Summary
Aim of the study
Solitary central osteomas of the jaw seem to be especially rare lesions; since 1955, only 12 cases have been reported and 4 of these were located in the maxilla.
Osteomas are benign osteogenic lesions considered as real tumours but without infiltrative or metastatic potential. Their growth potential is usually limited, but certain rare and large cases of peripheral osteoma are described in literature. Although surgery is recommended, there are no reports of malignant transformation. In this study, we describe successful implant rehabilitation in a patient with a central osteoma of the maxilla with immediate loading in a fresh extraction socket.
Materials and methods
The report concerns a 33-year-old woman with a compromised deciduous first molar in the left premolar region of the maxilla; an asymptomatic bony expansion of the palatal and vestibular sides of the left canine/premolar/molar area of the maxilla and by radiograph revealed a well-defined radiopaque mass. An immediate non-occlusal loading was performed, and complete loading of the implant was completed five months later.
Discussion and conclusion
The pathogenesis of these osteomas is unclear. Several authors reported a clear history of traumatic events, but others had no history of previous trauma or contributory medical factors. Since in our case no cancer growth happened over a period of more than four years, we decided to perform an immediate loading procedure during the implant rehabilitation. The outcome was successful.
Keywords: osteoma, central osteoma, peripheral osteoma, immediate loading
Introduction
An osteoma is a rare, benign, osteogenic tumour consisting of compact mature or cancellous bone.
Three types can be identified: a peripheral (periosteal) osteoma develops as a peripheral mass attached to the cortical plate; a central osteoma arises from an endosteal bone surface; extra-skeletal soft tissue osteoma. These types of osteomas are most frequently localised in facial bones. The mandible is involved in the majority of cases described in the literature, particularly the lingual aspect of the body, the angle, and the inferior border. Solitary central osteomas, of the jaw are less frequent than peripheral osteomas, and to our knowledge, only 12 cases have been reported since 1955.
Although aetiology is unknown in some cases, it can be related to traumatic injuries or inflammatory processes associated with systemic diseases, such as encephalocraniocutaneous lipomatosis (ECCL).
Multiple jaw osteomas are typical manifestations of Gardener’s syndrome, which is also characterised by enostoses, dense bone islands, odontomas, and supernumerary or unerupted teeth. Outside this syndrome, craniofacial bone osteomas are solitary lesions.
Histologically, osteomas are found in dense compact bone with few marrow spaces (compact osteoma) or bony trabeculae and fibro-fatty marrow with enclosing fibroblasts and mature bone-like architecture (cancellous osteoma).
Diagnosing a central osteoma is particularly challenging because there are many similar jaw lesions, such as osteochondroma, fibrous dysplasia, chondroma, central ossifying fibroma, condensing osteitis, tori and exostoses, idiopathic osteosclerosis, osteoblastoma, cementoblastoma, complex odontoma, and dense bone islands.
Although surgery is recommended, there are no reports of malignant transformations in the literature.
The purpose of this article is to describe the successful implant rehabilitation in a patient with a central osteoma of the maxilla with immediate loading in a fresh extraction socket.
Clinical case
A 33-year-old woman was referred to the oral department of our hospital to replace a compromised deciduous first molar in the left premolar region of the maxilla. Intraoral examination revealed an asymptomatic bony expansion of the palatal and vestibular sides of the left canine/premolar/molar area of the maxilla. The overlying mucosa was intact with normal coloration. A panoramic radiograph revealed a well-defined radiopaque mass without a radiolucent rim located around and subjacent to the roots of all teeth from the canine to the third molar and involving the entire structure of the impacted first premolar (Fig. 1). Involvement of the paranasal sinus was also noted. A computed tomography scan determined that the mesio-distal length was 51 mm, and the bucco-palatal expansion was 22 mm in the second molar region. Based on these results, the clinical and radiographic working diagnosis was a central osteoma. The patient was in good health with no history of previous trauma or contributing medical factors. There was no history of temporo-mandibular joint disease or malocclusion or signs of occlusal trauma. During the first surgery, the impacted first premolar was removed under general anaesthesia, and no graft material was used to fill the defect area. An excisional biopsy entirely included in the first premolar area of the lesion was performed at the same time, and the 3 × 3-mm fragment was submitted for histopathological examination (Figs. 2, 3). The biopsy revealed a mass entirely consisting of lamellar mature bone with no sign of inflammation or cartilaginous tissue (Fig. 4). The histological aspects were compatible with a compact central osteoma. Four years later, a second panoramic radiograph showed complete healing of the bone with dense compact radiopacity in the first premolar region (Fig. 5). A second computed tomography scan did not show evidence of central osteoma expansion (Fig. 6). The patient was admitted for a second surgical intervention, and the deciduous first premolar was removed and replaced with a 3.6 × 13-mm implant (TSA® Advance, DEFCON Tissue Care®) placed in the fresh extraction socket under local anaesthesia. The implant was immediately loaded without any contact with the opposite dentition (Fig. 7). Sutures were removed after one week showing good softissue healing (Fig. 8). Five months later, a third panoramic radiograph showed direct contact between the bone radiopacity and the entire implant surface (Fig. 9), which was compatible with osseointegration.
