Abstract
BACKGROUND: The incidence of diabetes in the general population is increasing world-wide. The increase is attributed to the consumption of saturated fatty acids, obesity, lack of physical activity, genetic predisposition, and other factors, but knowledge about the reasons, biological mechanisms, and late complications is insufficient. It is therefore important to clarify the reasons more exactly through long-term clinical trials to stop the rise of diabetes and its complications. AIM: To evaluate the 10-year incidence of type 2 diabetes in apparently healthy Greek adults. METHODS: In 2001-2002, a random sample of 1514 men (18-87 years old) and 1528 women (18-89 years old) was selected to participate in the ATTICA study. During 2011-2012, the 10-year follow-up was performed. Patients diagnosed with diabetes at baseline (n = 210) and those lost at the 10-year follow-up (n = 1347) were excluded, yielding a final sample of 1485 participants. RESULTS: During the period of investigation, diabetes was diagnosed in 191 cases corresponding to a 12.9% incidence (95%CI: 10.4-15.4), with 13.4% (95%CI: 10.8-16) in men and 12.4% (95%CI: 10.1-14.7) in women. A relative increase was observed in the second half of the 10-year follow-up when age became significant. Multiple logistic regression analysis revealed that age (OR = 1.14, 95%CI: 1.09-1.19), abnormal waist-to-height ratio (OR = 3.27, 95%CI: 1.07-10.0), fasting blood glucose (OR per 1 mg/dl = 0.05, 95%CI: 1.02-1.08), energy intake (OR per 500 kcal = 1.02, 95%CI: 1.01-1.35), and family history of diabetes (OR = 2.8, 95%CI: 1.30-6.03) were the most significant baseline predictors for diabetes, after adjusting for potential confounders. Waist-to-height ratio showed the best explanatory power of all anthropometric variables. Physical activity exerts an effect on risk factors. Being active was found to eliminate the aggravating effect of diabetes family history and fasting blood glucose. CONCLUSIONS: The findings confirm the escalating increase of type 2 diabetes incidence in Greece, which is in line with global trends. A lifestyle change in individuals at risk of developing diabetes towards healthier eating and increased physical activity would be an effective and inexpensive means of reducing diabetes.
Keywords: type 2 diabetes, incidence, risk factor, epidemiology, physical activity, lifestyle, visceral obesity
Abbreviations: ADA – American Diabetes Association; CI – confidence interval; CVD – cardiovascular disease; BMI – body mass index; EASD – European Association for the Study of Diabetes; ESC – European Society of Cardiology; NCEP-ATP III – National Cholesterol Education Program Adult Treatment Panel III; IPAQ – International Physical Activity Questionnaire; OR – odds ratio; P-P plot – probability-probability plot; RIA – radioimmunoassay; SPSS – statistical package for social sciences; WH – waist-to-hip; WHO – World Health Organization; WHt – waist-to-height
1. Introduction
Despite ongoing advances in treatment and management of diabetes and its complications, the disease is developing into a constantly advancing epidemic. Since 1980, the number of patients with diabetes worldwide has more than doubled, particularly in America, Africa, and Western Europe [1], and is expected to almost quadruple within the next 20 years, i.e., before 2030, amounting to 552 million cases [2]. This prospect is alarming, given that diabetes is a well-established risk factor for the development of micro- and macrovascular complications; it increases the risk of coronary artery disease, neuropathy, nephropathy, eye disease, and others [3].
The exponential growth of diabetes is accompanied by a serious financial burden. The joint statement of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD) has underlined that the healthcare expenditure for diabetes in Europe is expected to increase from 75 billion euro in 2011 to 90 billion in 2030 [4], or 123 euro/person, based on the population of Europe in 2011 [5]. Since no curative treatment exists, primary prevention should be the cornerstone of the global response to the disease. Lifestyle interventions, including nutrition therapy, regular exercise, and cessation of smoking and alcohol, have been found to exert a significantly beneficial effect on diabetes onset [6-8]. Multifactorial treatment combining lifestyle with medication has been proven beneficial [9].
Since diabetes has a "metabolic memory", which can extend the beneficial effect of therapy over many years, early prevention and effective intervention are of utmost importance [10]. As a result, quantifying the extent of type 2 diabetes is fundamental for managing patients in health service delivery systems. Unfortunately, long-term investigations of diabetes incidence are rare in the literature, especially in Mediterranean populations. Greece experienced the lowest rates of cardiovascular disease (CVD) and diabetes in the 1960s and 1970s. Researchers from the Salamis Study found that the self-reported prevalence of diabetes was 8.7% in 2002 [11] and 10.3% in 2006 [12].
The most recent study to provide incidence data about diabetes was the ATTICA study [13]. Specifically, the prevalence of type 2 diabetes in 2001-2012 was calculated as 7.6% in men and 5.9% in women [14], while the age-adjusted 5-year incidence (2006) of diabetes was found to be 5.5% (men: 5.8%; women: 5.2%) [15]. These results are in line with the alarming incidence rates of diabetes worldwide. However, many findings are limited in statistical power because of the small number of incident cases studied, or the lack of representative samples; therefore accurate estimates of the determinants of diabetes could not be made. In the present work, the 10-year diabetes incidence (2002-2012) and the impact of several clinical, biological, and lifestyle factors relevant for diabetes development were examined within the context of the ATTICA study.
