Abstract
Background
Iterative reconstruction technique has been proposed as a means of reducing patient radiation dose in pediatric CT. Yet, the effect of such reductions on diagnostic accuracy has not been thoroughly evaluated.
Objective
This study compares accuracy of diagnosing pediatric acute appendicitis using contrast-enhanced abdominopelvic CT scans performed with traditional pediatric weight-based protocols and filtered back projection reconstruction versus a filtered back projection/iterative reconstruction technique blend with reduced volume CT dose index (CTDIvol).
Materials and methods
Results of pediatric contrast-enhanced abdominopelvic CT scans done for pain and/or suspected appendicitis were reviewed in two groups: A, 192 scans performed with the hospital’s established weight-based CT protocols and filtered back projection reconstruction; B, 194 scans performed with iterative reconstruction technique and reduced CTDIvol. Reduced CTDIvol was achieved primarily by reductions in effective tube current-time product (mAseff) and tube peak kilovoltage (kVp). CT interpretation was correlated with clinical follow-up and/or surgical pathology. CTDIvol, size specific dose estimates (SSDE) and performance characteristics of the two CT techniques were then compared.
Results
Between groups A and B, mean CTDIvol was reduced by 45%, and mean SSDE was reduced by 46%. Sensitivity, specificity and diagnostic accuracy were 96%, 97% and 96% in group A vs. 100%, 99% and 99% in group B.
Conclusion
Accuracy in diagnosing pediatric acute appendicitis was maintained in contrast-enhanced abdominopelvic CT scans that incorporated iterative reconstruction technique, despite reductions in mean CTDIvol and SSDE by nearly half as compared to the hospital’s traditional weight-based protocols.
Keywords: Iterative reconstruction, Radiation dose reduction, Appendicitis, Computed tomography, Pediatrics
Introduction
Up to 8 percent of children visiting an emergency department with acute abdominal pain will ultimately be diagnosed with appendicitis [1]. Delayed diagnosis may result in appendiceal rupture, abscess formation and/or septic shock [1]. Although US is recommended as the first-line imaging modality in children and adolescents, up to 60% of pediatric patients diagnosed with appendicitis in the United States now undergo preoperative CT scanning, increased from 1% to 5% in 1997 [2, 3].
Increased CT usage likely reflects the greater sensitivity and diagnostic confidence that CT affords [1]. Meta-analysis of 26 pooled studies demonstrated 94% sensitivity and 95% specificity for appendicitis with pediatric CT vs. 88% sensitivity and 94% specificity with pediatric US [4]. Yet, CT exposes patients to ionizing radiation. While controversy remains regarding the cancer risk associated with pediatric CT, it seems prudent to keep radiation dose as low as reasonably achievable (ALARA) without compromising diagnostic accuracy. To this end, many institutions, including our own, have adopted a staged imaging approach to evaluation of suspected appendicitis that begins with US and proceeds to CT only when diagnostic uncertainty persists or complications such as abscess formation are suspected [5, 6]. With such an approach, Krishnamoorthi et al. [6] showed a 53% reduction in CT scans performed.
For cases in which CT remains necessary, our hospital and others have reduced radiation dose through establishment of child-sized CT protocols, with smaller radiation doses given to smaller patients [7]. Child-sized CT protocols have been in use at our institution for more than a decade, scaled to patient weight and reconstructed with filtered back projection. More recently, iterative reconstruction technique has been introduced as a means of either improving image quality or reducing radiation dose. The iterative reconstruction technique employed at our institution (iDose4; Philips Healthcare, Cleveland, OH) reduces noise within CT data in both projection and image domains by iterative comparison to statistical models [8, 9]. While more computational power is required to implement iterative reconstruction technique, technical advances now allow image reconstruction speeds comparable to those achieved with filtered back projection reconstruction [8].
The reduction in background noise that iterative reconstruction technique provides can be leveraged to lower radiation dose while maintaining spatial and low-contrast resolution [8, 10]. Reductions in volume CT dose index (CTDIvol) of up to 60% have been advocated [7]. Yet, few studies have assessed the effects of such changes on diagnostic performance. This study was undertaken to compare diagnosis of acute appendicitis using contrast-enhanced abdominopelvic CT scans performed with our hospital’s traditional pediatric protocols vs. those incorporating iterative reconstruction technique and reduced CTDIvol.