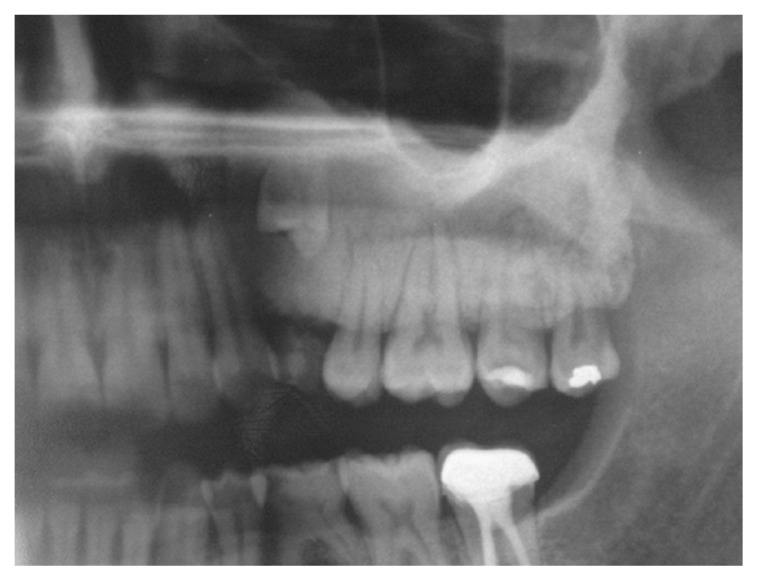
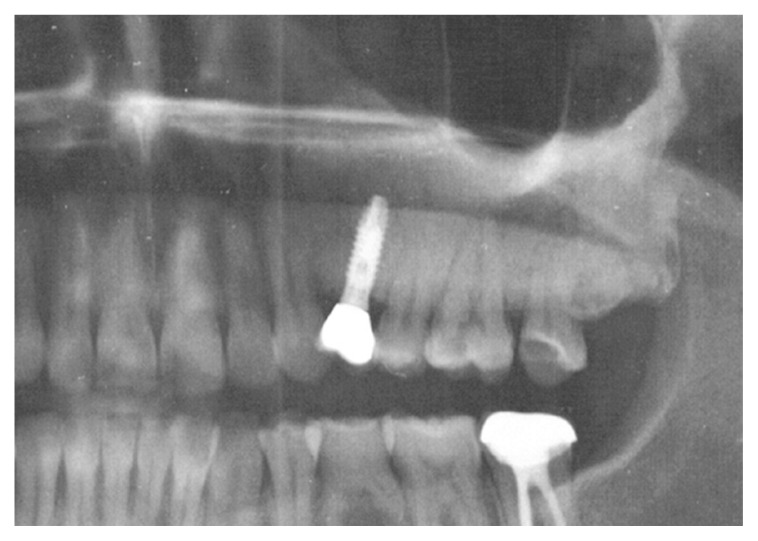
Figure 1.
Detail from the panoramic radiograph showing a well-defined radiopaque mass without a radiolucent rim located around and subjacent to the roots of all teeth from the canine to the third molar. The entire structure of the impacted first premolar is involved.
