Abstract
Objectives
To assess the joint effects of water and sanitation infrastructure, whether they are redundant services preventing the same cases of diarrheal disease, act independently, or act synergistically; and to assess how these effects vary by country and over time.
Methods
We used data from 217 Demographic and Health Surveys conducted in 90 countries between 1986 and 2013. We used modified Poisson regression to assess the impact of water and sanitation infra-structure on the prevalence of diarrhea among children under five.
Results
The impact of water and sanitation varied across surveys, and adjusting for socioeconomic status drove these estimates towards the null. Sanitation had a greater effect than water infrastructure when all 217 surveys were pooled; however, the impact of sanitation diminished over time. Based on survey data from the past ten years, we saw no evidence for benefits in improving drinking water or sanitation alone, but we estimated a 6% reduction of both combined (prevalence ratio = 0.94, 95% confidence limit 0.91-0.98).
Conclusions
Water and sanitation interventions should be combined to maximize the number of cases of diarrheal disease prevented in children under five. Further research should identify the sources of variability seen between countries and across time. These national surveys likely include substantial measurement error in the categorization of water and sanitation, making it difficult to interpret the roles of other pathways.
Keywords: Cross Sectional analysis, Demographic and Health Surveys, Diarrhea, Interaction, Sanitation, Water
Introduction
Diarrheal diseases are a leading cause of death in children under five in developing countries worldwide (1), accounting for over 700,000 child deaths in 2011 (2). The frequency of diarrheal diseases in developing countries is largely attributed to a lack of clean water and adequate sanitation (3). While the network of water quality, human waste disposal, health status, and disease transmission has been meticulously documented and is widely understood (4, 5), the joint effects of multiple interventions in preventing disease are not well understood.
Four key studies have investigated the interaction between water and sanitation services. Esrey (6) used cross-sectional data from 8 Demographic and Health Surveys (DHS) to show that 1) improved water supply had no meaningful effect on health if improved sanitation was not concurrent and 2) larger impacts were seen with both interventions than the improvements to water or sanitation alone. In a cohort study among Filipino infants, VanDerslice and Briscoe (7) reported that improved water was most protective when a community had better sanitation. Similarly, a meta-analysis by Gundry et al. (8) showed that the protective effect of improved water interventions was stronger when a greater proportion of households had access to improved sanitation. Finally, mathematical modelling suggests that water quality improvements may have little to no impact when sanitation conditions are poor (9). The different conclusions in these four studies may be the result of differences in underlying contextual factors, such as social and environmental conditions. Improved sanitation infrastructure may have a greater impact on diarrheal disease than improved water infrastructure (6, 10). However, the extent of the impact from these facilities has varied, possibly because of context.
Extending upon this work, as well as a prior DHS analysis that examined water and sanitation benefits separately (10), we used data from 217 DHS to examine both the independent and joint effects of improved water and sanitation. We also examined whether these effects vary geographically (such as between countries), over time, or between rural and urban areas. These standardized surveys provide the opportunity to address these questions on a large scale.
Methods
We used data from DHS surveys completed between 1986 and 2013. These are country-specific surveys on population demographics and health that have been conducted in over 90 developing countries using standardized household questionnaires. In some instances, we included only surveys that were completed in the past 10 years (2003-2013), and when a country had multiple surveys in the past 10 years, we used only the most recent. This selection was based on the desire to achieve a balance between using a dataset that is most relevant to current conditions, having a sufficient sample size to conduct our analysis, and preventing some countries from being overrepresented. These surveys typically employ a two-stage sampling strategy wherein a country is divided into enumeration areas (clusters), and then households are randomly selected within each cluster. Other household surveys, such as the Multiple Indicator Cluster Surveys, were considered. However, we opted to limit our analysis to DHS surveys in order to limit differences in survey methodology.
Household characteristics, demographics, and health information were obtained from eligible women ages 15-49 in each household surveyed, although in some countries, only ever-married women (age 15-49) were interviewed. Childhood diarrhea was ascertained by asking mothers whether each child under five years of age in the household had experienced diarrhea in the two weeks preceding the interview.