Materials and methods
With Institutional Review Board approval and waiver of consent, this retrospective study was performed using data from the picture archiving and communication system (PACS) (Impax; AGFA Healthcare Corporation, Greenville, SC), electronic medical record (Epic; Epic Systems Corporation, Verona, WI) and CT scanner archives at a university children’s hospital. To identify eligible subjects, indications were reviewed for all non-angiographic contrast-enhanced abdominopelvic CT scans done in patients younger than 18 years of age and 82 kg (180 pounds) of weight between June 2008 and September 2012. The study period was chosen to provide approximately 2 years of data for each of the two CT protocols being compared. Scans for which the indication was suspicion of acute appendicitis or abdominal pain without history of appendectomy were eligible for inclusion. Those that did not follow established pediatric protocols, because of technologist error or unavailability of the iDose4-equipped CT scanners, were excluded, as they did not represent the groups under investigation. Follow-up scans done in patients with prior CT documentation of appendicitis were also excluded because the diagnosis of appendicitis in these patients was already known by the interpreting radiologist. In the absence of previously documented appendicitis, serial scans done in patients for distinct episodes of pain more than 4 weeks apart were not excluded, since a prior negative CT examination does not preclude development of appendicitis at a later date.
From June 2008 through October 18, 2010, weight-based pediatric CT scans using filtered back projection reconstruction (group A) were done on one of six multidetector-row CT (MDCT) scanners (Mx8000-4 or –IDT 16 and Brilliance-16P, -64 or -iCT 256; Philips Healthcare, Cleveland, OH). Weight-based pediatric protocols had been previously established for each of these scanners in collaboration with a qualified medical physicist to maintain diagnostic performance while reducing the amount of radiation used relative to adult techniques.
From October 19, 2010, through September 2012, CT scans (group B) were performed on one of two MDCT scanners with iterative reconstruction technique software (Ingenuity-128 or Brilliance-64 with iDose4; Philips Healthcare, Cleveland, OH) and were reconstructed with a filtered back projection/iterative reconstruction technique blend at iDose4 level 5. The iDose4 level is user-specified and determines the strength of iterative reconstruction technique applied, with noise reduction relative to filtered back projection ranging from 11% at iDose4 level 1 to 55% at iDose4 level 7 [8]. Increasing iterative reconstruction strength leads to greater reduction of noise [8]. However, it also incrementally alters image texture, resulting in an increasingly “plastic” look [8]. To balance these effects, we chose an intermediate iterative reconstruction level (iDose4 level 5) that provided 37% noise reduction but was still acceptable in appearance [8].
Scan parameters for groups A and B are shown in Table 1. Effective tube current-time product in milliampere-seconds (mAseff) was reduced by 32–40% in group B patients weighing 9 kg or more, and peak kilovoltage (kVp) was reduced from 120 to 100 in group B patients weighing less than 45 kg. In patients weighing less than 9 kg, mAseff reduction was capped at 20–25% due to lower inherent tissue contrast in the absence of adipose. A kVp of 120 was maintained in patients weighing more than 45 kg to avoid beam attenuation effects and further increases in image noise [11, 12]. Group B parameter changes were in keeping with manufacturer recommendations and were made incrementally under the guidance of a medical physicist after careful subjective and objective analysis of image quality. In establishing these new protocols, a reduction in hepatic signal-to-noise ratio of 12–14% was accepted in group B as compared to group A because we believed that there was potential to further reduce our baseline CTDIvol. As tolerated, scans were performed with positive gastrointestinal contrast (Omnipaque [iohexol] 300; GE Healthcare Inc., Princeton, NJ) diluted 3:100 with water and administered by mouth or nasogastric tube over 1.5–2 h preceding the scan on a volume per age scale. Intravenous contrast (Omnipaque [iohexol] 300; GE Healthcare Inc., Princeton, NJ), 2 mL/kg, was also administered.
Table 1.
