Abstract
Objectives: The patterns of purchasing prescription antimicrobials with or without a prescription from retail pharmacies in Ulaanbaatar, Mongolia, were examined in relation to purchasers’ socioeconomic status and price of the product.
Methods: A survey was conducted at 250 randomly selected pharmacies in Ulaanbaatar. A total of 619 customers were interviewed, and the medicines they bought at the stores were examined by medical doctors. The use of prescriptions and advice in purchasing medicines and sociodemographic characteristics of the subjects were determined.
Results: Interviews were conducted with 297 customers who purchased prescription antimicrobials in front of the store in which they made their purchase. Among these 297 customers, only 19.5% (n=58) purchased medicine with a formal prescription, and 37.4% (n=111) purchased medicines on their own initiative and without the guidance of medical professionals. Purchase without a prescription was not associated with the subjects’ gender, age, educational status or area of residence. Lower-priced antimicrobials were purchased without prescriptions more frequently than those with a higher price (P<0.05).
Conclusion: The purchase of antimicrobials without prescriptions is common across all sociodemographic strata in Ulaanbaatar, Mongolia. Considering the increases in number of retail pharmacies and in sales of antimicrobials associated with economic development, measures to enforce regulations and to promote education among the general public and pharmacy professionals are required.
Keywords: antimicrobials, drug resistance, self-medication, prescription, Ulaanbaatar
Introduction
It has been estimated that over 50% of antibiotics worldwide are purchased from pharmacies or retailers without a prescription1). A report estimated 20–50% of human use of antibiotics in a community setting is questionable2). There are several possible reasons for purchasing without a prescription, including a traditional culture of self-medication, accessibility to pharmacies or retailers, affordability in terms of price, sense of savings by avoiding a visit to a doctor and lack of incentives for medical professionals to issue a prescription.
Drug-resistant pathogens have been reported in both developed and developing countries3,4,5). The ready availability of antimicrobials without a prescription in developing countries is expected to result in increased overuse or misuse of these agents, which is anticipated to increase the emergence of drug-resistant pathogens6,7,8).
Economic development is associated with increased accessibility to pharmaceutical products along with improvements in socioeconomic conditions of the population in developing countries. Previous studies have suggested that people with a higher socioeconomic status are more likely to use antimicrobial medications even where there is universal access to health care and medicines9, 10). There is concern about whether people with a higher socioeconomic status use medicines with a valid prescription. If this is not the case, use of antimicrobial agents without a prescription by the growing socioeconomically well-off population will likely increase rapidly, resulting in further emergence of drug-resistant pathogens.
Mongolia has shown remarkable economic growth, with an increase of 8.7% in annual GDP from 2004 to 200611). According to the national health accounts, the country spends 6.7% of its gross domestic product on health12). Of the total health expenditure, 14% is out of pocket spending including payments to purchase medicine12). This is regarded as 0.9% of GDP being spent out of pocket on health-care purchases by individuals13). A total of 2.7 million people live in the country, and 28.1% of them are under the age of 15 years. The country has a 97.6% literacy rate, and 60% of the population lives in urban areas13). According to a health report in 2007, the major diseases reported in the country were related to the respiratory, digestive, genitourinary and circulatory systems, and the morbidity rates were 973, 839, 773and 646 per 10,000 population, respectively14).
With the encouragement of privatization in the early 1990s, the country has transformed to a free market economy, and this has brought with it a rapid increase in the number of private pharmacies15). Although there is national regulation prohibiting the sale of prescription antimicrobials to customers without a prescription, this is not followed in practice, as drugs can often be purchased at pharmacies without a prescription.
There has been little research regarding the patterns of purchasing prescription antimicrobials with or without a prescription from retail pharmacies. Such data regarding the patterns of antimicrobial purchase by the general public in a developing country will provide baseline information to allow formulation of national pharmaceutical policies to promote the “rational use” of medicine.
The present study was performed to examine the patterns of antimicrobial purchase with or without a prescription from retail pharmacies in Ulaanbaatar, Mongolia, according to demographic characteristics, socioeconomic status and price of the products.
Methods
Study area and subjects
This study was performed between December 2006 and January 2007 in Ulaanbaatar City (population of 0.9 million), the capital city of Mongolia. Subjects were customers 18 years of age or over who purchased medicines from one of the 250 retail pharmacies randomly selected with a 1/2 selection ratio from the 500 retail pharmacies listed by the Ulaanbaatar City Pharmaceutical Department. A list of 250 selected pharmacies was developed for this survey. Subjects who bought only bandages, ointments, cosmetics and other products were excluded from the study.