Water and sanitation sources for each household were measured by asking the respondent about the “main source of drinking water” and the “kind of toilet facilities” that were used by household members. We then classified sanitation facilities and sources of drinking water as being either improved or unimproved using the classification system of the Joint Monitoring Programme (JMP) for Water and Sanitation (11): (1) improved water sources were defined as a protected spring, protected well, tubewell or borehole, public tap, piped water to yard, piped water into dwelling or rainwater; (2) unimproved water sources were defined as an unprotected spring or well, tanker truck or bottled water, or surface water; (3) an improved sanitation facility was defined as a sewer system, flush toilet (or pour-flush toilet to pit latrine, septic tank, or to an unknown location), septic tank, composting toilet, ventilated improved pit latrine, or pit latrine with a slab; and (4) an unimproved sanitation facility was defined as a flush or pour flush to elsewhere (i.e., open gutter), hanging toilet or hanging latrine, pit latrine without a slab, bucket, bush, field or no facilities. To assess the independent and joint effects of improved water and improved sanitation, we classified households in the following way: (1) uses unimproved water and unimproved sanitation (neither improved); (2) uses improved water and unimproved sanitation (improved water only); (3) uses unimproved water and improved sanitation (improved sanitation only), and (4) uses improved water and improved sanitation (both improved).
Several potential confounders were included in the analysis. For each survey, a socioeconomic status (SES) index was constructed using principal components analysis (12) of the mother’s age and education, household asset ownership (cooking fuel, floor material, electricity, radio, television, refrigerator, bicycle, motorcycle or scooter, and a car or truck), the highest education level in the household, and whether or not the child had a health card. Within each survey, SES quintiles were derived based on the index. Many DHS datasets include a wealth index/quintile variable; however, we chose to create our own since those provided by the DHS typically included drinking water source and sanitation facilities in the index. In addition to the SES index, we adjusted for the child’s age in years, the child’s sex (female versus male), and whether the household was in an urban or rural area.
Modified Poisson regression, accounting for complex sampling, was used to estimate unadjusted and adjusted prevalence ratios (PR) and 95% confidence limits (95%CL) for the prevalence of diarrhea in children under five years of age. We first estimate these PRs for each specific survey. For the pooled analyses, data from multiple surveys were combined, and a single model was used which included a fixed effect for each survey (survey dummies). To test for longitudinal trends, we first ran a pooled model for each year, which included all surveys conducted during that year, the year previous, or the following year. To highlight within country time trends, we used a multilevel linear regression with the log PR of each survey as the dependent variable and year as a continuous predictor. These models also included a random intercept and slope for each country. All statistical analysis was conducted using STATA 11.2 (StataCorp LP, College Station, TX).
For assessing interaction, we determined whether the observed joint effect of both water and sanitation together was greater than, equal to, or less than the expected joint effect (13, 14). For multiplicative interaction, the expected joint effect is the product of the two independent effects (PR11 = PR10 * PR01). For additive interaction, the expected joint effect is the sum of the two independent effects minus one (PR11 = PR10 + PR01 - 1). The 95% CL for the expected joint effect was calculated using the delta method (15). A synergistic interaction would be evident if the observed joint effect of both exposures exceeds the expected effect. This implies that the effect of one exposure is greater in the presence of the other. If, however, the observed effect is equal to the expected effect, then the two exposures are likely independent; the effect of each does not depend on the presence of the other. Another possible outcome is some form of antagonism, where the observed joint effect is less than the expected effect, suggesting that the effect of each exposure is diminished in the presence of the other. This implies that the two exposures are acting on the same pathway and preventing the same cases.
Results
Survey Specific Results
217 surveys from 74 countries had data on diarrhea, source of drinking water, sanitation facility, and necessary covariates (data by country and survey year can be seen in Table S1). The prevalence of diarrhea among children <5 years of age ranged from 4.4% (Maldives, 2009) to 39.6% (Senegal,1986), and the median across surveys was 16.1%. Coverage of improved water and sanitation services also varied across countries. For example, in 37 surveys, many from African countries, showed that >50% of children lived in households lacking access to both improved water and sanitation, whereas in 50 surveys >50% of children had access to both services.
The effect of improved drinking water varied substantially across surveys, even after adjusting for potential confounders (Figure 1). The strongest protective effect was observed in Vietnam (2002) (PR 0.51, 95%CL 0.28-0.91), and the strongest harmful effect, though not statistically significant, was observed in Armenia (2000) (PR 1.64, 95%CL 0.76-3.56). A total of 23 surveys showed a significant protective effect of improved drinking water, while 190 had effects that overlapped the null, and 4 had a harmful effect. Adjustment for confounders tended to attenuate the effect of improved water (unadjusted PRs for each survey can be seen in Figure S1).
