Abstract
Background:
A nosocomial outbreak in a 740-bed hospital in Athens, Greece, was investigated in January-February 2012.
Methods:
Recommendations on infection control measures were given and two case-control studies were conducted among patients (study A) and health care workers (HCWs) (study B). Compliance to control measures was evaluated.
Results:
The absence of a routine recording system of nosocomial-acquired gastroenteritis cases led to a 10 days delay in outbreak identification. In total, 63 gastroenteritis cases were identified; 30 HCWs and 33 patients. In the multivariable analysis of study A the disease incidence among patients was statistical significantly associated with a prior incident of vomitus in their room (OR=7.96, 95% CI=1.29-49.2). In study B, the incidence was associated with the history of direct contact with a symptomatic patient (OR=3.03, 95%CI 1.01-9.12). Twenty one (75%) of the symptomatic HCWs reported absence from work for a median of 2 days (range: 1-4). Seven (25.0%) continued to work despite being symptomatic. Only, 11.1% of patients were isolated or cohorted after developing symptoms. In-hospital virological testing was not feasible and one specimen sent to a university laboratory was positive for norovirus.
Conclusions:
An appropriately designed protocol regarding the detection, the management and the laboratory investigation of nosocomial gastroenteritis outbreaks should be followed in order effective containment to be reassured. Hippokratia 2014; 18 (3): 204-208.
Keywords: gastroenteritis, outbreak, nosocomial, hospital, norovirus
Introduction
Nosocomial viral gastroenteritis outbreaks have been increasingly documented the last years especially during winter and early spring1-4. The majority of such outbreaks is attributed to noroviruses; a genetically diverse group of viruses in the Caliciviridae family5 which are highly infectious, resistant to surface disinfectants and viable in the environment up to 12 days6,7. They are usually large and difficult to be contained and in most cases, the primary transmission route is person-to-person spread of the virus8-10. Even though viral gastroenteritis is usually mild, illness can be severe and prolonged in hospitalized patients especially immunocompromised, the elderly, and chronically-ill10-12.
On 23 January 2012 the Hellenic Center for Disease Control and Prevention (HCDCP) was informed about an outbreak of acute gastroenteritis among hospitalized patients and health-care workers (HCWs) in a large hospital in Athens. In this article, we present the main conclusions of the epidemiological investigation and management of the outbreak.
Methods
Outbreak setting
The outbreak occurred in a 740-bed, tertiary-care hospital in Athens, which consists of 15 buildings and 24 wards dispersed in an area of 428,000 m2. The hospital serves as a referral hospital providing services to a large number of patients, mainly elderly and patients with chronic pulmonary, cardiology, and oncology diseases.
Results of initial investigation and management
According to the physicians, symptoms were suggestive of viral gastroenteritis. Person-to-person transmission was suspected since cases had gradually derived from different wards of the same building and seemed to be dispersed. Stool specimens from gastroenteritis cases were bacteriologically tested but virological testing was not possible. Faecal samples were collected by all cases and were tested for Salmonella spp. and Shigella spp.
All wards were contacted for the retrospective identification of possible nosocomial-acquired cases since the beginning of the year and the head nurses were requested to daily report possible new cases among patients and personnel. Recommendations on infection control measures, such as hand hygiene, thorough sterilization of environment and equipment, and isolation and cohorting of symptomatic patients were given13. Symptomatic HCWs were asked not to return at work for a minimum of 48 hours after the resolution of their symptoms.
Epidemiological investigation
Two 1:1 case-control studies were conducted among hospitalized patients and HCWs (case-control studies A and B, respectively). Gastroenteritis cases that occurred after January 1, 2012 were recorded. Cases were defined as patients or HCWs that presented vomiting and/or diarrhoea after their admission to the hospital and the bacteriological testing (for Salmonella spp. and Shigella spp.) was negative. Patients that arrived at the hospital with gastroenteritis symptoms, or developed such symptoms within the first 12 hours of hospitalization and patients whose symptoms were attributed to another illness or were considered drug-related were excluded.
Controls were defined as patients or HCWs without a history of the aforementioned symptoms for at least two days before the interview. In study A, controls were selected from the same wards as the cases via simple random sampling, using the hospital registries and a random number table. The control group for case-control study B was randomly selected using a list of HCWs of each ward. Cases and controls in this latter study were matched by professional identity (physicians, nurses, and paramedical staff).