Survey procedure
Three teams each consisting of two medical doctors carried out face-to-face interviews using a standardized questionnaire. A team with two medical doctors waited in front of the 250 randomly selected retail pharmacies and made contact with customers 18 years of age and over immediately after they purchased medicines. At least 1 hour was spent by one of the three interview teams in front of each retail pharmacy. A total of 291.7 team-hours, excluding the time spent moving from one pharmacy to another, were spent to complete the interviews in front of the 250 retail pharmacies. Informed consent was obtained for the interviews, which lasted approximately 3 min each. A total of 619 customers who purchased medicine agreed to participate in the study and answered the interviewers’ questions.
A standardized questionnaire was developed in English and translated into Mongolian. The translation was verified by confirming back translation from Mongolian to English. The questionnaire was pretested with ten customers by comparing the results of interviews with the same customers by two different teams. Ninety-four percent of the results of one team matched with the results obtained by the other team. The reliability of the questionnaire was regarded as reasonable. The answers of another ten customers regarding the types of medicine bought, documents the customers brought for purchasing medicines and recommendations given at pharmacies were compared with the information given by pharmacy staff where the customers bought medicine. The consistency of the answers from customers and information from pharmacy staff was confirmed for eight out of the ten customers. Although over-reporting from customers concerning the use of prescriptions was anticipated, the questionnaire for the customers regarding the purchase of medicine was regarded as reasonably valid.
Interviewers participated in a 3-day training workshop before conducting actual interview surveys to gain an understanding of the objectives and protocol and to obtain appropriate skills necessary to conduct the interviews.
The survey procedures received approval from the Institutional Review Board of Tokyo Medical and Dental University (No. 381/06) and from the Ethical Review Board of the Ministry of Health of Mongolia (No. 24/06) prior to the study.
Measurements
The following information related to the purchase of medicine was recorded: reason(s) for purchasing medicines (disease or illness); names and quantities of medicines purchased; presentation of any type of note provided by a medical doctor (formal prescription, patient card listing the bearer’s disease and medicines or a list of medicines); recommendations given by medical doctors or pharmacy staff for purchasing medicine; participation in health insurance; use of health insurance in purchasing medicine; and demographic and socioeconomic characteristics. The names and quantities of medicines purchased were individually confirmed by medical doctors who conducted the interviews.
From the information gathered, subjects were divided into the following three categories: purchase with a formal prescription, purchase following guidance of a medical professional but without a formal prescription (including purchase with a patient card or list of medicines provided by a physician, purchase without any type of note but following a physician’s advice and purchase without any type of note but following a pharmacy’s or a druggist’s advice) and purchase by the customer’s own initiative.
With regard to demographic and socioeconomic characteristics, gender, age, education and area of residence were identified. “Area of residence” was categorized into “ger” (yurt) residence or “urban residential” areas. Ger residences consist of traditional round felt tents and wooden huts and generally do not have access to a water supply, sanitation facilities or central heating systems. Living in a ger residence was regarded as an indicator of low socioeconomic status.
Prescription antimicrobial medicines were confirmed by medical doctors who conducted interviews based on the 14th edition of the List of Essential Medicines developed by the WHO16).
Analysis
The percentages of respondents purchasing medicine with a prescription or based on professional advice (i.e., with a formal prescription, following guidance of a medical professional but without a formal prescription or on their own initiative without the guidance of medical professionals) were calculated according to type of medicine and group of antimicrobial. Percentages of individuals purchasing particular types of medicine with a formal prescription were compared with those for other medicines by Fisher’s exact test. The trends in the percentages of customers who purchased prescription antimicrobials based on a prescription or professional advice were examined by the chi-square test for trend.
In addition, the percentages of respondents purchasing prescription antimicrobials with a prescription and professional advice were calculated according to sociodemographic characteristics and price of prescription antimicrobials.
Data were analyzed using SPSS for Windows version 14.
Results
Of the total of 619 customers who completed the interviews and examination of medicines bought at the retail pharmacies, 97.6% participated in the social health insurance scheme, and only 2.4% used their health insurance to obtain the medicine at the reduced price afforded by their health insurance. The major diseases for which the respondents purchased medicine were acute respiratory infections (n=287), gastrointestinal disease (n=69) cardiovascular disease (n=66) and disorders of the genitourinary system (n=47). Table 1 shows demographic characteristics of respondents who purchased medicine at retail pharmacies with a prescription or following professional advice.