Figure 1.
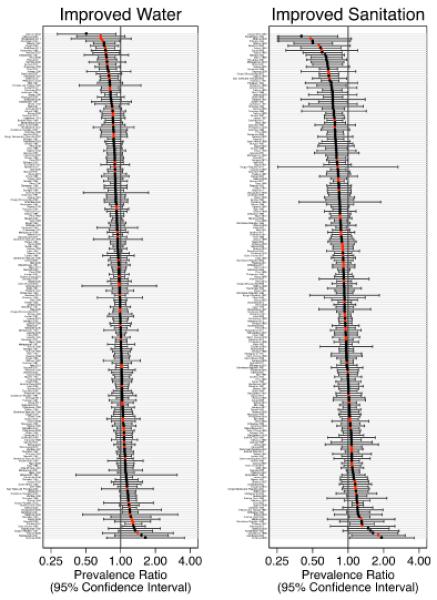
The effect of improved drinking water and improved sanitation in each of the 217 Demographic and Health Surveys, 1986-2013. Prevalence ratios are for diarrhea comparing those with the improved service to those without, adjusted for child’s age and sex, household wealth quintile, and urban/rural residence. Red markers indicate the most recent surveys for countries with surveys completed since 2003. Note: For display purposes, confidence limits are truncated if the lower limit is < 0.25. This is indicated by an arrowhead.
The adjusted effect of improved sanitation also varied across surveys, with PRs ranging from 0.40 (95% CL 0.20-0.82) in Kazakhstan (1999) to 1.93 (95% CL 1.03-3.63) in Armenia (2005) (Figure 1). 41 surveys showed a significant protective effect, 168 had effects overlapping the null, and 7 showed a statistically significant harmful effect. Jordan (2012) had too few children in the unimproved category to estimate the effect of sanitation. Similar to what was seen for improved drinking water, adjustment for confounders had a mostly attenuating effect on the impact of improved sanitation (unadjusted PRs can be seen in Figure S1).
Pooled Results
When pooling data across all 217 surveys, the unadjusted prevalence of diarrhea was 8.9% lower (PR 0.92, 95%CL 0.91-0.93) among those with improved drinking water compared to those without (Table 1, Model 1). When we accounted for differences in household SES and access to sanitation services the effect was attenuated (PR 0.97, 95% CL 0.96-0.99; Table 1, Model 3). Adjusting for the child’s age, sex, and urban/rural residence had no effect on the impact of improved water, suggesting that these covariates are not confounders (Table 1, Model 4). The unadjusted effect of improved sanitation (PR 0.85, 95% CL 0.84-0.86) was stronger than that of drinking water (Table 1, Model 2). This effect was also attenuated after accounting for household SES (PR 0.93, 95% CL 0.92-0.95; Table 1, Model 3) but remained stronger than the adjusted effect of improved drinking water. There was little evidence of a difference in the effect of water or sanitation between urban and rural areas (Table S2).
Table 1.
Prevalence ratios (and 95% Confidence Limits) for diarrhea among children < 5 years of age in 217 Demographic and Health Surveys, 1986-2013. All models include survey fixed effects and account for complex sampling design. Models 1-4 include all 217 surveys. Models 5-8 include only the most recent surveys for countries with a survey completed since 2003
| All Surveys | Last 10 Years | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
|
Improved Water vs.
Unimproved |
0.919 (0.908 - 0.929) |
0.973 (0.961 - 0.985) |
0.971 (0.960 - 0.983) |
0.944 (0.922 - 0.966) |
0.977 (0.954 - 1.000) |
0.975 (0.952 - 0.999) |
||
|
| ||||||||
|
Improved Sanitation
vs. Unimproved |
0.852 (0.841 - 0.863) |
0.932 (0.918 - 0.945) |
0.929 (0.915 - 0.942) |
0.902 (0.880 - 0.924) |
0.967 (0.942 - 0.994) |
0.961 (0.935 - 0.988) |
||
|
| ||||||||
|
Female Child vs.
