Abstract
This study examined a 24-year-old patient with delayed encephalopathy, who was admitted to hospital with complaints of headache and visual impairment 1 week after acute carbon monoxide poisoning. The results of a visual field assessment, electroencephalography and head magnetic resonance imaging indicated damage to the cerebral cortex. After a 2-week treatment period, the patient had recovered from the visual impairment, but exhibited digit- and letter-reading difficulty. The Chinese aphasia battery and the number and letter battery supplement were conducted. The results revealed that the patient exhibited digit and letter alexia, while the ability to read Chinese characters was preserved. In contrast, the patient exhibited a deficit in Chinese character writing, while number and letter writing remained intact. Following treatment, reading and writing ability was improved and electroencephalographic abnormalities were ameliorated. Overall, our experimental findings demonstrated that delayed encephalopathy following acute carbon monoxide poisoning was characterized by digit and letter alexia.
Keywords: carbon monoxide, delayed encephalopathy, digit alexia, letter alexia, poisoning, neural regeneration
Research Highlights
A case of delayed encephalopathy, presenting with headache and visual impairment after acute carbon monoxide poisoning, was examined.
INTRODUCTION
Carbon monoxide poisoning is the fourth most common type of poisoning in China[1], and is a leading cause of neurological disturbances[2]. The psychiatric and neurological symptoms of carbon monoxide poisoning include headache, muscle weakness, drowsiness, memory disturbances, apraxia, delirium, speech disorder, epileptic seizure, ataxia, and symptoms of Parkinsonism[3,5]. Most symptoms are non-specific, and some appear after a delay period[6,8]. Nevertheless, selective alexia has seldom been documented. The causes of dyslexia are poorly understood, but have been linked to damage to a reading-specific brain region in the left hemisphere known as the visual speech area. In this study, we describe a case of delayed encephalopathy with digit and letter alexia following carbon monoxide poisoning.
CASE REPORT
General patient information (Table 1)
Table 1.
General patient information

Diagnosis
The patient was diagnosed with delayed encephalopathy after acute carbon monoxide poisoning. Treatments included hyperbaric oxygen therapy, as well as a low dose of methylprednisolone (80 mg a day) and drugs for neurotrophy. This project was approved by the Administrative Regulations on Medical Institution, formulated by the State Council of the People's Republic of China[11]. Written informed consent was obtained from the patient prior to the study.
At admission, the patient complained of visual impairment, as well as digit and letter alexia after acute carbon monoxide poisoning. All symptoms appeared to be related to cortical injury. Other common diseases that cause acute focal cortical injury include stroke (ischemia and hemorrhage), trauma, and metabolic diseases (such as mitochondrial encephalomyopathy). Li et al[12] reported a case of digit alexia after left parietal lobe hemorrhage.
In the current study, cranial MRI did not support the diagnosis of stroke and metabolism diseases (Figure 2). The clinical history did not provide information indicating the development of alexia, except after the carbon monoxide poisoning. Successful treatment of delayed encephalopathy after acute carbon monoxide poisoning also supported the diagnosis.
Figure 2.

Brain imaging examination.
T2-weighted brain magnetic resonance imaging (A) and magnetic resonance angiography (B) at 8 days after carbon monoxide intoxication revealed no abnormal findings. R: Right.
Figure 1.

Visual impairment of the patient before and after treatment.
Visual field examination was performed at day 2 when the patient was admitted to the hospital. Right homonymous hemianopia was evident in both eyes pre-treatment (A). After 2 weeks of treatment, the patient's visual deficit had fully recovered (B).
Figure 3.

Electroencephalography at 10 days after carbon monoxide poisoning.
Widespread 6.5 – 7.5 Hz slow wave activity with low amplitude could be seen.
When the patient was discharged from the hospital, electroencephalography revealed apparent improvement, and 8 – 9 Hz α wave activity returned as the predominant background rhythm.
Figure 4.