CT parameters. Lower CTDIvol is achieved in group B primarily by reductions in mAseff and kVp as compared to group A.
| Traditional weight-based protocols with FBP (Group A) |
Reduced-CTDIvol protocols with FBP/IRT blend (Group B) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Section thickness (mm) | 3 | 3 | ||||||
| Section interval (mm) | 1.5 | 1.5 | ||||||
| Rotation time (s) | 0.5 – 0.8 | 0.5 | ||||||
| Pitch | 0.7 – 1.0 | 0.9 | ||||||
| Reconstruction filter | Standard B | Standard B | ||||||
| Patient weight (kg) | n | mAseff | kVp |
Mean CTDIvol (mGy) |
n | mAseff | kVp |
Mean CTDIvol (mGy) |
| <9 | 3 | 70–75 | 120 | 4.6 | 4 | 56 | 100 | 2.2 |
| 9–17 | 3 | 80 | 120 | 4.9 | 1 | 52 | 100 | 2.1 |
| 5 | 3 | |||||||
| 18–26 | 3 | 90 | 120 | 5.5 | 5 | 58–60 | 100 | 2.3 |
| 7 | 0 | |||||||
| 27–35 | 2 | 100 | 120 | 6.3 | 2 | 64–68 | 100 | 2.5 |
| 4 | 7 | |||||||
| 36–44 | 1 | 120 | 120 | 7.3 | 2 | 75–80 | 100 | 3.1 |
| 9 | 7 | |||||||
| 45–67 | 5 | 150 | 120 | 9.3 | 6 | 95–96 | 120 | 6.3 |
| 8 | 1 | |||||||
| 68–81 | 1 | 200 | 120 | 12.2 | 1 | 119–120 | 120 | 7.9 |
| 6 | 2 | |||||||
FBP filtered back projection, IRT iterative reconstruction technique, mAseff effective milliampere-seconds, kVp peak kilovoltage, CTDIvol volume CT dose index, n number of subjects
For all scans, patient age, gender and body width, CTDIvol, reference phantom diameter, CT diagnosis, and clinical outcome were recorded, including operative findings and pathology results, when available. Body width was measured with electronic calipers on axial images at the level of the splenic vein [13]. CTDIvol, a measure of radiation output from the CT scanner [14], was determined for each scan either directly from scanner archives or from archived dose pages in PACS. CTDIvol attributable to the planning CT radiograph was not displayed on all scanners used during the study and was therefore excluded. If patients required more than one acquisition due to motion or incomplete coverage, then the CTDIvol of the first acquisition was used. For comparison between groups, CTDIvol was normalized for a 32-cm reference phantom by multiplying each CTDIvol referencing the 16-cm phantom by 0.5 (personal communication, Philips Healthcare). Because size specific dose estimate (SSDE) conversion factors correct for differences in reference phantom diameter, raw CTDIvol data were used in SSDE calculations [15].
SSDE is an estimate of individual patient dose and was compared between groups in addition to CTDIvol to account for differences in patient size [15]. SSDE was calculated according to the following equation: SSDE (mGy) = f × CTDIvol (mGy), where f is a conversion factor obtained from published tables based on patient body width and reference phantom diameter [15].
To determine CT diagnosis, original CT reports were reviewed; no reinterpretation of the scans was performed for purposes of this study. Scans had been interpreted either by one of three fellowship-trained pediatric radiologists (with 6, 7 and 18 years of experience by the end of the study period) or by one of four general radiologists (with 2, 18, 20 and 21 years of experience at the end of the study period). These latter studies were included in the analysis because general diagnostic radiologists and pediatric radiologists have been shown to have comparable accuracy in CT diagnosis of pediatric appendicitis [16].
In the absence of inflammatory changes or abscesses, CT scans on which the appendix was not identified by the interpreting radiologist were classified as negative, since nonvisualization of the appendix has a negative predictive value of 98.7% [17]. Scans for which interpretation by the radiologist was equivocal were classified as positive if they were reported to be suggestive of appendicitis or if appendicitis was listed as the most likely diagnosis in a differential. Equivocal scans were classified as negative if the radiologist indicated a low suspicion of appendicitis, stated that appendicitis simply “could not be ruled out” or listed other diagnoses as being more likely. Because both inability to identify the appendix and equivocation with respect to diagnosis are potential reflections of image quality, the number of scans on which the appendix was not found and the number of scans with equivocal reports were recorded for each group.