The structured questionnaire for study A included demographic and clinical characteristics and possible risk factors in relation to in-hospital practices and exposures (exposure to a roommate’s vomitus or diarrhoea, patient's transfers to/from other wards, isolation or cohorting of symptomatic patients and visits from friends or relatives with gastroenteritis symptoms). The questionnaire for study B included demographic and clinical characteristics, shifts and possible risk factors (contact with symptomatic patients or HCWs and type of contact, working in more than one wards and escorting patients to other wards), as well as questions regarding the implementation of control measures (HCW absence from work due to gastroenteritis, contact with patients while being symptomatic). Contact was defined as a) direct contact with a symptomatic person (nursing care, clinical examination), b) contact with patients' vomitus or diarrhoea, or c) contact with patient's inanimate environment (e.g. sheets, blankets).
Cases were asked about possible risk factors up to 48 hours before symptoms onset and controls about risk factors up to 48 hours before the interview. Data were collected through personal interviews. Finally, the duration of the outbreak was calculated as the number of days from the onset of the first case to the onset of the last case14.
Microbiological investigation
It was requested specimens to be sent to the Microbiology Laboratory of the University of Athens for virological testing (norovirus, rotavirus, adenovirus).
Statistical analysis
Stata 11.0 software (STATA, College Station, Texas, USA) was used for data analysis. Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated. Associations between categorical and quantitative variables were tested by Student's t-test (for normally distributed variables) or Mann-Whitney test (for skewed variables). The multivariable analysis was performed by multiple logistic regression using backwards elimination. Variables statistically significant at p < 0.05 were included. An association was considered as statistically significant when p < 0.05.
Ethical considerations
According to the Greek legislation, HCDCP is the competent authority for diseases' surveillance and outbreak investigation. The study was approved by the hospital's Ethics Committee and informed consent was obtained from all participants. The study was performed in compliance with the Helsinki Declaration and all the necessary measures to protect the confidentiality of personal data were taken.
Results
Epidemiological investigation and containment measures
In total, 63 gastroenteritis cases were identified; 30 HCWs and 33 patients. Five of them did not fulfill the criteria of the case definition, nine had been discharged and two had died due to their underlying disease and after recovery from gastroenteritis symptoms. Finally, 19 patients and 28 HCWs (13 physicians, 13 nurses and two paramedics) were included in the analysis.
The number of cases by date of symptoms onset among inpatients and HCWs is depicted in Figure 1. The first three recorded cases concerned hospitalized patients without an apparent epidemiological link. Ill patients came from the five wards of the same building, while the 28 ill HCWs were occupied in 13 different wards. The temporal distribution of cases by ward did not depict any specific transmission pattern.The total duration of the outbreak was 22 days. The shape of the epidemic curve indicates a person-to-person transmission. The attack rate among patients and HCWs was 15.0% and 16.9%, respectively. Attack rates by ward ranged from 3.4% to 18.5% for patients and from 6.3% to 42.9% for HCWs.
Figure 1. Distribution of cases (patients: n=19, health-care workers: n=28) by date of symptoms’ onset, Hospital X, Greece, January-February 2012.
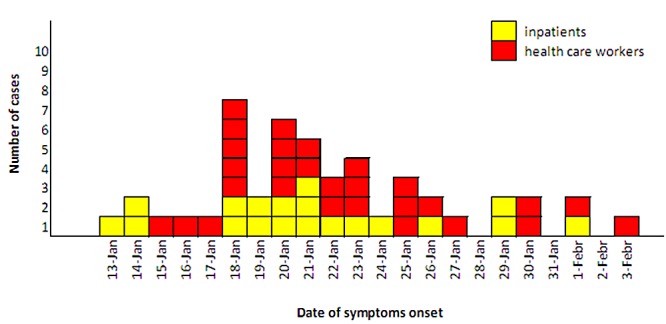
Diarrhoea was the prevalent symptom, reported by >80% of the cases in both groups, followed by vomiting, reported by 47.4% of patients and 67.9% of HCWs. The median duration of symptoms was 2 days (range: 1-7 days) among patients and 2 days (range: 1-4 days) among HCWs.
The results of the univariate analyses are presented in Table 1 and Table 2. Among HCWs, a history of direct contact with a symptomatic patient up to 48 hours before their symptoms' onset was associated with an increased risk for gastroenteritis (OR=3.03, 95%CI 1.01-9.12); no other factor was associated with the disease occurrence or considered to be a confounder of the observed association, so multivariable analysis was not performed for HCWs. According to the results of the multivariable analysis of case-control study A, the incidence of gastroenteritis among inpatients was statistical significantly associated with exposure to a roommate's vomitus (OR=7.96, 95% CI=1.29-49.2).
