Abstract
Youth with autism spectrum disorder often struggle to cope with co-occurring anxiety, depression, or anger, and having both internalizing and externalizing symptoms is a common clinical presentation. A number of authors have designed cognitive-behavioral interventions to address transdiagnostic factors related to multiple emotional problems, although none have applied this focus to youth with ASD. The current review article describes how a transdiagnostic emotion regulation framework may inform cognitive-behavioral interventions for youth with ASD, which until now have focused almost exclusively on anxiety. Research is needed to empirically test how a transdiagnostic intervention can address the processes of emotion regulation and assist youth with ASD to cope with their emotional disorders.
Keywords: autism spectrum disorder, cognitive behavior therapy, emotion regulation, transdiagnostic
Introduction
Emotional and behavioral difficulties are a serious set of associated issues for individuals with autism spectrum disorder (ASD) who by definition of their diagnosis of ASD already struggle with pervasive impairments in sociocommunicative functioning and restricted or repetitive behaviors or interests. For the purposes of this review, I view emotional and behavioral problems as symptoms that lead to significant impairment above the individual's baseline level of impairment related to his or her symptoms of ASD (i.e., above the impairment associated with the core social, communication, and repetitive features of ASD; as in Leyfer et al., 2006). Distinguishing core symptoms of ASD from comorbid internalizing and externalizing symptoms is particularly challenging, and a number of authors suggest that while some symptoms may reflect distinct disorders with unique etiologies, other symptoms are likely “co-occurring” issues, related to the etiology of the ASD or associated with symptoms of ASD (see also the commentaries by Folstein & Carbajal, 2012; Kerns & Kendall, 2012; Ollendick & White, 2012; Scahill, 2012; Wood & Gadow, 2010).
Rates of emotional and behavioral problems are high in youth with ASD, either when viewed as comorbid or as co-occurring. Using a population-based cohort, Totsika, Hastings, Emerson, Berridge, and Lancaster (2011) report that 59% of 5-year-olds with ASD and no intellectual disability have clinically significant levels of hyperactivity, 46% have clinically significant conduct problems, and 38% have clinically significant emotional problems. Across 5- to 16-year-olds with ASD and no intellectual disability, 85% are noted to have clinically significant levels of hyperactivity, 74% with clinically significant levels of emotional problems, and 64% with clinically significant conduct problems (Totsika, Hastings, Emerson, Lancaster, & Berridge, 2011; with similar rates for youth with ASD and intellectual disability). Using an adaptive psychiatric interview that distinguished ASD symptoms from other Axis I psychiatric symptoms, Simonoff et al. (2008) estimate that 70% of 12- to 16-year-olds with ASD meet criteria for at least one comorbid condition, with anxiety disorders being the most common set of disorders, at 42%. Similarly, Leyfer et al. (2006) developed the Autism Comorbidity Interview to distinguish between ASD-related social avoidance from social anxiety disorder and ASD-related agitation from generalized anxiety and found that 72% of their sample met criteria for at least one DSM-IV Axis I condition.1 These emotional and behavioral problems place a high burden on the individual, his or her family caregivers, and service providers, and detract tremendously from individual and family quality of life.
There is also substantial overlap of internalizing and externalizing symptoms in people with ASD. Approximately 40–50% of youth with ASD will meet criteria for two or more psychiatric disorders when using psychiatric interviews adapted to take into account ASD symptoms (Leyfer et al., 2006; Simonoff et al., 2008). Individuals with ASD who have high levels of depression or anxiety also show increased levels of noncompliance, aggressive behavior, and irritability (Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Matson & Nebel-Schwalm, 2007; Tantum, 2000), and difficulties with anger, depression, and anxiety are found to be correlated, both when using self-report (Quek, Sofronoff, Sheffield, White, & Kelly, 2012) and parent report data (Hurtig et al., 2009). Numerous studies of children with ASD highlight correlations within and between internalizing and externalizing symptoms (Gadow, DeVincent, & Pomeroy, 2006; Lecavalier, Gadow, DeVincent, & Edwards, 2008; Leyfer et al., 2006; Weisbrot, Gadow, DeVincent, & Pomeroy, 2005). This overlap is not surprising, given that even in the general population, both anxious and depressed individuals are noted to have associated difficulties with sadness, anger, and anxiety (Rohde, 2012). Such data have led authors to suggest that there may be a shared mechanism underlying problems with emotions (Trosper, Buzzella, Bennett, & Ehrenreich, 2009). They suggest that the various expressions of psychopathology are the manifestation of a broader syndrome, with “shared psychosocial and biological diatheses” (Barlow, Allen, & Choate, 2004, p. 210).
The fact that individuals with various psychiatric diagnoses may share common underlying problems has led many to suggest that there are limitations to a disorder-specific approach to treating emotional problems in the general population (Dudley, Kuyken, & Padesky, 2011). These issues may well extend to treating emotional problems in people with ASD, given the aforementioned rates. On a practical level, the current disorder-specific approach to treatment limits our ability to address multiple comorbidities in a real-world context. Clinicians are often asked to provide treatment to individuals with ASD who do not demonstrate symptoms that map efficiently onto diagnostic categories, yet who continue to struggle with stressors. A stress generation dynamic has been described to explain the nature of anxiety disorders within the context of ASD and can be readily applied to explain other emotional problems, such as depression or anger (Wood & Gadow, 2010). In their model, Wood and Gadow (2010) suggest that ASD-related stressors (of social confusion; peer rejections and victimization related to ASD symptoms; prevention or punishment of preferred behaviors or interests; and frequent aversive sensory experiences) lead to increased overall negative affectivity, anxiety disorders (depending on the experiences, social phobia, obsessive-compulsive disorder, generalized anxiety, or separation anxiety), or depression. In turn, such negative affectivity contributes to more ASD symptoms, conduct problems, and personal distress, which lead to even further ASD-related stressors, completing a negative cycle. Wood and Gadow's (2010) model is not limited to one form of anxiety disorder or even anxiety disorders more broadly. By explaining the cycle of a broad range of stressors and emotion problems, the model highlights how transdiagnostic mechanisms may be important contributors to psychopathology in youth with ASD.
