Abstract
Effective communication by nursing home staff is related to a higher quality of life and a decrease in verbal and physical aggression and depression in nursing home residents. Several communication intervention studies have been conducted to improve communication between nursing home staff and nursing home residents with dementia. These studies have shown that communication skills training can improve nursing aides’ communication with nursing home residents. However, these studies tended to be time-consuming and fairly difficult to implement. Moreover, these studies focused on the communicative benefits for the nursing home residents and their well-being, while benefits and well-being for the nursing aides were neglected. The current study focused on implementing a brief communication skills training program to improve nursing aides’ (N=24) communication with residents with dementia (N=26) in a nursing home. The effects of the training on nursing aides’ communication, caregiver distress, and job satisfaction and residents’ psychopathology and agitation were assessed relative to a control group condition. Nursing aides in the intervention group were individually trained to communicate effectively with residents during morning care by using short instructions, positive speech, and biographical statements. Mixed ANOVAs showed that, after training, nursing aides in the intervention group experienced less caregiver distress. Additionally, the number of short instructions and instances of positive speech increased. Providing nursing aides with helpful feedback during care aids communication and reduces caregiver burden, even with a brief intervention that requires limited time investments for nursing home staff.
Keywords: dementia, psychopathology, agitation, caregiver distress, job satisfaction
Introduction
Nursing home residents spend a lot of time in each other’s company and with nursing home staff, yet social interactions are limited. Interaction between nursing aides and nursing home residents accounts for only 10.7% of the time the aides spend in the nursing home,1 and communication is of a rather neutral and task-oriented style, rather than a positive and personal one.2 This is a missed opportunity, because effective communication is related to a higher quality of life,3 lower depression rates, and lower frequencies of verbal and physical aggression4 in nursing home residents.
What typically happens in nursing homes is that nursing home staff are over-accommodating in their communication style when interacting with nursing home residents, particularly those with dementia, based on stereotypes regarding these residents’ competencies. This is called the Communication Predicament Of Aging.5 Elderspeak, a communication style with high pitch, exaggerated intonation, simplified grammar, and slow speech,6 is a common communication style among nursing home staff. Although well intentioned, elderspeak decreases the chances of effective communication, because residents are not taken seriously as an interaction partner and, consequently, are talked to rather than talked with. Elderspeak reduces self-confidence among nursing home residents and contributes to mental and physical declines in the long run, because there are no frequent or high-quality interactions. These declines then reinforce the negative stereotypes one has regarding nursing home residents.7
It is not surprising, then, that several studies have focused on improving communication in nursing homes to break the circle of patronizing speech or elderspeak. One way to do this is with the Communication Enhancement Model.8 This model illustrates an intervention in which communication partners of the elderly adopt new, facilitating, rather than directing, roles and utilize new communication skills that match the level and individual needs of the older person they are talking to. This approach empowers the person being talked to, optimizes their well-being and level of cognitive functioning, and improves communication skills. Although this is a fairly general model that can be employed in different circumstances and for different populations, it also allows for a more targeted approach to improve communicative interactions in a certain setting.
Several communication intervention studies have been conducted to improve communication between nursing home staff and nursing home residents, including residents with dementia. Two communication intervention studies focused exclusively on improving communication skills and decreasing elderspeak in nursing homes.9,10 The results from both studies9,10 showed that, after training, nursing aides used elderspeak and authoritarian speech to a smaller extent and had a more respectful, caring, and less controlling style of speech toward residents than before they were trained.10
Another communication intervention study used memory books to improve communication in nursing homes for residents with moderate cognitive impairments.11 Personalized memory books contained biographical information and daily schedules that the residents could share with others. In addition, nursing aides were taught to use the memory books when interacting with the residents as part of a communication skills program. It was thought that including memory books in conversations would help to increase communication between residents as well as communication between residents and staff. Moreover, care information contained in the memory books could help to increase residents’ independent functioning during care routines and function as a distraction to decrease disruptive behaviors. The results of the study11 indicated that nursing aides in the intervention group talked more and displayed more positive communication with residents after receiving the training than before, without spending more time on care. A similar intervention, but conducted on a larger scale, demonstrated benefits of communication training with regard to both the quantity and quality of communication.2 There were more verbal interactions between nursing home staff and residents after training, and the communication style became more positive, social, and personal than before.