2. Methods
2.1 Baseline sampling (2001-2002)
The ATTICA epidemiological study [13] is a large prospective study carried out during 2001-2002 in the Athens metropolitan area including 78% urban and 22% rural subjects. Baseline random sampling suggested that it would be enough to enroll only one participant per household. The sampling process was multistage, based on age (5 strata), sex (2 strata), and distribution of the catchment area (i.e., 27 strata, census of 2001) in order to be as representative as possible.
People with cardiovascular disease or chronic viral infections or those living in institutions were not eligible. Exclusion of CVD at baseline was ensured with a detailed clinical evaluation, following standard criteria. From the 4056 inhabitants, randomly invited to participate, 3042 were finally enrolled in the study (75% participation rate); 1514 were men (46 ± 13 years) and 1528 were women (45 ± 13 years). All participants were interviewed by trained personnel (i.e., cardiologists, general practitioners, dietitians, and nurses) who used a standard questionnaire. Further details about the aims, design, and methods applied in the ATTICA study can be found elsewhere in the literature [13].
2.2 Baseline measurements
The baseline evaluation included the following information:
- Socio-demographic characteristics (age, sex, and years of school).
- Personal history of hypertension, hypercholesterolemia and diabetes.
- Family history of CVD, dietary, and other lifestyle habits (i.e., smoking and physical activity status).
Smokers were defined as persons who smoked at least one cigarette per day or had quitted within the previous year; the rest were defined as non-smokers. The International Physical Activity Questionnaire (IPAQ [16]) was used as an index of the weekly energy expenditure status which included frequency (times per week), duration (in minutes per time), and intensity of sports or other habits related to physical activity (in expended calories per time). Participants were classified into two groups:
1. Sedentary lifestyle.
2. At least moderately active during a substantial part of the day.
Body mass index (BMI) was calculated as weight (in kg) divided by standing height (in square meters). Dietary information was extracted from a validated semi-quantitative food-frequency questionnaire [17]. The participants were asked to report their average intake of several foods and liquids consumed during the previous 12 months. Energy intake, in kcal/day, was calculated based on the participants' responses in this questionnaire.
Blood samples were collected from the antecubital vein between 8 and 10 am, in a sitting position after 12 hours of fasting and alcohol abstinence. Diagnosis of type 2 diabetes was based on the criteria of the American Diabetes Association (ADA) [18], i.e., participants who had fasting blood glucose >125 mg/dl during the examination or who reported the use of antidiabetic medication were defined as having diabetes. Blood glucose levels (mg/dl) were measured with a Beckman Glucose Analyzer (Beckman Instruments, Fullerton, CA, USA). Serum insulin concentrations were assayed by radioimmunoassay (RIA100, Pharmacia Co., Erlangen, Germany).
Obesity was defined as BMI > 29.9 kg/m2, according to WHO criteria [19]. Waist and hip circumferences were measured (in cm), and waist-to-hip (WH) and waist-to-height (WHt) ratios were calculated. Abnormal WH ratio was considered to be >0.8 for women and >1 for men; abnormal WHt ratio was >0.5 for both sexes. Regarding other clinical characteristics, arterial blood pressure (3 recordings) was measured at the end of the physical examination, with the subjects in the sitting position after having rested for at least 30 minutes. Participants whose average blood pressure levels were ≥140/90 mmHg or those who were under antihypertensive medication were classified as being hypertensive. Hypercholesterolemia was defined as total cholesterol >200 mg/dl or by the use of lipid-lowering agents. The intra- and inter-assay coefficients of variation for cholesterol levels did not exceed 9%. The metabolic syndrome was defined according to NCEP-ATP III criteria [20].
2.3 Follow-up evaluation (2011-2012)
During 2011-2012, a 10-year follow-up was performed. Of the 3042 participants, 2583 completed the follow-up (85% participation rate). Participants were initially reached through telephone calls. Afterwards, face-to-face interviews were performed. In 35% of the participants, data were retrieved only through telephone calls. The study investigators performed a detailed evaluation of the participants' medical status using standardized procedures.
Among other endpoints, the re-examination included information about the development and management of diabetes during the 10-year period. Diagnosis of diabetes was based on ADA criteria, as performed in the baseline examination. Participants who did not provide biological samples―those who were reached only by telephone―were asked whether they had been diagnosed by a physician. Patients diagnosed with diabetes at baseline (n = 210) and those with no data of diabetes status at the 10-year follow-up (n = 1347 cases) were excluded from the analysis. Thus, the working sample consisted of 1485 participants who were free of diabetes at baseline and who developed diabetes during the 10-year follow-up period. This sample was sufficient to achieve 92% statistical power and to evaluate a relative risk of 0.70 between the null hypothesis and the alternative two-sided hypothesis with a significance level (alpha) of 0.05, when the exposure variable was increased by 1 unit.
2.4 Statistical analysis
The incidence of diabetes (and corresponding 95% CI) was calculated as the ratio of new cases among the 1485 participants, who were free of diabetes at baseline, and who participated in the follow-up. Continuous variables are presented as mean values ± standard deviation and categorical variables as frequencies. Associations between categorical variables were tested using the chi-square test. Comparisons of mean values of normally distributed variables between those who developed diabetes and the rest of the participants were performed using Student’s t-test, after controlling for equality of variances using Levene's test. For continuous variables which were not normally distributed (i.e., years of school), the Mann-Whitney non-parametric test was applied to evaluate the differences in the distributions of the skewed variables.
