Abstract
Background
Workplaces provide ideal environments for wellness programming. The purpose of this study was to explore exercise self-efficacy among university employees and the effects of a worksite wellness program on physical activity, cardiorespiratory fitness, and CVD risk factors.
Methods
Participants included 121 university employees (85% female). The worksite wellness program included cardiovascular health assessments, personal health reports, 8 weeks of pedometer-based walking and tracking activities, and weekly wellness sessions. Daily step count was assessed at baseline, week 4, and week 8. Exercise self-efficacy and CVD risk factors were evaluated at baseline and follow-up.
Results
Daily step count increased from 6566 ± 258 (LSM ± SE) at baseline to 8605 ± 356 at week 4 and 9107 ± 388 at week 8 (P < .0001). Steps increased among normal weight, overweight, and obese sub-groups. Exercise self-efficacy correlated with baseline steps (P < .05). Small improvements were observed in cardiorespiratory fitness, BMI, blood pressure, blood glucose, total cholesterol, and triglycerides (all P < .01).
Conclusions
A worksite wellness program was effective for increasing physical activity, cardiorespiratory fitness, and CVD risk factors among university employees. Exercise barriers and outcome expectations were identified and have implications for future worksite wellness programming.
Keywords: cardiovascular health, health promotion, pedometry, physical fitness, health behavior
BACKGROUND
Cardiovascular disease (CVD) persists as the leading cause of death in the U.S.1Although the CVD mortality rate has declined in recent years, rising rates of obesity and diabetes threaten to reverse this downward trend. National organizations2–3 have published a variety of evidence-based CVD prevention recommendations, yet widespread application of health promotion programs remains insufficient.
Workplaces provide ideal environments for the implementation of large-scale CVD prevention programs.1,4 However, successful wellness programming remains a laborious and resource-intensive challenge for many employers, necessitating simple and economical approaches. Many previous studies examined the impact of worksite wellness programs in the U.S. on physical activity,5– 8 but relatively few included university employees9–12 or cardiorespiratory fitness,9,11–14 an independent risk factor for CVD.15 Furthermore, factors that impact program adoption and adherence, such as participant self-efficacy, are often overlooked. Self-efficacy reflects a person’s confidence in his/her ability to effect change and is a key component of the health belief model,16 which posits that the likelihood of engaging in a health promoting behavior (such as physical activity) is directly influenced by the individual’s self-efficacy, perceived benefits, perceived barriers, and perceived susceptibility to a particular health problem.
We conducted a pilot worksite wellness trial designed to promote daily physical activity and healthful lifestyle behaviors among university campus employees. The aims of this study were (1) to examine exercise self-efficacy and its relation to physical activity level in university employees and (2) to evaluate the effects of a worksite wellness program on physical activity, cardiorespiratory fitness, and CVD risk factors.
METHODS
Study Recruitment, Worksite, and Eligibility Criteria
A worksite wellness program was offered to employees at Washington University in St. Louis, MO. The study was approved by the Washington University in St. Louis Institutional Review Board. Recruitment e-mails were sent to 832 staff employees in Central Fiscal Unit departments on the university’s Danforth Campus. Males and non-pregnant females ≥ 18 years of age were eligible, regardless of pre-existing health conditions, medication use, or physical activity level. In January 2012, 141 employees provided written informed consent during on-campus information and enrollment sessions; 121 employees completed baseline assessments and were enrolled in this prospective cohort study.
Worksite Wellness Program
The worksite wellness program was based on the health belief model16 and included cardiovascular health assessments, questionnaires, personal health reports, 8 weeks of pedometer-based walking and tracking activities, consultation opportunities with research team members throughout the program, weekly wellness education sessions, and participation rewards. The program was flexible, providing weekly monitoring of activity goals, weight, and blood pressure for some participants, while allowing others to attend sessions only occasionally based on their work schedules and preferences. The weekly education sessions were led by health professionals (eg, physical therapists, physiologist, registered dietitian, cardiologist) and included presentations/group discussions on walking wisdom, nutrition pointers, exercise recommendations, health assessment results, workstation wellness & office ergonomics, and lifestyle behaviors to enhance heart health. Research team members also led group walks.