To determine clinical outcomes, electronic medical records were reviewed through November 2012, resulting in a follow-up period of at least 2 months for all patients (and up to 54 months). For patients who underwent surgery, operative notes and pathology reports were reviewed for diagnosis. For patients who were discharged without surgery, records were reviewed for evidence of appendectomy at a later date, readmission to the hospital or return visits to the emergency department, pediatrician or surgeon.
True-positive CT examinations were defined as those for which CT findings of acute appendicitis were reported and intraoperative findings of appendicitis or positive pathology were documented. If surgery and pathology reports were discrepant, the pathology report was considered to be the gold standard. Positive CT findings of acute appendicitis generally included appendix diameter of greater than or equal to 7 mm (10 mm at the appendix tip), mural thickness of greater than 2 mm, and periappendiceal inflammation, with or without an appendicolith. Patients who had CT findings of appendiceal perforation (mural interruption, extraluminal gas, extraluminal appendicolith and/or developing abscess) but did not undergo appendectomy before November 2012 were also categorized as true positives if their clinical course was concordant. At our institution, these patients are typically treated with a course of antibiotics followed by appendectomy at a later date.
Scans were classified as true negatives if CT criteria for acute appendicitis were not met and patients were not diagnosed with appendicitis, either by appendectomy or clinical criteria, before November 2012. Scans were categorized as false positives if a CT diagnosis of acute appendicitis was made but operative findings and/or pathology results were negative or if symptoms resolved without treatment. False-negative examinations occurred when CT criteria of acute appendicitis were not met but the patient underwent appendectomy and had positive pathology.
Statistical analysis was performed with GraphPad Software (GraphPad Software Inc., La Jolla, CA). Categorical variables (patient gender, number of CT scans on which the appendix was not identified, number of CT scans with equivocal interpretations and number of patients with proven appendicitis) were compared between groups using Fisher exact test. Continuous variables (age, body width, CTDIvol and SSDE) were compared between groups using unpaired t-tests. Two-tailed P values of less than 0.05 were considered significant. CT performance characteristics were calculated according to standard equations: sensitivity=TP/(TP + FN); specificity=TN/(FP + TN); positive predictive value=TP/(TP + FP); negative predictive value=TN/(TN + FN); and diagnostic accuracy=(TP + TN)/(TP + TN + FP + FN); where TP equaled the number of true-positive cases, TN equaled the number of true-negative cases, FP equaled the number of false-positive cases, and FN equaled the number of false-negative cases [18].
Results
During the study period, a total of 482 contrast-enhanced abdominopelvic CT scans were done in eligible patients. Nine group A and 20 group B scans were excluded because they were not done according to established pediatric protocols. Forty-three group A and 24 group B scans were excluded due to pre-existing CT diagnosis of appendicitis. The remaining 386 scans met study inclusion criteria: group A, 192 scans (192 patients) performed with established pediatric weight-based protocols and filtered back projection reconstruction, and group B, 194 scans (190 patients) incorporating iterative reconstruction technique and reduced radiation parameters. More than one image acquisition was required in only 2% (3/192) group A and 4% (7/194) group B examinations, due to patient motion or incomplete coverage. There was no significant difference in gender (group A, 45% male (86/192); group B, 44% male (86/194); P=1.0), mean age (group A, 9.3 ± 4.8 years; group B, 9.5 ± 5.0 years; P=0.7), or mean body width (group A, 24.5 ± 4.6 cm; group B, 24.7 ± 4.7 cm; P=0.7). Reductions in mean CTDIvol of 45% (group A, 7.3 ± 2.3 mGy; group B, 4.0 ± 2.0 mGy) and mean SSDE of 46% (group A, 12.6 ± 2.5 mGy; group B, 6.8 ± 2.6 mGy) were highly statistically significant (P<0.0001). When stratified by body width (Table 2), SSDE in group A was within published pediatric diagnostic reference ranges (DRR), whereas SSDE in group B was below DRR [13].
Table 2.