Male Child |
0.927 (0.919 - 0.935) |
0.929 (0.913 - 0.945) |
||||||
|
| ||||||||
| Age of child in years | ||||||||
| 1 vs. 0 | 1.27 (1.256 - 1.285) |
1.326 (1.296 - 1.357) |
||||||
| 2 vs. 0 | 0.833 (0.822 - 0.844) |
0.866 (0.843 - 0.889) |
||||||
| 3 vs. 0 | 0.534 (0.525 - 0.543) |
0.559 (0.541 - 0.577) |
||||||
| 4 vs. 0 | 0.386 (0.379 - 0.393) |
0.396 (0.382 - 0.410) |
||||||
|
| ||||||||
| SES Quintile1 | ||||||||
| 2 vs. 1 | 0.992 (0.978 - 1.006) |
0.981 (0.967 - 0.995) |
0.995 (0.967 - 1.024) |
0.978 (0.951 - 1.007) |
||||
| 3 vs. 1 | 0.975 (0.960 - 0.990) |
0.958 (0.943 - 0.972) |
0.969 (0.940 - 0.999) |
0.947 (0.919 - 0.977) |
||||
| 4 vs. 1 | 0.933 (0.919 - 0.948) |
0.907 (0.892 - 0.921) |
0.938 (0.908 - 0.968) |
0.905 (0.876 - 0.935) |
||||
| 5 vs. 1 | 0.795 (0.781 - 0.810) |
0.767 (0.752 - 0.782) |
0.828 (0.799 - 0.859) |
0.786 (0.757 - 0.817) |
||||
|
| ||||||||
| Rural vs. Urban | 0.96 (0.946 - 0.975) |
0.941 (0.914 - 0.969) |
||||||
|
| ||||||||
| N | 1,584,397 | 1,581,441 | 1,577,881 | 1,577,881 | 491,539 | 491,689 | 491,201 | 491,201 |
SES = socioeconomic status
Quintile 1 represents the lowest level of SES, and quintile 5 represents the highest.
Longitudinal Trends
When excluding surveys conducted prior to 2003, the adjusted effect of improved sanitation was smaller (Table 1, Model 8). A gradual attenuation of the effect of sanitation over time can be observed in Figure 2. For example, when pooling surveys conducted between 1989 and 1991, the adjusted effect of improved sanitation was 0.89 (95%CL 0.83-0.95), and for surveys conducted between 2006 and 2008 the effect was null (PR 0.99, 95% CL 0.95-1.02). Because this trend may be due to the inclusion of different countries from varying time points, we used a multilevel model to investigate within-country trends. The predicted prevalence ratio for improved sanitation can be seen to increase over time (p=0.09) and approach the null in recent years, suggesting that this attenuation occurred within countries. The effect of improved drinking water appeared to be relatively constant over time.
Figure 2.
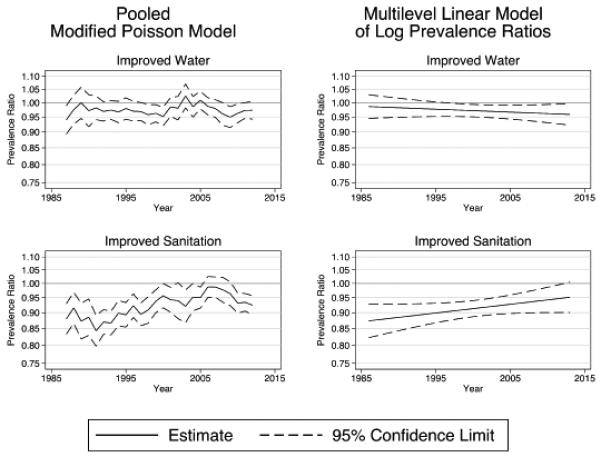
The effect of improved drinking water and improved sanitation over time in 217 Demographic and Health Surveys, 1986-2013. Prevalence ratios are for diarrhea comparing those with the improved service to those without, adjusted for child’s age and sex, household wealth quintile, and urban/rural residence. In the pooled modified poisson results, pooled models were run for each year, excluding all surveys except those conducted during that year, the year before, or the subsequent year. In the multilevel model results, a linear model of the log prevalence ratio was estimated only for countries with >1 survey.
