Abstract
Background
New oral anticoagulants have similar efficacy and lower bleeding rates compared with warfarin. However, in case of bleeding there is no specific antidote to reverse their effects. We evaluated the preferences and values of anticoagulants of patients at risk of atrial fibrillation and those who have already made a decision regarding anticoagulation.
Methods
We conducted a cross-sectional study of Veterans in the primary care clinics and the international normalized ratio (INR) laboratory. We developed an instrument with patient and physician input to measure patient values and preferences. The survey contained a hypothetical scenario of the risk of atrial fibrillation and the attributes of each anticoagulant. After the scenario, we asked participants to choose the option that best fits their preferences. The options were: 1) has better efficacy at reducing risk of stroke; 2) has been in the market for a long period of time; 3) has an antidote to reverse the rare case of bleeding; 4) has better quality of life profile with no required frequent laboratory tests; or 5) I want to follow physician recommendations. We stratified our results by those patients who are currently exposed to anticoagulants and those who are not exposed but are at risk of atrial fibrillation.
Results
We approached 173 Veterans and completed 137 surveys (79% response rate). Ninety subjects were not exposed to anticoagulants, 46 reported being on warfarin, and one reported being on dabigatran at the time of the survey. Ninety-eight percent of subjects stated they would like to participate in the decision-making process of selecting an anticoagulant. Thirty-six percent of those exposed and 37% of those unexposed to anticoagulants reported that they would select a medication that has an antidote even if the risk of bleeding was very small. Twenty-three percent of the unexposed and 22% of the exposed groups reported that they would prefer the medication that gives the best quality of life.
Conclusion
Our study found that patients who may be exposed to an anticoagulation decision prefer to actively participate in the decision-making process, and have individual values for making a decision that cannot be predicted or assumed by anyone in the health care system.
Keywords: warfarin, oral anticoagulant, bleeding risk, atrial fibrillation, patient decision making, medication selection
Introduction
Warfarin has been an effective medication for the prevention of stroke among atrial fibrillation (AF) patients for many decades.1 However, it requires frequent international normalized ratio (INR) monitoring and diet restrictions that impact quality of life.2 Only half of patients with AF and without a contraindication to anticoagulation use warfarin.3 This underutilization is not fully understood; however, physicians’ bleeding risk perceptions might play a role.4
Novel anticoagulants (NOAC) have been a welcomed alternative for the prevention of stroke among subjects with AF.5 Several non-inferiority studies showed that the NOAC are at least as effective as warfarin and that at efficacious doses have similar to lower rates of bleeding.6 Yet, the lack of a drug-specific antidote that could reverse anticoagulation in case of an emergency has raised concerns about the safety of these medications when used in real-world settings.7 The introduction of the NOAC gives patients anticoagulation options, although only 25%–37% of patients reported discussing these options with their physicians.8,9
Given the increasing complexity of selecting an anticoagulant, it is imperative that we finally understand how patients prefer to approach their options, and their perspectives on the information that matters to them. Our study explores patient preferences and values regarding the current anticoagulant alternatives. This knowledge will help us develop strategies to achieve shared decision making (SDM) for anticoagulant selection and evaluate the impact of SDM on adherence to these medications.
Methods
Study population
Between May and August 2013, we recruited patients from the waiting area of the primary care clinics and from the outpatient laboratory at the Miami Veterans Affairs (VA) Medical Center, Miami, Florida. Recruitment occurred on alternating days, and we attempted to recruit all patients present in the primary care clinic between 8 am and 12 pm, and all subjects going to the laboratory for INR monitoring. The rationale for recruiting patients from both the primary care clinic and the anticoagulation laboratory was to ensure the inclusion of patients at risk of AF and not exposed to anticoagulants as well as patients on anticoagulants. Recruiting patients at risk of AF rather than those who have already made a decision about which anticoagulant to take prevents bias as a result of cognitive dissonance. Cognitive dissonance is a state of struggle or mental conflict that ensues when beliefs or cognitions are contradicted by new information. When cognitive dissonance occurs, most subjects reject, explain, or avoid the new information.10 Other investigators evaluating decision making regarding anticoagulation have reported this strategy of including subjects at risk of AF rather than subjects who have already made an anticoagulation decision.11
Twenty percent of the patients attending the Miami VA primary care clinics and clinical laboratories are above 65 years of age, 60% belong to a minority group, 65% have hypertension, and 10% have heart failure. The use of NOAC is non-formulary at the Miami VA primary care clinics, limiting our ability to recruit subjects taking these medications. We conducted this pilot study as preparation for research for a Patient Centered Outcomes Research Institute proposal. Our purpose was to achieve diverse participation of patients who may be exposed to an anticoagulation decision.