Continuous variables were tested for normality through P-P plots. Since the exact time to event (i.e., development of diabetes) was not known, the relative risk of developing the disease during the 10-year follow-up period was estimated using odds ratio (OR) and the corresponding 95% confidence interval (CI) by stepwise multiple logistic regression analysis. Interactions between gender and other covariates were tested in all steps, and when significant, they remained in the final model. The Hosmer-Lemeshow test was applied to evaluate the model's goodness-of-fit. The -2 log-likelihood ratio of the initial vs. final model was also calculated to evaluate the model's performance (the lower the better).
All known confounders were included in the models, after testing for colinearity. The SPSS version 18 (Statistical Package for Social Sciences, SPSS Inc, Chicago, IL, U.S.A.) software was used for all statistical calculations.
3. Results
3.1 Diabetes incidence
During the period of investigation, diabetes was diagnosed in 191 cases corresponding to a 12.9% incidence (95% CI: 10.4-15.4), or 129 per 1000 free of diabetes participants at baseline, with 13.4% (95% CI: 10.8-16) in men and 12.4% (95% CI: 10.1-14.7) in women. It could be speculated (assuming a constant annual increment) that the annual incidence was 1.29% overall, or 1.34% and 1.24% for men and women, respectively. Stratified by age group, the analysis revealed that the incidence of diabetes was the lowest (1.5%) in people under 35 years of age, but has risen to 29.2% for participants over 74 years of age. The men-to-women incidence was approximately 1-to-1 in almost all age groups. However, women under 35 years and between 65-74 years were 3.18-times and 1.55-times more likely to develop diabetes compared to men of the same age group. Conversely, among participants >74 years old, men were 1.33-times more likely to develop the disease than women (Table 1).
Table 1. Ten-year diabetes incidence in ATTICA study participants by gender and age group.
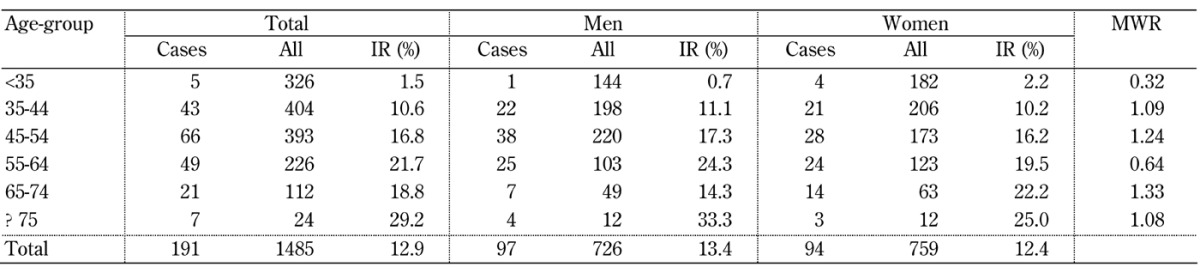
Legend: Diabetes incience among participants <35 and ≥75 years old was low, so the calculated incidence in these groups should be carefully interpreted. Abbreviations: IR – incidence rate, MWR – men-to-women rate.
Diabetes incidence during the second mid-term of the 10-year follow-up of the ATTICA study (i.e., 2007-2012) showed a relative increase. After excluding 100 diabetes cases before 2007, the remaining 91 new cases were used to calculate the preceding 5-year incidence over the 1385 participants. A relative increase between the two periods was observed overall, i.e., from 5.5% (2002-2007) to 6.6% (2007-2012), and by gender, i.e., from 5.8% to 6.8% for men and from 5.3% to 6.3% for women (Table 2). However, when age was included in the analysis, the difference in incidence rates between the two time periods was not significant for both sexes (p > 0.05).
Table 2. Progression of diabetes incidence during the preceding 10-year period of the ATTICA study (baseline, 2007, and 2012 follow-up).
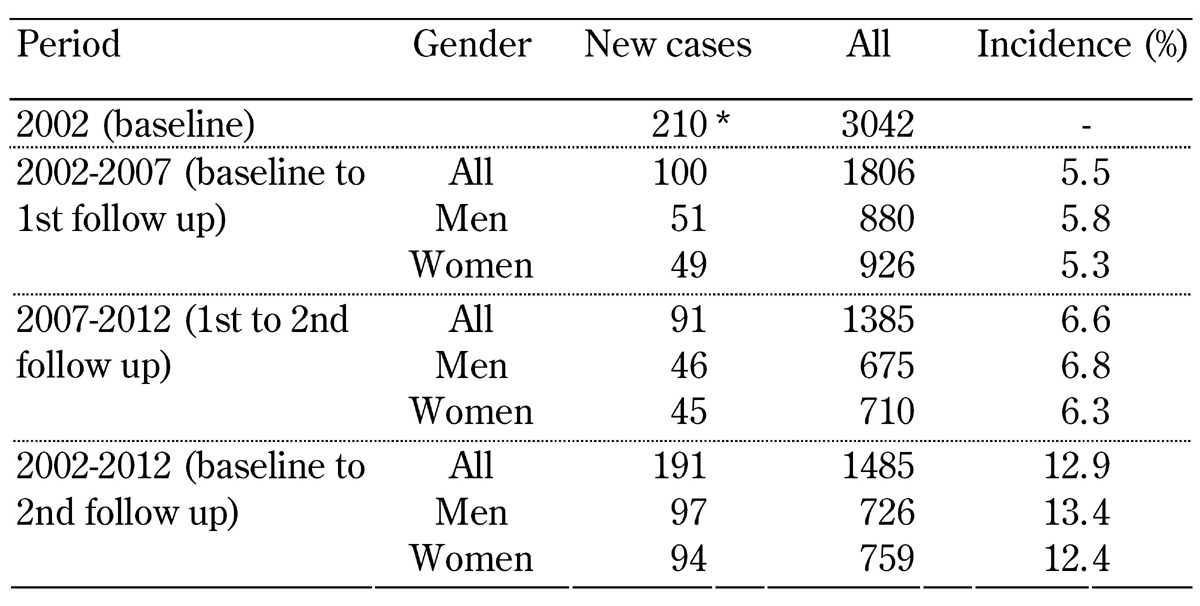
Legend: * n = 210 people with diabetes at baseline were excluded from the analysis.