The Need for a Transdiagnostic Cognitive-Behavioral Approach
While there does exist an important and growing literature on the efficacy of cognitive behavior therapy (CBT) for anxiety disorders in youth with ASD (McNally Keehn, Lincoln, Brown, & Chavira, 2013; Reaven, Blakeley-Smith, Culhane-Shelburne, & Hepburn, 2012; Sofronoff, Attwood, & Hinton, 2005; White, Ollendick, Scahill, Oswald, & Albano, 2009; Wood et al., 2009), the majority of this treatment research does not account for youth who specifically have co-occurring depression or anger problems, and none have examined commensurate changes in these other important emotional domains. Further, there is far less evidence demonstrating ways of treating conduct problems, oppositionality, attentional problems, or depression in individuals with ASD, although some promising initial pilot work is emerging in these areas (Scarpa & Reyes, 2011; Singh et al., 2011; Sofronoff, Attwood, Hinton, & Levin, 2007; Spek, van Ham, & Nyklíček, 2013). Having co-occurring disorders is known to be related to poor prognosis in and following therapy for typically developing individuals (Rohde, 2012), which may also explain why a significant proportion of youth with ASD in treatment for an anxiety disorder continue to exhibit problems with anxiety following the disorder-specific intervention (McNally Keehn et al., 2013; Reaven et al., 2012; Wood et al., 2009). Relying solely on a diagnosis-driven approach may make it difficult to find interventions to address the underlying factors that might lead to any combination of anxiety, depression, or anger-related problems, which, if addressed, could facilitate change across several presenting problems. At the same time, Dudley et al. (2011) note that although disorder-specific models may emphasize differences in treatment applicability, there are considerable similarities among evidence-based manuals, which may in fact be helpful to address multiple emotional problems. This exists even within the very limited CBT literature for children with ASD, with two randomized controlled trials (RCTs) using almost exactly the same “tool kit” for anger and anxiety (Sofronoff et al., 2005, 2007).
A number of cognitive-behavioral interventions exist targeting transdiagnostic factors that are common across presenting problems, in individuals without ASD (Boisseau, Farchione, Fairholme, Ellard, & Barlow, 2010; Ehrenreich, Goldstein, Wright, & Barlow, 2009). While a systematic review of the evidence for the effectiveness of transdiagnostic approaches for youth and adults is beyond the scope of this review, there are a number of findings that suggest that a transdiagnostic conceptualization can inform treatment planning. For instance, a recent RCT in adults with anxiety disorders (without ASD) using group transdiagnostic CBT, designed to address multiple types of anxiety disorders (e.g., used in a uniform way to target social anxiety, generalized anxiety disorder, and specific phobia), was found to be as efficacious as disorder-specific CBT for these conditions (Norton & Barrera, 2012) and more efficacious than a group relaxation training program (Norton, 2012). This group transdiagnostic treatment also appears to result in greater improvements in comorbid mood disorders compared to diagnostic-specific CBT from previous studies (rates of 67% improvement in the transdiagnostic group versus approximately 49% in benchmarking studies; Norton et al., 2013). Other research groups have demonstrated that transdiagnostic CBT for adults with anxiety and depression is efficacious compared to waitlist controls, using RCT designs (Farchione et al., 2012; Johnston, Titov, Andrews, Spence, & Dear, 2011; Titov et al., 2013), and may assist in long-term relapse prevention compared to treatment as usual for adults who received inpatient CBT (Ebert, Tarnowski, Gollwitzer, Sieland, & Berking, 2013). The research on transdiagnostic CBT for children or youth with anxiety and depression is less developed, leaving many to call for more research using RCT designs (Kendall, Settipani, & Cummings, 2012; Rohde, 2012). To date, most research on transdiagnostic CBT in youth is limited to case studies (e.g., Ehrenreich-May & Bilek, 2012) or open trials (Bilek & Ehrenreich-May, 2012), although ongoing RCT studies appear promising (Ehrenreich-May, Queen, Bilek, Remmes, & Marciel, 2013).
Emotion regulation is often a core focus of these transdiagnostic models (McLaughlin, Hatzenbuehler, Mennin, & Nolen-Hoeksema, 2011), which has been implicated in over half of DSM-IV Axis I and all of the Axis II disorders (Chambers, Gullone, & Allen, 2009). For example, the Unified Protocol for the Treatment of Emotional Disorders is a transdiagnostic cognitive-behavioral intervention for adults with anxiety or depression (UP; Barlow et al., 2011; Farchione et al., 2012) that focuses on the internal emotional experience and emotion regulation, employing commonly used strategies of psychoeducation, reappraisal, and exposure (for a discussion of its development and how it differs from traditional CBT, see Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010). The UP was recently adapted for children and adolescents (UP-Y; Ehrenreich et al., 2009; Trosper et al., 2009), with a focus on treating anxiety, depression, and anger. The eight-module intervention consists of five mandatory modules (emotion education, emotion awareness, cognitive flexibility, exposure to distressing emotions, and relapse prevention) and three optional modules (motivational enhancement, crisis management, and parenting skills). Youth remain in the module until they demonstrate mastery over the material (up to 21 sessions in total). Preliminary research with adolescents demonstrates significant reduction in anxiety and depressive symptomatology, and an increase in parent-reported child emotion regulation (Bilek & Ehrenreich-May, 2012). Ehrenreich-May and colleagues’ pioneering application of an emotion regulation framework (Gross & Thompson, 2007) stands to inform how we address emotional problems in youth with ASD, who struggle in many respects to a greater degree with emotion regulation than typically developing peers. The following article outlines a developmental contextual emotion regulation framework to assist in the treatment planning for youth with ASD who struggle with multiple emotional problems.