A communication intervention that purely focused on communication between nursing aides and residents with dementia involved training about effective verbal and nonverbal communication techniques through role play.12 Basic strategies for effective communication were discussed, such as making sure that residents were wearing their glasses or hearing aids when they needed them. Additionally, strategies for communicating effectively with residents with problem behaviors were taught. Results of this Nursing Assistant Communication Skills Program (NACSP) were that residents’ well-being improved after the intervention, and they exhibited depressive symptoms and verbally aggressive behavior to a lesser extent 3 and 6 months later compared to before the staff were trained.
In the FOCUSED communication intervention program, which was specifically targeted at patients with Alzheimer’s disease, nursing aides were educated regarding the difficulties in communication and language that these patients often experience.13 Also, strategies for effective communication in different stages of language deterioration were taught, such as using short sentences and closed-ended questions. Results showed that the training program enhanced nursing aides’ knowledge of Alzheimer’s disease and improved their attitudes toward patients. After training, nursing aides were more satisfied with their communication with the patients. For example, they experienced a greater feeling of control during communication. Nursing aides reported that their newly acquired skills would cause them to try to communicate with residents more.
Overall, the abovementioned intervention studies were all effective in demonstrating improvements in communication between nursing home staff and residents with dementia. These residents all suffer from degenerative memory loss and problems with learning and communication. Frustration with their impairments in these various cognitive domains may therefore lead to agitation and the display of problem behaviors. If staff are trained to understand the causes of these behaviors and receive strategies for adequately responding to these behaviors by using more appropriate communication techniques, then substantial improvement in the quantity and quality of communication between residents and staff is possible, as are subsequent improvements in well-being among nursing home residents.
The present study included the best components of these intervention studies and the Communication Enhancement Model, but in a brief, portable format. A drawback of most previous intervention studies is that they were time-consuming for the researchers and nursing home staff12,13 and rather invasive for nursing home residents, with a number of these studies involving the presence of a research team from early morning until close to bedtime.2,11 Moreover, all studies discussed above focused on the communicative benefits for the residents and their well-being, whereas well-being of the nursing aides was generally not taken into account. Therefore, the current study implemented a brief, small-scale communication skills training program that aimed to improve the quantity and quality of nursing aides’ communication with residents. Secondary benefits were expected to occur with regard to a reduction in caregiver distress, an increase in nursing aides’ job satisfaction, and decreases in depression and problem behaviors among nursing home residents. If successful, this brief intervention could be implemented more easily compared to the interventions previously discussed in a wide variety of settings, as fewer restrictions with regard to the setting and time would be involved and the burden placed on nursing home staff could be kept to a minimum.
Methods
Participants
Participants in this study were the nursing aides and residents of a nursing home for people with dementia in the Netherlands.
Nursing staff
Nursing aides were recruited in staff meetings. Based on this criterion and the research schedule, the final nursing staff sample consisted of 24 nursing aides. Temporary employees were excluded from participation, because staff were required to be available for participation in all research phases. Two nursing aides were excluded during the study due to their unavailability during training and postintervention observations. There were no significant a priori differences between the intervention and control group (P>0.05) on demographic characteristics. In the whole sample, 91.67% were certified nursing assistants, and 8.33% were licensed practical nurses. The mean age was 43.21 years.
Residents
Prior to the study, a letter of consent was sent to residents’ family members or representatives. Fifty-two consented to the resident participating. Twenty-two residents were excluded, one because of a life expectancy of less than 6 months, and 21 for different reasons, for example, not being able to complete the Mini-Mental State Exam (MMSE) due to communication problems or unwillingness to participate. The MMSE was used to assess the severity of cognitive impairment.14,15 This instrument can distinguish people with dementia from other patient groups and control groups. In this study, the MMSE (including the conversation held during the assessment) was also used to determine whether residents were sufficiently communicative for participation in the study. Four residents were excluded because of low MMSE scores. The final sample consisted of 26 residents. All residents had a dementia diagnosis. There were no significant a priori differences between the intervention and control group (P>0.05) demographic characteristics. In the whole sample, the mean age was 84.95 years and the mean MMSE score was 11.17.