Table 1. Demographic characteristics of respondents who purchased medicine at retail pharmacies with a prescription or following professional advice in Ulaanbaatar, Mongolia (n=619).
| Demographic characteristics | n (%) | Percentage of customers who purchased
medicine |
P | ||
|---|---|---|---|---|---|
| With a formal prescription | Following guidance of a medical professional but without a formal prescription |
Customer’s own initiative and without the guidance of a medical professional |
|||
| At least one antibiotic | 619 | 16.8 | 41.2 | 42.0 | |
| Gender | |||||
| Male | 190 (30.9) | 17.4 | 43.2 | 39.5 | |
| Female | 424 (69.1) | 16.7 | 40.6 | 42.7 | 0.544 |
| Age categories | |||||
| ≤19 | 34 (5.5) | 32.4 | 29.4 | 38.2 | |
| 20–29 | 147 (23.7) | 15.0 | 39.5 | 45.6 | |
| 30–39 | 133 (21.5) | 21.1 | 39.8 | 39.1 | |
| 40–49 | 128 (20.7) | 11.7 | 46.9 | 41.4 | |
| 50–59 | 100 (16.2) | 18.0 | 36.0 | 46.0 | |
| 60≤ | 77 (12.4) | 13.0 | 49.4 | 37.7 | 0.560 |
| Education, complete | |||||
| College or university | 260 (42.0) | 18.1 | 39.6 | 42.3 | |
| Vocational school | 54 (8.7) | 16.7 | 40.7 | 42.6 | |
| Senior high school | 214 (34.6) | 17.8 | 44.4 | 37.9 | |
| Junior high school | 75 (12.1) | 12.0 | 38.7 | 49.3 | |
| Elementary school | 15 (2.4) | 6.7 | 40.0 | 53.3 | |
| None | 1 (0.2) | 0.0 | 0.0 | 100.0 | 0.233 |
| Area of residence | |||||
| Ger residential area | 131 (21.2) | 17.6 | 44.3 | 38.2 | |
| Urban residential area | 488 (78.8) | 16.6 | 40.4 | 43.0 | 0.414 |
P values were calculated using the chi-squire test for trend.
Table 2 shows the medicines purchased by customers according to the type of medicine and the conditions of presenting a prescription or other notes and professional advice. For all medicines, 16.8% of the customers presented a formal prescription, 41.2% of the customers bought medicine following advice by medical professionals but did not receive advice from physicians and 42.0% bought medicine on their own initiative without guidance of a medical professional. The percentages of respondents purchasing prescription antimicrobials using a formal prescription, following professional advice but without a prescription and on their own initiative were 19.5%, 43.1% and 37.4%, respectively. The trends in purchase of prescription antimicrobials based on a prescription or professional advice were significantly greater for the purchase of antimicrobials (P<0.05) and gastrointestinal medicine (P<0.01) than for purchase of other medicines. Purchase of analgesics was less reliant on a prescription or professional advice (P<0.01) than purchase of other medicines.
Table 2. Medicines purchased by customers at retail pharmacies with a prescription or following professional advice in Ulaanbaatar, Mongolia (n=619).
| Type of medicine | n | Percentage of customers who purchased
medicines |
P | ||
|---|---|---|---|---|---|
| With a formal prescription |
Following guidance of a medical professional butwithout a formal prescription |
Customer’s own initiative and without the guidance of a medical professional |
|||
| At least one medicine | 619 | 16.8 | 41.2 | 42.0 | |
| Antimicrobials | 297 | 19.5 | 43.1 | 37.4 | 0.015 |
| Analgesics, anti-inflammatory medicines | 188 | 12.8 | 37.2 | 50.0 | 0.006 |
| Vitamins and minerals | 176 | 16.5 | 35.8 | 47.7 | 0.191 |
| Antiasthmatic and medicines for chronic obstructive pulmonary disease | 78 | 19.2 | 34.6 | 46.2 | 0.823 |
| Cardiovascular medicine, diuretics | 68 | 17.6 | 48.6 | 33.8 | 0.276 |
| Gastrointestinal medicine | 68 | 25.0 | 50.0 | 25.0 | 0.002 |
| Anti-allergic | 28 | 25.0 | 50.0 | 25.0 | 0.060 |
| Sleeping pills and psychotherapeutic medicine | 13 | 7.7 | 38.5 | 53.8 | 0.292 |
| Others | 155 | 18.7 | 44.5 | 36.8 | 0.157 |
P values were calculated using the chi-squire test for trend. The comparison group was customers who were not in each category.