Emotion Regulation Formulation
Emotion regulation is defined as the process of effectively managing emotions in response to environmental demands and has been implicated in conceptualizations of emotional disorders in children and adults (see Aldao, Nolen-Hoeksema, & Schweizer, 2010, for a comprehensive review). Emotion regulation strategies are typically initiated, either consciously (effortful and controlled) or unconsciously (effortless and automatic), in response to emotion-eliciting stimuli, with the aim of altering the degree or type of a person's emotional experience or the stimuli (Aldao & Nolen-Hoeksema, 2010). Successful emotion regulation, through the use of adaptive and the disuse of maladaptive strategies, has been implicated as an instrumental act for positive outcomes in children (Garnefski, Rieffe, Jellesma, Terwogt, & Kraaij, 2006). Whether an emotion regulation strategy is adaptive is determined by its outcome, as it refers to processes that are successful in achieving the appropriate affect and do not have negative long-term costs (Campbell-Sills & Barlow, 2007). This last point is important, as it sets the stage for determining whether a particular emotion regulation behavior should be promoted to reduce distress or seen as a problematic behavior. For instance, a child may have a specific ritual that he or she likes to perform to reduce test-taking anxiety (e.g., making sure his or her desk is organized correctly and counting to five quietly before starting). When put into practice, this ritual may be adaptive if there are no negative consequences to it (i.e., it does not lead to social, personal, or other negative outcomes) and if it does not interfere with test taking. Instead, it helps the child control his or her stress and focus on the task at hand. This same behavior may be considered maladaptive if adherence to it qualifies as an obsession and interference with it leads to behavioral issues or problems with the ability to take the test. It may also be considered maladaptive if it leads to additional negative outcomes, such as social isolation.
A number of recent review articles suggest that problems with emotion regulation may explain many of the emotional and behavioral problems in individuals with ASD. Mazefsky et al. (2013) outline the ways in which emotion regulation impairments may be related to ASD. Given the high rates of psychiatric comorbidities, it may be that a comorbid psychiatric condition impacts emotion regulation skills in youth with ASD. Conversely, it may be that individuals with ASD have core deficits in emotion regulation, which then account for emotional and behavioral problems in this population, similar to the research on transdiagnostic factors associated with multiple psychiatric comorbidities in the typically developing population (e.g., McLaughlin et al., 2011). It may also be that the same emotion regulation impairments that are associated with the onset of anxiety and mood disorders are related to the presentation of symptoms of ASD, with shared underlying clinical and biological mechanisms. For instance, emotion regulation occurs in the prefrontal and ventromedial prefrontal cortex, including the amygdala (Kross, Davidson, Weber, & Ochsner, 2009), and these same areas have been implicated in the social impairments found in individuals with ASD (Gallager & Frith, 2003; see Mazefsky et al., 2013, for a detailed review of the neurological basis of emotion regulation deficits in individuals with ASD).
Ultimately, Mazefsky and colleagues suggest that emotion regulation deficits in individuals with ASD are related to interactions among many elements, including the presence of neural circuitry that explains both psychiatric issues and ASD symptoms (e.g., abnormal amygdala/prefrontal cortex function and connectivity), of psychiatric conditions, of greater baseline levels of negative affectivity and hyperarousal, and of ASD-related behavioral (e.g., lack of social motivation, awareness of emotion) and cognitive features (e.g., perseveration, rigidity, poor problem solving, and information processing). Given the many different potential interactions, it is likely that multiple profiles of emotion regulation characterize individuals with ASD (Mazefsky, Pelphrey, & Dahl, 2012), and a framework with which to organize emotion regulation is important to understand individual differences and determine specific ways of intervening (Mazefsky & White, 2014; Sofronoff, Beaumont, & Weiss, 2014).
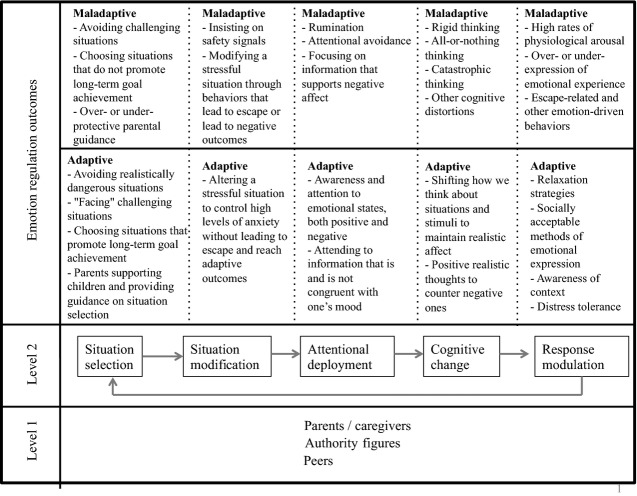
Gross and Thompson (2007) describe five temporally linked domains of a person–situation interaction where emotions can be regulated: situation selection, situation modification, attentional deployment, cognitive change, and response modulation. By employing a transdiagnostic case conceptualization that examines each component, clinicians can foster a child's internal skills to help him or her regulate emotions when confronted with challenges. For instance, these five components serve as the framework of Ehrenreich-May's UP-Y program, informing intervention design to address emotion regulation problems in youth without ASD. Understanding how youth with ASD demonstrate maladaptive and adaptive emotion regulation processes can greatly assist treatment planning. Figure1 presents common adaptive and maladaptive aspects of each component, and how it can be examined with an ASD lens (described below).
Figure 1.
Transdiagnostic emotion regulation model. The five processes of Gross and Thompson's (2007) modal model of emotion regulation, with each one leading to the next, and response modulation affecting one's situation selection or other ER domains (Level 2). Successful emotion regulation, at any one domain, is considered an individual–relational interaction with parents/caregivers, peers, and other authority figures (e.g., teachers; Level 1). Each process may be “adaptive” or “maladaptive,” depending on any given strategy's short- and long-term outcomes.
Situation Selection
Situation selection (Figure1) involves the “purposeful approach toward situations believed to result in pleasant emotions, and avoidance of situations believed to result in undesirable emotions” (Trosper et al., 2009, p. 238). Staying away from a truly dangerous situation is an example of adaptive situation selection. Successful situation selection requires an understanding of context and an ability to estimate probable outcomes. While many individuals with ASD may have no trouble understanding familiar situations that have concrete and predictable (and particularly nonsocial) rules, novel situations that are social and unstructured decrease the likelihood of an adaptive response (Baron-Cohen, Ring, et al., 1999; Baron-Cohen, Wheelwright, Stone, & Rutherford, 1999; Lawson, Baron-Cohen, & Wheelwright, 2004; Minshew, Meyer, & Goldstein, 2002). Such situations require tolerance for uncertainty, learning new rules, flexibility, understanding of context, and theory of mind, all demands that are often challenging for individuals with ASD (Gomot & Wicker, 2012). The insistence on routine and ritual exhibited by many youth with ASD, which has been associated with emotional problems (Gotham et al., 2013), may lead to an increased likelihood of choosing a limited number of pleasurable and familiar situations. Adaptive situation selection also requires that children have opportunities to choose to experience a variety of situations, and many parents report issues around a lack of goodness-of-fit between a child with ASD's needs and the available environmental supports, thereby limiting situational options (Hodgetts, Nicolas, & Zwaigenbaum, 2013; Orsmond, Krauss, & Seltzer, 2004).