The patient was asked to write his name, address and occupation.
Before treatment, the patient was unable to complete this task. After treatment, the patient completed the task accurately.
Figure 5.
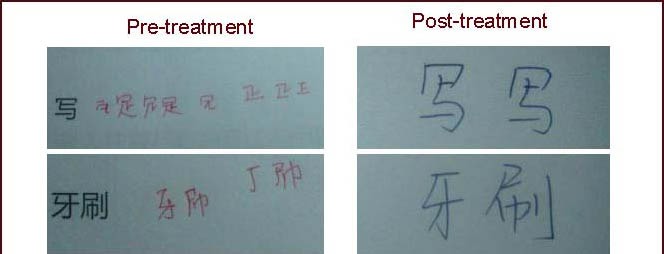
The patient was asked to copy the Chinese words shown on the left.
The patient exhibited difficulty before treatment, but not after treatment.
DISCUSSION
The symptoms of carbon monoxide poisoning are nonspecific. Delayed encephalopathy typically occurs suddenly after a lucid interval following acute exposure. Common symptoms of delayed encephalopathy include memory loss, cognitive dysfunction and neuropsychological impairment due to cerebral cortex damage, as well as pyramidal and extrapyramidal syndromes involving the globus pallidus and subcortical white matter.
In a number evaluation task, the patient was unable to read eight out of ten formulas or ten out of twenty numbers in the hundreds. In addition, he could not correctly recognize the digits of any numbers in the thousands. Most of these errors were not due to simple visual spatial impairment, which is typically exhibited as mistakenly recognizing “9” as “6”, or “13” as “31”. The present results indicated that our patient's condition was related to an impairment of the connection between visual identification and reading of numbers.
The specific brain regions underlying the patient's impaired letter and number reading ability, but preserved Chinese character reading ability, are currently unclear. The cerebral cortex is known to be susceptible to anoxia. Previous studies have reported that damage to the cortex, globus pallidus, cerebral deep white matter, putamen, caudate nucleus, thalamus and hippocampus exhibit abnormalities that are observable on magnetic resonance imaging scans in cases of delayed encephalopathy[13,14]. In the current study, no abnormality was observed on magnetic resonance imaging and magnetic resonance angiography scans, which eliminates the diagnosis of stroke or metabolic diseases. Electroencephalography was used to record the electrical activity of the brain. Although it may not be possible to determine the nature of the disease by the appearance of the electroencephalographic signal alone, diffuse slow wave activity in a conscious person typically indicates injury to the whole cortex in varying degrees. This measure may be more sensitive than magnetic resonance imaging. In the current patient, a partial defect in the visual field and widespread low amplitude θ wave on electroencephalography were observed, indicating neurological dysfunction of the cerebral cortex.
The cause of the patient's letter and number alexia, but preserved Chinese character reading, remains unclear. This pattern of performance has not been previously reported, although there have been reports of selective alexia such as Hangja alexia[15], Japanese alexia[16], selective alexia and agraphia sparing numbers[17,18]. Some studies have suggested that the processing of ideograms and phonograms may be mediated by different brain regions. In addition, letter and number reading appear to be dependent on dissociable processes[19]. Despite the difficulties in localizing the selective alexia exhibited by our patient, we propose that focal cortical dysfunction may account for the findings of the visual field test and electroencephalography. Functional MRI revealed activation of a wide area including left inferior/middle frontal gyri, bilateral medial frontal gyri, posterior inferior temporal area, bilateral middle occipital/fusiform gyri, and the bilateral cerebellum during Chinese letter reading[20,21,22]. Previous studies have indicated that Chinese characters involve more complicated neural connections compared with English letters and numbers[20]. As such, the latter may exhibit more impairment and less compensation after brain injury, because the functional brain area is relatively limited and is more likely to suffer complete damage. Recovery of writing skill is reported to be more difficult than the recovery of listening, reading or speaking[12]. This may explain why the patient's Chinese writing ability only partially recovered after treatment, whereas his reading ability completely recovered. A less complicated and less extensive brain network is involved in the reading of numbers and letters compared with that involved in reading Chinese words[23], so less compensation may be seen after injury. This may explain why number and letter reading were more difficult to recover in the present study.
Footnotes
Funding: This work was supported by National Natural Science Foundation of China (No. 81072242), Natural Science Foundation of Guangdong Province (No. S2011010004708), the Fundamental Research Funds for the Central Universities, Funds for Pearl River Science & Technology Star of Guangzhou City, Natural Science Foundation of Guangdong Province (No. 10151130001000001), and Science and Technology Project of Guangzhou (No. 2010Y1-C191).