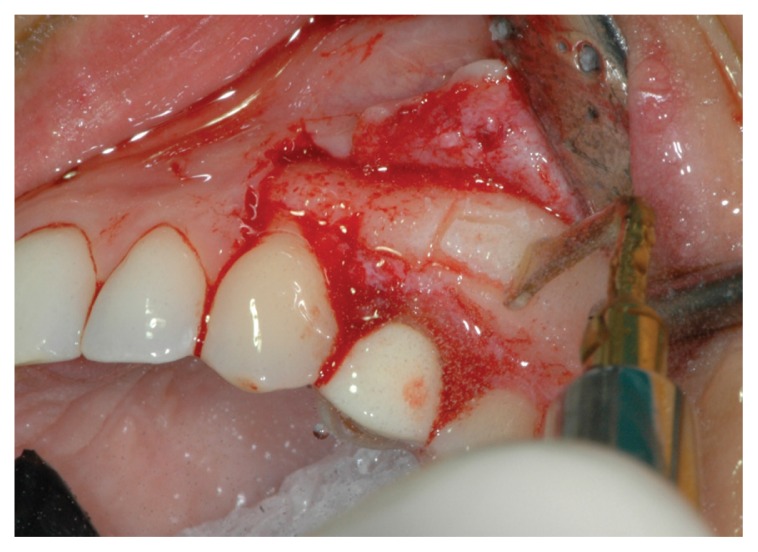
Figure 2.
Piezoelectric harvesting of a 3 × 3 mm bone fragment in the first premolar area. The margins of the excisional biopsy are all included in the lesion.
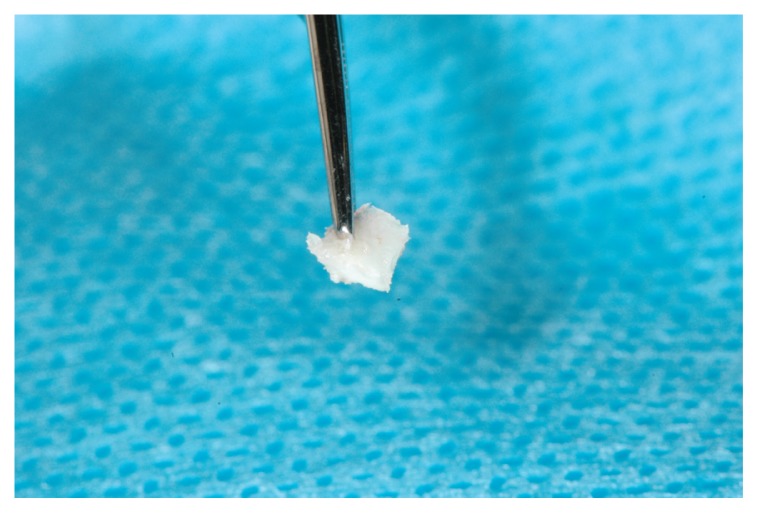
Figure 3.
Closer view of the biopsy fragment.
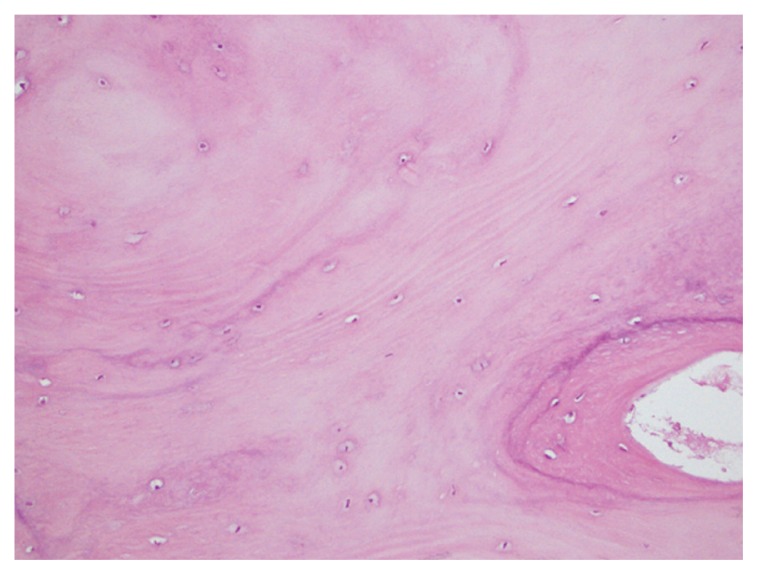
Figure 4.