Table 1. Results of univariate analysis, patient cases and controls, Hospital X, Greece, January-February 2012.
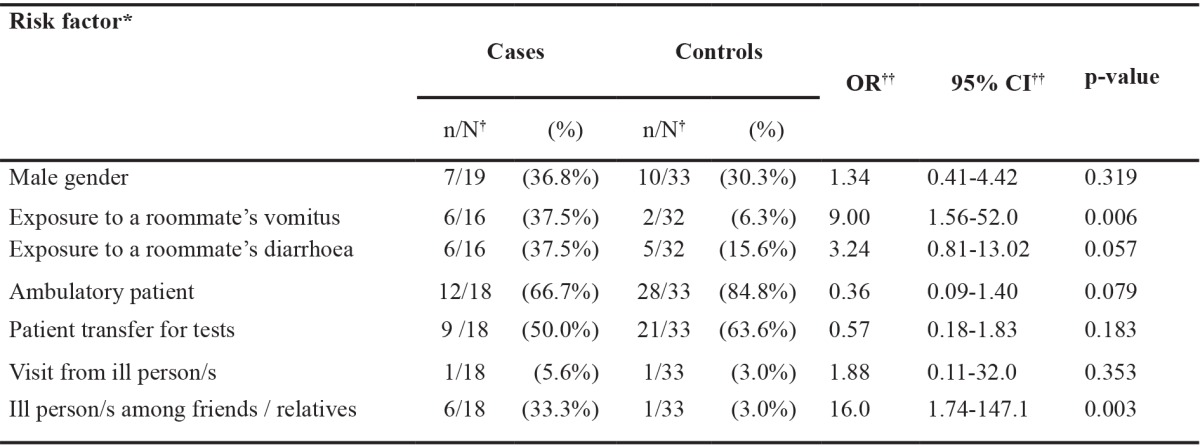
*: questions referred to the 48 hours before the symptoms’ onset (cases) / the interview (control), †N: number of participants for which an answer was available, ††OR: odds ratio, CI: confidence interval.
Table 2. Results of univariate analysis, health care workers and controls, Hospital X, Greece, January-February 2012.
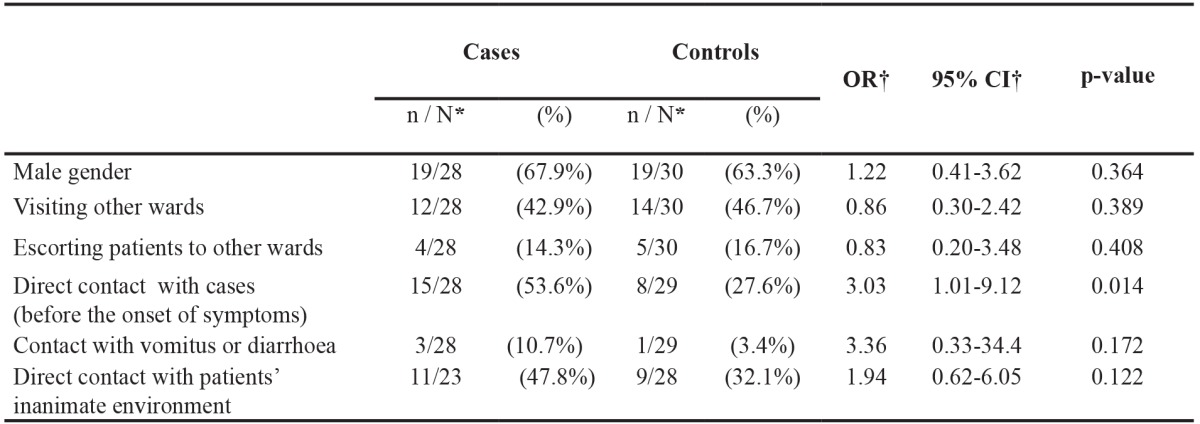
*N: number of participants for which an answer was available, †OR: odds ratio, CI: confidence interval
Furthermore, in terms of infection control measures, 21 (75%) symptomatic HCWs reported being absent from work for a median of 2 days (range: 1-4 days) while seven (25.0%) continued to work and having direct contact with hospitalized patients despite being symptomatic. Only, 11.1% of patients reported that they had been transferred to a different room (isolated/ cohorted) after developing symptoms.
Microbiological testing
One stool specimen from a hospitalized patient with gastroenteritis was collected and sent for testing. The specimen was tested positive for norovirus by real-time PCR; further typing was not carried out.