The distribution of the baseline demographic, lifestyle, and clinical parameters of ATTICA study participants, based on their diabetes status at the 10-year follow-up, is presented in Table 3. Non-adjusted analysis revealed that individuals who developed diabetes were approximately 10 years older, had higher fasting glucose (but lower fasting insulin levels), and were more likely to be hypertensive, hypercholesterolemic, and predisposed to diabetes. With regards to anthropometric characteristics, patients with diabetes had higher BMI and waist circumference, and were more likely to have abnormal waist circumference, using 102/88 cm and 94/80 cm as cut-off values for men and women, respectively. Those who developed diabetes also had abnormal WH and WHt ratios. As expected, metabolic syndrome occurred more often in this group. However, smoking status, years of education, energy intake, and physical activity did not differ significantly between the two groups.
Table 3. Baseline characteristics of the ATTICA study participants according to 10-year diabetes incidence (n = 1485).
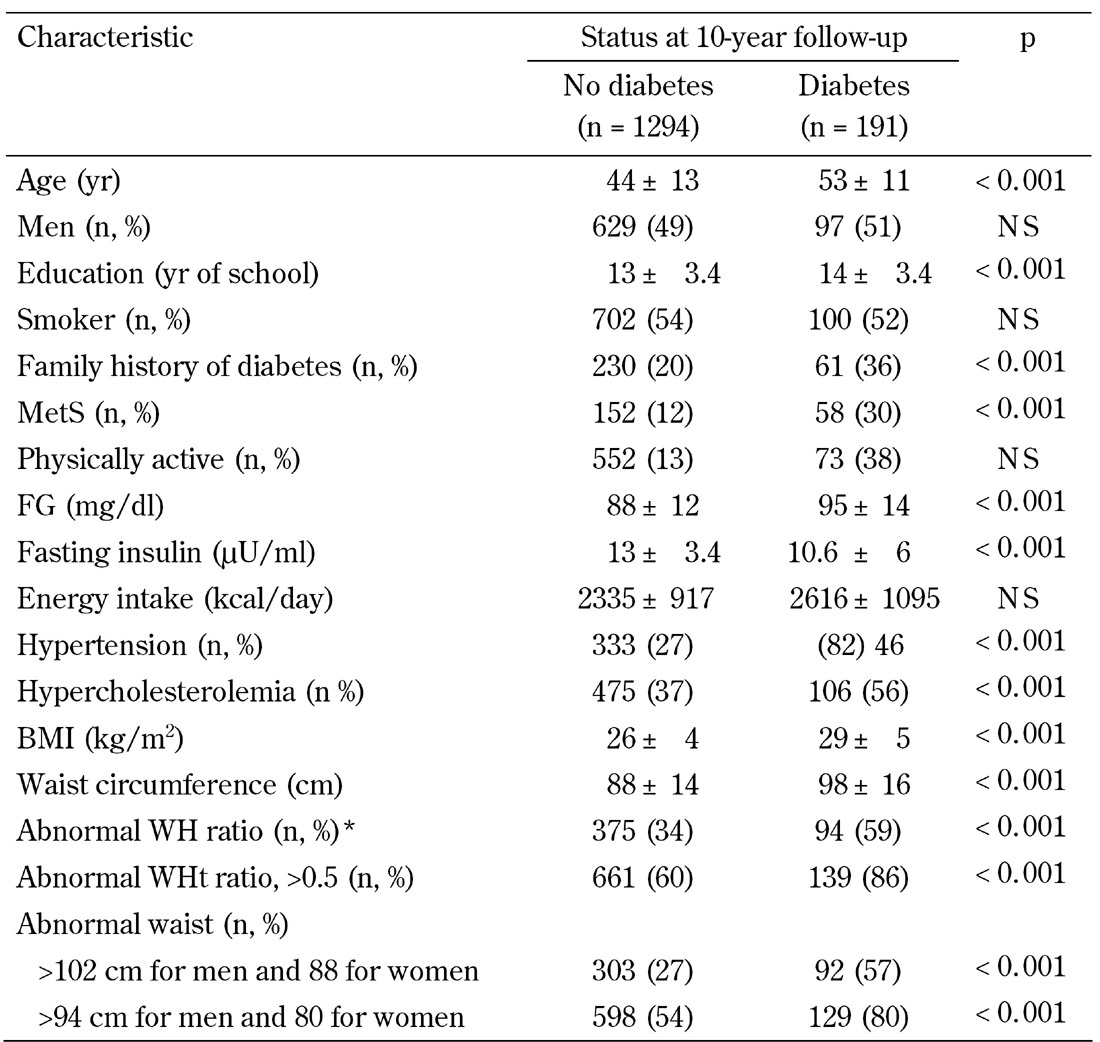
Legend: Data are mean ± SD or number (n) and percentage. * >0.8 for women and 1 for men.