Measurement
The measurements used were adaptations from existing communication intervention programs that included observations of communicative interactions between nursing aides and residents.1,2,11
Communication skills checklists
Nursing aides’ communication was assessed with two communication skills checklists. First, the Communication Skills Checklist (CSC)2 was used to measure the quantity of effective and ineffective instructions, positive and negative speech, and biographical statements. Additionally, it was used to assess if activities of care were announced and if the resident was called by name. The interrater reliability in the current study was 75.40%.
The second checklist, the Observation Form of General Communication (OFGC), was designed for this study to be able to measure general characteristics of speech. With this checklist, the frequency of positive, neutral, and negative speech was tallied. These frequencies were then summed to form the total frequency of speech. Speech was labeled positive, neutral, or negative depending on the content (for example, a compliment was labeled as positive, while unhelpful comments were labeled as negative). The interrater reliability was 78.80%.
Questionnaires
The Dutch version of the Cohen-Mansfield Agitation Inventory (CMAI-D) was used to measure the frequency of 29 agitated behaviors displayed by residents during the preceding 2 weeks. The interrater reliability of the CMAI is sufficient.16 The construct validity of the Dutch version is confirmed for nursing home residents with dementia.17
The Dutch version of the Neuropsychiatric Inventory Questionnaire (NPI-Q) was used to measure the severity of different types of psychopathology in residents and to assess the level of caregiver distress experienced by nursing aides because of these symptoms. The interrater reliability and the convergent validity of the NPI-Q are sufficient.18
Nursing aides’ job satisfaction was assessed with the short, Dutch version of the Utrecht Work Engagement Scale (UWES). This instrument measures three dimensions of work engagement: vigor, dedication, and absorption. The internal consistency (Cronbach’s α) is sufficient, and the three-factor structure has been confirmed.19
Design and procedure
Similar to other intervention programs, this study had a two-group comparison design.2,11 One ward served as the intervention group, and the other ward served as the control group. The two wards were completely separate: residents from different wards could not contact each other. The study was conducted in four phases: group assignment, baseline observations, training, and postintervention observations. Both observation phases had the same procedure and were conducted in both groups. The total time period from baseline through the postintervention phase was 8 weeks. With this pretest/posttest design and intervention group/control group comparison, it was possible to demonstrate improvements over time within groups (from baseline to postintervention) and to demonstrate improvements in the intervention group only after training.
Group assignment
Similar to previous intervention studies, the MMSE was administered to the residents in both groups. Wards were randomly assigned to an intervention and control group.2,11
Observation phases
The observations were conducted by two observers. Multiple practice sessions were held to maximize interobserver agreement.20 Use of the checklists was practiced by observing interactions between staff and residents in living rooms in the nursing home and by watching videos of interactions between nursing aides and residents.20 During the last practice session, interrater reliability was calculated.
During both observation phases, communication checklists and questionnaires were administered to the nursing staff. In the mornings, during residents’ activities of daily living, nursing aides’ communication was observed from behind a door or curtain, because, to be able to measure communication, hearing the conversations was sufficient. During these observations, the two communication skills checklists (CSC and OFGC) were used to record nursing aides’ communication. Administration of one checklist took 5 minutes. The CSC was administered at least twice to the same nursing aide and the OFGC was administered at least four times. Each nursing aide was observed interacting with different residents. It was not possible to always assess the same aide/resident dyad during both observation phases, because the usual work routine in the nursing home was followed to reduce the burden placed on the staff by the study. Also, some residents moved away or died during the study.
After each morning of observation, the nursing aides were asked to complete some of the questionnaires (NPI-Q, CMAI, UWES) described above. Nursing aides received instructions on how to fill in these questionnaires. After the final baseline observation, nursing aides were given a form which contained information about the purpose of the training and the communication skills that would be taught. This form was explained by the researchers.