Discussion
A nosocomial viral gastroenteritis outbreak in one of the largest Greek hospitals was notified in January 2012.
The duration of the outbreak was 22 days, shorter than the estimated mean of 32.5 days (range: 8-120) reported in a recent systematic review on norovirus nosocomial outbreaks10. Attack rates among patients and HCWs were similar with those reported by others15,16. However, we believe that not all cases were identified in the absence of a recording system, and that early cases may have been missed. Identification of hospitalized cases was challenging because of the disperse distribution of buildings, the high frequency of incontinence among patients or other causes of gastrointestinal symptoms, such as antibiotic-associated diarrhoea or vomiting due to an underlying condition14. This may explain why the chain of transmission between wards could not be accurately documented and identification of the index case was not possible.
The results of the outbreak investigation indicated person-to-person and airborne transmission which is the most frequently recognized pattern in nosocomial viral gastroenteritis outbreaks1,5,10. Aerosolized vomit can result in widespread environmental contamination and may be inhaled and swallowed8-10,17,18. It has been estimated that a single incident of vomiting may generate 300,000-3,000,000 infectious doses, in case of norovirus19. In this outbreak, the index case was probably a patient or a HCW infected in the community, as norovirus circulation the same period was high2,20.
Results of the analytical studies showed that control measures were not fully implemented. However, the number of new cases gradually decreased and complete closing of wards was not required. To our knowledge, this was the first time that an analytical epidemiological study was conducted for a gastroenteritis nosocomial outbreak in Greece, even though this is not the first one recognized21.
Early identification of the outbreak was impaired by the complex architecture of the hospital and the lack of a standard recording system. The delay in the identification of the outbreak could partly explain the failure in the verification of the aetiological agent. Insufficient laboratory investigation constitutes a limitation in the current study. Delayed reporting of such outbreaks appears to be common according to the literature22. Specific recommendations were given for the establishment of an internal syndromic surveillance system that will allow early identification of nosocomial cases based on symptoms (syndromic surveillance) and implementation of control measures. HCWs should be trained to suspect an outbreak of viral gastroenteritis when two or more patients and/or staff develop a new onset of vomiting and diarrhoea within one to two days.
In conclusion, an appropriately designed protocol regarding the prompt detection and management of nosocomial gastroenteritis outbreaks, prompt implementation of infection control measures and epidemiological and laboratory investigation is needed in order early containment to be ensured. Capacity for virological testing should be increased at the hospital level, and a reference laboratory could take on further typing of viruses.
Conflict of interest statement
Authors declare no conflict of interest.
Acknowledgements
Authors would like to thank the Microbiology Laboratory of the University of Athens. The findings and opinions in this article are those of the authors, and do not necessarily represent those of the Hellenic Center for Disease Control and Prevention.
References
- 1.Lopman BA, Adak GK, Reacher MH, Brown DW. Two epidemiologic patterns of norovirus outbreaks: surveillance in England and wales, 1992-2000. Emerg Infect Dis. 2003;9:71–77. doi: 10.3201/eid0901.020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopman B, Armstrong B, Atchison C, Gray JJ. Host, weather and virological factors drive norovirus epidemiology: time-series analysis of laboratory surveillance data in England and Wales. PLoS One. 2009;4:e6671–e6671. doi: 10.1371/journal.pone.0006671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris JP, Lopman BA, O'Brien SJ. Infection control measures for norovirus: a systematic review of outbreaks in semi-enclosed settings. J Hosp Infect. 2010;74:1–9. doi: 10.1016/j.jhin.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 4.Said MA, Perl TM, Sears CL. Healthcare epidemiology: gastrointestinal flu: norovirus in health care and long-term care facilities. Clin Infect Dis. 2008;47:1202–1208. doi: 10.1086/592299. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer LA, Murphy JJ, Kaplan JE, Pinsky PF, Chacon D, Walmsley S, et al. 25- to 30-nm virus particle associated with a hospital outbreak of acute gastroenteritis with evidence for airborne transmission. Am J Epidemiol. 1988;127:1261–1271. doi: 10.1093/oxfordjournals.aje.a114918. [DOI] [PubMed] [Google Scholar]