Mean SSDE in groups A and B by body width, with comparison to published diagnostic reference ranges [13]
| Body width (cm) |
Group A | Group B | Diagnostic reference range (mGy) |
||
|---|---|---|---|---|---|
| n | Mean SSDE ± stdev (mGy) |
n | Mean SSDE ± stdev (mGy) |
||
| <15 | 2 | 10.5 ± 0.7 | 0 | NA | 5.8 – 12.0 |
| 15–19 | 35 | 10.6 ± 0.9 | 39 | 4.7 ± 0.3 | 7.3 – 12.2 |
| 20–24 | 68 | 11.4 ± 1.9 | 61 | 4.7 ± 0.4 | 7.6 – 13.4 |
| 25–29 | 60 | 14.2 ± 1.9 | 68 | 8.7 ± 2.4 | 9.8 – 16.4 |
| >30 | 27 | 15.1 ± 2.5 | 26 | 9.5 ± 1.7 | 13.1 – 19.0 |
n number of scans, SSDE size specific dose estimate, stdev standard deviation, NA not available
Outcome data are shown in Table 3. The overall rate of appendicitis based on clinical follow-up and surgical pathology was 27% (51/192) in group A and 28% (54/194) in group B (P=0.8). Of group A scans, 25% (49/192) were classified as true positives, 3% (5/192) as false positives, 1% (2/192) as false negatives and 71% (136/192) as true negatives. Of group B scans, 28% (54/194) were classified as true positives, 1% (1/194) as false positives and 71% (139/194) as true negatives. There were no false-negative scans in group B.
Table 3.
Outcome data by group.
| Group A | Clinical outcome | Group B | Clinical outcome | ||||
|---|---|---|---|---|---|---|---|
| + | − | + | − | ||||
| CT results | + | 49 | 5 | CT results | + | 54 | 1 |
| − | 2 | 136 | − | 0 | 139 | ||
| Total | 51/192 | 141/192 | Total | 54/194 | 140/194 | ||
| Percentage | 27% | 73% | Percentage | 28% | 72% | ||
+ = positive for appendicitis, − = negative for appendicitis
The rate of equivocal CT scan interpretations with respect to appendicitis was not significantly different between groups A and B (7% [13/192] and 3% [6/194], respectively; P=0.1). CT provided alternative diagnoses in 32% (62/192) of group A scans and 42% (82/194) of group B scans, most commonly inflammatory bowel disease, constipation, intussusception, small bowel obstruction, cholecystitis, pancreatitis or pyelonephritis. Considering all diagnoses (appendicitis and other), a specific etiology of the patient’s acute symptoms was suggested by 60% (116/192) of group A scans and 71% (137/194) of group B scans.
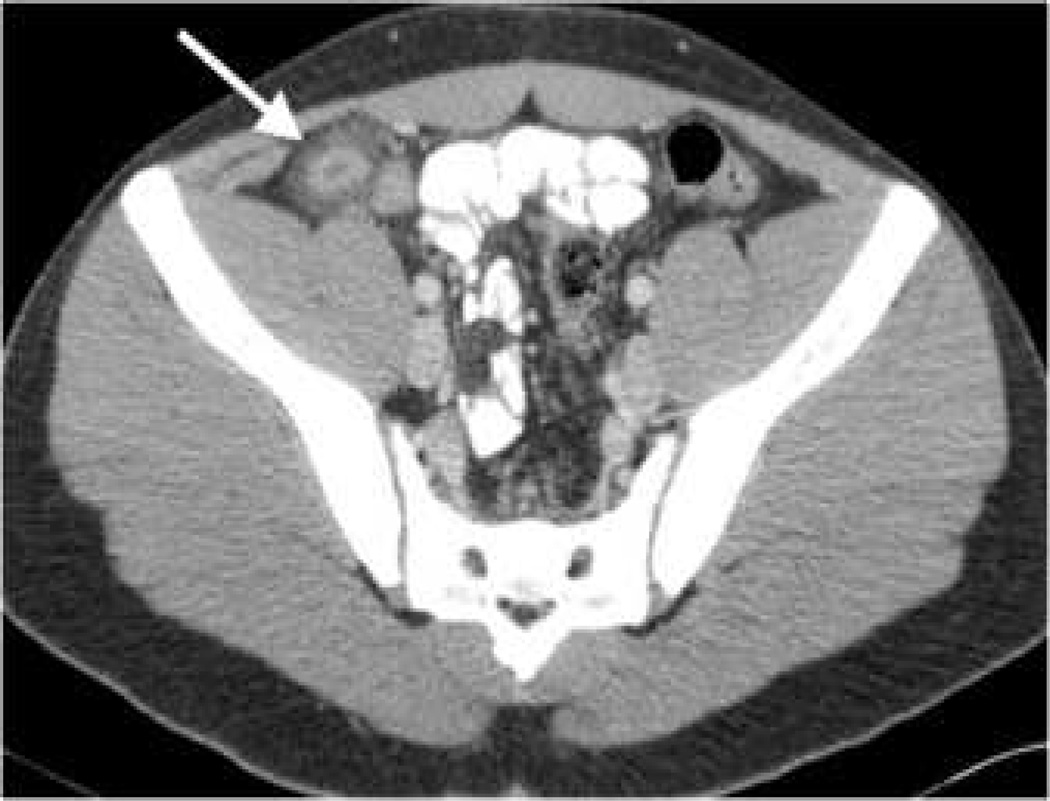
Representative images from true-positive scans in each group are shown in Figure 1. False-positive scans in group A consisted of two on which a bulbous appendiceal tip was surrounded by periappendiceal fluid, one on which the terminal ileum was mistaken for a dilated appendix, and two on which periappendiceal fat was secondarily edematous due to other processes in the abdomen (pancreatitis and intussuscepted Meckel diverticulum, respectively). Radiologists made the correct primary diagnoses in these latter two cases but also suggested concurrent appendicitis. Similarly, on the sole false-positive scan in group B, appendiceal thickening was likely secondary to colitis. Five of six patients with false-positive scans underwent laparotomy or laparoscopy. Appendectomy with negative pathology was performed in only three; the appendix was cleared by intraoperative inspection in two and by clinical followup in one.