Significant differences in baseline characteristics were observed between individuals for whom information on 10-year diabetes status was available (n = 1485) and those for whom it was not (n = 1347). The differences related to hypertension status (30% vs. 26%, p = 0.036), smoking habits (58% vs. 54%, p = 0.028), abnormal waist circumference (50% vs. 54%, p = 0.027), fasting glucose levels (88 ± 12 vs. 80 ± 13 mg/dl, p = 0.005), and fasting insulin levels (12 ± 3.0, 13 ± 3.4 μU/ml, p = 0.014). No differences were observed regarding the distribution of gender, years of education, family history of diabetes, physical activity status, metabolic syndrome, hypercholesterolemia status, BMI, abnormal waist-to-hip and waist-to-height ratios, and energy intake (all p-values > 0.05).
3.2 Determinants of 10-year diabetes risk
All the aforementioned comparisons are prone to confounders. Therefore, a multi-adjusted analysis was performed. The most predictive variables for 10-year diabetes incidence included age, family history of diabetes, abnormal WHt ratio, energy intake, and fasting glucose levels (Table 4). Specifically, a difference in baseline age of 1 year, and in fasting glucose of 1 mg/dl, were associated with a 14%, and almost 5%, higher risk of developing diabetes within a decade, whereas increasing daily energy intake by 500 Kcal was found to increase the risk by 2%. However, the highest risk of developing diabetes was observed among participants with a family history of diabetes or abnormal WHt ratio. The latter factors were associated with a 2.79-fold and 3.27-fold increase in diabetes incidence. Physical activity was found not to predict diabetes development regarding either intensity levels (low, moderate, vigorous) or type (aerobic, resistance, combo) (ps > 0.05, results not shown).
Table 4. Results from multiple logistic regression performed to evaluate various baseline characteristics in relation to the 10-year incidence of diabetes among ATTICA study participants (n = 1485).
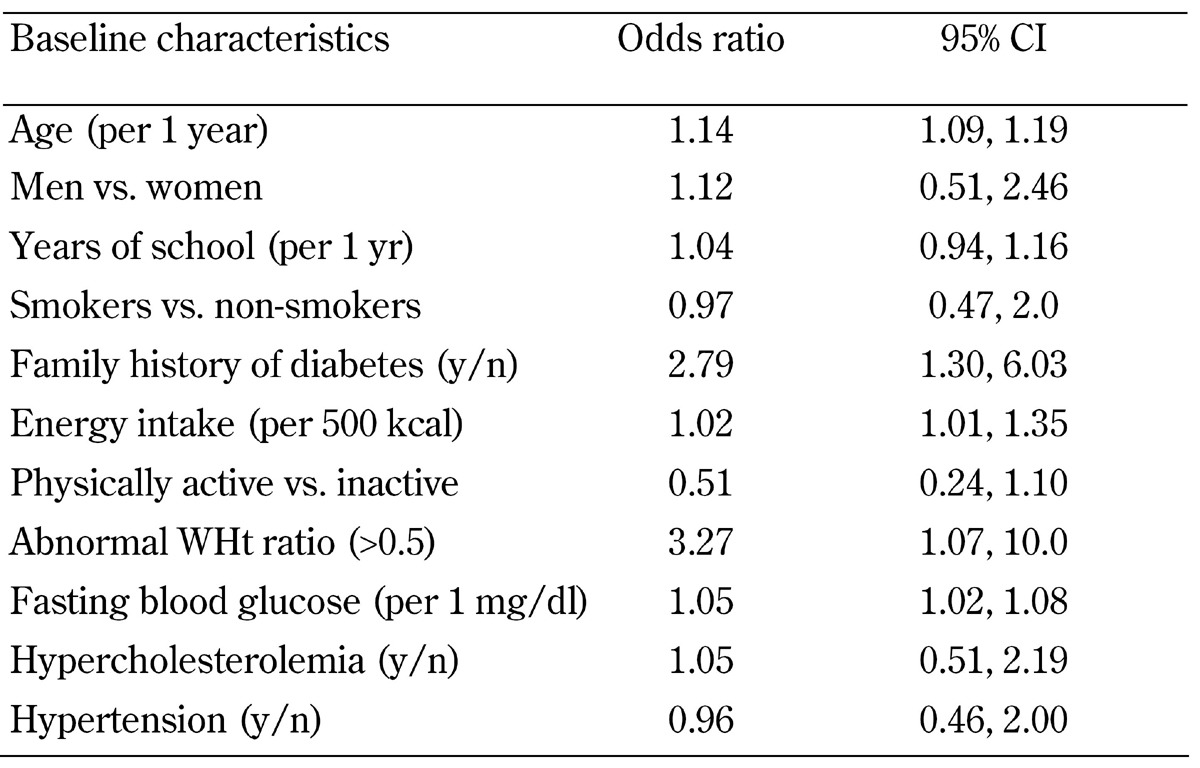
All anthropometric variables determining visceral obesity, including waist circumference (in cm), abnormal waist circumference (using both cut-off values of >94/80 and >102/88), and abnormal WH ratio, were entered separately into the models. They were all positively correlated with diabetes risk at a significant level (results not shown). Abnormal WHt ratio was maintained in the final model as it showed the best explanatory power compared to the other variables; it had a better goodness of fit of the estimated models, which also included gender, years of school, physical activity, smoking, hypercholesterolemia and hypertension status, and the lowest -2log-likelihood value.