Table 3 shows the prescription antimicrobials purchased according to the type of medicine and the conditions of presenting a prescription and professional advice. Among the 297 subjects who purchased prescription antimicrobials, amoxicillin (26.8%), ampicillin (22.4%), metronidazole (7.7%), chloramphenicol (6.8%) and sulfamethoxazole-trimethoprim (6.5%) were commonly purchased agents. The purchasing practices for oxacillin, cefazolin and doxycycline were significantly more reliant on a prescription and professional advice than those for purchases other than antimicrobial medicines (P<0.01).
Table 3. Prescription antimicrobials purchased by customers at retail pharmacies with a prescription or following professional advice in Ulaanbaatar, Mongolia, by antimicrobial agents (n=619).
| Group | Name | n | Percentage of customers who purchased
prescription antimicrobials |
P | ||
|---|---|---|---|---|---|---|
| With a formal prescription |
Following guidance of a medical professional but without a formal prescription |
Customer’s own initiative and without the guidance of amedical professional |
||||
| At least one prescription antimicrobial medicine | 297 | 19.5 | 43.1 | 37.4 | ||
| Nonprescription antimicrobial medicine | 322 | 14.3 | 39.4 | 46.3 | ||
| Antimicrobial medicine | ||||||
| Penicillins | Amoxicillin | 91 | 16.5 | 43.9 | 39.6 | 0.292 |
| Ampicillin | 76 | 21.1 | 32.8 | 46.1 | 0.450 | |
| Benzylpenicillin | 9 | 11.1 | 33.3 | 55.6 | 0.604 | |
| Phenoxymethylpenicillin | 4 | 25.0 | 25.0 | 50.0 | 0.845 | |
| Oxacillin | 2 | 100.0 | 0.0 | 0.0 | 0.009 | |
| Cephalosporins | Cefazolin | 12 | 41.7 | 58.3 | 0.0 | <0.001 |
| Ceftriaxone | 2 | 0.0 | 50.0 | 50.0 | 0.720 | |
| Cephalexin | 1 | 100.0 | 0.0 | 0.0 | ||
| Aminoglycosides | Gentamicin | 11 | 18.2 | 54.5 | 27.3 | 0.293 |
| Tetracyclines | Doxycycline | 9 | 55.6 | 33.3 | 11.1 | 0.002 |
| Macrolides | Erythromycin | 10 | 40.0 | 30.0 | 30.0 | 0.069 |
| Clarithromycin | 1 | 0.0 | 100.0 | 0.0 | 0.653 | |
| Others | Chloramphenicol | 23 | 4.3 | 39.2 | 56.5 | 0.184 |
| Synthetic antibacterial medicines | ||||||
| Sulfonamide | Sulfamethoxazole-Trimethoprim | 22 | 27.3 | 31.8 | 40.9 | 0.247 |
| Quinolones | Ciprofloxacin | 11 | 9.1 | 81.8 | 9.1 | 0.139 |
| Others | Metronidazole | 26 | 19.2 | 57.7 | 23.1 | 0.052 |
P values were calculated using the chi-squire test for trend. The comparison group was customers who did not buy antimicrobial medicine.
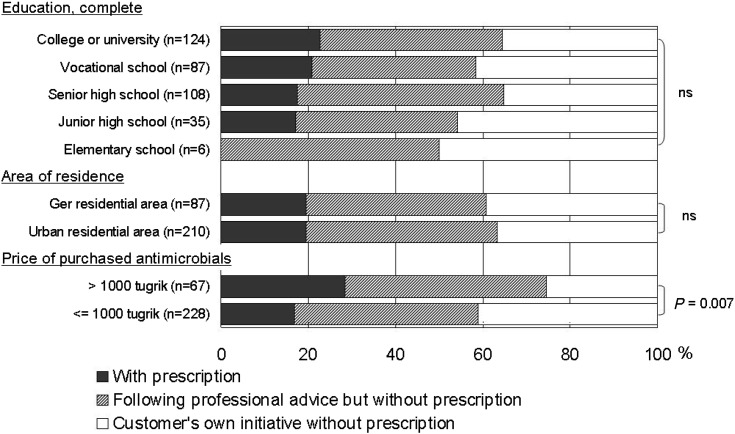
Figure 1 shows the prescription antimicrobials purchased by customers by the conditions of presenting a prescription or other notes and professional advice according to sociodemographic characteristics and price of the product. Similar trends in purchase of antimicrobials based on a prescription or professional advice were shown for different educational statuses and areas of residence. The trends were also similar for gender and age categories. The trends in purchase of antimicrobials based on a prescription or professional advice for individuals who purchased prescription antimicrobials costing more than 1000 tugrik (approximately equivalent to US$0.95) were significantly greater than for those who purchased prescription antimicrobials costing 1000 tugrik or less (P<0.01).