Survey instrument
To create our survey instrument, we performed key informant interviews with four AF patients to discuss what they knew about anticoagulant medications and how they viewed different scenarios of risk and benefits. We also asked them to discuss medication characteristics of importance to them (mild or serious side effects, convenience, quality of life, efficacy, costs, etc). We also interviewed four cardiologists to address their perspectives on preferences and their perceptions of what characteristics would be important to the patient. Using this information, we developed our instrument, which was reviewed by a cardiologist, three primary care physicians, and one patient regarding the language and the pertinence of the questions. We pilot-tested the survey on ten patients and made minor revisions to the questions to improve understanding of their meaning.
The questionnaire started by asking subjects to self-report AF status and use of anticoagulation. Then, we gave subjects a hypothetical scenario describing the risks of having AF, and the advantages and disadvantages of the different types of anticoagulants. The survey continued with eight questions that addressed the following: 1) patients’ preferences regarding participation in the decision-making process; 2) anticoagulation options that seemed more aligned with their values; 3) the reason or anticoagulant characteristic that prompted the patient choice; 4) patients’ preferences with respect to relying on the physician preference versus making their own decision; 5) the effect of the cost factor on patient decisions; 6) and the way the patient would like to receive information regarding this issue; 7) the desire to receive new information once a decision has been made; 8) comfort level with revisiting the decision with the physician in light of new information. The hypothetical scenario was as follows:
You have been diagnosed with a heart condition that increases the chance of having a stroke. The rhythm in your heart is not normal and from now on it is advisable for you to take a blood thinner to reduce your risk of having a stroke. There are several options: 1. A blood thinner or anticoagulant (warfarin) that has been on the market for decades and successfully reduces the risk of stroke if the blood is adequately thinned. To make sure of that, the doctor orders blood tests with certain frequency to keep anticoagulation appropriate. In some patients, the blood could get overly thinned or over anticoagulated. When that happens the risk of bleeding increases. Serious bleeding, although rare, can occur in your brain or in your gut. If this happens the doctor can hold your medication and even give you an antidote that reverses the anticoagulation and gets the blood back to normal. 2. A new anticoagulant or blood thinning medication, which is as good as the older one at reducing the risk of stroke, some studies suggest that it may be slightly better. For this medication, there is no need to check blood tests to make sure the blood is adequately thinned. Still the blood can get too thin and patients may very rarely bleed in the brain or gut in the same way that could happen with the older medication. There is no antidote for this medication so doctors cannot get the blood back to normal in the case of an emergency.
The scenario was followed by a question evaluating patients’ perspectives about their options. The question reads as follows:
For me the best strategy when making a decision is to a) choose the medication that can reduce the most my risk of stroke even if there is no antidote, b) choose the medication that has been in the market the longest even if that means having frequent blood tests, c) choose the medication that gives me the best quality of life by not needing frequent blood tests, especially If the risks of bleeding and stroke are fairly similar among all medications and if bleeding is rare, d) choose the medication that has an antidote, and e) allow the doctor to make the decision for me.
Patients had to read all options and then choose the one that best described their preference. On the other hand, the question that addressed how patients would like to receive information allowed patients to mark all the options that applied.
Results
Out of 173 veterans approached, we completed 137 surveys for a response rate of 79%. All patients were male and of the 137 subjects, 90 subjects did not self-report AF or exposure to anticoagulants, 46 subjects self-reported being on warfarin, and one subject self-reported being on dabigatran at the time of the survey.
