Dear Editor,
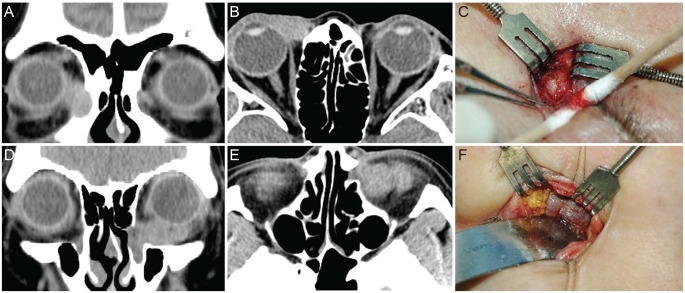
Recently, we experienced two cases of lacrimal sac tumors discovered in patients who presented with persistent epiphora after receiving dacryocystorhynostomy (DCR). A 75-year-old female visited the clinic complaining persistent epiphora in the right eye for 5 years. The patient was diagnosed with nasolacrimal duct obstruction in the right eye and received a DCR twice 2 years ago at a local hospital, but epiphora persisted post operation. Lacrimal irrigation test revealed a reflux through contralateral puncta in the right eye. There was a protrusion superior to medial canthus and a mass was palpable at the medial side of the right orbit. Computed tomography (CT) scan confirmed a 3-cm-sized mass involving the right lacrimal sac and surrounding soft tissue of inferomedial orbit (Fig. 1A and 1B). An excisional biopsy was performed and diagnosed as invasive squamous cell carcinoma from lacrimal sac. Wide resection of lacrimal sac and nasolacrimal duct via anterior orbitotomy and medial maxillectomy via lateral rhinotomy was performed (Fig. 1C). The patient received adjuvant radiotherapy and is under observation.
Fig. 1.
Computed tomography (CT) scan and operation images of epiphora patients diagnosed with tumor in lacrimal duct (A,B). Preoperative orbital CT images of the 75-year-old female patient show a 3-cm mass at the right lacrimal sac. (C) An excisional biopsy was performed and a mass invading the lacrimal sac and the inferomedial orbit was found (D) and (E). Preoperative orbital CT images of the 51-year-old female patient show a mass invading the left lacrimal sac and the inferomedial orbit. (F) An excisional biopsy was performed and a mass invading the left lacrimal sac was observed.
The second case presents a 51-year-old female whose history included a DCR received at a local hospital for epiphora in the left eye. She was complaining of persistent epiphora and swelling of upper and lower eyelids. The slit lamp examination and lacrimal irrigation test was normal. Sinus endoscopy showed intact bony opening from the previous DCR. A CT scan was done and a mass occluding the lacrimal sac and invading the inferomedial orbit was observed (Fig. 1D and 1E). An excisional biopsy was performed and the pathology report diagnosed a papilloma with mild nuclear dysplasia, which has a risk of advancing into a squamous carcinoma. Wide resection of inferomedial orbit including lacrimal sac and endoscopic medial maxillectomy was performed (Fig. 1F). Pathology report diagnosed a carcinoma arose from papilloma, and the patient received adjuvant radiotherapy.
This is the first case series of lacrimal sac tumors discovered in patients with persistent epiphora after receiving DCR in Korea. A tumor originating from the lacrimal sac is a rare cause of epiphora [1], but a half of the cases turn out to show malignancy with a high mortality rate, which raises a need for precaution.
Tumors of lacrimal sac can be categorized into three types. The first type is a primary tumor in the lacrimal sac, in which 72% of the cases are malignant. The second type is a tumor invading from the nearby tissue such as eyelids, paranasal sinuses or orbits. The third type is an inflammatory tumor such as sarcoidosis or Wegener's granulomatosis, which may require an internal medical approach to evaluate systemic symptoms.
Epithelial tumor is the most common type of primary tumor in the lacrimal sac. Benign epithelial tumors include papilloma and oncocytoma, and can be treated with surgical resection [2,3]. Malignant epithelial tumors include squamous cell carcinoma and transitional cell carcinoma, and a wide resection including lacrimal canaliculi, sac and nasolacrimal duct with lateral rhinotomy is needed with preoperative and/or postoperative radiotherapy. If the tumor is invasive, an orbital exenteration including wide resection, lymphadenectomy and paranasal sinus resection is required. The local recurrence rate is 50% and the mortality rate is 50% for invasive squamous cell carcinoma and 100% for transitional cell carcinoma. Non-epithelial tumor includes mesenchymal tumor and lymphoproliferative tumor [2,3].
Because recent DCRs are performed using sinus endoscopes to avoid scar formation, it is more difficult to find tumors than in conventional DCRs. The possibility of a tumor in the lacrimal sac must be ruled out in the patients with a palpable mass superior to the medial canthus, a bloody reflux and/or a simultaneous exophthalmos [3,4]. Palpation around the medial canthal area and pathologic confirmation of tissue whenever discovering any sign of abnormality is important, especially when eyelid swelling or epiphora persist after DCR. Imaging study of the lacrimal drainage system using CT scan is also a good screening process.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Merkonidis C, Brewis C, Yung M, Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol. 2005;89:1589–1591. doi: 10.1136/bjo.2005.072199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valenzuela AA, McNab AA, Selva D, et al. Clinical features and management of tumors affecting the lacrimal drainage apparatus. Ophthal Plast Reconstr Surg. 2006;22:96–101. doi: 10.1097/01.iop.0000198457.71173.7b. [DOI] [PubMed] [Google Scholar]
- 3.Heindl LM, Junemann AG, Kruse FE, Holbach LM. Tumors of the lacrimal drainage system. Orbit. 2010;29:298–306. doi: 10.3109/01676830.2010.492887. [DOI] [PubMed] [Google Scholar]
- 4.Golan S, Leibovitch I, Landsberg R. Unexpected pathologies in patients referred for endoscopic DCR. Eur Arch Otorhinolaryngol. 2014;271:3053–3058. doi: 10.1007/s00405-014-2892-y. [DOI] [PubMed] [Google Scholar]