Biopsy showed a mass consisting entirely of mature, lamellar bone and no sign of inflammation or cartilaginous tissue.
Figure 5.
Panoramic radiograph showing complete healing of the bone with dense compact radiopacity in the first premolar region four years after first surgery.
Figure 6.
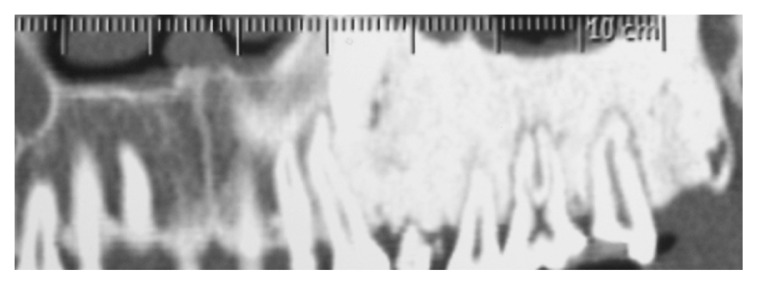
Computed tomography scan performed four years after extraction of the impacted premolar showing complete healing of the bone with dense compact radiopacity in the first premolar region and no change in central osteoma size.
Figure 7.
The deciduous first premolar was removed under local anaesthesia, and a 3.6 × 13 mm implant was placed in the fresh extraction socket and immediately loaded without any contact with the opposite dentition.
Figure 8.
One week after implant placement there is a good integration between provisional restoration end soft tissues.
Figure 9.
A panoramic radiograph taken five months after implant placement shows direct contact between the bone radiopacity and the entire implant surface.
The provisional crown was removed, and the implant was fully loaded with a definitive abutment and a cemented metal-ceramic restoration (Fig. 10).
Figure 10.
Detail from a panoramic radiograph taken one year after complete loading of the implant.
Discussion and conclusion
Central osteomas are benign osteogenic lesions considered to be real tumours that lack infiltrative or metastatic potential (1–3). These osteomas are, in fact, bone-within-bone lesions (2–4), but they have not been reported to undergo malignant transformations (4, 5).
The pathogenesis of these osteomas is unclear. Several authors reported a clear history of traumatic events, but others did not relate them to a history of previous trauma or contributory medical factors. In 2005, Zielinska-Kazamierska et al. (3) published a case of a solitary central osteoma of the mandible in a patient with encephalocraniocutaneous lipomatosis (ECCL), which also presented many other craniofacial abnormalities. Although ECCL pathogenesis is also unknown, Kaplan et al. (2) observed that the opposing teeth seem grossly overerupted, and in view of a history of seizures, trauma may contribute to jaw infection.
In 2011, Santos et al. (1) reported a case where the lesion was found in a site of previous extraction and suggested that the tooth removal may have triggered excessive, localised growth of the endosteal osteoblasts which led to the development of central osteoma.
The neoplastic nature of these lesions is supported by their slowl, continuous growth. Therefore, although both peripheral and central osteomas usually have limited growth potentials, some of these lesions can reach large dimensions.
Solitary central osteomas of the jaw seem to be particularly rare; few cases have been reported in the international literature in English language. Since 1955, only 12 cases have been reported, and only four concerned the maxilla, including one in the anterior maxilla (Rajayogeswaranav and Evson 1981) (6), one in the premolar region with sinus involvement (Firat et al. 2005) (7), and two in the premolar/molar region of the maxilla, one of which involved the paranasal sinus (Kaplan et al. 2008, Santos et al. 2011) (1, 2). A recent study published by Larrea-Oyarbide et al. (2008) (8) described 132 osteomas of the craniofacial region that were not considered for the same reasons presented by Bulut et al. (4) in 2010 and Kaplan et al. in 2008 (2). Thus, this case is the fifth reported case of a solitary central osteoma of the maxilla.