The pedometer-based activities incorporated American Heart Association (AHA) Start Walking Program resources,17 which enabled our participants to register under a company name that was set up specifically for this study. A major feature of this program is the web-based Activity Tracker, which contains a drop-down menu of 27 recreational, sport, and household activities, a choice of intensity levels, and a built-in calculator that converts activity time (in minutes) to steps and miles for non-ambulatory activities such as swimming and cycling. For example, 30 minutes of cycling outdoors at moderate intensity equates to approximately 7272 steps, while swimming at a vigorous intensity for 15 minutes is estimated to equal 4999 steps. This Activity Tracker then serves as a diary to store all of the individual’s physical activity information, which can be viewed and tallied by day, week, month, or any specified period of time. The Activity Tracker also contains a Nutrition Diary, Company Scoreboard, and individualized walking plans based on a 10-question Walking Plan Quiz that asks about the individual’s current activity level, estimated fitness (based on the duration that they can maintain a brisk walking pace), age, weight, preference regarding single versus split walking bouts, health goals, and barriers. Participants were instructed to wear their pedometer daily and encouraged to track their daily physical activity with the AHA Activity Tracker. Specific goals that we encouraged participants to strive toward included accumulating 10,000 steps/day and completing at least 3000 steps in 30 minutes on five days/week to achieve sufficient moderate-intensity physical activity,18 consistent with national recommendations of 150 minutes/week of moderate-intensity physical activity.3
Outcomes
Outcome measures included pedometer step counts as an estimate of daily physical activity, exercise self-efficacy, CVD risk factor assessment, and a post-program survey. Baseline assessments were completed before the 8-week pedometer-based intervention began and follow-up assessments were performed immediately after completion of the 8-week intervention. Step counts were quantified at baseline, week 4, and week 8. Exercise self-efficacy and CVD risk factors were assessed at baseline and follow-up. All assessments were conducted at the worksite.
Physical activity
Daily step counts were measured using Yamax SW-200 Digi-Walker Electronic Pedometer Step Counters (Yamasa Corporation; Tokyo, Japan) and 7-day pedometer step count logs at baseline, week 4, and week 8. The reported accuracy of this pedometer model for ambulatory physical activity is 99% in healthy adults.19 Average daily step count was used to determine physical activity category: sedentary (< 5000 steps/day), low active (5000–7499), somewhat active (7500–9999), active (10,000–12,499), or highly active (≥ 12,500).20 Based on the results of Tudor-Locke et al21 that 4 or more days of pedometer monitoring provide a reliability intra-class correlation greater than 0.90 for predicting weekly physical activity of adults, we required our participants to have at least 4 days of step count data each week to be included in the step count analyses.
Exercise self-efficacy
Exercise self-efficacy was assessed with the Barriers Specific Self-Efficacy Scale (BARSE)22 and the Multidimensional Outcome Expectations for Exercise Scale (MOEES).23 The BARSE22 is used to quantify perceived capability of performing regular exercise amidst commonly identified barriers. For each item, participants indicate their confidence in performing regular exercise in the face of a defined barrier on a 100-point scale, ranging from 0% (not at all confident) to 100% (highly confident) in 10-point increments. A total score is calculated by summing the confidence ratings and dividing by the number of items completed, resulting in a maximum possible score of 100. Total BARSE scores were computed for participants who responded to ≥ 10 of the 13 items. To identify the most frequently reported barriers, we tallied items for which participants chose values ≤ 30%, reflecting low or no confidence in their ability to overcome that barrier.
The MOEES23 is used to assess three domains of exercise outcome expectations: physical, social, and self-evaluative. Participants indicate the degree to which they agree or disagree with each statement on a 5-point ordinal scale with choices of 1 (strongly disagree), 2 (disagree), 3 (neutral), 4 (agree), and 5 (strongly agree). Each MOEES domain is scored by summing the ratings for each item within that domain. Total MOEES scores were calculated by summing item responses for all domains for participants who responded to ≥ 80% of the items. Higher scores indicate higher exercise outcome expectations. To identify the most frequently reported exercise outcome expectations, we tallied items for which participants chose values of 4 (agree) or 5 (strongly agree).
CVD risk factors
Cardiovascular health assessments were conducted after an overnight fast and included height, weight, body composition, waist circumference, blood pressure, resting pulse rate, fasting lipid and glucose levels, and cardiorespiratory fitness. Assessments were made on campus by trained investigators and research staff using National Health and Nutrition Examination Survey procedures.24 Height was measured with a portable stadiometer, body weight and body composition were measured on the Biospace InBody520 Body Composition Analyzer (Biospace, Los Angeles, CA; reported accuracy 98%25), and body mass index (BMI) was calculated. Waist circumference was measured at the superior border of the iliac crest with a Gulick II tape measure over bare skin.24 Blood pressure and resting pulse rate were measured in duplicate using Omron HEM-907XL Professional Digital Blood Pressure Monitors (Omron Healthcare, Kyoto, Japan; reported accuracy within 2 mmHg for systolic and 3 mmHg for diastolic blood pressure.26) following 10 minutes of seated rest, with one minute between readings. Fasting lipid and glucose concentrations were determined using Cholestech Analyzers (Cholestech LDX System®, Hayward, CA) and a single finger-stick blood sample. Because the accuracy of this instrument is dependent upon technique,27 the same trained members of our research team performed the cholesterol and glucose analyses at both assessment time points.