Maladaptive situation selection typically refers to problematic avoidance of situations. Avoidance has long been implicated within cognitive and learning models of emotional disorders, particularly as a mechanism that maintains the association between the stimulus and emotional response, through negative reinforcement. It also prevents the process of extinction and habituation from occurring (which would weaken the conditioning). Avoidance is a common element of anxiety disorders (Aldao et al., 2010; Rapee, 2002), and depression, where individuals withdraw from pleasurable activities and social situations (Mash & Wolfe, 2002). It further compounds anger responses as well, when there is a likelihood that the situation will arise in the near future and is believed to be threatening. When confronted with the possibility of negative emotion-eliciting situations, children with ASD have been shown to resort to avoidance more than typically developing peers (Jahromi, Meek, & Ober-Reynolds, 2012) and may act in ways to avoid being exposed to the situation, never building the skills or confidence related to it. Youth with ASD are at increased risk of avoiding novel situations as a result of insistence on routine and ritual (Gotham et al., 2013), further failing to experience opportunities for increased competence and confidence. Similarly, they are at greater risk of avoiding or withdrawing from social situations as a result of impairments in sociocommunicative skill (Dawson & Lewy, 1989; Jawaid et al., 2012), losing important opportunities for social skills growth and social engagement (Orsmond et al., 2004). Facing emotion-eliciting situations through graduated exposure is a foundational element of cognitive behavior therapy for children with and without ASD (Munoz-Solomando, Kendall, & Whittington, 2008; Reaven et al., 2012; Wood et al., 2009). The use of social stories is another strategy often employed to address weaknesses in dealing with novel situations, understanding, and predictive skill (Ivey, Heflin, & Alberto, 2004). Further, the application of priming as a means of exposure to assist in transitions or to new situations (Schreibman, Whalen, & Stahmer, 2000), and programming for the generalization of skills to new situations (Kleeberger & Mirenda, 2010), is viewed as an evidence-based strategy in applied behavior analysis for children with ASD.
Situation Modification
Situation modification (Figure1) involves altering situations to address emotional responses. Successful problem solving, defined as the conscious act of modifying the emotion-eliciting situation or its consequences (Snyder, 2010; Spering, Wagener, & Funke, 2005), represents adaptive situation modification. Individuals with ASD are known to have difficulties with social and “real-world” problem solving (Channon, Charman, Heap, Crawford, & Rios, 2001), which can lead them to act in inappropriate ways or serve to make the problem situation worse. For example, if faced with a stressful situation at school, an effective solution may be to speak to the teacher, and by doing so, could serve to modify the situation in an appropriate way. An ineffective solution might be to lose control over one's anger and act aggressively in class. Both options “solve” the problem by modifying the environment, yet one is clearly more adaptive than the other. Helping children with ASD to problem-solve effectively is thought to be an important part of improving their adaptive emotion regulation (Magyar & Pandolfi, 2012).
A more subtle maladaptive modification would be to overly rely on “safety signals” to indicate that an aversive stimulus will not occur in a situation (Campbell-Sills & Barlow, 2007). Safety signals “can be inanimate objects (e.g., a certain room in the home), behaviors (e.g., sitting at a desk close to an exit), or other people (e.g., a parent)” (Trosper et al., 2009, p. 238). An overreliance on safety signals teaches an individual to depend on the external world for control and safety and leads to a dependence on the external signal for temporary emotional relief, instead of learning that he or she can manage successfully in the emotion-eliciting situation. The behavioral rigidities found in ASD may serve as safety signal behaviors, by perseverating on those cues that maintain emotional relief (Howlin, 2004). For instance, a child who must keep his or her desk in a specific way to avoid feeling uncomfortable in class is relying on that rule for regulation. When children are able to identify and distance themselves from an overreliance on safety signals, they develop a positive internal locus of control, which is related to reduced anxiety, depression, and anger (Clark, Olympia, Jensen, Heathfield, & Jenson, 2004). Finally, youth with ASD who exhibit an intense adherence to routine and ritual may demonstrate maladaptive situation modification by attempting to ensure that their environments remain exactly the same, a violation of which can result in a host of emotionally driven responses (Barnhill, 2007; Dominick, Davis, Lainhart, Tager-Flusberg, & Folstein, 2007). It is also clear that behavioral rigidities in ASD serve a host of functions in addition to those that connote safety, such as sensory reinforcement or producing adult attention, and that understanding this function is instrumental for developing effective behavioral interventions (Kennedy, Meyer, Knowles, & Shukla, 2000).
When we do not have an opportunity to choose or modify our situations, we continue to regulate our emotions via our attentional deployment (Figure1), which involves how we choose to focus or distance our attention on the situation. Three aspects of attentional deployment are considered here: (a) emotional awareness, (b) mood-congruent attentional bias, and (c) rumination. Emotional awareness is defined “as an attentional process that serves to monitor and differentiate emotions, locate their antecedents, but ignore the physical arousal that is part of the emotion experience” (Rieffe et al., 2011, p. 656) and has been implicated as a prerequisite process to successful attentional deployment. Children with ASD have difficulties with emotional awareness of themselves and others (Tanaka et al., 2012; Williams & Happé, 2010), including difficulties assessing and labeling their own emotions (i.e., alexithymia; Fitzgerald & Bellgrove, 2006; Hill, Berthoz, & Frith, 2004; Szatmari et al., 2008). Poor emotion awareness has been linked to internalizing symptoms in children with and without ASD (Rieffe et al., 2011) and is a barrier to constructive help seeking and problem solving (Zeman, Shipman, & Suveg, 2002). Helping children to learn about emotional signals, and how emotions are related to their thoughts and actions, can improve the ability to control emotions (Friedberg & McClure, 2002; Scarpa & Reyes, 2011). In fact, teaching about emotions is a common aspect of well-known behavioral early intervention programs for children with ASD (Smith, 2006).