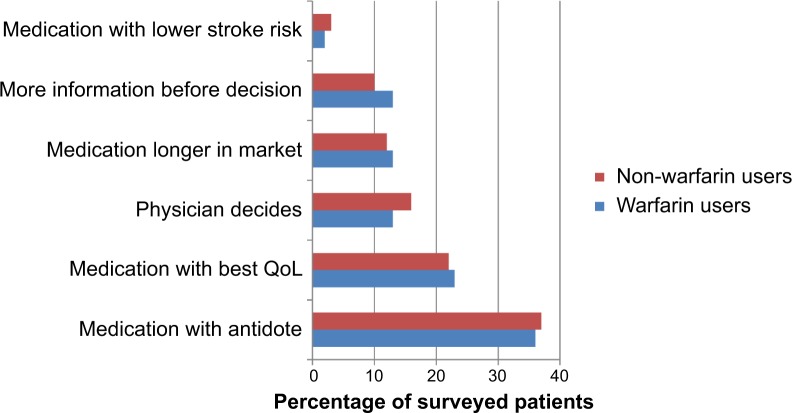
Ninety-eight percent of subjects stated they would like to participate in the decision-making process of selecting an anticoagulant. Figure 1 identifies the preferences and values for selecting an anticoagulant for both those subjects unexposed and those subjects exposed to anticoagulants. Thirty-six percent of those exposed and 37% of the unexposed reported that they would select a medication that has an antidote even if the risk of bleeding was very small. The second most commonly cited attribute of importance was the “medication that gives the best quality of life”, reported by 23% of the unexposed and 22% of the exposed. The distribution of medication attributes cited as important was similar between exposed and unexposed AF subjects. The largest difference was three percentage points for “letting the physician make the decision”, which was slightly more common among those unexposed to warfarin, and for “needing more information before making the decision”, which was slightly more common among warfarin users.
Figure 1.
Anticoagulant preferences that influence medication selection among all surveyed patients stratified by warfarin exposure status.
Abbreviation: QoL, quality of life.
Only 16% of all subjects stated that the best way to make a decision is doing what the doctor thinks is best. This perception was slightly different between subjects exposed to warfarin (13%) and those not exposed (16%). Seventy-five percent of all subjects stated that they would like to receive new information even after making their anticoagulation decision, and 96% stated that after receiving new information they would like to discuss options again with the doctor.
When we asked about the influence that a co-payment of between $20 and $40 may have in their anticoagulation decision, we found that in the Veteran population, 65% would prefer warfarin, 19% would prefer an NOAC, and 16% would like to have more information or let the doctor decide. When introducing financial considerations, the preference for warfarin increased from 50% to 65%, while the preference for NOAC decreased from 25% to 19%.
When asked from whom or from what source subjects would prefer to receive anticoagulation information, the most common answer was from their physician (82%), followed by the pharmacist (42%), and a nurse in the doctor’s office (37%). Other sources were a video they could watch at home (21%), a video they could watch before seeing the doctor (18%), a brochure to take home (16%), or a nurse who would call them at home (15%).
Discussion
This exploratory survey reveals that 85% of subjects want to actively participate in an anticoagulation decision and that the values used to make a selection are broad and potentially different from the values considered important to their physicians. Our study also found that among surveyed veterans, the issues of safety and quality of life were the most important considerations, while efficacy was a less important factor when making a selection of anticoagulant.
Although there are limited data on patient preferences regarding the choice between warfarin and NOAC, the literature that explored the decision between warfarin and aspirin found that patients’ values play an important role in therapy selection and that subjects are at least as interested in the safety of medications and quality of life as they are in efficacy.12 Even more so, a prior qualitative study has shown that anticoagulation issues that matter to patients can vary significantly.13 A clear example of this phenomenon is that the laboratory monitoring needed for warfarin has been described by some patients as reassuring, in the sense that the patient could see that the medication was working, and as nuisance by many others.14
Our study is one of the few studies evaluating how patients would approach a choice between warfarin and NOAC. We were surprised to find that a large proportion of subjects would not consider an NOAC as acceptable due to the lack of an antidote, even when told that the risk of bleeding was very small. We made an effort to present the most relevant positive and negative characteristics identified by patients themselves, and used concise statements without mention of drug names to gauge the characteristics that drove preference. Nevertheless, it was evident in the literature that the way scenarios are presented can influence the selection made.