Cardiorespiratory fitness was estimated with the 3-minute Tecumseh Step Test,28,29 using an 8-inch step and a metronome set to 96 beats/minute. After stepping, the participant was seated and the right radial pulse rate was measured for 30 seconds, beginning 30 seconds into recovery. This recovery pulse rate was used as an estimate of recovery heart rate to determine cardiorespiratory fitness category (ie, outstanding, very good, good, fair, low, or poor) based on age- and sex-specific criteria for recovery heart rate.28,29 Lower heart rate values one minute after completion of the step test indicate higher fitness. A Physical Activity Readiness Questionnaire30 was used to identify participants requiring further screening by qualified research team members before performing the step test. Participants with concerning health assessment results were advised to see their primary care provider.
Personal Health Reports
Participants received personal health reports after the baseline and follow-up cardiovascular health assessments to enhance their awareness and knowledge of their current health status. The single-page reports included results of their vital signs (blood pressure and resting pulse rate), anthropometrics (height, weight, BMI, body composition, and waist and hip circumferences), blood lipids and glucose, and cardiorespiratory fitness level. A personal health report guide accompanied the reports to provide a clear explanation of the importance of each measurement, the reference ranges, and the scientific evidence and citations of expert panels. Participants were offered the opportunity to review their results with a health professional on our research team.
Survey
Upon completion of the worksite program, participants were asked to complete a 10-question, anonymous, web-based survey (SurveyMonkey)31 to provide information about their perceived benefits of participation, program components that they valued, physician follow-up, and medication changes. Results from 78 survey respondents were tabulated and expressed as a percentage.
Statistical Analyses
Data were analyzed using SAS software, version 9.3 (SAS Institute Inc., Cary, NC) and SPSS software, version 19.0 (SPSS Inc., Chicago, IL). Steps across time were compared using Generalized Estimating Equations (GEEs) with an exchangeable correlation matrix to account for the correlation of multiple measurements for each participant. Physical activity categories across time were compared using GEEs with a multinomial probability distribution and an independent correlation matrix. Comparisons between time points (baseline, week 4, and week 8) were analyzed using least squares means (LSM) with a Tukey-Kramer adjustment for multiple comparisons. Exercise self-efficacy scores and CVD risk factors at baseline and follow-up were analyzed with paired t-tests. Spearman correlations were used to identify relationships between exercise self-efficacy scores and daily step counts at baseline and follow-up. Self-efficacy scores included in the correlation analyses were the total BARSE score, total MOEES score, MOEES physical outcome expectations score, MOEES social outcome expectations score, and MOEES self-evaluative outcome expectations score. Results are expressed as mean ± SD unless indicated otherwise.
RESULTS
One hundred twenty-one employees (85% female; 90% white, 8% black, 2% other; mean age 46 ± 11 years) enrolled in one week, meeting our target; 17 individuals (14.0%) were lost to follow-up after baseline assessments. Program completers and drop-outs did not differ in age, sex, or baseline step count (P > .05), but drop-outs had a higher BMI than completers (31.6 kg/m2 vs. 28.1 kg/m2, respectively, P = .02).
At baseline, 67% of the 121 enrollees were categorized as sedentary or low active based on daily step counts <7500,20 69% were overweight or obese (ie, BMI ≥ 25.0 kg/m2),32 21% had low or poor cardiorespiratory fitness based on step test recovery pulse rate,29 40% had elevated blood pressure (ie, ≥ 120 mmHg systolic or ≥ 80 mmHg diastolic),33 63% had at least one lipid value outside of desirable ranges based on National Cholesterol Education Program standards,34 and 32% had impaired fasting glucose (ie, ≥ 100 mg/dL).35 See Table 1 for health assessment results at baseline and follow-up for program completers.
Table 1.
Health assessment results of employees at baseline and follow-up
| Baseline | Follow-up | *P < .01 | 9 5 % CI | |
|---|---|---|---|---|
| Body Weight (kg) | 78.3 ± 19.9 | 77.4 ± 19.9 | * | −0.5 to −1.2 |
| BMI (kg/m2) | 28.2 ± 6.2 | 27.9 ± 6.2 | * | −0.2 to −0.4 |
| % Body fat | 37.6 ± 8.3 | 36.5 ± 8.8 | * | −0.8 to +8.8 |
| Female | 38.5 ± 7.9 | 37.6 ± 8.3 | * | −0.6 to −1.2 |
| Male | 32.6 ± 8.4 | 30.2 ± 9.3 | * | −1.6 to −3.1 |
| Waist circumference (cm) | 96.6 ± 14.6 | 95.1 ± 14.7 | * | −0.5 to −2.6 |
| Female | 95.4 ± 14.0 | 93.8 ± 14.0 | * | −0.3 to −2.5 |
| Male | 103.5 ± 16.6 | 102.1 ± 16.8 | −3.2 to +0.4 | |
| Systolic BP (mm Hg) | 115 ± 18 | 110 ± 14 | * | −3 to −7 |
| Diastolic BP (mm Hg) | 73 ± 11 | 70 ± 9 | * | −2 to −5 |
| Resting pulse rate (pulses/min) | 76 ± 11 | 73 ± 11 | * | −1 to −4 |
| Recovery pulse rate (pulses/30 sec) | 47 ± 8 | 44 ± 7 | * | −2 to −4 |
| Total cholesterol (mg/dL) | 190 ± 35 | 183 ± 31 | * | −2 to −12 |
| HDL cholesterol (mg/dL) | 58 ± 18 | 52 ± 16 | * | −3 to −8 |
| LDL cholesterol (mg/dL) | 109 ± 31 | 112 ± 27 | −2 to +8 | |
| Non-HDL cholesterol (mg/dL) | 132 ± 36 | 131 ± 32 | −6 to +3 | |
| Triglycerides (mg/dL) | 148 ± 91 | 122 ± 72 | * | −14 to −38 |
| Fasting blood glucose (mg/dL) | 95 ± 12 | 91 ± 12 | * | −2 to −6 |
Values reflect Mean ± SD and 95% confidence interval (CI) for employees who completed the study.