Except in cases in which the lesion is sufficiently large or symptomatic, central osteomas are usually detected by a routine radiographic survey. In the previously reported cases, patient age ranged from 13 to 67 years with a mean age of 42 years, and there was no sex bias (female to male ratio of 1:1).
Microscopically, central and peripheral osteomas are composed of normal compact or trabecular mature bone or a combination of both (2). Radiographically, these osteomas appear as uniform radiopaque masses with well-defined borders and can often be related to impaction or root displacement. A single case of root resorption caused by a central osteoma was reported by Bulut et al. in 2010 (4). Usually, root resorption is a rare complication associated with idiopathic osteosclerosis, which are asymptomatic, intrabony, radiopaque lesions of unknown origin that correspond to dense, trabeculated, non-inflamed vital bone on a histological evaluation (9). On radiographs, these lesions are well delineated from the surrounding normal bone and can be smooth or irregular in outline (10). These idiopathic lesions have a distribution similar to osteomas, with mandibular predilection that varies between 89.3 and 100% primarily in the premolar molar region (9–11). Although sometimes they are described as dense bone islands, bone scar, focal peri-apical osteopetrosis, or enostoses, the term idiopathic osteosclerosis is preferred because it implies that the origin is unknown (12). These lesions can reach 7 cm in dimension without bone expansion (10). Distinguishing between central osteoma and idiopathic osteosclerosis is challenging because they have similar histological and radiographic properties. A diagnosis for a central osteoma requires evidence of growth, expansion, or root displacement (4). However, diagnoses can be difficult or impossible in young patients if expansion or displacement does not occur.
Similar radiopaque foci may develop in peri-apical areas of non-vital teeth as a reaction to inflammatory disease of the pulp. These non-expansile lesions are designated as condensing osteitis or focal chronic sclerosing osteomyelitis (13).
In our case, the expansion was sufficient to support a diagnosis of central osteoma.
However, osteochondroma should be included in differential diagnoses. Together with chondroma and osteoma, it is one of the most common benign condylar tumours, but macroscopic analysis reveals bone proliferation with a hyaline cartilage cap, and histology shows a normal osteochondral junction (14).
Although surgery is recommended for central osteomas, there are no reports of malignant transformation in the literature (4, 5). In the case of a central osteoma of the mandible in a patient with encephalocraniocutaneous lipomatosis published in 2005, Zielinska-Kazamierska et al. (3) specified that mandibular resection was necessary due to the extent of the lesion, rather than its character. In 2005, Kerkhaert et al. (5) reported that surgical treatment is only indicated in patients with clinical symptoms. In the present case, we decided not to enucleate the lesion, because despite a mesio-distal extension of 51 mm, the bucco-palatal expansion did not cause any malocclusion or malfunction. Moreover, the lesion was asymptomatic and had an extremely low growth potential. As Kaplan et al. (2) reported in 2008, although a number of rare, large cases of peripheral osteomas have been described in the literature, their growth potential is usually limited. In our case, radiographic three-dimensional observation showed that no growth had occurred over a period of more than four years.
We decided to perform an immediate loading procedure during the implant rehabilitation. No implant site under-preparation was needed to decrease the risk of early implant failure because the patient had high bone density, which suggested we would achieve optimal primary stability. During the surgical procedure, mesio-distal and bucco-palatal ISQ values were determined to be 64 and 63, respectively.
Two types of immediate implant loading are described in the literature: immediate non-occlusal loading and immediate occlusal loading. The main difference is the complete absence of contact between the provisional prosthesis and the opposite dentition in non-occlusal loading. In their literature review, Esposito et al. (15) compared the success rate of immediate non-occlusal versus occlusal loading and concluded that it is unclear whether it is beneficial or not to avoid occlusal contact during the osseointegration phase, and a high degree of primary implant stability (high insertion torque value) seems to be one of the prerequisites for a successful procedure.
In our case, an immediate non-occlusal loading was performed, and complete loading of the implant was completed five months later.
Acknowledgements
We thank the operating unit of Anatomy - Pathological S. Gerard Hospital in Monza, Director Prof. Dr. Giorgio Cattoretti and Maria Gabriella Valente, for their kind cooperation.
