Abstract
Effects of gender and employment situation on weight loss and lifestyle modification were assessed in a 3-month intervention study done for overweight and obesity. A total of 384 individuals in Izumo City Japan, participated from 2000 to 2006. Lifestyle modifications were quantitatively evaluated by calculating calories of energy intake and expenditure. Eleven men and 15 women failed to complete the intervention; they were significantly younger in both genders, and the women had a higher rate of employment than the completing group (91 men and 267 women). Intervention induced a weight loss of 1.9 kg for men and 1.6 kg for women, with no significant differences by gender. Significant differences were found in changes in energy intake and expenditure in both genders, but these disappeared after adjusting for weight. There were significant decreases in weight (1.6 kg in unemployed, 2.5 kg in employed) in men. Increases in walking and exercise for the employed were smaller than those for the unemployed. The relationship between changes in weight and energy balance by employment status was independently significant using multiple regression analysis. Employment is associated with difficulty in losing weight due to limited exercise time in behavioral intervention.
Keywords: obesity, weight loss, employment, gender, physical activity
Introduction
The prevalence of overweight and obesity is rapidly increasing worldwide and may be associated with metabolic syndrome and diabetes1). Obesity occurs less frequently in the Japanese compared with western ethnic populations2, 3). While the prevalence of obesity with a BMI over 30 in the Japanese is currently estimated to be 2–3% and 25% of the population are overweight, recent social and lifestyle changes in Japan have caused an increase in the prevalence of obesity and diabetes4).
This has drawn the attention of health policy makers, who wish to develop public health strategies for preventing overweight and obesity5,6). The combination of overeating and physiological inactivity is the major cause of overweight and obesity. Lifestyle modification produces long-term beneficial changes in diet and levels of physical activity and reduces obesity and diabetes7). We previously developed a multicomponent three-month weight loss program covering nutrition, physical activity and supportive group therapy8). The objectives of the intervention were a 5% weight loss through lifestyle modification and improvement of biochemical parameters. Our intervention induced significant decreases in energy intake and an increase in the physical activities of the participants, with the weight loss showing a significant association with the improvement in metabolic measurements8). However, there were a number of participants who failed to complete or maintain the modified behavior producing the weight loss9).
Significant factors commonly reported to be associated with weight loss have included extreme obesity, a history of repeated attempts, cardiovascular disease risk factors, female gender, level of education, self-efficacy, physical self-image, income, employment and marital status10, 11, 12, 13). We identified body weight at the baseline as a predictor of success in weight loss effects8). The prevalence of overweight and obesity is increasing rapidly in middle-aged Japanese men, and working conditions affect overweight and obesity14). However, weight loss intervention programs for men and employees have so far received little attention.
We conducted an investigation to assess predictors, such as gender and employment situation, of weight loss and lifestyle modification in a behavioral intervention study and to identify the hallmarks of successful weight loss intervention. There have been only a limited number of studies of these factors and their relationship that have successfully determined any association, and the research methodologies have varied substantially. The strengths of our investigation were a comprehensive and quantitative evaluation of energy balance including energy intake and expenditure and a community setting including employed and unemployed participants.
Subjects and Methods
Subjects
A total of 384 clinically healthy participants (age, 55.8 ± 8.6 y; BMI, 25.1 ± 3.1 kg/m2) in Izumo City, Shimane Prefecture, Japan, who were interested in overweight and obesity prevention, voluntarily participated in our behavioral program for obesity prevention from 2000 to 2006. They were recruited through an advertisement in a local newspaper and demonstrated no clinical symptoms. The ethics committee of Shimane University School of Medicine approved all study protocols in 2000, and all subjects gave written informed consent.
The subjects participated in a behavioral weight loss program for three months involving diet, exercise and supportive group therapy. The program was based on becoming informed and learning about a participant’s health risks related to obesity, healthy life skills, setting specific behavioral goals, modifying behavior determinants and reinforcing desired behavior. This approach began with a health check to determine each subject’s situation regarding obesity and to prescribe medications for obesity-associated diseases, such as CVD, diabetes, dyslipidemia or hypertension. The following percentages of subjects were administered drugs at the baseline: 18% for hypertension, 11% for dyslipidemia, 4% for gout and 2% for ischemic heart disease or diabetes. Participants were recommended to continue taking medicine during the intervention according to their physician’s instructions. Participants’ demographic factors and lifestyle information were obtained using a self-reported questionnaire. The next step was to provide each subject with intensive, professional, individual information by which to improve their unhealthy lifestyle, i.e., overeating and insufficient physiological activity, and to assist with the self-monitoring ability of each subject, i.e., weekly checking of weight, daily estimations of caloric intake and monitoring physical activity. Participants established their specific behavioral and anthropometric goals, as related to their individual lifestyle and measured physiological data. During the 3-month program, participants were encouraged to maintain a daily record of their goal-oriented efforts15), including a step count using a pedometer (HJ-002, Omron Co. Ltd, Tokyo, Japan), and to record their body weight once a week. Weekend group programs provided support through local contacts and meetings with specialists to reaffirm their efforts and belief that they could personally control their health condition and environment8).