P < .01 for change from baseline to follow-up.
Daily step count increased from 6566 ± 258 (LSM ± SE) at baseline to 8605 ± 356 at week 4 and 9107 ± 388 at week 8. The increase in step count over time (P < .0001) was greater from baseline to week 4 (P < .0001) than from week 4 to week 8 (P = .02). Although obese participants took significantly fewer steps than normal weight and overweight participants at baseline (P = .003 and P = .006, respectively), the increase in steps over time was evident among all BMI categories, without interaction (P = .58), as shown in Figure 1.
Figure 1.
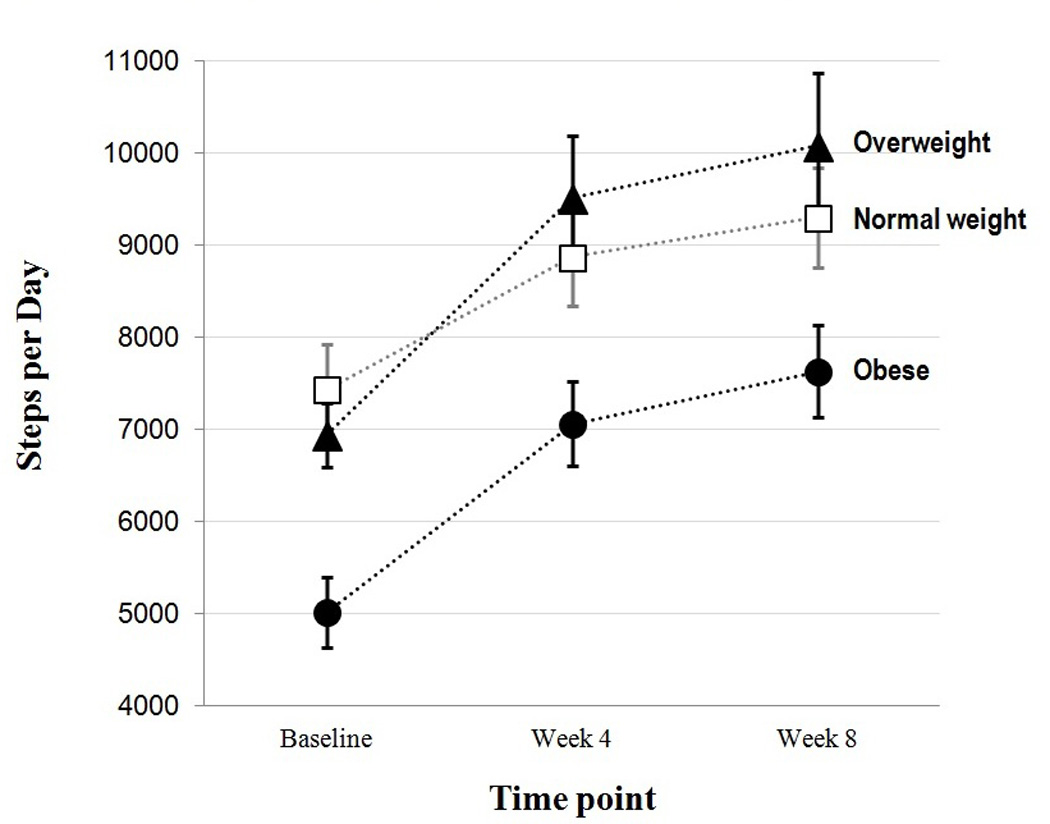
Employees’ daily step counts by weight status at baseline, week 4, and week 8.
Favorable shifts in physical activity categories (P < .0001) and in cardiorespiratory fitness categories (Z = −4.427, P < .001) were observed across time, as shown in Figure 2. The proportion of participants achieving 10,000 steps/day increased from 6% at baseline to 25% at week 4 and 36% at week 8 (Figure 2A). The odds of a participant being in a lower physical activity category at baseline was more than three times as likely as at week 4 (OR 3.3, 95% CI 2.7–4.7, P < .0001) and nearly five times as likely as at week 8 (OR 5.0, 95% CI 3.3–7.4, P < .0001). Figure 2B depicts the reduction in prevalence of poor or low cardiorespiratory fitness (from 21% to 6% of participants) and the increase in outstanding fitness (from 31% to 45% of participants).