In a study that presented a stroke scenario and a non-fatal gastrointestinal bleed scenario, patients preferred warfarin over aspirin to reduce risk of stroke in spite of the gastrointestinal bleed risk.15 However, another study found that increasing the reported annual rates of intra-cerebral bleeding from 0.1% per year to 4% led to a drop in the percentage of people accepting anticoagulation treatment from 80% to 39%.16 Alternatively, a study that presented quality of life differences between warfarin and NOAC have found that 58% of patients were willing to switch from NOAC to warfarin.17 Yet, no safety issues were presented, so it is difficult to extrapolate what patients would select as anticoagulant if they received all the information that might be relevant to them.
Our study is one of the few that present the lack of antidote as a characteristic to consider, and surprisingly, this issue played a major role in the selection of anticoagulation. Our preliminary data suggest that the introduction of the NOAC may have shifted the preferences that patients have on the subject, and that the lack of antidote may make them more bleeding averse. Yet, as found by others, anticoagulation perspectives may vary significantly according to age, sex, socio-economic status, and years with the condition.13
Another, interesting finding of our study was the fact that the majority of subjects wanted to make a decision by themselves but still preferred to receive information from their own physicians rather than other sources. This poses many logistical but also perception challenges. Literature evaluating the warfarin versus aspirin decision has found that physicians used a different set of values when making a decision. For example in Devereaux et al, subjects were more stroke averse when choosing between aspirin and warfarin, while the physicians had the opposite distribution of preferences and were more bleeding averse.15 Other literature has also supported the fact that physicians cannot predict patients’ preferences.18 Moreover, physicians tend to believe that SDM regularly occurs when choosing an anticoagulant, while patients believe the physician chose the medications for them.14 It is critical to close this gap in the definition of SDM to be able to satisfy the high proportion of patients that may be interested in making an informed decision.
The use of alternative strategies to direct the anticoagulation discussion, such as using a decision aid tool, may help physicians present information in a patient-centered way and understand what the values guiding the selection are. These tools have shown promising results at improving the understanding of risk and benefits in the warfarin versus aspirin decision.19 Nevertheless, decision aid tools would require significant buy-in from health systems that are generally unaware that a problem exists in the way patients are selecting anticoagulation, particularly due to the limited data demonstrating that interventions that promotes patient-centeredness and improves health behaviors can also improve clinical outcomes.20 Yet, there is a potential non-adherence problem with NOAC; it has been described that more than a quarter of subjects may be taking their NOAC only once a day.8 The recent emphasis on providing patient-centered care and the inclusion of patients’ preferences in evidence-based recommendations21 should allow the introduction of strategies to improve informed decision making in clinical practice.
Our study was an exploratory survey to openly gather trends in patient preferences. This approach was selected, by design, to follow the spirit of patient-centeredness. As such, the study has several methodological limitations. First, we did not conduct a formal process of instrument validation; however, the survey was developed using a patient- and expert-centered approach. Second, we did not collect individual patient characteristics, make preference comparisons between groups, or used numerically-based trade-off scenarios. Our design reflected our goal to understand the broad perspectives patients may have with respect to the tension created by making choices between efficacy, safety, costs, and quality of life issues. Third, since we recruited Veterans (where the new anticoagulants are non-formulary), we were only able to survey one patient taking new anticoagulants. Nevertheless, the purpose was to elicit how the patients would approach this decision, and for that reason we wanted to include a large number of unexposed patients, which was accomplished. Lastly, the values and preferences of the Veterans may differ from those in the general population, and thus this study has unknown external validity.