BMI was also a significant predictor of diabetes (OR = 1.11, 95%CI: 1.01-1.22). However, it was removed from the final model because it was correlated with WHt ratio (r = -0.42, p < 0.05) and induced undesirable colinearity. BMI and WHt ratio showed similar goodness-of-fit and -2log-likelihhod values (223.6 and 224.1, respectively) when included in the model alone. However, the final decision to maintain WHt ratio was made because of its ability to represent more clearly abdominal obesity, which plays a crucial role in diabetes development. No difference in the predictive power of anthropometric measurements was observed between genders (p for interaction of all anthropometric variables with gender was >0.05 in the age-adjusted model). All aforementioned relationships were independent of gender, years of education, physical activity, smoking habits, and history of hypercholesterolemia and hypertension.
Finally, even though physical activity was found not to play a significant role in diabetes incidence, stratified analysis revealed a moderating effect (p for interaction <0.05). Specifically, being active was found to eliminate the previously observed aggravating effect of diabetes family history and fasting blood glucose levels. In the active group, the only significant risk factor apart from age was the abnormal WHt ratio, which increased diabetes risk by the factor 10.1.
4. Discussion
We studied the long-term incidence of diabetes in Greece based on prospective data from the ATTICA study. It showed that 129 new cases of diabetes per 1000 people were diagnosed during the ten years’ observation period (2002-2012), with almost equal representation of both genders (13.4% for men and 12.4% for women). Given that the entire Greek population amounts to 10.8 million in 2011 [21], an estimate of 1.5 million new cases within the past 10 years means a serious rise in diabetes incidence. This alarming trend is in accordance with diabetes incidence rates worldwide; for example, 14% in Mexico (18-year follow up) [22], 10.3% in Iran (9-year follow up) [23], and 19.7% (including type 1 diabetes) in Spain (13-year follow-up) [24].
The trend towards rising incidence rates is also reflected by the higher rate in the second five-year follow-up period, compared with the first one. Since screening for diabetes is not carried out systematically, but remains a matter of people's voluntary decision, the increase is a true increase in number, and is not due to improved screening procedures. In this regard, the financial impact of the epidemic spread of the disease becomes more critical and deserves particular consideration. Based on the accelerating increase in diabetes incidence and improved type 2 diabetes prognosis [25], it becomes clear that the health care cost for diabetes management per person will escalate continuously, which represents a current global trend [2].
Diabetes development results from a continuous interplay between genes and environmental/behavioral factors [26]. In this study, the observed increase in diabetes incidence was mainly a result of population aging, abnormal WHt ratio, elevated fasting glucose level, and family history of diabetes. Among all anthropometric variables, WHt ratio, along with BMI, was found to have the best explanatory power of diabetes risk prediction, with a 3.27- and 1.11-times increased risk per unit, respectively. While BMI is already well known as a risk factor for diabetes [27], WHt ratio is relatively new. One of the suggested advantages in choosing WHt ratio instead of BMI is the ability to use one single cut-off point (0.5), irrespectively of age, sex, or ethnicity [28], resulting in an immediate and simple message, namely to "keep the waist circumference to less than half the height". A recent meta-analysis of epidemiological studies found that the WHt ratio represents a superior diagnostic tool in detecting subjects with high cardiometabolic risk, including diabetes; however, this has proved more useful in Asian populations [29]. The latter may explain why the two measurements (BMI and WHt) were found to be equal in predicting diabetes risk.
Family history of diabetes was the second risk factor to play a crucial role in diabetes development in our study. It increased the risk of diabetes by factor 2.8, thus confirming the disease's genetic component [30]. Age, blood glucose level, and energy intake also had an aggravating effect. Specifically, diabetes risk was found to increase by 14% per 1 year's increase in age, by 5% per 1 mg/dl increase in fasting glucose (or 50% per 10 mg/dl), and by 2% per 500 kcal increase in energy intake.
It is generally thought that regular physical activity substantially reduces the risk of developing type 2 diabetes, with recent studies suggesting a tailored exercise program, instead of a "one size fits all" approach [31]. Surprisingly, in our study, physical activity was not found to exert a beneficial effect on diabetes incidence, similarly to the 5-year follow-up [15]. This points to a change in the importance of this factor over time, even though the Greek population is moving towards a more active lifestyle [32]. However, the observed moderating effect of exercise, which to the best of our knowledge has not been reported elsewhere, needs to be discussed. It was reported, that even though family predisposition to diabetes and elevated fasting glucose increase the risk of developing diabetes, being active outweighs the aggravating effect of both risk factors. This emphasizes the particular importance of exercise in stabilizing health. Surprisingly, active participants with a WHt ratio of >0.5 show a 10.1-fold increased risk of developing diabetes, while for inactive participants WHt was not significant. This finding seems strange, but may be explained by the intense stress for the body when engaging in physical activity, which may conflict with its beneficial effect. More studies are needed to investigate this phenomenon.