Figure 2.
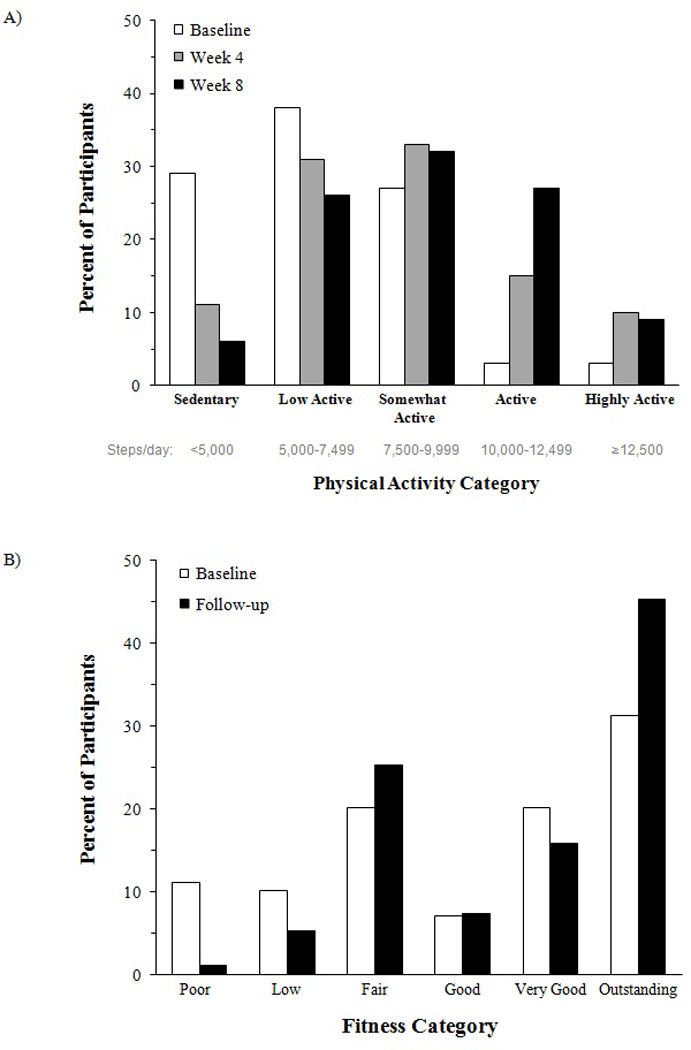
Percentage of participants in each physical activity category (A) and cardiorespiratory fitness category (B).
Exercise self-efficacy scores from the BARSE (barriers) and MOEES (expectations) correlated with daily steps at baseline (ρ = 0.289, P = .003 and ρ = 0.193, P = .049, respectively); similar results were observed at follow-up. There was not a significant difference in BARSE scores from baseline to follow-up (59.0 ± 17.5% to 61.6 ± 17.9%, P = .11). There were small changes in total MOEES scores (62.3 ± 6.5 to 63.3 ± 6.8, P = .04) and MOEES social outcome expectations domain scores (12.4 ± 2.9 to 12.9 ± 3.4, P = .01) from baseline to follow-up. The most frequently reported exercise barriers and outcome expectations are listed in Table 2.
Table 2.
Exercise self-efficacy: the most prevalent exercise barriers and exercise outcome expectations at baseline
| Barriers Specific Self-Efficacy Scale (BARSE) Item |
Prevalence of 'low confidence' |
|
| I believe that I could exercise 3 times per week for the next 3 months even if: | ||
| My schedule conflicted with my exercise session. | 42% | |
| I felt pain or discomfort when exercising. | 40% | |
| It became difficult to get to the exercise location. | 39% | |
| I was not interested in the activity. | 30% | |
| I didn't like the particular activity program that I was involved in. | 29% | |
|
Multidimensional Outcome Expectations for Exercise Scale (MOEES) Item |
Outcome Expectation Domain |
Prevalence of 'agreement' |
| Exercise will improve my overall body functioning. | Physical | 100% |
| Exercise will improve the functioning of my cardiovascular system. | Physical | 99% |
| Exercise will increase my muscle strength. | Physical | 98% |
| Exercise will help manage stress. | Self-evaluative | 98% |
| Exercise will improve my ability to perform daily activities. | Physical | 96% |
Values reflect the proportion of participants with ≤ 30% confidence to overcome each BARSE item, and the proportion of participants who chose 4 (agree) or 5 (strongly agree) for each MOEES item. BARSE and MOEES items are listed in rank order.
Results of the survey administered at the conclusion of the program revealed that the top reasons for enrolling in the worksite program included a desire to improve or maintain health (94% of respondents) and free health assessments (74% of respondents); 73% of respondents perceived beneficial health changes due to participating in the program; 9% contacted their physician based on their health assessment results; 4% began or changed a medication during the study; 92% would participate in a similar program if offered again; 90% desire another worksite pedometer-based walking and physical activity tracking program; and worksite wellness program components of greatest interest were exercise and physical activity (82% of respondents), health assessments (73%), and weight management (66%).
