolescents. J Pediatr. 2005;146:751–758. doi: 10.1016/j.jpeds.2005.01.045. [DOI] [PubMed] [Google Scholar]
- 33.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Ann Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 34.Landrine H, Klonoff EA, Corral I, Fernandez S, Roesch S. Conceptualizing and measuring ethnic discrimination in health research. J Behav Med. 2006;29:79–94. doi: 10.1007/s10865-005-9029-0. [DOI] [PubMed] [Google Scholar]
- 35.Landrine H, Klonoff EA. The schedule of racist events: A measure of racial discrimination and a study of its negative physical and mental health consequences. J Black Psychol. 1996;22(2):144–168. [Google Scholar]
- 36.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 37.Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. J Amer Acad Child Adolesc Psych. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 39.English D, Lambert SF, Evans MK, Zonderman AB. Neighborhood racial composition, racial discrimination, and depressive symptoms in African Americans. Amer J Community Psychology. 2014 doi: 10.1007/s10464-014-9666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: a review. Clinical Psychology Review. 2010;30:338–348. doi: 10.1016/j.cpr.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 41.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 42.Hudson DL, Neighbors HW, Geronimus AT, Jackson JS. The relationship between socioeconomic position and depression among a US nationally representative sample of African Americans. Social Psychiatry Psychiatric Epi. 2012;47:373–381. doi: 10.1007/s00127-011-0348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Major B, Gramzow RH, McCoy SK, Levin S, Schmader T, Sidanius J. Perceiving personal discrimination: the role of group status and legitimizing ideology. Journal of personality and social psychology. 2002;82:269–282. [PubMed] [Google Scholar]
- 44.Pinel EC. Stigma consciousness in intergroup contexts: The power of conviction. J Exp Soc Psychol. 2002;38:178–185. [Google Scholar]
- 45.Pinel EC. Stigma consciousness in intergroup contexts: The power of conviction. J Exp Soc Psychol. 2002;38:178–185. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.