- 6.Cheesbrough JS, Barkess-Jones L, Brown DW. Possible prolonged environmental survival of small round structured viruses. J Hosp Infect. 1997;35:325–326. doi: 10.1016/s0195-6701(97)90230-9. [DOI] [PubMed] [Google Scholar]
- 7.Kuusi M, Nuorti JP, Maunula L, Minh Tran NN, Ratia M, Karlsson J, et al. A prolonged outbreak of Norwalk-like calicivirus (NLV) gastroenteritis in a rehabilitation centre due to environmental contamination. Epidemiol Infect. 2002;124:481–487. doi: 10.1017/s0950268802007276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanerva M, Maunula L, Lappalainen M, Mannonen L, von Bonsdorff CH, Anttila VJ. Prolonged norovirus outbreak in a Finnish tertiary care hospital caused by GII.4-2006b subvariants. J Hosp Infect. 2009;71:206–213. doi: 10.1016/j.jhin.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Fankhauser RL, Monroe SS, Noel JS, Humphrey CD, Bresee JS, Parashar UD, et al. Epidemiologic and molecular trends of "Norwalk-like viruses" associated with outbreaks of gastroenteritis in the United States. J Infect Dis. 2002;186:1–7. doi: 10.1086/341085. [DOI] [PubMed] [Google Scholar]
- 10.Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect. 2012;140:1151–1160. doi: 10.1017/S0950268811002731. [DOI] [PubMed] [Google Scholar]
- 11.Grima A, Gatt A, Zahra G, Gambin A. Outbreak of norovirus infection in a nursing home for the elderly in Malta, November-December 2008. Euro Surveill. 2009;14:pii: 19103. [PubMed] [Google Scholar]
- 12.Lopman BA, Reacher MH, Vipond IB, Sarangi J, Brown DW. Clinical manifestation of norovirus gastroenteritis in health care settings. Clin Infect Dis. 2004;39:318–324. doi: 10.1086/421948. [DOI] [PubMed] [Google Scholar]
- 13.Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention. Updated norovirus outbreak management and disease prevention guidelines. MMWR Recomm Rep. 2011;60:1–18. [PubMed] [Google Scholar]
- 14.Zingg W, Colombo C, Jucker T, Bossart W, Ruef C. Impact of an outbreak of norovirus infection on hospital resources. Infect Control Hosp Epidemiol. 2005;26:263–267. doi: 10.1086/502537. [DOI] [PubMed] [Google Scholar]
- 15.Billgren M, Christenson B, Hedlund KO, Vinjé J. Epidemiology of Norwalk-like human caliciviruses in hospital outbreaks of acute gastroenteritis in the Stockholm area in 1996. J Infect. 2002;44:26–32. doi: 10.1053/jinf.2001.0946. [DOI] [PubMed] [Google Scholar]
- 16.Lopman BA, Reacher MH, Vipond IB, Hill D, Perry C, Halladay T, et al. Epidemiology and cost of nosocomial gastroenteritis, Avon, England, 2002-2003. Emerg Infect Dis. 2004;10:1827–1834. doi: 10.3201/eid1010.030941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teunis PF, Moe CL, Liu P, Miller SE, Lindesmith L, Baric RS, et al. Norwalk virus: how infectious is it? J Med Virol. 2008;80:1468–1476. doi: 10.1002/jmv.21237. [DOI] [PubMed] [Google Scholar]
- 18.Marks PJ, Vipond IB, Regan FM, Wedgwood K, Fey RE, Caul EO. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol Infect. 2003;131:727–736. doi: 10.1017/s0950268803008689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caul EO. Hyperemesis hiemis--a sick hazard. J Hosp Infect. 1995;30:498–502. doi: 10.1016/0195-6701(95)90054-3. [DOI] [PubMed] [Google Scholar]
- 20.Mounts AW, Ando T, Koopmans M, Bresee JS, Noel J, Glass RI. Cold weather seasonality of gastroenteritis associated with Norwalk-like viruses. J Infect Dis. 2000;181 Suppl 2:S284–S287. doi: 10.1086/315586. [DOI] [PubMed] [Google Scholar]
- 21.Georgiadou SP, Loukeris D, Smilakou S, Daikos GL, Sipsas NV. Effective control of an acute gastroenteritis outbreak due to norovirus infection in a hospital ward in Athens, Greece, April 2011. Euro Surveill. 2011 [PubMed] [Google Scholar]
- 22.Loveridge P, Cooper D, Elliot AJ, Harris J, Gray J, Large S, et al. Vomiting calls to NHS Direct provide an early warning of norovirus outbreaks in hospitals. J Hosp Infect. 2010;74:385–393. doi: 10.1016/j.jhin.2009.10.007. [DOI] [PubMed] [Google Scholar]