Anthropometric measurements
Anthropometric evaluation was performed before and after the intervention. After an overnight fast, body weight was measured to an accuracy of ± 0.1 kg with a standard scale while dressed in only very light clothing, and height was measured to an accuracy of ± 0.1 cm using a stadiometer. Waist circumference (WC) was measured at the midline between the iliac crest and the lowest rib margin at minimum respiration. Measurement was repeated for WC, and a third measurement was made if the difference between the first two readings was more than 0.5 cm. Body mass index (BMI) was computed as weight (kg) divided by squared height (m2).
Resting energy expenditure (REE) was measured by an indirect calorimeter after a 12-hour overnight fast. After a 15-min resting period, expired gas collection was achieved through a mouthpiece covering the nose for 3 minutes during the entire sampling period. Oxygen concentration was determined by nondispersive infrared analysis (VMB-002N, VINE Inc., Tokyo, Japan). The calculated energy equivalent of oxygen was 4.825 kcal/l16).
Diet
Information on the participant’s daily diet was obtained using an established self-administered quantitative food frequency questionnaire17) before and after the behavioral intervention. Trained nutritionists asked each participant about their weekly frequency of food intake for the most recent month. The questionnaire investigated the average intake and frequency of intake for one month regarding “the 30 kinds of food groups,” which included soup, meat, seafood, vegetables, grains, potato, egg, beans including tofu, fruits, milk, cheese, deserts, snacks, pickles, seasonings and alcohol, as established by the Working Committee for Health Guideline of the Japanese Ministry of Health and Welfare for Japanese people. The average intake at one meal was confirmed by showing examples of food models or photographs. Average daily nutrient intake (kcal/day) for the most recent month was calculated using standard food composition tables for Japan18). Prior to the start of the intervention program, each participant was provided with dietary advice regarding changes to improve their eating habits and caloric intake.
Physical activity
Habitual physical activity was assessed before and after the intervention using a questionnaire, which was subdivided into physical activity, including walking and other physical activity (exercise) during leisure time. Participants counted the number of steps they took using a pedometer for one week before the intervention and during the program. We calculated the total daily energy expenditure (kcal/day) for REE and physical activity. Physical activity calorie expenditure was calculated as follows: body weight (kg)×metabolic equivalent (Met)×time (h). Defining Met for sitting/resting as 1, for example, that of normal walking is 3. We evaluated Met as an index for intensity of physical activity according to the Exercise and Physical Activity Guide19). Prior to the start of the intervention program, all participant received advice regarding changes to improve their physical activity.
Statistical analyses
We evaluated lifestyle modification as an energy balance per day by calculating the energy intake and expenditure of participants. Participants were divided into an employed group and an unemployed group, the latter of which included housewives, farmers and self-employed persons. Analysis of data was done with SPSS statistical analysis software (Version 17.0J, SPSS Japan Inc., Tokyo, Japan). Results are expressed as mean ± S.D. Comparisons between gender and employment situation were performed by the Student’s t-test to assess the differences in anthropometric parameters and energy balance. To evaluate whether gender or employment situation had affected values in the intervention, we used a paired Student’s t-test. An χ2 test was used for frequency of dropout by gender or employment situation. Multiple linear regression analysis was done to investigate whether weight loss was independently related to gender, employment situation or energy balance. A nominal two-sided P value of less than 0.05 was used to assess significance.
Results
Characteristics of dropout group in behavioral intervention
The characteristics of the participants in the behavioral intervention are shown in Table 1. In total, 102 men and 282 women participated in the interventional program, with 11 men (10.8%) and 15 women (5.3%) dropping out. This dropout group was significantly younger for both genders, with a higher rate of employment for the women than for the completing group. There was no significant difference in dropout rate by gender. Compared with the continuing group, the dropout women were significantly heavier and the men had significantly larger WCs, but there were no significant differences in intake and expenditure of energy in either gender.
Table 1. Characteristics of all participants in behavioral intervention.