5. Limitations
There are some limitations to the present study. Firstly, the baseline evaluation was performed only once, and may be prone to measurement error. Secondly, the exact date of diabetes development was not available and was thus not included in the study. Instead, we included the date of diabetes diagnosis, which was available. In consequence, calculation of person-time and incidence rates was not feasible, and was thus not performed.
Participants with CVD at baseline, for whom information about diabetes status was not available in the 10-year follow-up, were excluded from the current analysis, along with 1347 participants for whom diabetes status was not known at baseline. This may have influenced diabetes incidence. Moreover, the true incidence of diabetes may have been underestimated in participants whose medical information was retrieved only through telephone interviews.
As for diabetes determinants, relative risks were estimated by odds ratios through multiple logistic regression analysis, which may overestimate the actual relative risk. However, it has been reported that for low-prevalence diseases, odds ratio is an accurate estimate of the relative risk. Another issue in prospective studies is that associations with disease incidence are based entirely on baseline information, but many lifestyle factors such as energy intake, physical activity, and smoking status may have changed during the long 10-year period and no timely information updates have been carried out.
Finally, the diabetes risk model was adjusted for most major confounders except psychological parameters, such as perceived stress and anxiety, which have significantly increased within the past 5 years in Greece because of the socioeconomic crisis.
The advantages of the present study include a large, representative sample, a prospective design for a fairly long period of 10 years, and the assessment of various lifestyle characteristics and, therefore, the ability to control for potential confounders.
6. Conclusions
Despite continuous progress in medical science, the results presented are discouraging and point to a continuous increase in diabetes incidence. The prevalence of the disease has risen in Greece during the past 10 years, which confirms global trends. Given that population aging is inevitable, the aggravating effects of a family history of diabetes and obesity may be balanced by an active lifestyle. This implies a need for the promotion of healthier nutrition and more physical activity to decrease the incidence rates of diabetes.
The new findings reported here shed light on the reasons for diabetes etiology. They highlight the significantly predictive power of the WHt ratio (vs. other anthropometric measures). This finding may be helpful for the design of future clinical trials with tailored intervention protocols.
Disclosures: Demosthenes Panagiotakos and Ekavi Georgousopoulou received research grants from Coca-Cola SA.
Acknowledgments
The authors would like to thank the investigators of the ATTICA study group: Yannis Skoumas, Natassa Katinioti, Labros Papadimitriou, Constantina Masoura, Spiros Vellas, Yannis Lentzas, Manolis Kambaxis, Konstadina Palliou, Vassiliki Metaxa, Agathi Ntzouvani, Dimitris Mpougatsas, Nikolaos Skourlis, Christina Papanikolaou, Georgia-Maria Kouli, Aimilia Christou, Adella Zana, Maria Ntertimani, Aikaterini Kalogeropoulou, Alexandros Laskaris, Mihail Hatzigeorgiou and Athanasios Grekas for their assistance with the initial physical examination and follow-up evaluation. Also, we are grateful to Efi Tsetsekou for her assistance with the psychological evaluation, and to the laboratory team, including Carmen Vassiliadou and George Dedoussis (genetic analysis), Marina Toutouza-Giotsa, Constadina Tselika, and Sia Poulopoulou (biochemical analysis), and Maria Toutouza for database management.
References
- 1.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA. et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.IDF Diabetes Atlas. sixth edition International Diabetes Federation; [Google Scholar]
- 3.Fox CS. Cardiovascular disease risk factors, type 2 diabetes mellitus, and the Framingham Heart Study. Trends Cardiovasc Med. 2010;20(3):90–95. doi: 10.1016/j.tcm.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H. et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34(39):3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 5.World Population Prospects: The 2012 Revision. http://esa.un.org/unpd/wpp/Excel-Data/population.htm.