Figure 1.
Prescription antimicrobials purchased by customers at retail pharmacies with a prescription or following professional advice in Ulaanbaatar, Mongolia, by educational status, area residence and price of antimicrobials (n=297). P values were calculated using the chi-squire test for trend.
Discussion
This is the first survey regarding the situation pertaining to purchase of medicines from retail pharmacies in a rapidly developing country. Among the 297 customers who purchased prescription antimicrobials, only 19.5% purchased medicine with a formal prescription, and 37.4% purchased medicine on their own initiative without the guidance of a medical professional. Purchase of prescription antimicrobials with a prescription was not associated with the customers’ gender, age, educational status or area of residence. Purchase of prescription antimicrobials without prescriptions was common across all sociodemographic strata in Ulaanbaatar.
Mongolia established a social health insurance scheme in 1994, and 80% of the population was enrolled by 200617, 18). All Mongolian residents are eligible to be covered under this insurance scheme, which is managed independently of the general health budget of the government. The people enrolled in the scheme pay premiums and are reimbursed for costs of inpatient hospital care. The cost of outpatient care is not covered by the insurance. Health services provided by not only health institutions managed by the government but also those provided by privatized institutions are covered by the social health insurance. The number of hospital beds per 10,000 population, 75.2 as of 2002, was three times that of Thailand and 1.1 times that of South Korea19). The number of physicians per 10,000 population, 27.8 as of 2002, was 9 times that of Thailand and 1.4 times that of South Korea19). The availability of health-care resources enables people in urban areas to have reasonable access to health services. This social health insurance scheme enables customers with health insurance to purchase medicine at a reduced cost and reimburses the rest of the cost to the retail pharmacies contracted with the insurer when a customer brings a formal prescription form provided by a medical doctor. However, only 2.4% of the subjects obtained the benefit of purchasing medicine at a discounted rate. The advantages of the high enrollment rate in social health insurance should be fully utilized to enforce purchase of prescription antimicrobials only with a prescription. Prompt reimbursement of pharmacies for the cost of purchased medicines, facilitation of visits to medical doctors to obtain a prescription and promotion of the benefits to customers of using their health insurance to purchase prescription medicine should be encouraged.
Despite the availability of the social health insurance benefit for purchase of prescription antimicrobials with a prescription, more than one third of the customers who purchased antimicrobials did so on their own initiative and without the guidance of medical professionals. Self-medication by the majority of community members is also reported in other developing countries, although the average percentage of prescription use varies and reflects enforcement of the related regulations20,21,22). Some selected antimicrobials, those antimicrobials introduced to the country recently, such as oxacillin, cefazolin and doxycycline, were bought by very few customers on their own initiatives. The majority of customers who purchased these medicine sought prescriptions or at least a note provided by a medical doctor. On the other hand, more than half of those who purchased chloramphenicol did so on their own initiative and without the guidance of medical professionals.
It is concerned that there were no associations between prescription use and socioeconomic status. It is generally regarded that people in a high social class have a tendency to purchase antimicrobials9, 10). The present results showed that people in a high social class purchase antimicrobials without a prescription in a manner similar to those in a low social class. This situation suggests that there will be more people in a high social class who can afford to buy medicine as they like as society continues to develop. They will purchase medicine without consulting medical professionals. This will sharply increase the use of antimicrobials without a prescription in conjunction with expansion of the economy and the subsequent increase in the economically well-off population. Unlike the results obtained by the current survey, a report from Vietnam showed a greater percentage of self-medication among a low educational level group (43.7%) than among a high educational level group (17.6%)23). Careful investigation is required if the lack of socioeconomic gradients in the use of a prescription to purchase antimicrobials is consistent.