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| Completing | Dropouts | P | Completing | Dropouts | P | |
| Number | 91 | 11 | 267 | 15 | ||
| Age (years) | 56.2 ± 9.5 | 49.6 ± 10.9 | 0.031 | 56.3 ± 8.0 | 49.3 ± 8.7 | 0.001 |
| Purpose of participation | ||||||
| Weight loss | 81.3% | 81.8% | NS | 83.9% | 80.0% | NS |
| Improvement of metabolic disorders | 15.4% | 18.2% | 15.4% | 13.3% | ||
| Others | 3.3% | 9.1% | 0.7% | 6.7% | ||
| Body weight (kg) | 72.9 ± 10.7 | 68.5 ± 8.8 | NS | 59.0 ± 8.3 | 63.3 ± 7.7 | NS |
| BMI (kg/m2) | 26.0 ± 3.2 | 24.3 ± 2.0 | NS | 24.7 ± 3.0 | 26.5 ± 3.3 | 0.032 |
| Waist circumference (cm) | 89.7 ± 8.7 | 83.7 ± 6.0 | 0.003 | 79.6 ± 9.6 | 81.6 ± 10.0 | NS |
| Energy intake (kcal) | 2278 ± 497 | 2453 ± 665 | NS | 1946 ± 392 | 1809 ± 425 | NS |
| Energy expenditure (kcal) | 2373 ± 620 | 2120 ± 687 | NS | 1831 ± 426 | 1888 ± 410 | NS |
| Employed | 59 | 10 | NS | 105 | 11 | 0.009 |
| Unemployed | 32 | 1 | 162 | 4 | ||
Data are expressed as means ± standard deviation. The difference between completing subjects and dropouts were tested by either the χ2 test or Student’s t-test. NS: nonsignificant (P≥0.05).
Characteristics of the completing group at the baseline
Characteristics of the completing group in the behavioral intervention at baseline are shown in Table 2. Men and women were of the same average age (56 y), but showed a significant difference for overweight (BMI: 26.0 kg/m2 in men; 24.7 kg/m2 in women) and visceral obesity (WC: 89.7 cm in men; 79.6 cm in women).
Table 2. Baseline data and results of to behavioral intervention of the completing group.
| Baseline |
Results at three months |
|||||
|---|---|---|---|---|---|---|
| Men | Women | P | Men | Women | P | |
| Number | 91 | 267 | 91 | 267 | ||
| Age (years) | 56.2 ± 9.5 | 56.3 ± 8.0 | NS | |||
| Body weight (kg) | 72.9 ± 10.7 | 59.0 ± 8.3 | <0.001 | –1.9 ± 2.1* | –1.6 ± 2.0* | NS |
| BMI (kg/m2) | 26.0 ± 3.2 | 24.7 ± 3.0 | 0.001 | –0.68 ± 0.73* | –0.66 ± 0.85* | NS |
| Waist circumference (cm) | 89.7 ± 8.7 | 79.6 ± 9.6 | <0.001 | –2.4 ± 3.2* | –2.3 ± 3.1* | NS |
| Energy intake (kcal) | 2278 ± 497 | 1946 ± 392 | <0.001 | –386 ± 404* | –259 ± 365* | 0.006 |
| Energy intake (kcal/bw) | 32 ± 7 | 33 ± 8 | NS | –5 ± 6* | –4 ± 6* | NS |
| Protein (g) | 76 ± 19 | 70 ± 17 | 0.002 | –8 ± 15* | –5 ± 16* | NS |
| Lipid (g/day) | 59 ± 21 | 57 ± 18 | NS | –13 ± 18* | –10 ± 17* | NS |
| Carbohydrate(g) | 308 ± 88 | 283 ± 66 | 0.005 | –46 ± 65* | –33 ± 61* | NS |
| Alcohol (kcal) | 218 ± 205 | 30 ± 51 | <0.001 | –53 ± 137* | –13 ± 36* | <0.001 |
| Energy expenditure (kcal) | 2373 ± 620 | 1831 ± 426 | <0.001 | 176 ± 142* | 127 ± 102* | <0.001 |
| Energy expenditure (kcal/bw) | 33 ± 9 | 31 ± 7 | NS | 3 ± 3* | 3 ± 2 | NS |
| Walking (kcal) | – | – | – | 120 ± 86* | 101 ± 82* | NS |
| Exercise without walking (kcal) | – | – | – | 60 ± 95* | 26 ± 56* | <0.001 |
| Resting energy expenditure (kcal) | 1849 ± 416 | 1387 ± 311 | <0.001 | –51 ± 361* | 43 ± 287 | 0.017 |
| Resting energy expenditure (kcal/bw) | 26 ± 6 | 24 ± 5 | 0.002 | –0.0 ± 5.1 | 1.5 ± 4.9 | 0.019 |
| Energy balance (kcal) | – | – | – | –562 ± 402 | –386 ± 398 | <0.001 |
| Energy balance (kcal/bw) | – | – | – | –8 ± 6 | –7 ± 7 | NS |
Data are expressed as means ± standard deviation. *The difference by intervention was tested by the paired Student’s t-test. The difference between men and women was tested by the Student’s t-test. NS: nonsignificant (P≥0.05).
Men had significantly higher intakes and expenditures of energy compared with women, but there were no such significant differences when expressed relative to body weight at baseline. For the intake of major nutrients, men took in more protein, carbohydrates and alcohol than women, but intake of lipid showed no significant difference by gender. Physical activity during leisure time mainly consisted of walking.