Fig. 1.
Axial (a) and coronal (b) contrast-enhanced CT images of the pelvis in a 15-year-old boy show a 14-mm diameter appendix (arrow) with periappendiceal fat stranding, indicating presence of inflammation (group A, traditional pediatric weight-based protocol with filtered back projection reconstruction; 3 mm axial and coronal section thickness; CTDIvol 16 mGy; SSDE 23 mGy). Axial (c) and coronal (d) contrast-enhanced CT images of the pelvis in a 12-year-old boy show a 14-mm diameter, fluid-filled appendix (arrow) and periappendiceal inflammation (group B, filtered back projection/iterative reconstruction technique blend; 3 mm axial and coronal section thickness; CTDIvol 3 mGy; SSDE 5 mGy). Surgical pathology confirmed appendicitis in both patients
The two false-negative scans in group A, both with equivocal CT reports and positive pathology, had borderline (7–8 mm) appendiceal diameters without appreciable periappendiceal inflammation. None of the patients for whom CT was classified as negative because the appendix was not identified was ultimately diagnosed with appendicitis, and the number of such cases did not differ significantly between groups (12% [22/192], group A; 9% [18/194], group B; P=0.5).
Sensitivity, specificity and diagnostic accuracy were 96%, 97% and 96% for group A, compared to 100%, 99% and 99% for group B. Positive and negative predictive values were 91% and 99% for group A and 98% and 100% for group B. Although mean CTDIvol and SSDE were reduced in group B by 45% and 46%, respectively, CT performance characteristics were not diminished.
Discussion
Our results indicate that addition of iterative reconstruction technique to size-adjusted pediatric CT protocols allows significant reductions in CTDIvol and SSDE (45% and 46% in our study, respectively) without sacrificing diagnostic accuracy or decreasing diagnostic confidence. An important discovery in our study was the absence of false negative CT reports in group B. By preventing the incremental increase in image noise that would otherwise accompany a reduction in CTDIvol [8, 9], use of iterative reconstruction technique may temper a rise in false-negative results. Reductions in sensitivity and diagnostic accuracy were not encountered in our study. Rather, performance characteristics were very similar between groups.
Ultimately, appendicitis was diagnosed and confirmed clinically in a relatively low percentage of patients in both groups (27%, group A; 28%, group B), similar to the 26.5% appendicitis rate reported by Krishnamoorthi [6]. Inclusion of scans performed in patients with prior CT diagnosis of appendicitis would have increased our appendicitis rate but might also have falsely elevated diagnostic performance measures, as the diagnosis of appendicitis was already known by interpreting radiologists. Inclusion of patients who were not scanned according to specified pediatric protocols would have increased SSDE in both groups but would not have accurately reflected the techniques under investigation with respect to either SSDE or diagnostic performance.