Independent and Joint Effects of Water and Sanitation
When all 217 surveys were combined, the prevalence of diarrhea was lower when a household had either improved water, improved sanitation, or both compared to when they had neither service (Table 2, Model 9). The unadjusted independent effect of improved sanitation, however, was stronger than that of improved water. Adjusting for confounders resulted in a marked attenuation of both independent effects and the joint effect (Table 2, Model 10). The adjusted independent effect of improved water was statistically significant but small (PR 0.98, 95% CL 0.97-0.99). The adjusted independent effect of sanitation was some-what larger (PR 0.95, 95% CL 0.92-0.97). Having both improved water and sanitation resulted in a 9.9% lower prevalence of diarrhea (PR 0.90, 95% CL 0.89-0.92). When considering only surveys from the past 10 years, having both improved water and sanitation resulted in a 5.9% lower prevalence of diarrhea.
Table 2.
The independent and joint effects of water and sanitation. Prevalence ratios (and 95% Confidence Limits) for diarrhea among children < 5 years of age in 217 Demographic and Health Surveys. All models are modified poisson regressions, include survey fixed effects, and account for complex sampling design. Models 9-10 include all 217 surveys. Models 11-12 include only those surveys completed since 2003.
| All Surveys | Last 10 Years | |||
|---|---|---|---|---|
|
| ||||
| Model 9 | Model 10 | Model 11 | Model 12 | |
| Neither Improved | 1.000 (Ref.) |
1.000 (Ref.) |
1.000 (Ref.) |
1.000 (Ref.) |
| Improved Water Only | 0.954 (0.941 - 0.967) |
0.979 (0.965 - 0.993) |
0.978 (0.949 - 1.007) |
0.993 (0.964 - 1.023) |
| Improved Sanitation Only | 0.881 (0.863 - 0.901) |
0.945 (0.924 - 0.966) |
0.942 (0.903 - 0.983) |
0.996 (0.954 - 1.041) |
| Both Improved Water and Sanitation |
0.816 (0.803 - 0.829) |
0.901 (0.885 - 0.918) |
0.875 (0.848 - 0.904) |
0.941 (0.908 - 0.975) |
|
| ||||
| Female Child vs. Male Child | 0.927 (0.919 - 0.935) |
0.929 (0.913 - 0.945) |
||
|
| ||||
| Age of child in years | ||||
| 1 vs. 0 | 1.270 (1.256 - 1.285) |
1.326 (1.296 - 1.357) |
||
| 2 vs. 0 | 0.833 (0.822 - 0.844) |
0.866 (0.843 - 0.889) |
||
| 3 vs. 0 | 0.534 (0.525 - 0.543) |
0.559 (0.541 - 0.577) |
||
| 4 vs. 0 | 0.386 (0.379 - 0.393) |
0.396 (0.382 - 0.410) |
||
|
| ||||
| SES Quintile1 | ||||
| 2 vs. 1 | 0.980 (0.966 - 0.994) |
0.978 (0.951 - 1.006) |
||
| 3 vs. 1 | 0.957 (0.943 - 0.972) |
0.947 (0.919 - 0.976) |
||
| 4 vs. 1 | 0.906 (0.892 - 0.921) |
0.904 (0.875 - 0.934) |
||
| 5 vs. 1 | 0.767 (0.753 - 0.782) |
0.786 (0.757 - 0.816) |
||
|
| ||||
| Rural vs. Urban | 0.960 (0.946 - 0.974) |
0.941 (0.914 - 0.969) |
||
|
| ||||
| N | 1,577,881 | 1,577,881 | 491,201 | 491,201 |
|
| ||||
| Multiplicative Interaction | ||||
| Expected Joint Effect2 | 0.841 (0.816-0.865) | 0.925 (0.897-0.952) | 0.921 (0.865-0.977) | 0.990 (0.928-1.052) |
| p-value for interaction3 | 0.019 | 0.039 | 0.043 | 0.042 |
|
| ||||
| Additive Interaction | ||||
| Expected Joint Effect4 | 0.835 (0.809-0.862) | 0.924 (0.895-0.952) | 0.920 (0.862-0.977) | 0.990 (0.927-1.052) |
| p-value for interaction3 | 0.090 | 0.058 | 0.059 | 0.041 |
SES = socioeconomic status. 1Quintile 1 represents the lowest level of SES, and quintile 5 represents the highest.
Product of the two independent effects (PRWater × PRSanitation). 95% Confidence limits calculated using the delta method.
p-values calculated using the delta method.
Sum of the two independent effects – 1 (PRWater + PRSanitation − 1). 95% Confidence limits calculated using the delta method.