Similar to the situation in other developing countries, the average price of antimicrobials is rather cheap. Among the 297 customers who bought antimicrobials, 228 spent 1000 tugrik (approximately equivalent to US$0.95) or less. A greater percentage of customers who bought antimicrobials and paid more than 1000 tugrik used a prescription. A study in Vietnam reported that the average amount spent on medicine was US$1.1022). A balance between the customer’s ability to pay for antimicrobials and elimination of overuse of antimicrobials should be considered.
While the results of this survey revealed the actual patterns of antimicrobial purchase from retail pharmacies by the general population, further studies regarding customers’ in-depth knowledge on rational use of prescription antimicrobials and accessibility to consultation with pharmacists and physicians and knowledge and practices concerning the use of antimicrobials of medical doctors and pharmacists will help in the design of pharmacy education programs for both the public and professionals.
It is regulated by law that all retail pharmacies should register with the Ministry of Health and specify a responsible qualified pharmacist. As of 2007, 807 pharmacies were registered throughout the country. Business related to medicine is only allowed in these registered pharmacies, except for nutritional supplements and sanitary supplies such as bandages. Although the sale of medicine based on a prescription brought by the customer is encouraged, it is not well enforced.
Efforts to promote the rational use of medicine have already been implemented in the principles of the national drug policies in Mongolia24). To facilitate purchase of medicine with a prescription, reimbursement by the social health insurance of a part of the price of medicine purchased at pharmacies with a prescription was introduced in 2005. Careful monitoring of sales of antimicrobials and the practice of issuing prescriptions is required.
According to the information provided in the present study, a mechanism to give incentives to issue and use prescriptions should be properly implemented in addition to raising awareness of the need to enforce regulations throughout the country. Pharmacists and druggists are frontline health-care workers, and they play an important role in providing information and advice to patients regarding the appropriate use of medicine25). Therefore, continuing education and licensing schemes should be introduced to enhance the professional ethics of pharmacy professionals and ensure that they have up-to-date knowledge on the use of medicines.
The subjects of this study were customers who visited retail pharmacies and not the general public. Therefore, percentages or frequencies of use of prescription microbials with or without a prescription among the general population are not provided in this study. The quality of the medicines sold at retail pharmacies is another concern where there is high consumer demand and competition among retailers. Sampling investigations of products sold at pharmacies would give answers to these concerns.
Conclusion
The percentage of purchases of prescription antimicrobials without a prescription from retail pharmacies in Ulaanbaatar, Mongolia, was 80%. This study found that the high percentage of purchases of prescription antimicrobials without a prescription is common across all sociodemographic strata. Considering the increases in the number of retail pharmacies and in sales of antimicrobials associated with economic development, measures to enforce regulations and to promote education among the general public and pharmacy professionals are required.
Acknowledgments
This study was financially supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (17406019). The authors are grateful to the Pharmacology Department of the Health Science University of Mongolia for helping carry out the field survey, especially Dr. G. Choijamch, Dr. P. Batkhuyag, Dr. Ch. Eruult, Dr. J. Bayarmaa and Ms. D.Tserenkhorloo.
References
- 1.Cars O, Nordberg P. Antibiotic resistance – the faceless threat. Int J Risk Saf Med 2005; 17: 103–110. [Google Scholar]
- 2.Harrison PF, Lederberg J. Antimicrobial Resistance: Issues and Options. National Academy Press, Washington DC, 1998; 37-49. [PubMed] [Google Scholar]
- 3.Kunin CM. Resistance to antimicrobial drugs – a worldwide calamity. Ann Int Med 1993; 118: 557–561. [DOI] [PubMed] [Google Scholar]
- 4.Byarugaba DK. A view on antimicrobial resistance in developing countries and responsible risk factors. Int J Antimicrob Agents 2004; 24: 105–110. doi: 10.1016/j.ijantimicag.2004.02.015 [DOI] [PubMed] [Google Scholar]
- 5.Okeke IN, Laxminarayan R, Bhutta ZA, et al. Antimicrobial resistance in developing countries. Part I: recent trends and current status. Lancet Infect Dis 2005; 5: 481–493. doi: 10.1016/S1473-3099(05)70189-4 [DOI] [PubMed] [Google Scholar]
- 6.Radyowijati A, Haak H. Improving antibiotic use in low-income countries: an overview of evidence on determinants. Soc Sci Med 2003; 57: 733–744. doi: 10.1016/S0277-9536(02)00422-7 [DOI] [PubMed] [Google Scholar]
- 7.Van Duong D, Binns CW, Le TV. Availability of antibiotics as over-the-counter drugs in pharmacies: a threat to public health in Vietnam. Trop Med Int Health 1997; 2: 1133–1139. doi: 10.1046/j.1365-3156.1997.d01-213.x [DOI] [PubMed] [Google Scholar]
- 8.Kunin CM. Use of antimicrobial drugs in developing countries. Int J Antimicrob Agents 1995; 5: 107–113. doi: 10.1016/0924-8579(94)00039-W [DOI] [PubMed] [Google Scholar]
- 9.Henricson K, Stenberg P, Rametsteiner G, et al. Socioeconomic factors, morbidity and drug utilization – an ecological study. Pharmacoepidemiol Drug Saf 1998; 7: 261–267. doi: [DOI] [PubMed] [Google Scholar]
- 10.Kristiansson C, Gotuzzo E, Rodriguez H, et al. Access to health care in relation to socioeconomic status in the Amazonian area of Peru. Int J Equity Health 2009; 8: 11. doi: 10.1186/1475-9276-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UNDP Employment and poverty in Mongolia. In: United Nations Development Programme. United National Development Programme, Ulaanbaatar, 2007; 22-25.