Response by gender to behavioral intervention
Response to the behavioral intervention by gender is shown in Table 2. The intervention resulted in a significant reduction in body weight (1.9 kg in men, 1.6 kg in women) and BMI (0.68 kg/m2 in men and 0.66 kg/m2 in women). There was no significant difference in weight, BMI or WC (2.4 cm in men and 2.3 cm in women) by gender. Seventy-six men (83.5%) and 209 women (78.3%) reduced their body weight; the range of changes in body weight was from 2.2 kg to –11.2 kg.
Daily food intakes were significantly reduced in terms of energy (men –17%; women –13%), protein (men –11%; women –7%), fat (men –22%; women –18%), carbohydrates (men –15%; women –12%) and alcohol (men –24%; women –43%) following intervention. Intervention induced significant decreases in intake of energy (386 kcal in men and 259 kcal in women) and alcohol (53 kcal and 13 kcal), but the change in intake of protein, lipid and carbohydrate was not significant by gender before and after intervention, respectively.
Habitual physical activity significantly increased (walking and exercise: 120 and 60 kcal in men and 101 and 26 kcal in women, respectively) after intervention compared with the baseline. Increases in energy expenditure from walking by gender were not significant, but those from exercise in men compared with women before and after intervention were significant.
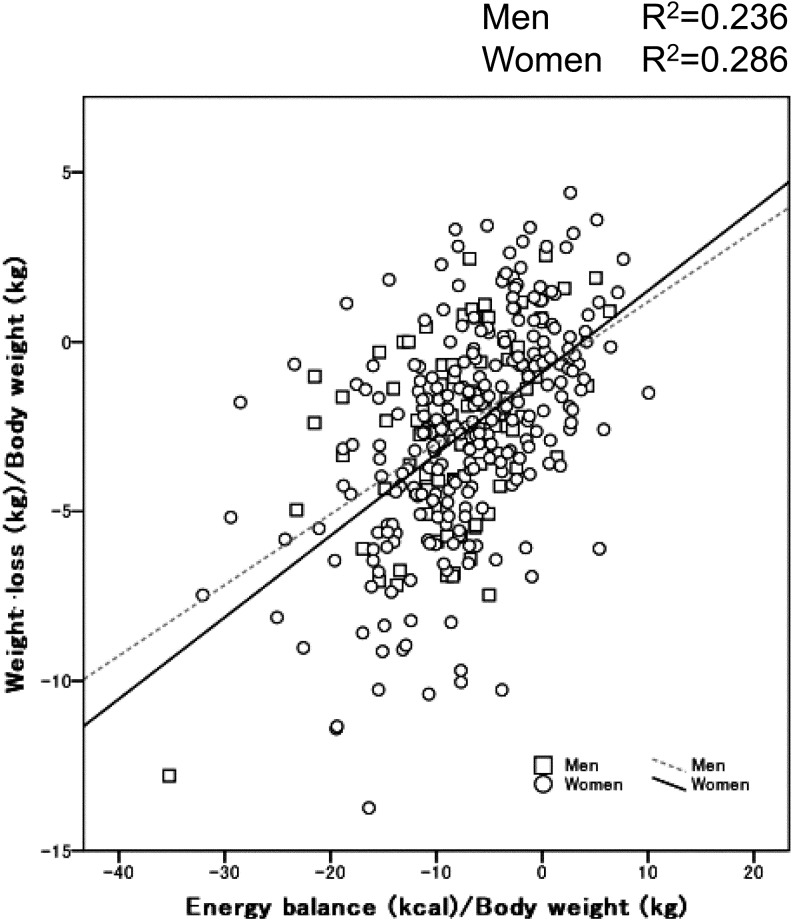
Energy balance significantly decreased in men (562 kcal) compared with in women (386 kcal), with no significant difference in energy balance by gender. The relationship between weight loss and energy balance is shown in Figure 1, which expresses values adjusted for body weight at the baseline for gender comparisons. A positive correlation between weight loss and energy balance was observed in both the men and women. Furthermore, adjusted R2 values (0.236 in men and 0.286 in women) between weight loss and changes in energy balance were significant, but the relationship between weight loss and changes in energy balance by gender was not significant according to multiple regression analysis (Table 3).
Figure 1.
Relationship between weight loss and change in energy balance by gender.
Table 3. Standard regression coefficients (b) for weight-loss (kg)/body weight (kg) at the baseline using multiple regression analysis.
| Independent variables | R2 | F | β | P | |
|---|---|---|---|---|---|
| Model 1 | 0.281 | 46.2 | <0.001 | ||
| Gender | –0.012 | NS | |||
| Employment pattern | 0.097 | 0.036 | |||
| Changes in energy balance/bw | 0.518 | <0.001 | |||
| Model 2 | 0.284 | 46.7 | <0.001 | ||
| Gender | –0.033 | NS | |||
| Age | –0.107 | 0.018 | |||
| Changes in energy balance/bw | 0.518 | <0.001 | |||
| Model 3 | 0.286 | 35.3 | <0.001 | ||
| Gender | –0.021 | NS | |||
| Age | –0.079 | NS | |||
| Employment pattern | 0.056 | NS | |||
| Changes in energy balance/bw | 0.516 | <0.001 | |||
Multiple linear regression analysis was conducted to investigate whether weight loss was independently related to gender, employment situation or energy balance. NS: nonsignificant (P≥0.05).