When individuals struggle with emotions, they often show an attention bias on information that is related to the problem emotion, confirming its validity by being more likely to notice situational signals that are in line with the emotion and less able to see the signals that are not. Regardless of whether the bias is toward threat-related cues (common in anxiety and anger; Bögels & Zigterman, 2000; Koster, Verschuere, Crombez, & Van Damme, 2005; Mineka, Rafaeli, & Yovel, 2003; Williams, Mathews, & MacLeod, 1996; Yovel & Mineka, 2005) or hopeless and rejection-related cues (common in depression; Williams et al., 1996; Yovel & Mineka, 2005), children benefit from seeing the positive and neutral elements of their situations (Groden, Kantor, Woodard, & Lipsitt, 2011). Children with ASD may be at greater risk to focus on negative or irrelevant cues (Embregts & van Nieuwenhuijzen, 2009), and although they are often detail oriented (O'Riordan, Plaisted, Driver, & Baron-Cohen, 2001), they may miss the most contextual and central information required to counter their emotional states (Farrugia & Hudson, 2006). According to parent report, children with ASD are often less able to focus and shift their attention on emotionally relevant stimuli compared to peers, indicating that their attentional biases may be highly rigid (Bailey, Hatton, Mesibov, Ament, & Skinner, 2000; Hepburn & Stone, 2006; Janes, 2001; Konstantareas & Stewart, 2006; Landry & Bryson, 2004). Rumination is a related maladaptive attentional strategy, defined as “a pattern of responding to distress in which an individual passively and perseveratively thinks about his or her upsetting symptoms and the causes and consequences of those symptoms, while failing to initiate the active problem solving that might alter the cause of that distress” (McLaughlin & Nolen-Hoeksema, 2011, p. 186). Rumination includes excessive worry and brooding, which can lead to emotional distress in children and youth with ASD (Rieffe et al., 2011). As children with ASD are predisposed to perseverate, they are at risk of rumination, and interventions are required to improve their abilities to shift their focus toward positive topics when needed.
It is important to note that the mechanisms underlying rumination in children with and without ASD may differ. Problems with attention in individuals with ASD extend beyond a problematic focus on emotionally laden stimuli or situations, or with coping with distress, and may instead be caused by broader deficits in executive functions, including response inhibition, working memory, cognitive flexibility (set-shifting), planning, and fluency (Ozonoff & Strayer, 1997; Pennington & Ozonoff, 1996). It is well known that children with ASD have difficulties shifting attention from one activity, rule, or interest, even when the focus is not distressing and there is no negative affect (Ozonoff, Strayer, McMahon, & Filloux, 1994), suggesting that perseveration is related to overall difficulties with cognitive control. This speaks to broader impairments in attention as potential risk factors and causes for rumination in individuals with ASD, rather than the emotional experience being the cause. (Mazefsky, Oswald, et al., 2012; Mazefsky, Pelphrey, et al., 2012) suggest that motivationally significant topics, such as intense interests, may lead to dampened cognitive flexibility and to impaired ability to disengage attention and that this reduced ability can lead to emotion regulation problems. This broader cause of rumination in individuals with ASD highlights the need for interventions to address cognitive flexibility and attentional difficulties beyond emotion regulation to assist individuals with ASD in emotion regulation tasks. Such attentional deployment is a hallmark of mindfulness-based interventions, which aim to bring attention to emotions in a nonjudgmental way, promoting acceptance and a move away from both suppression and rumination (de Bruin, Zijlstra, & Bögels, 2014). In adults with ASD, mindfulness-based cognitive therapy has been successfully used to reduce rumination, anxiety, and depression (Spek et al., 2013). In young children with ASD, particular interventions have focused on improving joint attention between mother and child, and this improvement in joint attention has led to improvements in emotion regulation (Gulsrud, Jahromi, & Kasari, 2010).
Even if we cannot control the situation or our attention to it, our emotional reactions can be modified through our thoughts about the situation and our capacity to cope with it, known as cognitive change (Figure1; Gross & Thompson, 2007). Reappraisal typically involves using evidence to alter the valence or intensity of the experience (Trosper et al., 2009). Developing reasonable interpretations of a distressing situation (i.e., reappraisal), rather than directly attempting to change it, can lessen its emotional impact (Aldao et al., 2010). Reappraisal also occurs through the interpretations of the meanings we place on the emotions themselves (Gross & Thompson, 2007). Like all emotion regulation strategies, reappraisal is a developmental process, which only fully emerges at approximately age 10 years (as cited in Chambers et al., 2009; Ochsner & Gross, 2005). Prior to this age, more concrete levels of reappraisal continue to be effective, such as using positive statements to offset negative ones, and it is these that can most help youth with ASD. Children with ASD are at great risk of employing maladaptive cognitive change strategies, including “all-or-nothing” and catastrophic thinking, which can impact their interpretations of emotion-eliciting situations (Attwood, 2004; Fujii et al., 2013). They have been shown to be capable of developing cognitive change strategies, including coping statements and thinking in more neutral or positive ways about distressing situations, to counteract these cognitive distortions (Beaumont & Sofronoff, 2008; Reaven et al., 2012; Sofronoff et al., 2005).
Response Modulation
Response modulation (Figure1) involves the physiological and behavioral ways of regulating emotion after it is felt. For example, relaxation strategies are meant to lessen physiological arousal, resulting in a calmer emotional state (Weersing, Rozenman, Maher-Bridge, & Campo, 2012). Children with ASD are less able to sooth and are more sensitive to negative stimuli than matched peers (Janes, 2001; Konstantareas & Stewart, 2006; Landry &Bryson, 2004). They may also exhibit an overall higher rate of physiological arousal (Bal et al., 2010; Hirstein, Iversen, & Ramachandran, 2001; Kylliäinen & Hietanen, 2006). If used appropriately, relaxation strategies, such as progressive muscle relaxation, can help children with ASD to experience a negative emotion at a suitable level, while staying in the situation to benefit from exposure (Mullins & Christian, 2001; Sofronoff et al., 2005, 2007).