There are no funding sources that supported the work as well as institutional or corporate affiliations with the authors.
References
- 1.Santos TS, Frota R, Martins-Filho PRS, Melo AR, Melo AR, Andrade ESS, Silva EDO, Avelar RL. Central osteoma of the maxilla with involvement of paranasal sinus. J Craniofac Surg. 2011;22:589–591. doi: 10.1097/SCS.0b013e318208555d. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan I, Nicolaou Z, Hatuel D, Calderon S. Solitary central osteomas of the jaws: a diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e22–e29. doi: 10.1016/j.tripleo.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Zielinska Kazamierska B, Grodecka J, Jabonska-Polakowsaka L, Arkuzewski P. Mandibular osteoma in the encephalocraniocutaneous lipomatosis. J Craniomaxillofac Surg. 2005;33:286–9. doi: 10.1016/j.jcms.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Bulut E, Ozan B, Gunhan O. Central osteoma associated with root resorption. J Craniofacial Surg. 2010;21:419–421. doi: 10.1097/SCS.0b013e3181cfa7d7. [DOI] [PubMed] [Google Scholar]
- 5.Kerckhaert A, Wolvius E, Van der wal K, Oosterhuisa J. W Giant osteoma of the mandible: case report. J Craniomaxillofac Surg. 2005;33:282–5. doi: 10.1016/j.jcms.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Rajayogeswaranav V, Evson JW. Endosteal (central) osteoma of the maxilla. Br Dent J. 1981;150:162–3. doi: 10.1038/sj.bdj.4804562. [DOI] [PubMed] [Google Scholar]
- 7.Firat D, Sirin Y, Bilgic B, Ozyuvaci H. Large central osteoma of the maxillary antrum. Dentomaxillofac Radiol. 2005;34:322–5. doi: 10.1259/dmfr/15263929. [DOI] [PubMed] [Google Scholar]
- 8.Larrea-Oyarbide N, Valmaseda-Castellon E, Berini-Aytes L, et al. Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med. 2008;37:38–42. doi: 10.1111/j.1600-0714.2007.00590.x. [DOI] [PubMed] [Google Scholar]
- 9.Petrikowski CG, Peters E. Longitudinal radiographic assessment of dense bone islands of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:627–34. doi: 10.1016/s1079-2104(97)90131-1. [DOI] [PubMed] [Google Scholar]
- 10.Kawai T, Murakami S, Kishino M, Sakuda M. Gigantic dense bone island of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:108–15. doi: 10.1016/s1079-2104(96)80387-8. [DOI] [PubMed] [Google Scholar]
- 11.Yonetsu K, Yuasa K, Kanda S. Idiopathic osteosclerosis of the jaws: panoramic radiographic and computed tomographic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:517–21. doi: 10.1016/s1079-2104(97)90156-6. [DOI] [PubMed] [Google Scholar]
- 12.Sisman Y, Ertas ET, Ertas H, Sekerci AE. The frequency and distribution of idiopathic osteosclerosis of the jaw. Eur J Dent. 2011;5:409–414. [PMC free article] [PubMed] [Google Scholar]
- 13.Miloglu O, Yalcin E, Buyukkurt MC, Acemoglu H. The frequency and characteristics of idiopathic osteosclerosis and condensing osteitis lesions in a Turkish patient population. Med Oral Patol Oral Cir Bucal. 2009;1;14:640–5. doi: 10.4317/medoral.14.e640. [DOI] [PubMed] [Google Scholar]
- 14.González-Otero S, Navarro-Cuéllar C, Escrig-de Teigeiro M, Fernán-dez-Alba-Luengo J, Navarro-Vila C. Osteochondroma of the mandibular condyle: Resection and reconstruction using vertical sliding osteotomy of the mandibular ramus. Med Oral Patol Oral Cir Bucal. 2009;1;14:194–7. [PubMed] [Google Scholar]
- 15.Esposito M, Grusovin MG, Achille H, Coulthard P, Worthington HV. Intervention for replacing missing teeth: different times for loading dental impants (Review) Cochrane Database of Systematic Reviews. 2009;21 doi: 10.1002/14651858.CD003878.pub4. [DOI] [PubMed] [Google Scholar]