Response by employment status to behavioral intervention
The baseline data and response to the behavioral intervention by employment situation are shown in Table 4. At the baseline, employed participants were significantly younger for both genders, with lower values for BMI and WC in women compared with the unemployed group. The employed group had no significant differences in intake and expenditure of energy compared with the unemployed group, but there were significant differences in intake of lipid between the women before and after intervention.
Table 4. Baseline data and response to behavioral intervention by employment pattern.
| Men |
Women |
||||||
|---|---|---|---|---|---|---|---|
| Unemployed | Employed | P | Unemployed | Employed | P | ||
| Number | 32 | 59 | 162 | 105 | |||
| Age (years) | 64.5 ± 4.4 | 51.8 ± 8.5 | <0.001 | 59.1 ± 6.9 | 51.8 ± 7.6 | <0.001 | |
| Purpose of participation | |||||||
| Weight-loss | 78.1% | 83.1% | NS | 84.6% | 82.9% | NS | |
| Improvement of metabolic disorders | 18.8% | 13.6% | 14.8% | 16.2% | |||
| Others | 3.1% | 3.4% | 0.6% | 1.0% | |||
| Baseline | Body weight (kg) | 70.1 ± 8.7 | 74.5 ± 11.3 | NS | 59.5 ± 8.5 | 58.4 ± 7.9 | NS |
| BMI (kg/m2) | 25.4 ± 2.4 | 26.3 ± 3.6 | NS | 25.3 ± 3.0 | 24.2 ± 3.0 | 0.016 | |
| Waist circumference (cm) | 88.9 ± 6.9 | 90.1 ± 9.6 | NS | 81.2 ± 9.5 | 77.1 ± 9.3 | 0.001 | |
| Energy intake (kcal/bw) | 2295 ± 587 | 2269 ± 446 | NS | 1936 ± 407 | 1962 ± 369 | NS | |
| Protein (g) | 77 ± 21 | 76 ± 18 | NS | 69 ± 18 | 71 ± 15 | NS | |
| Lipid (g/day) | 58 ± 26 | 60 ± 18 | NS | 55 ± 17 | 60 ± 19 | 0.026 | |
| Carbohydrate (g) | 323 ± 104 | 301 ± 77 | NS | 287 ± 71 | 278 ± 58 | NS | |
| Alcohol (kcal) | 189 ± 194 | 234 ± 210 | NS | 26 ± 47 | 36 ± 55 | NS | |
| Energy expenditure (kcal) | 2367 ± 571 | 2376 ± 649 | NS | 1841 ± 426 | 1816 ± 428 | NS | |
| Response | Body weight (kg) | –2.5 ± 1.7 | –1.6 ± 2.2 | 0.038 | –1.7 ± 2.0 | –1.4 ± 1.9 | NS |
| BMI (kg/m2) | –0.92 ± 0.59 | –0.55 ± 0.77 | 0.021 | –0.71 ± 0.84 | –0.57 ± 0.88 | NS | |
| Waist circumference (cm) | –3.4 ± 2.6 | –1.9 ± 3.3 | 0.023 | –2.5 ± 3.1 | –2.0 ± 3.0 | NS | |
| Energy intake (kcal/bw) | –388 ± 508 | –385 ± 340 | NS | –252 ± 369 | –270 ± 362 | NS | |
| Protein (g) | –8 ± 17 | –8 ± 14 | NS | –5 ± 17 | –6 ± 14 | NS | |
| Lipid (g/day) | –13 ± 21 | –13 ± 16 | NS | –10 ± 16 | –11 ± 18 | NS | |
| Carbohydrate (g) | –48 ± 86 | –45 ± 51 | NS | –34 ± 63 | –32 ± 56 | NS | |
| Alcohol (kcal) | –50 ± 126 | –55 ± 144 | NS | –11 ± 35 | –18 ± 36 | NS | |
| Energy expenditure (kcal) | 246 ± 174 | 138 ± 104 | <0.001 | 142 ± 108 | 104 ± 87 | 0.002 | |
| Walking (kcal) | 145 ± 100 | 106 ± 74 | 0.040 | 110 ± 85 | 86 ± 75 | 0.018 | |
| Exercise except walking (kcal) | 101 ± 130 | 31 ± 57 | 0.001 | 32 ± 63 | 18 ± 43 | 0.039 | |
| Energy balance (kcal) | –635 ± 458 | –523 ± 368 | NS | –394 ± 405 | –374 ± 389 | NS | |
Data are expressed as means ± standard deviation. *The difference by intervention was tested by the paired Student’s t-test. The difference between completing subjects and dropouts were tested by either the χ2 test or Student’s t-test. NS: nonsignificant (P≥0.05).