Training
The training program addressed communication skills suitable for different types of dementia. The number of training sessions for each nursing aide was based on the mean scores on the CSC during baseline. For each aide, all effective skills were added up (short instructions, general instructions, biographical statements, positive speech). Subsequently, the ineffective elements (multiple instructions, negative speech) were subtracted. The seven nursing aides with the lowest resulting scores received two training sessions; the others with higher scores received one session. This way, in the brief time available for the study, as many nursing aides as possible received the communication training and the intensity was based on the extent to which they already possessed the relevant skills.
During the training of the intervention group, nursing aides were individually observed during residents’ activities of daily living. The CSC was used to record the use of specific communication skills and types of instructions. During these observations, nursing aides were observed interacting with several residents, to make sure enough feedback could be provided. After these observations, nursing aides received feedback on their communication. First, they were asked how they had experienced the observed interactions. Subsequently, they received feedback on which effective communication skills and instructions (short instructions, general instructions, biographical statements, positive speech) they had used and which they should have used. They were encouraged to keep using the effective communication skills they had used and to start using the skills they had not used. If they had not used an effective skill, the use and purpose of the skill were explained. Finally, if nursing aides used ineffective skills (multiple instructions, negative speech), it was explained to nursing aides why they should not use these skills.
Preparation of analyses
The scores on the different items of each questionnaire (UWES, CMAI-D, NPI-Q symptoms, NPI-Q caregiver distress) were added up to form the total scores. Average scores on each skill on the communication skills checklists were calculated for baseline and postintervention measurements for each nursing aide.
Data were analyzed using 2 (group) × 2 (time) mixed analyses of variance (ANOVAs). These were the same analyses as in other intervention studies.2,11 For significant main or interaction effects, partial eta-squared scores were calculated, for which 0.01 was considered a small effect, 0.06 a medium effect, and 0.14 a large effect.21 Data regarding the quantity of positive and negative speech on the CSC were not analyzed, because these were measured for training purposes only and these variables were also measured with the OFGC.
Results
Nursing staff
Nursing staff’s communication skills when interacting with residents were assessed as well as measures of their distress that could be attributed to their interactions with residents and their job satisfaction.
Communication
Quantity and quality of speech
The mean number of communication skills used is shown in Table 1. This table shows that the style of speech was mostly neutral, rather than positive or negative. Negative speech was very uncommon. The percentages of interactions in which the resident was called by name and activities of care were announced were already very high during baseline (>80%).
Table 1.
Mean number of effective and ineffective communication skills and percentage of effective interactions (Observation Form of General Communication and Communication Skills Checklist) for both groups during both observation phases
| Group | Baseline
|
Postintervention
|
|||
|---|---|---|---|---|---|
| M | SE | M | SE | ||
| Total speech | Training | 32.32 | 1.94 | 35.05 | 2.92 |
| Control | 33.98 | 1.78 | 36.73 | 2.68 | |
| Neutral speech | Training | 28.68 | 1.82 | 29.25 | 2.80 |
| Control | 30.41 | 1.68 | 31.67 | 2.58 | |
| Positive speech | Training | 3.11 | 0.55 | 5.09 | 0.90 |
| Control | 3.30 | 0.51 | 4.35 | 0.83 | |
| Negative speech | Training | 0.52 | 0.18 | 0.70 | 0.29 |
| Control | 0.27 | 0.16 | 0.69 | 0.26 | |
| Biographical statements | Training | 1.59 | 0.51 | 1.64 | 0.77 |
| Control | 1.19 | 0.47 | 2.27 | 0.71 | |
| Call by name (%) | Training | 90.91 | 9.32 | 95.45 | 5.18 |
| Control | 84.62 | 8.57 | 92.31 | 4.77 | |
| Announce activity (%) | Training | 83.33 | 7.45 | 100.00 | 3.58 |
| Control | 100.00 | 6.20 | 96.15 | 2.98 | |
Abbreviations: M, mean; SE, standard error.
There were no significant interactions between time and group or main effects of group (P>0.05) for the different types of communication skills. The main effect of time was significant for the number of positive statements on the OFGC, after applying a Bonferroni correction (F[1,22]=9.10, P<0.05). This is a large effect.21 Table 1 shows that, in both groups, positive speech increased with time.
Additionally, there was a trend that the percentage of interactions in which activities of care were announced increased in the intervention group and decreased in the control group (F(1,20)=3.64, P<0.10). However, in the control group, the maximum score had already been reached at baseline, which means that the score could only decrease or remain the same.