The results of Model 10 suggest very little interaction on the multiplicative scale. The expected joint effect, under the assumption of no multiplicative interaction, was 0.93 (0.98*0.95), only slightly larger than the observed joint effect of 0.90 (p-value for difference=0.039). Similarly, Model 10 shows little interaction on the additive scale, where the expected joint effect of 0.92 (0.98+0.95-1), only slightly different from the observed (p=0.058). This is evidence that water and sanitation are likely operating primarily on different pathways. When considering only surveys from the past 10 years, however, Model 12 shows synergistic interaction for water and sanitation. Neither alone had any effect on the prevalence of diarrhea; however, both together had a protective effect. On the multiplicative and additive scales, the observed effect was larger than the expected effect (p=0.042 and p=0.041, respectively).
Discussion
Our findings confirm the results of previous studies that water and sanitation infrastructure reduce the risk of diarrheal disease in children and that water and sanitation likely operate independently. We found, however, that the individual effect of improved sanitation and improved water in our overall sample was smaller than that found in two previous meta-analyses. Fewtrell et al. (5) and Esrey et al.(16) reported reduced risks of diarrheal disease of 32% and 22% for sanitation interventions and 22% and 17% for water interventions, respectively, in contrast to the 7% and 3% reductions reported by our study (Table 1, Model 4). One significant difference is that these previous meta-analyses were summaries of intervention trials, many of which were of short duration with unblinded participants. Such intervention trials often attempt to measure the efficacy of an intervention under idealized conditions as opposed to its “real-world” effectiveness, which is often smaller.
Other cross-sectional studies (6, 10) using the DHS reported smaller effect sizes than those of the meta-analyses. For example, Fink et al. (10) used data from 171 surveys and found that intermediate and high quality water compared to low quality water reduced the odds of diarrhea by 8% and 9%, respectively. High and intermediate quality sanitation had slightly stronger reductions of 8% and 13%, respectively. Our results, however, showed even smaller effect sizes than these previous studies, especially for improved drinking water. There are three primary reasons for this: First, our analysis includes more up-to-date data from the DHS. Early surveys tended to show a much stronger effect of improved sanitation, while more recent surveys were more likely to show a null effect. Second, we estimated prevalence ratios, instead of prevalence odds ratios as previous studies had done. The odds ratio will be exaggerated relative to the prevalence ratio, especially when the outcome is not rare, as is the case in our data. Third, we use a different classification scheme for improved/unimproved water and sanitation. Our results suggest that the JMP scheme may not capture disease risk as well as technology classification schemes used in other studies. For example, when using the infrastructure categorization scheme of Fink et al. (10), we see a stronger protective effect of flush and pour-flush technology, but little effect of latrine technologies (see Supplemental Material). These differences are largely due to the fact that Fink et al. (10) use a three-level categorization which allows for a more extreme contrast. For drinking water, there is the additional difference that some technologies, such as bottled water, are classified by the JMP as unimproved but as the highest category by Fink et al. (10).
Confounding presents a substantial challenge for observational studies of water and sanitation. Households with unimproved services are much more likely to be of a lower SES, and therefore have higher risk of disease due to pathways other than water or sanitation, such as hygiene or contaminated food. Because SES is highly correlated with water and sanitation services, it is difficult to differentiate the effects. Our results show the presence of substantial confounding – the effect of improved drinking water is largely explained by differences in SES, yet SES was still highly protective even after adjusting for water and sanitation. If our measurement of water and sanitation technologies does not accurately capture the risks they pose, then SES may be capturing some of the true risk associated with water and sanitation in addition to capturing the effect of other pathways.
Our results also highlight the heterogeneity of the effect of improved water and sanitation across surveys. In many surveys, improved infrastructure is protective, in others it has no effect, and in a few it appears to be harmful. In the presence of high heterogeneity, a single effect measure is less useful and can even be misleading. This heterogeneity has several potential sources. First, classifying water and sanitation technologies across a variety of settings is a challenging task. Some of the observed heterogeneity may be due to a differing degree of measurement error between surveys. Second, in the absence of any type of bias or measurement error, sampling error will still result in some variability in the effect size across studies, even though the true underlying parameter of interest is the same. Lastly, it is likely that the effect of these improved services varies across time and place.
We have shown that the effect of improved sanitation has attenuated over the past 25 years, even within the same country. This finding is unique to our study, and may explain some of the variability seen across surveys. One possible explanation for this observed attenuation is that environmental contamination has decreased over time. This would reduce the fraction of cases attributable to poor sanitation, thus reducing its effectiveness at preventing disease. This and other explanations, such as the adoption of sub-optimal technology, are beyond the scope of this analysis but should be a focus of future research.