Intervention resulted in significant decreases in weight (1.6 kg in employed, 2.5 kg in unemployed) and WC (1.9 cm and 3.4 cm, respectively) in men. In women, body weight (1.4 kg in employed, 1.7 kg in unemployed) and WC (2.0 cm and 2.5 cm, respectively) decreased in the employed group, but neither were significant either before or after intervention.
There were significant increases in walking and exercise but no significant decrease in energy intake before or after intervention for both genders. The relationship between weight loss and changes in energy balance by employment status was independently significant according to multiple regression analysis (Table 3).
Discussion
The present intervention for 3 months yielded a 3% reduction in body weight and WC at baseline. Weight loss was affected by decreases in intake of energy and increases in physical activities, as indicated by higher scores (0.518) of β of energy balance using multiple regression analysis. The National Heart, Lung and Blood Institute in the U.S.A. has recommended that the initial goal of weight loss therapy be the lowering of body weight by approximately 10 percent from baseline over a 6-month period20). Therefore, we recommended to our participants that they attempt to achieve a 5% weight loss over 3 months. Our results indicate some improvement in anthropometric and metabolic levels8,9), however, we consider the results unsatisfactory insofar as the anthropometric parameters are concerned. This is principally because while physical activity was significantly increased during the program, participants failed to achieve the 5% weight reduction target. Therefore, we must consider additional factors in the search for more effective lifestyle modification and weight loss for future intervention programs.
Our intervention resulted in significantly smaller reductions in body weight and WC in the employed men and only slight decreases for employed women compared with the unemployed group. Difficulties in weight loss for the employed were associated with an inadequate increase in walking and exercise. The decrease in energy intake was similar for both the employed and unemployed. Multiple regression analysis confirmed that the relationship between weight loss and employment status was independent of changes in energy balance. The present study suggests that being an employee in Japan is associated with difficulty in losing weight due to limited exercise time in behavioral intervention.
Most studies reporting on unsuccessful weight loss in western countries have shown an association with unemployment and poor income, whereas our results demonstrated a link between employment and unsuccessful weight loss. This suggests that the Japanese employee is too busy with work-related duties to take time to engage in health-promoting activities, either in the workplace or at home21,22). The demands of a greater workload may factor into the eating disorders and sedentary lifestyle of the Japanese worker14). In contrast, our unemployed group, which included housewives, farmers and the self-employed, had free time available in which to focus on physical exercise and activity.
It has also been reported that women have a greater ability to induce weight loss than men11,12,13). However, our results showed that gender was not an independent predictor for successful weight loss or completion of the intervention. Changes in weight and energy balance in men were greater than in women. Previous behavioral studies have shown initial body weight and extreme obesity to be significantly associated with subsequent weight loss8,23). Furthermore, body weight was the major determinant of REE in obese subjects24). Therefore, we evaluated changes in weight and energy balance relative to body weight at baseline. Any significant differences in changes in energy balance by gender disappeared after adjustment for body weight. There were also no significant gender-related differences in weight loss or energy balance changes in the multiple regression analyses. Thus, although differences in weight loss by gender have been reported in many prior studies, the participant’s employment situation was the more powerful factor in our case.
As for the participants who did not complete the intervention, this group was younger and had a higher rate of employment relative to the completing group. Dalle Grave et al.25) also reported that their dropouts were significantly younger than those completing the program. The fact that most younger participants work, together with the psychosocial factors of youth, likely affect the dropout rate during intervention26).
Japanese workers engaged in constant overtime work experience mental and physical stress due to the excessive workload and sleep deprivation22). The prevalence of overweight and obesity in the workplace is increasing rapidly in most countries due to the work environment. Therefore, overweight and obesity can be considered a work-related disease that needs to be controlled in the workplace5,27). Japan’s Ministry of Health, Labour and Welfare introduced a nationwide health screening and intervention program in April 2008 specifically targeting metabolic syndrome6), but only screening for visceral obesity and metabolic syndrome was implemented in 2008. Certain cost-effective strategies for preventing and controlling overweight and obesity in employees have been identified for worksite settings. However, job insecurity and stress have become widespread problems due to intensive global competition through the deregulation of labor. This has been shown to have a significant impact on health and a decreased level of social support for a growing number of workers28). As social support is essential to behavioral intervention, lifestyle modification programs should be established at the community level as well as in the workplace for more effective obesity prevention in the employee.
The findings of this study suggest that our short-term intervention methods could be improved to achieve greater success in weight loss and completion rates, particularly in regards to physical activities for employees. The addition of prescribed tailored exercise strategies during work and leisure time seems promising29). Booster interventions such as phone, mail or Internet contact may help to enhance the overall effectiveness of intervention30). Research is also needed into possible changes in the workplace environment, such as making stairs and public transportation more accessible. Initial self-efficacy and perceived barriers to physical activity have been shown to correlate with weight loss in a consistent manner across analyses10). We must also further investigate these motivational and psychosocial factors in employees.