Response modulation also involves how emotions are behaviorally expressed. Trosper et al. (2009) note that emotional expression lies on a continuum from inhibition, to appropriate expression, to exaggeration of emotional response. Children with emotional disorders are known to show both an under- and overcontrol of emotional expression, by inhibiting emotional expression and by expressing it in nonconstructive, excessive ways (Zeman et al., 2002). The appropriate expression of emotion is influenced by how it is modeled by others and the larger social context (Gross & Thompson, 2007; Zeman & Shipman, 1998), and youth with ASD are often susceptible to missing such cues (Loveland, Pearson, Tunali-Kotoski, Ortegon, & Gibbs, 2001). As such, an important part of intervention is to help youth to understand the social situation and how best to express their feelings (Friedberg & McClure, 2002; Williams, Gray, & Tonge, 2012). Teaching behavioral self-management strategies to children with ASD is a common aspect of applied behavior analysis and can include differentially reinforcing prosocial ways of expressing emotions (Lee, Simpson, & Shogren, 2007).
As avoidance is to situation selection, escape-related behaviors are to response modulation, implemented once a person experiences a distressing emotion in an effort to reduce the intensity. When objectively dangerous situations exist, escape is an important adaptive strategy of responding to an emotional signal. However, individuals with emotional difficulties often aim to escape situations that they interpret as threatening or undesirable, and by doing so, serve to maintain the contingency linking the negative emotion to the situation (Trosper et al., 2009). As such, response modulation is thought to influence one's situation selection (Gross & Thompson, 2007). Such emotion-driven behaviors take many forms, including withdrawal, aggression, or flight (Barlow et al., 2004), and children with ASD are well known to react to negative emotions with behaviors that serve escape functions (Jahromi et al., 2012). They also struggle more to tolerate experiencing negative affect compared to peers (Goldstein & Schwebach, 2004; Loveland & Tunali-Kotoski, 1997). There is a robust literature in applied behavior analysis indicating how differential reinforcement can address behaviors that serve escape functions (e.g., Hagopian, Wilson, & Wilder, 2001; Harper, Iwata, & Camp, 2013). Helping children with ASD endure negative affect in an acceptable way, without attempting to escape, is a critical component of helping them manage their emotions (Singh et al., 2011).
A Developmental Contextual Framework of Emotion Regulation
Emotion regulation is described as an individual-context transactional process (Figure1, Level 1; Gross & Thompson, 2007) embedded within an ecological framework of multiple systems of influence (Bronfenbrenner, 1986, 1992). That is, the development and continued use of emotion regulation require an alignment among a child's internal capabilities and the provision of ecological resources found in the family, school, and larger community (often described as “developmental assets”; Benson, 2006; Lerner, 2005). The comprehensive model of positive youth development (or thriving) articulated by Lerner and colleagues provides an ideal example of how an ongoing process of emotion regulation requires particular child characteristics and external supports (Geldhof, Weiner, Agans, Mueller, & Lerner, 2014). We are influenced by, and influence, our ecological assets, which include “the presence, quantity, and accessibility of human, material, and social resources in the environment” (Lerner, 2005, p. 40).
There are indeed key individuals who are instrumental in promoting successful emotion regulation in youth with and without ASD. Parents play a critical role supporting all children in selecting appropriate situations, scaffolding skills and the development of confidence, and modeling appropriate regulation strategies (Gross & Thompson, 2007). Scaffolding is defined as a process where a more experienced individual (e.g., parent) provides assistance to the child in a way that helps him or her develop within a zone of proximal development (Harrop & Green, 2012; Vygotsky, 1978) and involves three overarching components: contingency, fading, and transfer of responsibility (van de Pol, Volman, & Beishuizen, 2010). A number of parent strategies, which appear to target specific emotion regulation domains as discussed above, can be used to scaffold (Reiss, unpublished manuscript): distraction (altering attentional deployment), reassurance (as a safety signal; situation modification), encouragement/praise (response modulation), guidance/problem solving (situation modification), following/elaborating (elaborating on a child's distress), or direction/control (verbally or physically directing a child's attentional deployment or situation selection; Calkins & Johnson, 1998; Eisenberg & Fabes, 1994; Grolnick, Kurowski, & McMenamy, 1998; Rubin, Hastings, Chen, Stewart, & McNichol, 1998). In the context of emotion regulation, a parent's behavior “scaffolds” a child's emotion regulation development if it is tailored to the developmental level and degree of needs of the child in a particular context, faded as the child begins to demonstrate more competence in handling the context, and is done in a way that the child gains more understanding and responsibility for emotion regulation. For instance, adaptive situation selection for children involves the developmentally appropriate provision of guidance from parents, who need to assist in choosing the appropriate contexts (e.g., children may not want to go to the dentist, but parents rightly override that situation selection choice). As well, through shared attention and engagement in emotion-eliciting situations, parents help their children to attend adaptively to modulate their distress (Raver, 1996).
Parental emotional scaffolding has been associated with emotion regulation in children with and without ASD, although the research is still sparse. Mothers of children with and without ASD are able to synchronize their behaviors to their children's attention and behavior (Siller & Sigman, 2002; Watson, 1998), and mothers of children with ASD are able to adapt their scaffolding to their children's individual levels of need, both of which are critical for successful scaffolding (Kasari, Sigman, Mundy, & Yimiya, 1988; Konstantareas, Zajdeman, Homatidis, & McCabe, 1988). Parents are often integral parts of behavioral intervention programs for children with ASD, and there is substantial evidence that providing parents with the skills to implement pivotal response training (a form of applied behavior analysis) can assist in teaching children with ASD self-management skills (Koegel & Kern Koegel, 2006; Schreibman & Koegel, 1996). When scaffolding is present, children with developmental disabilities show greater improvements in social skills, including aspects of emotional regulation (Baker, Fenning, Crnic, Baker, & Blacher, 2007), and more recently, Gulsrud et al. (2010) demonstrated that children with ASD and their parents “co-regulate” emotions during distressing events. In this latter study, 34 mother–child dyads participated in a joint attention intervention, and the authors studied children's emotion regulation through behavioral observation across all intervention sessions. The authors found that mothers (and children) were more likely to use emotion regulation strategies during periods of distress compared to periods without distress and that child comfort strategies (physical self-comfort and comfort seeking) were correlated with maternal active (prompting/helping, redirection of attention, and providing physical comfort) and vocal strategies (vocal comfort and reassurance). Of interest, maternal scaffolding was positively related to children's levels of externalizing behaviors, suggesting that mothers are more likely to employ scaffolding in the presence of challenging behavior. Perhaps most important, over the course of the 24-session joint engagement intervention, mothers demonstrated more emotional scaffolding, commensurate with children demonstrating improved emotional regulation.