Quantity and quality of instructions
Table 2 shows the mean number of short, general, and multiple instructions. Short instructions were used much more frequently than multiple instructions. There were no significant interactions between time and group for the different types of instructions (P>0.05). The main effect of time was significant for the number of short instructions (F(1,22)=5.10, P<0.05). This is a large effect.21 Table 2 shows that the number of short instructions increased with time in both groups. The main effect of group was significant for the number of multiple instructions (F(1,22)=9.12, P<0.01). This is a large effect.21 Table 2 shows that the number of multistep instructions was lower in the intervention group than in the control group. However, this difference was significant only in the postintervention phase (Levene’s t[15]=3.74, P=0.002).
Table 2.
Mean number of effective and ineffective instructions (Communication Skills Checklist) for both groups during both observation phases
| Group | Baseline
|
Postintervention
|
|||
|---|---|---|---|---|---|
| M | SE | M | SE | ||
| Short instructions | Training | 6.73 | 1.15 | 9.07 | 1.14 |
| Control | 6.92 | 1.06 | 8.62 | 1.05 | |
| General instructions | Training | 2.23 | 0.34 | 2.23 | 0.39 |
| Control | 2.65 | 0.31 | 2.08 | 0.36 | |
| Multiple instructions | Training | 0.59 | 0.18 | 0.11 | 0.15 |
| Control | 0.81 | 0.16 | 0.81 | 0.13 | |
Abbreviations: M, mean; SE, standard error.
Caregiver distress
Figure 1 shows the mean caregiver distress scores for both groups during both observation phases. The time × group interaction was significant (F(1,24)=5.20, P<0.05) on the caregiver distress scores. This is a large effect.21 Figure 1 shows that caregiver distress decreased from baseline to postintervention observations in the intervention group, whereas the opposite pattern occurred in the control group. This confirms the hypothesis that communication skills training can decrease nursing aides’ caregiver distress. There were no significant main effects of time and group (P>0.05) for the caregiver distress scores. Note that caregiver distress scores were low overall, all mean scores were below 10, while the maximum score is 60 on the NPI-Q.
Figure 1.
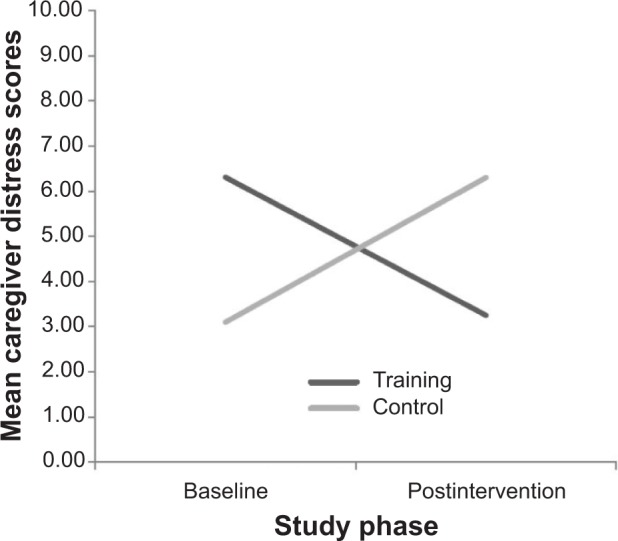
Mean caregiver distress scores for both groups during both observation phases.
Job satisfaction
The mean job satisfaction scores were 46.55 during baseline and 45.27 during postintervention observations for the intervention group. For the control group, these scores were 48.31 and 45.77, respectively. Because the maximum score on the UWES is 54, these scores are considered high. There were no significant interactions between time and group or main effects of time and group for the job satisfaction scores (P>0.05). Scores were comparable across groups, with a downward trend in the control group.
Residents
Residents were evaluated by their nursing aides with regard to their level of agitation and psychopathology.