DISCUSSION
A multi-faceted, pedometer-based worksite wellness program was successful at increasing physical activity and cardiorespiratory fitness within 8 weeks. Notably, individuals in all BMI categories demonstrated increases in daily step count over time. Our program promoted modest improvements in several CVD risk factors, as reported in previous worksite studies.36,37
Average daily step counts of our participants upon enrollment (6566) was slightly higher than those reported by Bassett et al38 (5117 steps/day) for a nationwide sample of 1136 adults and similar to the baseline results of Chan et al39 (7029 step/day) for 106 employees from five worksites. Our observed increase in daily step count did not reach a plateau during the 8-week program. Conversely, Chan et al39 reported a plateau in daily step count (10,480) at week 4 of a 12-week pedometer-based worksite intervention. This difference may be explained by their higher rate of attrition than ours (41% vs. 14%), as the least active employees may be more likely to drop out, or by the lower physical activity level achieved by our participants at week 4 (8605 steps/day). At week 8, only 36% of our participants achieved the 10,000 steps/day goal. Similarly, Wilde et al40 reported that 38–50% of female participants reached 10,000 steps/day when following a prescribed 30-minute walk. Gilson et al41 also aimed to increase physical activity among university employees in Australia. Encouraging employees to take brisk walks during breaks and to stand more frequently during the work day added 6–10 minutes of walking time each day,41 which equates to approximately 600–1000 additional steps/day.18
Given the strong and independent associations between physical inactivity, low cardiorespiratory fitness, and CVD risk,15 workplace programs aiming to increase overall physical activity and/or the proportion of moderate-to-vigorous physical activity have the potential to improve the cardiovascular health of many employed adults. The modest improvements observed in adiposity, blood pressure, resting pulse, recovery pulse rate after exercise, total cholesterol, trigylcerides, and fasting blood glucose in the present study are consistent with an increase in physical activity and have been observed in previous worksite studies.42 Walking at the workplace may allow individuals to overcome commonly perceived barriers to exercise participation, such as schedule conflicts or difficulty getting to the exercise location, as reported by many of our participants. Because walking does not require specialized training, equipment, or facilities, it is an ideal activity for college campus employees. Pedometers are simple, economical tools for monitoring and increasing physical activity and may enhance worksite walking initiatives. The ongoing visual feedback that pedometers provide may increase extrinsic motivation and activity awareness,6 while encouraging healthy peer competition. The AHA Activity Tracker,17 which 98 of our 121 participants registered for, was easy to use and complemented the pedometer-based activities.
Another favorable aspect of our program was the provision of personal health reports after each assessment. As observed previously,14 individualized health reports motivate many employees to make behavioral changes due to increased awareness of their health status and disease risk factors. The combination of free health assessments (which the majority of participants reported as being an important reason for enrolling), personal health reports, and weekly education sessions led by health professionals, addressed the “perceived susceptibility” component of the health belief model, while the education sessions and pedometer-based activities helped to address perceived benefits and barriers to enhance self-efficacy. In support of these strategies, Rooney et al6 observed that predictors of enhanced self-efficacy (i.e., confidence in overcoming exercise barriers) among 400 female employees were setting daily step count goals, wearing a pedometer “all of the time,” and keeping a step log. In the current study, we observed improvements in self-efficacy with respect to exercise outcome expectations, but not in participants’ confidence in overcoming exercise barriers, on average.
Our worksite wellness program was designed to be convenient, with all activities held on-campus, optional weekly wellness sessions, use of the AHA Activity Tracker that could be accessed from any device with internet access, and e-mail as the primary communication mode. In support of our strategies, Lauzon et al43 reported that primary contact via e-mail was well-received by participants, submission of step count logs to the research team provided accountability, and a program requiring greater time commitment likely would have prevented participation. Participant education through weekly wellness sessions and CVD risk screening likely promoted changes in other health behaviors, such as dietary patterns and physician visits. Participants may have also been exposed to additional lifestyle education through the recommended AHA web-based resources. Although we are unable to distinguish the relative contributions of each wellness program component, a systematic review of worksite health promotion programs reported that providing incentives, offering a multi-component approach, and focusing on health behaviors in addition to physical activity yield higher participation levels among employees.44
Limitations of the study include lack of a control group, few male participants, and the inability of the pedometers to quantify non-ambulatory activities or activity intensity. Furthermore, we cannot determine the extent to which dietary changes influenced the CVD risk factor outcomes and we acknowledge that a program of longer duration and/or higher intensity may have produced greater benefits. Greater participation among female employees is consistently reported in worksite health promotion studies.44 Similar to our finding that individuals with higher BMI are more likely to drop out, Speck et al45 reported higher drop-out rates among participants at an academic worksite with baseline step counts < 7499 steps/day. These results indicate that recruitment strategies and program components should be tailored to those less likely to participate, such as obese and sedentary individuals.