Recent advances in the treatment of anxiety disorders in youth with ASD underscore how parents play a role in the development and treatment of their children's anxiety disorders (Reaven, 2011; Wood et al., 2009). Reaven and Hepburn (2006; see also Reaven, 2011) describe the critical role parents play in the maintenance of anxiety in youth with ASD, and these influences can be applied to emotion regulation more broadly. Parents of youth with ASD are more likely to experience parenting stress and parental anxiety compared to parents of typically developing youth, and such states may predispose parents to tolerate children's maladaptive emotion regulation strategies (e.g., avoidance), preventing the development of adaptive coping. In turn, the failure to develop a repertoire of adaptive strategies leads to less perceived competence and the perpetuation of maladaptive strategies in challenging situations. Parent-involved cognitive behavior therapy leads to greater changes in anxiety for children with ASD compared to child-only CBT or to waitlist controls (Puleo & Kendall, 2011; Sofronoff et al., 2005), lending support to the need to involve parents in children's emotion regulation treatment.
Peers and authority figures (i.e., teachers) also play critical roles in influencing the growth and implementation of emotion regulation (Jahromi, Bryce, & Swanson, 2013). In typically developing children, self-regulation is correlated with emotional and behavioral engagement in school (Denham et al., 2003; Valiente, Lemery-Chalfant, & Castro, 2007; Valiente, Lemery-Chalfant, Swanson, & Reiser, 2008) and with prosocial peer engagement and peer acceptance (Valiente, Swanson, & Lemery-Chalfant, 2012). More recently, emotional regulation has been correlated with prosocial peer engagement in preschool children with ASD (Jahromi et al., 2013). Unfortunately, individuals with ASD are more likely to have relationships with atypical social agents in their environment (e.g., educational assistants, therapists, and other specialized support staff; Bauminger & Kasari, 2000; Daniel & Billingsley, 2010; Humphrey & Symes, 2010; Mesibov & Shea, 1996) as well as negative typical relationships (e.g., peers and teachers), and these relationships can have a profound impact on the cognitive schemata children form about themselves, others, and the future, greatly impacting their social-emotional characteristics (Bauminger, 2007). It is important to consider the various ways that peers can be involved in supporting children's development in the five discussed components of emotion regulation. For instance, there is emerging evidence that peer supports (such as peer “buddies”) can be used as a part of cognitive-behavioral interventions for anxiety in youth with ASD to provide ecologically valid opportunities for social and emotional development (White et al., 2013; Wood et al., 2009). Typically developing peers have also been used to teach complex social behaviors to children with ASD through pivotal response training (Pierce & Schreibman, 2013), highlighting how peers may be instrumental in teaching individuals with ASD complex socioemotional skills, including those involved in emotion regulation.
Conclusion
A disorder-specific approach to treating emotional problems may miss the main underlying maladaptive processes that can lead to problems with anxiety, depression, or anger, which are often found to be co-occurring in youth with ASD. A transdiagnostic framework has been effectively employed to treat emotion regulation impairments in typically developing youth with anxiety and depression (Ehrenreich-May & Bilek, 2012), and the components of this model have direct relevance to maladaptive processes often found in youth with ASD. Assessing maladaptive situation selection, situation modification, attentional deployment, cognitive change, and response modulation in youth with ASD may prove to be a useful method of formulating individual treatment plans to address emotional problems at a transdiagnostic level. Further research is needed to empirically test how a transdiagnostic intervention can address the processes of regulation and assist youth with ASD to cope with anger, anxiety, and depression.
Acknowledgments
I wish to thank Dr. Irene Drmic, Dr. J. Gayle Beck, and the manuscript reviewers for their helpful comments on earlier drafts of this article. This research was supported by the Chair in Autism Spectrum Disorders Treatment and Care Research (Canadian Institutes of Health Research #284208 in partnership with NeuroDevNet, Sinneave Family Foundation, CASDA, Autism Speaks Canada, and Health Canada), Spectrum of Hope Autism Foundation, and by a New Investigator Fellowship from the Ontario Mental Health Foundation.
Notes
A more recent pilot study of a smaller sample of adolescents with high-functioning ASD, using a newly modified psychiatric interview, suggests that earlier reports of rates may be overestimated by not comprehensively taking into account ASD symptoms, although even here rates continue to remain high (Mazefsky, Oswald, et al., 2012).