Our approach in this study has some limitations. BMI values and weight loss of participants in our intervention were lower than those in Western countries, but BMI and WC were similar to those reported in several population-based investigations in Japan4, 31), in line with our results. Further, it is known that short-term results do not necessarily continue for the long term, and our study was a short-term 3-month weight loss program. However, as our method included developing each participant’s greater awareness and autonomous improvement of behavior, this may result in a more enduring modification of behavior after completion of the program, as compared with a program incorporating strict compliance with rules and a complicated prescription of lifestyle modification. Finally, the present study done from 2000 to 2006, but there has since been significant change in the trend of occupation and obesity32).
In conclusion, being a Japanese employee in Japan is associated with difficulty in losing weight due to limited exercise time in the course of behavioral intervention. Demonstrated effectiveness of workplace and community efforts to control overweight and obesity may serve to encourage employers to provide required programs of physical activity and exercise.
Acknowledgments
This study was supported in part by Grants-in-Aid (12670355, 14570334 and 20590602 to K.S., 13680173 to A.N.) for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science and Technology.
References
- 1.WHO. Obesity. Preventing and managing the global endemic. WHO Technical Report Series, WHO, Geneva, No. 894, pp. 1–253, 2000. [PubMed] [Google Scholar]
- 2.WHO/IASO/IOTF. The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Health Communications, Australia Pty Ltd., 2000. [Google Scholar]
- 3.Hsieh SD, Yoshinaga H, Muto T, et al. Health risks among Japanese men with moderate body mass index. Int J Obes Relat Metab Disord 2000; 24: 358–362. doi: 10.1038/sj.ijo.0801157 [DOI] [PubMed] [Google Scholar]
- 4.Yoshiike N, Seino F, Tajima S, et al. Twenty-year changes in the prevalence of overweight in Japanese adults: The National Nutrition Survey 1976-1995. Obes Rev 2002; 3: 183–190. doi: 10.1046/j.1467-789X.2002.00070.x [DOI] [PubMed] [Google Scholar]
- 5.Katz DL, O’Connell M, Yeh MC, et al. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep 2005; 54 (RR-10): 1–12. [PubMed] [Google Scholar]
- 6.Kohro T, Furui Y, Mitsutake N, et al. The Japanese national health screening and intervention program aimed at preventing worsening of the metabolic syndrome. Int Heart J 2008; 49: 193–203. doi: 10.1536/ihj.49.193 [DOI] [PubMed] [Google Scholar]
- 7.Lindström J, Louheranta A, Mannelin M, et al. Finnish Diabetes Prevention Study GroupThe Finnish Diabetes Prevention Study (DPS): Lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 2003; 26: 3230–3236. doi: 10.2337/diacare.26.12.3230 [DOI] [PubMed] [Google Scholar]
- 8.Shiwaku K, Nogi A, Anuurad E, et al. Difficulty in losing weight by behavioral intervention for women with Trp64Arg polymorphism of the beta3-adrenergic receptor gene. Int J Obes Relat Metab Disord 2003; 27: 1028–1036. doi: 10.1038/sj.ijo.0802375 [DOI] [PubMed] [Google Scholar]
- 9.Li L, Ikenishi R, Iwamoto M, et al. Predictive values of anthropometric measurements for visceral obesity and metabolic syndrome in educational intervention. J Jpn Assoc Rural Med 2008; 56: 852–862(In Japanese). [Google Scholar]
- 10.Teixeira PJ, Going SB, Sardinha LB, et al. A review of psychosocial pre-treatment predictors of weight control. Obes Rev 2005; 6: 43–65. doi: 10.1111/j.1467-789X.2005.00166.x [DOI] [PubMed] [Google Scholar]
- 11.Davis NJ, Emerenini A, Wylie-Rosett J. Obesity management: physician practice patterns and patient preference. Diabetes Educ 2006; 32: 557–561. doi: 10.1177/0145721706290437 [DOI] [PubMed] [Google Scholar]
- 12.Martín AR, Nieto JM, Ruiz JP, et al. Overweight and obesity: the role of education, employment and income in Spanish adults. Appetite 2008; 51: 266–272. [DOI] [PubMed] [Google Scholar]
- 13.Thande NK, Hurstak EE, Sciacca RE, et al. Management of obesity: a challenge for medical training and practice. Obesity 2009; 17: 107–113. doi: 10.1038/oby.2008.478 [DOI] [PubMed] [Google Scholar]