- 12.Ministry of Health Mongolia. Mongolian National Health Accounts. Ministry of Health, Ulaanbaatar, 2005. [Google Scholar]
- 13.National Statistical Office of Mongolia Monogolian Statistical Yearbook. National Statistical Office of Mongolia, Ulaanbaatar, 2008. [Google Scholar]
- 14.Ministry of Health Mongolia. Annual Health Report of Mongolia. Ministry of Health, Ulaanbaatar, 2008. [Google Scholar]
- 15.World Bank The Mongolian Health System at a Crossroads: an Incomplete Transition to a Post-Semashko Model. World Bank, Washington DC, 2007; 31-35. [Google Scholar]
- 16.World Health Organization (WHO) WHO Model List of Essential Medicines 14th List. WHO, Geneva, 2005; 23. [Google Scholar]
- 17.Bolormaa T, Tumurbat B, Bujin TS, et al. Mongolia: health system review. In: Health System in Transition. World Health Organization, Copenhagen, 2007; 9: 35-38.
- 18.Bayarsaikhan D, Kwon S, Ron A. Development of social health insurance in Mongolia: successes, challenges and lessons. Int Soc Secur Rev 2005; 58: 27–44. doi: 10.1111/j.1468-246X.2005.00224.x [DOI] [Google Scholar]
- 19.World Health Organization Regional Office for the Western Pacific (WHO/WPRO) Core indicators. WHO/WPRO. http://www.wpro.who.int/information_sources/databases/core_indicators/. Accessed November 22, 2010.
- 20.Kamat VR, Nichter M. Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med 1998; 47: 779–794. doi: 10.1016/S0277-9536(98)00134-8 [DOI] [PubMed] [Google Scholar]
- 21.Al-Bakri AG, Bustanji Y. Yousef Al-M. Community consumption of antibacterial drugs within the Jordanian population: sources, patterns and appropriateness. Int J Antimicrob Agents 2005; 26: 389–395. doi: 10.1016/j.ijantimicag.2005.07.014 [DOI] [PubMed] [Google Scholar]
- 22.Okumura J, Wakai S, Umenai T. Drug utilization and self-medication in rural communities in Vietnam. Soc Sci Med 2002; 54: 1875–1886. doi: 10.1016/S0277-9536(01)00155-1 [DOI] [PubMed] [Google Scholar]
- 23.Saradamma RD, Higginbotham N, Nichter M. Social factors influencing the acquisition of antibiotics without prescription in Kerala State, South India. Soc Sci Med 2000; 50: 891–903. doi: 10.1016/S0277-9536(99)00380-9 [DOI] [PubMed] [Google Scholar]
- 24.Munkhdelger CH, Tserenlkhagva R. Legislation Guideline for Pharmaceutical Sector. Mongolia Ministry of Health and World Health Organization, Ulaanbaatar, 2007; 280 (in Mongolian). [Google Scholar]
- 25.Department of Essential Drugs and Other Medicines, World Health Organization (WHO) The role of the pharmacist in self-care and self-medication. WHO/DAP/98.13, WHO, Geneva, 1998; 15. [Google Scholar]