Our results underscore the importance of both water and sanitation for preventing diarrheal disease in children under five. Water and sanitation also provide other important health and non-health benefits to users, such as privacy and safety, warranting more investigation. When examining the independent and joint effects among all 217 surveys, either water or sanitation alone has a modest protective effect, and the joint effect of both together is roughly what is expected based on the independent effects. However, when using surveys from the past 10 years, water and sanitation infrastructure appear to be synergistic. In contrast to meta-analyses that reported combining interventions provide no additional benefit beyond what is seen with a single intervention (5, 16), these results support findings by Balthazar et al. (17), Esrey (6), and VanDerslice (7) that combined interventions are more protective in reducing diarrheal episodes than single interventions. Although these data provide no evidence of protection in the presence of either improved water or sanitation infrastructure alone; when in combination the services are protective. These two findings have a single underlying message − both interventions combined are better than a single intervention.
Supplementary Material
Acknowledgements
This work was supported by the National Institutes of Health. The data analyzed in this article come from the publicly available Demographic Health Surveys and can be accessed from their original format at www.dhsprogram.com.
References
- 1.Bartram J, Cairncross S. Hygiene, sanitation, and water: Forgotten foundations of health. PLoS Med. 2010 Nov 9;7(11):e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker CL, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013 Apr 20;381(9875):1405–16. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003 Jun 28;361(9376):2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 4.Curtis V, Cairncross S, Yonli R. Domestic hygiene and diarrhoea - pinpointing the problem. Trop Med Int Health. 2000 Jan;5(1):22–32. doi: 10.1046/j.1365-3156.2000.00512.x. [DOI] [PubMed] [Google Scholar]
- 5.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM., Jr. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: A systematic review and meta-analysis. Lancet Infect Dis. 2005 Jan;5(1):42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 6.Esrey SA. Water, waste, and well-being: A multicountry study. Am J Epidemiol. 1996 Mar 15;143(6):608–23. doi: 10.1093/oxfordjournals.aje.a008791. [DOI] [PubMed] [Google Scholar]
- 7.VanDerslice J, Briscoe J. Environmental interventions in developing countries: Interactions and their implications. Am J Epidemiol. 1995 Jan 15;141(2):135–44. doi: 10.1093/oxfordjournals.aje.a117401. [DOI] [PubMed] [Google Scholar]
- 8.Gundry S, Wright J, Conroy R. A systematic review of the health outcomes related to household water quality in developing countries. J Water Health. 2004 Mar;2(1):1–13. [PubMed] [Google Scholar]
- 9.Eisenberg JN, Scott JC, Porco T. Integrating disease control strategies: Balancing water sanitation and hygiene interventions to reduce diarrheal disease burden. Am J Public Health. 2007 May;97(5):846–52. doi: 10.2105/AJPH.2006.086207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fink G, Gunther I, Hill K. The effect of water and sanitation on child health: Evidence from the Demographic and Health Surveys 1986-2007. Int J Epidemiol. 2011 Oct;40(5):1196–204. doi: 10.1093/ije/dyr102. [DOI] [PubMed] [Google Scholar]
- 11.UNICEF. World Health Organization . Progress on drinking water and sanitation: 2012 update. USA: 2012. [Google Scholar]
- 12.Vyas S, Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006 Nov;21(6):459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 13.Rothman KJ, Greenland S, Lash TL. Moder epidemiology. 3rd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. [Google Scholar]
- 14.VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiologic Methods. 2014;3(1):33–72. [Google Scholar]
- 15.Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992 Sep;3(5):452–6. doi: 10.1097/00001648-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Esrey SA, Potash JB, Roberts L, Shiff C. Effects of improved water supply and sanitation on ascariasis, diarrhoea, dracunculiasis, hookworm infection, schistosomiasis, and trachoma. Bull World Health Organ. 1991;69(5):609–21. [PMC free article] [PubMed] [Google Scholar]
- 17.Baltazar J, Briscoe J, Mesola V, Moe C, Solon F, Vanderslice J, et al. Can the case- control method be used to assess the impact of water supply and sanitation on diarrhoea? A study in the Philippines. Bull World Health Organ. 1988;66(5):627–35. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