Several study limitations were identified, including that the study was performed in a retrospective fashion. Radiologists were not blinded to patient history, vital signs, laboratory tests or other imaging study results, which may have influenced their CT interpretations. Furthermore, we cannot be certain how closely each radiologist followed standard CT criteria for diagnosing appendicitis. Nonetheless, these factors parallel actual radiology practice, apply to both groups equally and do not detract from the finding of preserved diagnostic accuracy between groups.
Some group A scans were performed on older CT models than the state-of-the-art scanners used for group B. Technical differences other than image noise (e.g., increased patient motion associated with slower image acquisition) could have influenced diagnostic performance on the older scanners. Yet, this limitation would not have influenced performance in group B, the group of primary interest.
Factors that may have affected accuracy with respect to clinical diagnosis of appendicitis include lack of a gold standard in patients who did not undergo appendectomy, variability in the length and amount of clinical follow-up, and variable interval between imaging and surgery. Additionally, some patients could have received follow-up treatment elsewhere without our knowledge, leading to overestimation of our diagnostic performance. Both study groups were equally susceptible to these effects.
Diagnostic accuracy of CT in pediatric patients weighing 82 kg (180 pounds) or more was not evaluated. Due to insufficient numbers, data regarding CT diagnosis of appendicitis in patients weighing less than 9 kg is also inconclusive. Both of these patient groups require further study.
The study did not isolate the effects of CTDIvol reduction and iterative reconstruction technique on diagnostic performance. Therefore, we cannot conclude that an equivalent CTDIvol reduction in the absence of iterative reconstruction technique would have resulted in non-diagnostic images. However, the finding that SSDE in group B was below published diagnostic reference ranges for all body widths (Table 2) argues that image quality in this group would have been substandard had iterative reconstruction technique not been applied. Diagnostic reference ranges were established by evaluation of CT scans reconstructed with filtered back projection alone, and their lower limit indicates the dose that should be exceeded in order to achieve the “image quality necessary to provide an accurate diagnosis” [13]. As diagnostic reference ranges are reconsidered in light of iterative reconstruction technique, this lower limit will likely shift downward, at least in the setting of acute appendicitis.
Other iterative reconstruction technique software may perform differently than iDose4, and baseline CTDIvol will affect the degree to which image quality is altered by a given dose reduction. Therefore, our results may not be directly transferrable to all imaging centers. Implementation of similar protocol changes should be performed in collaboration with a qualified medical physicist with attention to CT scanner specifications, available iterative reconstruction algorithms, baseline CTDIvol, objective quality measures and diagnostic performance indices. We anticipate that sites with baseline CTDIvol similar to or higher than ours will have similar results. At sites with lower baseline CTDIvol, staged CTDIvol reductions of lesser magnitude would be prudent, followed by reassessment.
Conclusion
Addition of iterative reconstruction technique and a 46% reduction in CTDIvol to the hospital’s traditional pediatric CT protocols resulted in no loss of sensitivity, specificity or accuracy in the diagnosis of acute appendicitis.
Acknowledgements
Dr. Didier is supported by National Institute of Biomedical Imaging and Bioengineering grant #1R25EB016671.
Footnotes
Conflicts of interest None
Contributor Information
Ryne A. Didier, Department of Diagnostic Radiology, DC7R, Oregon Health & Science University, 3181 S.W. Sam Jackson Park Road, Portland, OR 97239, USA
Petra L. Vajtai, Department of Diagnostic Radiology, DC7R, Oregon Health & Science University, 3181 S.W. Sam Jackson Park Road, Portland, OR 97239, USA Department of Pediatrics, Oregon Health & Science University, Portland, OR, USA.
Katharine L. Hopkins, Email: hopkinsk@ohsu.edu, Department of Diagnostic Radiology, DC7R, Oregon Health & Science University, 3181 S.W. Sam Jackson Park Road, Portland, OR 97239, USA; Department of Pediatrics, Oregon Health & Science University, Portland, OR, USA.