In summary, a pedometer-based worksite wellness program for university campus employees promoted greater levels of physical activity and improved cardiorespiratory fitness within 8 weeks. This pilot study allowed us to partner with a local university and assist them in identifying health initiatives that may be successful in their employee population. College campuses provide a unique environment for worksite wellness programs due to aesthetically pleasing and safe places to walk, as well as potential access to facilities in which health assessments may be conducted. Worksite programs that improve CVD risk factors have the potential to reduce the physical and economic burden of CVD and other chronic diseases. Future studies should explore combinations of worksite wellness activities that maximize program effect and employee participation.
ACKNOWLEDGEMENTS
We would like to acknowledge the contributions of Cindi L. Inman, Annie E. Goldring, and Michael Ju Kim for the conduct of wellness program activities and Karen Steger-May for biostatistical analyses. The authors are grateful to Kelly Laswell and personnel in the Office of Human Resources at Washington University in St. Louis for their collaborative efforts.
FUNDING SOURCES
This study was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448, sub-award TL1 TR000449, from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding was provided by a Washington University Program in Physical Therapy Research Division Pilot Award and the St. Louis Community/University Health Research Partnerships grant supported by Washington University in St. Louis, Saint Louis University, and BJC HealthCare.
Contributor Information
Carling E. Butler, Email: carling.butler@utsouthwestern.edu.
B. Ruth Clark, Email: clarkru@wustl.edu.
Tamara L. Burlis, Email: burlist@wusm.wustl.edu.
Jacqueline C. Castillo, Email: Jackie.castillo@gmail.com.
Susan B. Racette, Email: racettes@wustl.edu.
REFERENCES
- 1.Carnethon M, Whitsel LP, Franklin BA, et al. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120(17):1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.U. S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington (DC): 2008. [Accessed 2013]. http://www.health.gov/paguidelines/. [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (NIOSH) [Accessed 2013];Total Worker Health. 2013 http://www.cdc.gov/niosh/TWH/.
- 5.Dishman RK, DeJoy DM, Wilson MG, Vandenberg RJ. Move to Improve: a randomized workplace trial to increase physical activity. Am J Prev Med. 2009;36(2):133–141. doi: 10.1016/j.amepre.2008.09.038. [DOI] [PubMed] [Google Scholar]
- 6.Rooney B, Smalley K, Larson J, Havens S. Is knowing enough? Increasing physical activity by wearing a pedometer. WMJ. 2003;102(4):31–36. [PubMed] [Google Scholar]
- 7.Wyatt HR, Peters JC, Reed GW, et al. Using electronic step counters to increase lifestyle physical activity: Colorado on the Move. J Phys Act Health. 2004;1(3):181–190. [Google Scholar]
- 8.Freak-Poli RL, Cumpston M, Peeters A, Clemes SA. Workplace pedometer interventions for increasing physical activity. Cochrane Database Syst Rev. 2013;4:CD009209. doi: 10.1002/14651858.CD009209.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Anshel MH, Brinthaupt TM, Kang M. The disconnected values model improves mental well-being and fitness in an employee wellness population. Behav Med. 2010;36(4):113–122. doi: 10.1080/08964289.2010.489080. [DOI] [PubMed] [Google Scholar]
- 10.Croteau KA. A preliminary study on the impact of a pedometer-based intervention on daily steps. Am J Health Promot. 2004;18(3):217–220. doi: 10.4278/0890-1171-18.3.217. [DOI] [PubMed] [Google Scholar]
- 11.Haines DJ, Davis L, Rancour P, Robinson M, Neel-Wilson T, Wagner S. A pilot intervention to promote walking and wellness and to improve the health of college faculty and staff. J Am Coll Health. 2007;55(4):219–225. doi: 10.3200/JACH.55.4.219-225. [DOI] [PubMed] [Google Scholar]
- 12.Soroush A, Der Ananian C, Ainsworth BE, et al. Effects of a 6-month walking study on blood pressure and cardiorespiratory fitness in U.S. and Swedish adults: ASUKI step study. Asian J Sports Med. 2013;4(2):114–124. doi: 10.5812/asjsm.34492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talbot LA, Metter EJ, Morrell CH, Frick KD, Weinstein AA, Fleg JL. A pedometer-based intervention to improve physical activity, fitness, and coronary heart disease risk in National Guard personnel. Mil Med. 2011;176(5):592–600. doi: 10.7205/milmed-d-10-00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Racette SB, Deusinger SS, Inman CL, Burlis TL, Highstein GR, Buskirk TD, Steger-May K, Peterson LR. Worksite Opportunities for Wellness (WOW): effects on cardiovascular disease risk factors after 1 year. Prev Med. 2009;49(2–3):108–114. doi: 10.1016/j.ypmed.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams PT. Physical fitness and activity and separate heart disease risk factors: a meta-analysis. Med Sci Sports Exerc. 2001;33(5):754–761. doi: 10.1097/00005768-200105000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 17.American Heart Association. [Accessed 2013];2013 http://www.startwalkingnow.org/. [Google Scholar]
- 18.Marshall SJ, Levy SS, Tudor-Locke CE, et al. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–415. doi: 10.1016/j.amepre.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 19.Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35(5):867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- 20.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting “how many steps are enough?”. Med Sci Sports Exerc. 2008;40(7 Suppl):S537–S543. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 21.Tudor-Locke C, Burkett L, Reis JP, Ainsworth BE, Macera CA. How many days of pedometer monitoring predict weekly physical activity in adults? Prev Med. 2005;40(3):293–298. doi: 10.1016/j.ypmed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 22.McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J Behav Med. 1992;15(1):65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- 23.Wójcicki TR, White SW, McAuley E. Assessing outcome expectations in older adults: the multidimensional outcome expectations for exercise scale. J Gerontol B Psychol Sci Soc Sci. 2009;64(1):33–40. doi: 10.1093/geronb/gbn032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. [Accessed 2013];National Health and Nutrition Examination Survey (NHANES), Anthropometry Procedures Manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Anthropometry_Procedures_Manual.pdf.