Agitation
The CMAI-D covers problem behaviors that can be expressed in the form of verbal or physical aggression, as well as inappropriate behaviors (eg, disrobing) and restlessness. The agitation scores on the CMAI-D ranged from 29 to 203. For the intervention group, the mean agitation scores were 44.75 during baseline and 44.37 during postintervention observations. For the control group, these scores were 51.00 and 48.20, respectively. Compared to the norms,17 these scores are considered to be somewhat above average. There were no significant interactions between time and group or main effects of time and group for the agitation scores (P>0.05). The scores across the groups were comparable but, within the groups, there was quite a bit of variation.
Psychopathology
Table 3 shows residents’ mean psychopathology scores regarding the total severity of psychopathology and the severity of specific symptoms, such as depression and anxiety. Most symptoms were uncommon, given the fact that the scores were below 1.00 (maximum is 3). An exception was the severity of irritability in the control group, which was 1.30 before and 1.70 after the intervention.
Table 3.
Mean severity of residents’ psychopathology (Neuropsychiatric Inventory Questionnaire) for both groups during both observation phases
| Group | Baseline
|
Postintervention
|
|||
|---|---|---|---|---|---|
| M | SE | M | SE | ||
| Total | Training | 7.56 | 1.59 | 5.44 | 1.44 |
| Control | 5.70 | 2.01 | 8.10 | 1.82 | |
| Depression | Training | 0.50 | 0.21 | 0.50 | 0.23 |
| Control | 0.60 | 0.26 | 0.60 | 0.29 | |
| Anxiety | Training | 0.56 | 0.19 | 0.63 | 0.23 |
| Control | 0.40 | 0.24 | 0.70 | 0.29 | |
| Apathy | Training | 0.81 | 0.25 | 0.50 | 0.23 |
| Control | 0.20 | 0.32 | 0.70 | 0.29 | |
| Disinhibition | Training | 0.63 | 0.26 | 0.81 | 0.24 |
| Control | 1.00 | 0.33 | 0.60 | 0.31 | |
| Irritability | Training | 0.75 | 0.28 | 0.56 | 0.28 |
| Control | 1.30 | 0.35 | 1.70 | 0.35 | |
Abbreviations: M, mean; SE, standard error.
After applying the Bonferroni correction, there were no significant interactions between time and group or main effects of time and group (P>0.05) regarding the total severity of psychopathology and that of specific symptoms. However, there was a trend for a decrease of the severity of psychopathology in the intervention group against an increase in the control group (F(1,24)=2.88, P=0.10).
A correlational analysis between the severity of irritability and the caregiver distress scores showed positive correlations between these two variables during baseline (r=0.44, P<0.05) and postintervention observations (r=0.53, P<0.01).
Discussion
This study implemented effective components from previously tested communication intervention studies1,2,8,11,12 in a brief, small-scale, portable intervention in one nursing home with participating nursing aides and residents with dementia. Our short intervention also focused on nursing aides’ well-being and burden, and was expected to improve nursing aides’ communication skills, decrease their levels of caregiver distress, and increase their job satisfaction, as well as decrease residents’ psychopathology.
The training focused on using short instructions, positive speech, and biographical statements, as these are relatively easy to teach to nursing home staff in a relatively short period of time. The results confirmed the hypothesis that, from baseline to postintervention observations, the intervention decreased the level of caregiver distress experienced by nursing aides in the intervention group only. Although predicted, this outcome is still surprising, given the low level of caregiver distress to begin with. This effect coincided with a trend of a decrease in the severity of psychopathology in the intervention group and high correlations between the severity of residents’ irritability and nursing aides’ caregiver distress.
The outcomes of the observed interactions between nursing home staff and residents reflect a dynamic interplay of how staff experience the stress of caregiving in concordance with negative behaviors by the residents. Decreases in caregiver distress in the intervention group could be an indication that the training provided a strategy for coping better during these interactions. Moreover, trained nursing aides may have felt more support as a result of the regular and positive feedback from the researchers during training. This feedback may have made them more aware of the good communication skills they already had and developed over the course of the training. Feelings of confidence and awareness of good caregiving skills might have given them the strength to calmly handle residents’ psychopathology and problem behaviors. This process could reflect another loop in the Communication Enhancement Model,8 in which nursing aides feel empowered when given appropriate feedback on their communication skills. The fact that nursing aides in the control group did not receive any feedback, yet invested time and effort in the study as well, may have contributed to their distress. Future research could demonstrate whether or not this does, in fact, happen. If so, control group participants should be given the opportunity for training after the intervention group has finished. Other intervention programs have not reported on these measures, which is why further research into this issue is necessary.