References
- 1.Callahan MJ, Rodriguez DP, Taylor GA. CT of appendicitis in children. Radiology. 2002;224:325–332. doi: 10.1148/radiol.2242010998. [DOI] [PubMed] [Google Scholar]
- 2.York D, Smith A, Phillips JD, von Allmen D. The influence of advanced radiographic imaging on the treatment of pediatric appendicitis. J Pediatr Surg. 2005;40:1908–1911. doi: 10.1016/j.jpedsurg.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Martin AE, Vollman D, Adler B, Caniano DA. CT scans may not reduce the negative appendectomy rate in children. J Pediatr Surg. 2004;39:886–890. doi: 10.1016/j.jpedsurg.2004.02.034. discussion 890. [DOI] [PubMed] [Google Scholar]
- 4.Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 5.Taylor GA, Wesson DE. Acute appendicitis in children: diagnostic imaging. In: Singer JI, Wiley JF, editors. UpToDate®. Philadelphia, PA: Wolters Kluwer Health; 2013. [Accessed 18 December 2013]. http://www.uptodate.com. [Google Scholar]
- 6.Krishnamoorthi R, Ramarajan N, Wang NE, et al. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA. Radiology. 2011;259:231–239. doi: 10.1148/radiol.10100984. [DOI] [PubMed] [Google Scholar]
- 7.Hopkins KL, Pettersson DR, Koudelka CW, et al. Size-appropriate radiation doses in pediatric body CT: a study of regional community adoption in the United States. Pediatr Radiol. 2013;43:1128–1135. doi: 10.1007/s00247-013-2680-7. [DOI] [PubMed] [Google Scholar]
- 8.Koninklijke Philips Electronics NV. iDose4 iterative reconstruction technique: breakthrough in image quality and dose reduction with the 4th generation of reconstruction. [Accessed 3 January 2013];2011 http://www.healthcare.philips.com/pwc_hc/main/shared/Assets/Documents/ct/idose_white_paper_452296267841.pdf. [Google Scholar]
- 9.Willemink MJ, de Jong PA, Leiner T, et al. Iterative reconstruction techniques for computed tomography. Part I: Technical principles. Eur Radiol. 2013;23:1623–1631. doi: 10.1007/s00330-012-2765-y. [DOI] [PubMed] [Google Scholar]
- 10.Mahesh M. Advances in CT technology and application to pediatric imaging. Pediatr Radiol. 2011;41:S493–S497. doi: 10.1007/s00247-011-2169-1. [DOI] [PubMed] [Google Scholar]
- 11.Siegel MJ, Schmidt B, Bradley D, et al. Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology. 2004;233:515–522. doi: 10.1148/radiol.2332032107. [DOI] [PubMed] [Google Scholar]
- 12.Karmazyn B, Liang Y, Klahr P, Jennings SG. Effect of tube voltage on CT noise levels in different phantom sizes. AJR Am J Roentgenol. 2013;200:1001–1005. doi: 10.2214/AJR.12.9828. [DOI] [PubMed] [Google Scholar]
- 13.Goske MJ, Strauss KJ, Coombs LP, et al. Diagnostic reference ranges for pediatric abdominal CT. Radiology. 2013;268:208–218. doi: 10.1148/radiol.13120730. [DOI] [PubMed] [Google Scholar]
- 14.Strauss KJ, Goske MJ. Estimated pediatric radiation dose during CT. Pediatr Radiol. 2011;41:S472–S482. doi: 10.1007/s00247-011-2179-z. [DOI] [PubMed] [Google Scholar]
- 15.American Association of Physicists in Medicine. College Park: American Association of Physicists in Medicine; 2011. Size specific dose estimates (SSDE) in pediatric and adult body CT examinations (Report No. 204) [Google Scholar]
- 16.Matsuno WC, Anaya R, Tay ET, et al. Computed tomographic scan diagnosis of appendicitis in children by pediatric and adult radiologists. Pediatr Emerg Care. 2012;28:265–267. doi: 10.1097/PEC.0b013e3182494fce. [DOI] [PubMed] [Google Scholar]
- 17.Garcia K, Hernanz-Schulman M, Bennett DL, et al. Suspected appendicitis in children: diagnostic importance of normal abdominopelvic CT findings with nonvisualized appendix. Radiology. 2009;250:531–537. doi: 10.1148/radiol.2502080624. [DOI] [PubMed] [Google Scholar]
- 18.Griner PF, Mayewski RJ, Mushlin AI, et al. Selection and interpretation of diagnostic tests and procedures. Principles and applications. Ann Intern Med. 1981;94:557–592. [PubMed] [Google Scholar]