- 14.Suwazono Y, Okubo Y, Kobayashi E, et al. A follow-up study on the association of working conditions and lifestyles with the development of (perceived) mental symptoms in workers of a telecommunication enterprise. Occup Med (London) 2003; 53: 436–442. doi: 10.1093/occmed/kqg102 [DOI] [PubMed] [Google Scholar]
- 15.McCormack G, Giles-Corti B, Lange A, et al. An update of recent evidence of the relationship between objective and self-report measures of the physical environment and physical activity behaviours. J Sci Med Sport 2004; 7(1 Suppl): 81–92. doi: 10.1016/S1440-2440(04)80282-2 [DOI] [PubMed] [Google Scholar]
- 16.Corp VINE . The instruction manual of nondispersive infrared analysis. VINE Corp, Tokyo, 2000. [Google Scholar]
- 17.Morimoto A, Takase Y, Hada K, et al. Evaluation of a “convenient method” for the estimation dietary food consumption. Jpn J Nutr 1977; 35: 235–245(In Japanese). doi: 10.5264/eiyogakuzashi.35.235 [DOI] [Google Scholar]
- 18.The Science and Technology Agency of Japan Standard Tables of Food Composition in Japan, 5th revised ed. Ministry of Finance Printing Bureau, Tokyo, Japan, 2005. [Google Scholar]
- 19.The Office for Lifestyle-Related Diseases Control Exercise and Physical Activity Guide for Health Promotion 2006 General Affairs Division, Health Service Bureau, Ministry of Health, Labour and Welfare of Japan, Tokyo, 2006. [Google Scholar]
- 20.The National Heart Lung and Blood Institute Obesity Education Initiative Expert Panel Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. National Institute of Health Publication, Bethesda, USA No. 98-4083, 1998. [Google Scholar]
- 21.Ikeda T, Nakata A, Takahashi M, et al. Correlates of depressive symptoms among workers in small- and medium-scale manufacturing enterprises in Japan. J Occup Health 2009; 51: 26–37. doi: 10.1539/joh.L7012 [DOI] [PubMed] [Google Scholar]
- 22.Sato Y, Miyake H, Thériault G. Overtime work and stress response in a group of Japanese workers. Occup Med (London) 2009; 59: 14–19. doi: 10.1093/occmed/kqn141 [DOI] [PubMed] [Google Scholar]
- 23.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999; 67: 132–138. doi: 10.1037/0022-006X.67.1.132 [DOI] [PubMed] [Google Scholar]
- 24.Aull JL, Rowe DA, Hickner RC, et al. Energy expenditure of obese, overweight, and normal weight females during lifestyle physical activities. Int J Pediatr Obes 2008; 3: 177–185. doi: 10.1080/17477160701874844 [DOI] [PubMed] [Google Scholar]
- 25.Dalle Grave R, Calugi S, Molinari E, et al. Weight loss expectations in obese patients and treatment attrition: an observational multicenter study. Obes Res 2005; 13: 1961–1969. doi: 10.1038/oby.2005.241 [DOI] [PubMed] [Google Scholar]
- 26.Hebl MR, Ruggs EN, Singletary SL, et al. Perceptions of obesity across the lifespan. Obesity 2008; 16 (Suppl 2): S46–S52. doi: 10.1038/oby.2008.458 [DOI] [PubMed] [Google Scholar]
- 27.Gabel JR, Whitmore H, Pickreign J, et al. Obesity and the workplace: current programs and attitudes among employers and employees. Health Aff (Millwood) 2009; 28: 46–56. doi: 10.1377/hlthaff.28.1.46 [DOI] [PubMed] [Google Scholar]
- 28.Cheng Y, Chen CW, Chen CJ, et al. Job insecurity and its association with health among employees in the Taiwanese general population. Soc Sci Med 2005; 61: 41–52. doi: 10.1016/j.socscimed.2004.11.039 [DOI] [PubMed] [Google Scholar]
- 29.Santos R, Silva P, Santos P, et al. Physical activity and perceived environmental attributes in a sample of Portuguese adults: results from the Azorean physical activity and health study. Prev Med 2008; 47: 83–88. doi: 10.1016/j.ypmed.2008.02.027 [DOI] [PubMed] [Google Scholar]
- 30.Müller-Riemenschneider F, Reinhold T, Nocon M, et al. Long-term effectiveness of interventions promoting physical activity: A systematic review. Prev Med 2008; 47: 354–368. doi: 10.1016/j.ypmed.2008.07.006 [DOI] [PubMed] [Google Scholar]
- 31.Shiwaku K, Anuurad E, Enkhmaa B, et al. Overweight Japanese with body mass indexes of 23.0-24.9 have higher risks for obesity-associated disorders: a comparison of Japanese and Mongolians. Int J Obes Relat Metab Disord 2004; 28: 152–158. doi: 10.1038/sj.ijo.0802486 [DOI] [PubMed] [Google Scholar]
- 32.National Institute of health and Nutrition. The National Health and Nutrition Survey Japan, 2010. The Japanese Ministry of Health, Labour and Welfare, 2012. (In Japanese).