Conclusion
In conclusion, our study found that patients who may be exposed to an anticoagulation decision prefer to actively participate in the decision-making process, would like to have this discussion with their own physicians, and have individual values for making a decision that cannot be predicted or assumed by anyone in the health care system. In the case of Veteran patients, safety and quality of life were the more important factors. We need to develop feasible strategies to identify patients’ values before anticoagulant selection, test their impact on SDM, and ultimately, test patient values’ influence on the appropriate use of anticoagulants for the prevention of stroke in AF.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857–867. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 2.Kneeland PP, Fang MC. Current issues in patient adherence and persistence: focus on anticoagulants for the treatment and prevention of thromboembolism. Patient Prefer Adherence. 2010;4:51–60. doi: 10.2147/ppa.s6101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stafford RS, Singer DE. National patterns of warfarin use in atrial fibrillation. Arch Intern Med. 1996;156(22):2537–2541. [PubMed] [Google Scholar]
- 4.Hylek EM, D’Antonio J, Evans-Molina C, Shea C, Henault LE, Regan S. Translating the results of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke. 2006;37(4):1075–1080. doi: 10.1161/01.STR.0000209239.71702.ce. [DOI] [PubMed] [Google Scholar]
- 5.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–962. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 6.Gonsalves WI, Pruthi RK, Patnaik MM. The new oral anticoagulants in clinical practice. Mayo Clin Proc. 2013;88(5):495–511. doi: 10.1016/j.mayocp.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Wallace H, Davies MW. The lack of antidotes for new oral anticoagulants. BMJ. 2014;348:g1438. doi: 10.1136/bmj.g1438. [DOI] [PubMed] [Google Scholar]
- 8.Choi JC, Dibonaventura MD, Kopenhafer L, Nelson WW. Survey of the use of warfarin and the newer anticoagulant dabigatran in patients with atrial fibrillation. Patient Prefer Adherence. 2014;8:167–177. doi: 10.2147/PPA.S56187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sardar P, Chatterjee S, Wu WC, Lichstein E, Ghosh J, Aikat S, Mukherjee D. Neworal anticoagulants are not superior to warfarin in secondary prevention of stroke or transient ischemic attacks, but lower the risk of intracranialbleeding: insights from a meta-analysis and indirect treatment comparisons. PLoS One. 2013;8(10):e77694. doi: 10.1371/journal.pone.0077694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Festinger L. A Theory of Cognitive Dissonance. 2nd ed. Redwood City, CA: Stanford University Press; 1962. [Google Scholar]
- 11.Alonso-Coello P, Ebrahim S, Guyatt GH, et al. Evaluating patient values and preferences for thromboprophylaxis decision making during pregnancy: a study protocol. BMC Pregnancy Childbirth. 2012;12:40. doi: 10.1186/1471-2393-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howitt A, Armstrong D. Implementing evidence based medicine in general practice: audit and qualitative study of antithrombotic treatment for atrial fibrillation. BMJ. 1999;318(7194):1324–1327. doi: 10.1136/bmj.318.7194.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moia M, Mantovani LG, Carpenedo M, et al. Patient preferences and willingness to pay for different options of anticoagulant therapy. Intern Emerg Med. 2013;8(3):237–243. doi: 10.1007/s11739-012-0844-3. [DOI] [PubMed] [Google Scholar]
- 14.Borg Xuereb C, Shaw RL, Lane DA. Patients’ and health professionals’ views and experiences of atrial fibrillation and oral-anticoagulant therapy: a qualitative meta-synthesis. Patient Educ Couns. 2012;88(2):330–337. doi: 10.1016/j.pec.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Devereaux PJ, Anderson DR, Gardner MJ, et al. Differences between perspectives of physicians and patients on anticoagulation in patients with atrial fibrillation: observational study. BMJ. 2001;323(7323):1218–1222. doi: 10.1136/bmj.323.7323.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fuller R, Dudley N, Blacktop J. Avoidance hierarchies and preferences for anticoagulation – semi-qualitative analysis of older patients’ views about stroke prevention and the use of warfarin. Age Ageing. 2004;33(6):608–611. doi: 10.1093/ageing/afh202. [DOI] [PubMed] [Google Scholar]
- 17.Attaya S, Bornstein T, Ronquillo N, et al. Study of warfarin patients investigating attitudes toward therapy change (SWITCH Survey) Am J Ther. 2012;19(6):432–435. doi: 10.1097/MJT.0b013e3182373591. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery AA, Fahey T. How do patients’ treatment preferences compare with those of clinicians? Qual Health Care. 2001;10(Suppl 1):i39–i43. doi: 10.1136/qhc.0100039... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Man-Son-Hing M, Laupacis A, O’Connor AM, et al. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: a randomized controlled trial. JAMA. 1999;282(8):737–743. doi: 10.1001/jama.282.8.737. [DOI] [PubMed] [Google Scholar]
- 20.Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. doi: 10.1002/14651858.CD003267.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomson R, Parkin D, Eccles M, Sudlow M, Robinson A. Decision analysis and guidelines for anticoagulant therapy to prevent stroke in patients with atrial fibrillation. Lancet. 2000;355(9208):956–962. doi: 10.1016/S0140-6736(00)90012-6. [DOI] [PubMed] [Google Scholar]