- 6.Mayor S. International Diabetes Federation consensus on prevention of type 2 diabetes. Int J Clin Pract. 2007;61(10):1773–1775. doi: 10.1111/j.1742-1241.2007.01547.x. [DOI] [PubMed] [Google Scholar]
- 7.Beziaud F, Halimi JM, Lecomte P, Vol S, Tichet J. Cigarette smoking and diabetes mellitus. Diabetes Metab. 2004;30(2):161–166. doi: 10.1016/s1262-3636(07)70102-7. [DOI] [PubMed] [Google Scholar]
- 8.Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, Rehm J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;32(11):2123–2132. doi: 10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Athyros VG, Elisaf MS, Alexandrides T, Achimastos A, Ganotakis E, Bilianou E, Karagiannis A, Liberopoulos EN, Tziomalos K, Mikhailidis DP. Long-term impact of multifactorial treatment on new-onset diabetes and related cardiovascular events in metabolic syndrome: a post hoc ATTEMPT analysis. Angiology. 2012;63(5):358–366. doi: 10.1177/0003319711421341. [DOI] [PubMed] [Google Scholar]
- 10.Bianchi C, Del Prato S. Metabolic memory and individual treatment aims in type 2 diabetes - outcome-lessons learned from large clinical trials. Rev Diabet Stud. 2011;8(3):432–440. doi: 10.1900/RDS.2011.8.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gikas A, Sotiropoulos A, Panagiotakos D, Peppas T, Skliros E, Pappas S. Prevalence, and associated risk factors, of self-reported diabetes mellitus in a sample of adult urban population in Greece: MEDICAL Exit Poll Research in Salamis (MEDICAL EXPRESS 2002) BMC Public Health. 2004;4:2. doi: 10.1186/1471-2458-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gikas A, Sotiropoulos A, Panagiotakos D, Pastromas V, Paraskevopoulou E, Skliros E, Pappas S. Rising prevalence of diabetes among Greek adults: findings from two consecutive surveys in the same target population. Diabetes Res Clin Pract. 2008;79(2):325–329. doi: 10.1016/j.diabres.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Pitsavos C, Panagiotakos DB, Chrysohoou C, Stefanadis C. Epidemiology of cardiovascular risk factors in Greece: aims, design and baseline characteristics of the ATTICA study. BMC Public Health. 2003;3:32. doi: 10.1186/1471-2458-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C. The epidemiology of Type 2 diabetes mellitus in Greek adults: the ATTICA study. Diabet Med. 2005;22(11):1581–1588. doi: 10.1111/j.1464-5491.2005.01731.x. [DOI] [PubMed] [Google Scholar]
- 15.Panagiotakos DB, Pitsavos C, Skoumas Y, Lentzas Y, Stefanadis C. Five-year incidence of type 2 diabetes mellitus among cardiovascular disease-free Greek adults: findings from the ATTICA study. Vasc Health Risk Manag. 2008;4(3):691–698. doi: 10.2147/vhrm.s2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papathanasiou G, Georgoudis G, Papandreou M, Spyropoulos P, Georgakopoulos D, Kalfakakou V, Evangelou A. Reliability measures of the short International Physical Activity Questionnaire (IPAQ) in Greek young adults. Hellenic J Cardiol. 2009;50(4):283–294. [PubMed] [Google Scholar]
- 17.Katsouyanni K, Rimm EB, Gnardellis C, Trichopoulos D, Polychronopoulos E, Trichopoulou A. Reproducibility and relative validity of an extensive semi-quantitative food frequency questionnaire using dietary records and biochemical markers among Greek schoolteachers. Int J Epidemiol. 1997;26(Suppl 1):S118–S127. doi: 10.1093/ije/26.suppl_1.s118. [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes Association. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20(7):1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 19.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000. 2000;894:i-xii:1–253. [PubMed] [Google Scholar]
- 20.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 21. http://en.wikipedia.org/wiki/Demographics_of_Greece.
- 22.Gonzalez-Villalpando C, Davila-Cervantes CA, Zamora-Macorra M, Trejo-Valdivia B, Gonzalez-Villalpando ME. Incidence of type 2 diabetes in Mexico: results of the Mexico City Diabetes Study after 18 years of follow-up. Salud Publica Mex. 2014;56(1):11–17. doi: 10.21149/spm.v56i1.7318. [DOI] [PubMed] [Google Scholar]
- 23.Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F. Sex-specific incidence rates of type 2 diabetes and its risk ractors over 9 years of follow-up: Tehran lipid and glucose study. Plos One. 2014;9(7):e102563. doi: 10.1371/journal.pone.0102563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vega T, Gil M, Lozano J. Age and sex differences in the incidence of diabetes mellitus in a population-based Spanish cohort. J Diabetes. 2014 doi: 10.1111/1753-0407.12183. In press. [DOI] [PubMed] [Google Scholar]
- 25.Andresdottir G, Jensen ML, Carstensen B, Parving HH, Rossing K, Hansen TW, Rossing P. Improved survival and renal prognosis of patients with type 2 diabetes and nephropathy with improved control of risk factors. Diabetes Care. 2014;37(6):1660–1667. doi: 10.2337/dc13-2036. [DOI] [PubMed] [Google Scholar]
- 26.Murea M, Ma L, Freedman BI. Genetic and environmental factors associated with type 2 diabetes and diabetic vascular complications. Rev Diabet Stud. 2012;9(1):6–22. doi: 10.1900/RDS.2012.9.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 28.Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247–269. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- 29.Savva SC, Lamnisos D, Kafatos AG. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes. 2013;6:403–419. doi: 10.2147/DMSO.S34220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison TA, Hindorff LA, Kim H, Wines RC, Bowen DJ, McGrath BB, Edwards KL. Family history of diabetes as a potential public health tool. Am J Prev Med. 2003;24(2):152–159. doi: 10.1016/s0749-3797(02)00588-3. [DOI] [PubMed] [Google Scholar]
- 31.Gill JM, Cooper AR. Physical activity and prevention of type 2 diabetes mellitus. Sports Med. 2008;38(10):807–824. doi: 10.2165/00007256-200838100-00002. [DOI] [PubMed] [Google Scholar]
- 32.Tzormpatzakis N, Sleap M. Participation in physical activity and exercise in Greece: a systematic literature review. Int J Public Health. 2007;52(6):360–371. doi: 10.1007/s00038-007-6118-6. [DOI] [PubMed] [Google Scholar]