With regard to the communicative interactions, the number of short instructions and instances of positive speech increased from baseline to postintervention in both groups. This is in accordance with the Communication Enhancement Model and the results of intervention studies that demonstrated the largest improvements in communication during one-on-one care interactions of staff with residents.2,11 In the present study, nursing aides fulfilled a more facilitative role when communicating with residents, taking into account the need for positive speech. The effects seemed to spill over to some extent to nursing aides in the control group, who may have heard about the trained skills during lunch breaks. Alternatively, the reappearance of the researchers after the training when they worked with nursing aides in the intervention group only may have had a positive effect on the quality of interactions between nursing aides and residents.
The contribution of this intervention study to the field is that, despite the relatively limited number of training sessions and the presence of good communication skills at baseline, the training still yielded positive results. First, the level of caregiver distress nursing aides experienced decreased only in the intervention group. It may therefore be useful in any kind of nursing home to regularly provide feedback on the observed skills. This contributes to nursing aides’ well-being and raises their confidence regarding their communication skills. This feedback should help them to be able to handle residents’ problem behaviors better, which may help decrease residents’ psychopathology. Although these reasons for the decreased caregiver distress seem plausible, future research should further examine those components of the training that contribute the most to a decrease in caregiver distress.
Second, the communication training resulted in an increase in the quantity and quality of communication, despite possible carryover effects to the control group. Regularly giving nursing aides feedback regarding their care interactions with the residents is a good strategy that may not only improve their communication skills, but also decrease caregiver distress. This process contributes to positive interactions between nursing aides and residents, which, in turn, might lower residents’ problem behaviors.
There were no direct effects of the intervention on the problem behaviors or psychopathology of the residents. Previously, one communication intervention study demonstrated reductions in proxy depression scores in the intervention group after implementation of a communicative intervention.22 Moreover, residents’ problem behaviors were associated with the aides’ proxy depression scores, with lower proxy depression scores after nursing aides were trained in the intervention group. The extent to which problem behaviors occur among nursing home residents and are evaluated by nursing home staff as such is strongly associated with the distress that their caregivers experience on the job. Training may not only reduce the level of distress, but may improve well-being among residents, at least as to how it is evaluated by nursing aides.
In future research, these complex relationships should be better disentangled in order to assess specific rather than combined benefits of communicative strategies on how residents feel and act. If, indeed, effective and positive communication results in improved well-being among both residents and nursing aides, then future training programs should focus on regular monitoring during care interactions followed by feedback to the nursing aides. Possibly, certain problem behaviors may decrease more than others, which would provide insight into specific triggers of these problem behaviors and how they can be reduced.
Conclusion
This small-scale intervention study showed good results with regard to improvements in the quantity and quality of communication over time, as well with regard to reductions in caregiver distress among trained nursing aides. This could be a promising model for future studies that aim to improve communication and well-being in nursing home staff and residents without substantial time investment and in a beneficial manner for everyone involved.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Burgio LD, Engel BT, Hawkins AM, McCormick K, Scheve A. A descriptive analysis of nursing staff behaviors in a teaching nursing home: differences among NAs, LPNs, and RNs. Gerontologist. 1990;30(1):107–112. doi: 10.1093/geront/30.1.107. [DOI] [PubMed] [Google Scholar]