- 25.Biospace. Body520 Users Manual. 2005 [Google Scholar]
- 26.White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit. 2001;6(2):107–110. doi: 10.1097/00126097-200104000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Santee J. Accuracy and precision of the Cholestech LDX System in monitoring blood lipid levels. Am J Health Syst Pharm. 2002;59(18):1774–1779. doi: 10.1093/ajhp/59.18.1774. [DOI] [PubMed] [Google Scholar]
- 28.Montoye HJ, Willis PW, III, Cunningham DA, Keller JB. Heart rate response to a modified Harvard step test: males and females, age 10–69. Res Q. 1969;40(1):153–162. [PubMed] [Google Scholar]
- 29.Mackenzie B. [Accessed 2012];Tecumseh Step Test. 2002 http://www.brianmac.co.uk/tecumseh.htm. [Google Scholar]
- 30.Chisholm DM, Collis ML, Kulak LL, Davenport W, Gruber N, Stewart G. PAR-Q validation report: the evaluation of a self-administered pre-exercise screening questionnaire for adults. Victoria, Canada: British Columbia Ministry of Health; 1978. [Google Scholar]
- 31.SurveyMonkey. [Accessed 2012];1999 www.surveymonkey.com. [Google Scholar]
- 32.National Heart, Lung, and Blood Institute and National Institute of Diabetes and Digestive and Kidney Diseases. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda, MD: National Institutes of Health; 1998. NIH Publication No. 98-4083. [Google Scholar]
- 33.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 34.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 35.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(Suppl 1):S64–S71. doi: 10.2337/dc12-s064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 37.Murtagh EM, Murphy MH, Boone-Heinonen J. Walking: the first steps in cardiovascular disease prevention. Curr Opin Cardiol. 2010;25(5):490–496. doi: 10.1097/HCO.0b013e32833ce972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bassett DR, Jr, Wyatt HR, Thompson H, Peters JC, Hill JO. Pedometer-measured physical activity and health behaviors in U.S. adults. Med Sci Sports Exerc. 2010;42(10):1819–1825. doi: 10.1249/MSS.0b013e3181dc2e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan CB, Ryan DA, Tudor-Locke C. Health benefits of a pedometer-based physical activity intervention in sedentary workers. Prev Med. 2004;39(6):1215–1222. doi: 10.1016/j.ypmed.2004.04.053. [DOI] [PubMed] [Google Scholar]
- 40.Wilde BE, Sidman CL, Corbin CB. A 10,000 step count as a physical activity target for sedentary women. Res Q Exerc Sport. 2001;72(4):411–414. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- 41.Gilson ND, Puig-Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomized control trial. Int J Behav Nutr Phys Act. 2009;6:43. doi: 10.1186/1479-5868-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330–339. doi: 10.1016/j.amepre.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lauzon N, Chan CB, Myers AM, Tudor-Locke C. Participant experiences in a workplace pedometer-based physical activity program. J Phys Act Health. 2008;5(5):675–687. doi: 10.1123/jpah.5.5.675. [DOI] [PubMed] [Google Scholar]
- 44.Robroek SJ, van Lenthe FJ, van Empelen P, Burdorf A. Determinants of participation in worksite health promotion programmes: a systematic review. Int J Behav Nutr Phys Act. 2009;6:26. doi: 10.1186/1479-5868-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Speck RM, Hill RK, Pronk NP, Becker MP, Schmitz KH. Assessment and outcomes of HealthPartners 10,000 Steps® program in an academic work site. Health Promot Pract. 2010;11(5):741–750. doi: 10.1177/1524839908330745. [DOI] [PubMed] [Google Scholar]