Conflicts of interest: None declared.
Ethical approval: This study was approved by the Ethics Committee, Sun Yat-sen Memorial Hospital in China.
(Edited by Wang XP, Li Y/Yang Y/Song LP)
REFERENCES
- [1].Jiang W, Wu CM, Deng X, et al. Analysis of poisoning cases from Chinese National Injury Surveillance System, 2006-2008. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31(9):1009–1012. [PubMed] [Google Scholar]
- [2].Weaver LK. Clinical practice. Carbon monoxide poisoning. N Engl J Med. 2009;360(12):1217–1225. doi: 10.1056/NEJMcp0808891. [DOI] [PubMed] [Google Scholar]
- [3].Lucas D, Lodde B, Jegaden D, et al. Occupational poisoning by carbon monoxide aboard a gas carrier. Report on 8 cases. Int Marit Health. 2010;62(3):176–179. [PubMed] [Google Scholar]
- [4].Fielding J, Lang W, White OB. Carbon monoxide poisoning: impact on ocular motility. Cogn Behav Neurol. 2010;23(4):256–261. doi: 10.1097/WNN.0b013e3181c5e2c1. [DOI] [PubMed] [Google Scholar]
- [5].Song IU, Chung SW. Chorea as the first neurological symptom of delayed encephalopathy after carbon monoxide intoxication. Intern Med. 2010;49(11):1037–1039. doi: 10.2169/internalmedicine.49.3210. [DOI] [PubMed] [Google Scholar]
- [6].Hsiao CL, Kuo HC, Huang CC. Delayed encephalopathy after carbon monoxide intoxication-long-term prognosis and correlation of clinical manifestations and neuroimages. Acta Neurol Taiwan. 2004;13(2):64–70. [PubMed] [Google Scholar]
- [7].Kwon OY, Chung SP, Ha YR, et al. Delayed postanoxic encephalopathy after carbon monoxide poisoning. Emerg Med J. 2004;21(2):250–251. doi: 10.1136/emj.2002.002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Choi IS, Cheon HY. Delayed movement disorders after carbon monoxide poisoning. Eur Neurol. 1999;42(3):141–144. doi: 10.1159/000008088. [DOI] [PubMed] [Google Scholar]
- [9].Chang DC, Lee JT, Lo CP, et al. Hyperbaric oxygen ameliorates delayed neuropsychiatric syndrome of carbon monoxide poisoning. Undersea Hyperb Med. 2010;37(1):23–33. [PubMed] [Google Scholar]
- [10].Gao SR. Exposition of standardized aphasia battery in Chinese. Lin Chuang Shen Jing Bing Xue Za Zhi. 1992;5(4):193–195. [Google Scholar]
- [11].State Council of the People's Republic of China. Administrative Regulations on Medical Institution. 1994 [Google Scholar]
- [12].Li R, Gao SR. A case of left parietal hemorrhage after digital alexia. Zhong Feng Yu Shen Jing Ji Bing Za Zhi. 1996;13(5):299–300. [Google Scholar]
- [13].Lin WC, Lu CH, Lee YC, et al. White matter damage in carbon monoxide intoxication assessed in vivo using diffusion tensor MR imaging. Am J Neuroradiol. 2009;30(6):1248–1255. doi: 10.3174/ajnr.A1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kim JH, Chang KH, Song IC, et al. Delayed encephalopathy of acute carbon monoxide intoxication: diffusivity of cerebral white matter lesions. Am J Neuroradiol. 2003;24(8):1592–1597. [PMC free article] [PubMed] [Google Scholar]
- [15].Kwon JC, Lee HJ, Chin J, et al. Hanja alexia with agraphia after left posterior inferior temporal lobe infarction: a case study. J Korean Med Sci. 2002;17(1):91–95. doi: 10.3346/jkms.2002.17.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sugishita M, Otomo K, Kabe S, et al. A critical appraisal of neuropsychological correlates of Japanese ideogram (kanji) and phonogram (kana) reading. Brain. 1992;115(Pt 5):1563–1585. doi: 10.1093/brain/115.5.1563. [DOI] [PubMed] [Google Scholar]
- [17].Starrfelt R. Selective alexia and agraphia sparing numbers-a case study. Brain Lang. 2007;102(1):52–63. doi: 10.1016/j.bandl.2006.09.005. [DOI] [PubMed] [Google Scholar]
- [18].Marangolo P, Nasti M, Zorzi M. Selective impairment for reading numbers and number words: a single case study. Neuropsychologia. 2004;42(8):997–1006. doi: 10.1016/j.neuropsychologia.2004.01.004. [DOI] [PubMed] [Google Scholar]
- [19].Park J, Hebrank A, Polk TA, et al. Neural dissociation of number from letter recognition and its relationship to parietal numerical processing. J Cogn Neurosci. 2012;24(1):39–50. doi: 10.1162/jocn_a_00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chee MW, Weekes B, Lee KM, et al. Overlap and dissociation of semantic processing of Chinese characters, English words, and pictures: evidence from fMRI. Neuroimage. 2000;12(4):392–403. doi: 10.1006/nimg.2000.0631. [DOI] [PubMed] [Google Scholar]
- [21].Booth JR, Lu D, Burman DD, et al. Specialization of phonological and semantic processing in Chinese word reading. Brain Res. 2006;1071(1):197–207. doi: 10.1016/j.brainres.2005.11.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yoon HW, Chung JY, Kim KH, et al. An fMRI study of Chinese character reading and picture naming by native Korean speakers. Neurosci Lett. 2006;392(1-2):90–95. doi: 10.1016/j.neulet.2005.09.027. [DOI] [PubMed] [Google Scholar]
- [23].Piras F, Marangolo P. Word and number reading in the brain: evidence from a voxel-based lesion-symptom Mapping study. Neuropsychologia. 2009;47(8-9):1944–1953. doi: 10.1016/j.neuropsychologia.2009.03.006. [DOI] [PubMed] [Google Scholar]