- 2.Bourgeois MS, Dijkstra K, Burgio LD, Allen RS. Communication skills training for nursing aides of residents with dementia: the impact of measuring performance. Clin Gerontol. 2004;27:119–138. [Google Scholar]
- 3.Zimmerman S, Sloane PD, Williams CS, et al. Dementia care and quality of life in assisted living and nursing homes. Gerontologist. 2005;45(Spec No 1):133–146. doi: 10.1093/geront/45.suppl_1.133. [DOI] [PubMed] [Google Scholar]
- 4.Toseland RW, Diehl M, Freeman K, Manzanares T, Naleppa M, McCallion P. The impact of validation group therapy on nursing home residents with dementia. J Appl Gerontol. 1997;16(1):31–50. [Google Scholar]
- 5.Ryan EB, Hummert ML, Boich LM. Communication predicaments of aging: patronizing behavior toward older adults. J Lang Soc Psychol. 1995;14(1–2):144–166. [Google Scholar]
- 6.Kemper S, Finter-Urczyk A, Ferrell P, Harden T, Billington C. Using elderspeak with older adults. Discourse Process. 1998;25(1):55–73. [Google Scholar]
- 7.Ryan EB, Giles H, Bartolucci G, Henwood K. Psycholinguistic and social psychological components of communication by and with the elderly. Language and Communication. 1986;6:1–24. [Google Scholar]
- 8.Ryan EB, Meredith SD, MacLean MJ, Orange JB. Changing the way we talk with elders: promoting health using the communication enhancement model. Int J Aging Hum Dev. 1995;41(2):89–107. doi: 10.2190/FP05-FM8V-0Y9F-53FX. [DOI] [PubMed] [Google Scholar]
- 9.Williams K, Kemper S, Hummert ML. Improving nursing home communication: an intervention to reduce elderspeak. Gerontologist. 2003;43(2):242–247. doi: 10.1093/geront/43.2.242. [DOI] [PubMed] [Google Scholar]
- 10.Williams KN. Improving outcomes of nursing home interactions. Res Nurs Health. 2006;29(2):121–133. doi: 10.1002/nur.20117. [DOI] [PubMed] [Google Scholar]
- 11.Burgio LD, Allen-Burge R, Roth DL, et al. Come talk with me: improving communication between nursing assistants and nursing home residents during care routines. Gerontologist. 2001;41(4):449–460. doi: 10.1093/geront/41.4.449. [DOI] [PubMed] [Google Scholar]
- 12.McCallion P, Toseland RW, Lacey D, Banks S. Educating nursing assistants to communicate more effectively with nursing home residents with dementia. Gerontologist. 1999;39(5):546–558. doi: 10.1093/geront/39.5.546. [DOI] [PubMed] [Google Scholar]
- 13.Ripich DN, Wykle M, Niles S. Alzheimer's disease caregivers: the focused program. A communication skills training program helps nursing assistants to give better care to patients with Alzheimer's disease. Geriatr Nurs. 1995;16(1):15–19. doi: 10.1016/s0197-4572(05)80073-4. [DOI] [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 15.Cockrell JR, Folstein M. Mini-Mental State Examination. In: Copeland JRM, Abou-Saleh MT, Blazer DG, editors. Principles and Practice of Geriatric Psychiatry. 2nd ed. Chichester: John Wiley & Sons; 2002. pp. 140–141. [Google Scholar]
- 16.Cohen-Mansfield J. Instruction Manual for the Cohen-Mansfield Agitation Inventory (CMAI) Rockville, MD: The Research Institute of the Hebrew Home of Greater Washington; 1991. [Google Scholar]
- 17.Zuidema SU, de Jonghe JF, Verhey FR, Koopmans RT. Agitation in Dutch institutionalized patients with dementia: factor analysis of the Dutch version of the Cohen-Mansfield Agitation Inventory. Dement Geriatr Cogn Disord. 2007;23:35–41. doi: 10.1159/000096681. [DOI] [PubMed] [Google Scholar]
- 18.Kaufer DI, Cummings JL, Ketchel P, et al. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci. 2000;12:233–239. doi: 10.1176/jnp.12.2.233. [DOI] [PubMed] [Google Scholar]
- 19.Schaufeli WB, Bakker AB. Bevlogenheid: een begrip gemeten [Work engagement: the measurement of a concept] Gedrag and Organisatie. 2004;17(2):89–112. Dutch. [Google Scholar]
- 20.Hazelhof T, Garenfeld W, Verdonschot T. Dementie en Psychiatrie. Amsterdam: Reed Business; 2011. Dutch. [Google Scholar]
- 21.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 22.Bourgeois MS, Dijkstra K, Hickey EM. Impact of communication interaction on measuring self- and proxy-rated depression in dementia. J Med Speech Lang Pathol. 2005;13(1):37–50. [Google Scholar]