References
- Aldao A. Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy. 2010;48(10):974–983. doi: 10.1016/j.brat.2010.06.002. doi:10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. doi:10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Attwood T. Cognitive behaviour therapy for children and adults with Asperger's syndrome. Behaviour Change. 2004;21(3):147–161. . doi:10.1375/bech.21.3.147.55995. [Google Scholar]
- Bailey DB, Jr, Hatton DD, Mesibov G, Ament N. Skinner M. Early development, temperament, and functional impairment in autism and fragile X syndrome. Journal of Autism and Developmental Disorders. 2000;30(1):49–59. doi: 10.1023/a:1005412111706. doi:10.1023/A:1005412111706. [DOI] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, Crnic KA, Baker BL. Blacher J. Prediction of social skills in 6-year-old children with and without developmental delays: Contributions of early regulation and maternal scaffolding. American Journal on Mental Retardation. 2007;112(5):375–391. doi: 10.1352/0895-8017(2007)112[0375:POSSIY]2.0.CO;2. doi:10.1352/0895-8017(2007)112[0375:POSSIY]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Bal E, Harden E, Lamb D, Van Hecke AV, Denver JW. Porges SW. Emotion recognition in children with autism spectrum disorders: Relations to eye gaze and autonomic state. Journal of Autism and Developmental Disorders. 2010;40(3):358–370. doi: 10.1007/s10803-009-0884-3. doi:10.1007/s10803-009-0884-3. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB. Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. doi:10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB. Ehrenreich-May J. The unified protocol for transdiagnostic t reatment of emotional disorders: Therapist guide. New York, NY: Oxford University Press; 2011. [Google Scholar]
- Barnhill GP. Outcomes in adults with Asperger syndrome. Focus on Autism and Other Developmental Disabilities. 2007;22(2):116–126. . doi:10.1177/10883576070220020301. [Google Scholar]
- Baron-Cohen S, Ring H, Wheelwright S, Bullmore ET, Brammer MJ, Simmons A. Williams SC. Social intelligence in the normal and autistic brain: An fMRI study. European Journal of Neuroscience. 1999;11(6):1891–1898. doi: 10.1046/j.1460-9568.1999.00621.x. doi:10.1046/j.1460-9568.1999.00621.x. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Stone V. Rutherford M. A mathematician, a physicist and a computer scientist with Asperger syndrome: Performance on folk psychology and folk physics tests. Neurocase. 1999;5(6):475–483. doi:10.1080/13554799908402743. [Google Scholar]
- Bauminger N. Brief report: Group social-multimodal intervention for HFASD. Journal of Autism and Developmental Disorders. 2007;37(8):1605–1615. doi: 10.1007/s10803-006-0246-3. . doi:10.1007/s10803-006-0246-3. [DOI] [PubMed] [Google Scholar]
- Bauminger N. Kasari C. Loneliness and friendship in high-functioning children with autism. Child Development. 2000;71(2):447–456. doi: 10.1111/1467-8624.00156. doi:10.1111/1467-8624.00156. [DOI] [PubMed] [Google Scholar]
- Beaumont R. Sofronoff K. A multi-component social skills intervention for children with Asperger syndrome: The Junior Detective Training Program. Journal of Child Psychology and Psychiatry. 2008;49(7):743–753. doi: 10.1111/j.1469-7610.2008.01920.x. doi:10.1111/j.1469-7610.2008.01920.x. [DOI] [PubMed] [Google Scholar]
- Benson PL. All kids are our kids: What communities must do to raise caring and responsible children and adolescents. 2nd ed. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
- Bilek EL. Ehrenreich-May J. An open trial investigation of a transdiagnostic group treatment for children with anxiety and depressive symptoms. Behavior Therapy. 2012;43(4):887–897. doi: 10.1016/j.beth.2012.04.007. doi:10.1016/j.beth.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Bögels SM. Zigterman D. Dysfunctional cognitions in children with social phobia, separation anxiety disorder, and generalized anxiety disorder. Journal of Abnormal Child Psychology. 2000;28(2):205–211. doi: 10.1023/a:1005179032470. doi:10.1023/A:1005179032470. [DOI] [PubMed] [Google Scholar]
- Boisseau CL, Farchione TJ, Fairholme CP, Ellard KK. Barlow DH. The development of the unified protocol for the transdiagnostic treatment of emotional disorders: A case study. Cognitive and Behavioral Practice. 2010;17(1):102–113. doi: 10.1016/j.cbpra.2009.09.003. doi:10.1016/j.cbpra.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22(6):723–742. . doi:10.1037/0012-1649.22.6.723. [Google Scholar]
- Bronfenbrenner U. Ecological systems theory. London, UK: Jessica Kingsley; 1992. [Google Scholar]
- de Bruin EI, Zijlstra BJH. Bögels SM. The meaning of mindfulness in children and adolescents: Further validation of the Child and Adolescent Mindfulness Measure (CAMM) in two independent samples from the Netherlands. Mindfulness. 2014;5:422–430. doi:10.1007/s12671-013-0196-8. [Google Scholar]
- Calkins SD. Johnson MC. Toddler regulation of distress to frustrating events: Temperamental and maternal correlates. Infant Behavior and Development. 1998;21(3):379–395. doi:10.1016/S0163-6383(98)90015-7. [Google Scholar]
- Campbell-Sills L. Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. New York, NY: Guilford Press; 2007. [Google Scholar]
- Chambers R, Gullone E. Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. doi:10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Channon S, Charman T, Heap J, Crawford S. Rios P. Real-life-type problem-solving in Asperger's syndrome. Journal of Autism and Developmental Disorders. 2001;31(5):461–469. doi: 10.1023/a:1012212824307. doi:10.1023/A:1012212824307. [DOI] [PubMed] [Google Scholar]
- Clark E, Olympia DE, Jensen J, Heathfield LT. Jenson WR. Striving for autonomy in a contingency-governed world: Another challenge for individuals with developmental disabilities. Psychology in the Schools. 2004;41(1):143–153. doi:10.1002/pits.10146. [Google Scholar]
- Daniel LS. Billingsley BS. What boys with an autism spectrum disorder say about establishing and maintaining friendships. Focus on Autism and Other Developmental Disabilities. 2010;25(4):220–229. doi:10.1177/1088357610378290. [Google Scholar]
- Dawson G. Lewy A. Arousal, attention, and the socioemotional impairments of individuals with autism. New York, NY: Guilford Press; 1989. [Google Scholar]
- Denham SA, Blair KA, DeMulder E, Levitas J, Sawyer KS, Auerbach–Major S. Queenan P. Preschool emotional competence: Pathway to social competence? Child Development. 2003;74(1):238–256. doi: 10.1111/1467-8624.00533. doi:10.1111/1467-8624.00533. [DOI] [PubMed] [Google Scholar]
- Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H. Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities. 2007;28(2):145–162. doi: 10.1016/j.ridd.2006.02.003. doi:10.1016/j.ridd.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Dudley R, Kuyken W. Padesky CA. Disorder specific and trans-diagnostic case conceptualisation. Clinical Psychology Review. 2011;31(2):213–224. doi: 10.1016/j.cpr.2010.07.005. doi:10.1016/j.cpr.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Ebert D, Tarnowski T, Gollwitzer M, Sieland B. Berking M. A transdiagnostic internet-based maintenance treatment enhances the stability of outcomes after inpatient cognitive behavioural therapy: A randomized controlled trial. Psychotherapy and Psychosomatics. 2013;82:246–256. doi: 10.1159/000345967. doi:10.1159/000345967. [DOI] [PubMed] [Google Scholar]
- Ehrenreich JT, Goldstein CR, Wright LR. Barlow DH. Development of a unified protocol for the treatment of emotional disorders in youth. Child & Family Behavior Therapy. 2009;31(1):20–37. doi: 10.1080/07317100802701228. doi:10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich-May J. Bilek EL. The development of a transdiagnostic, cognitive behavioral group intervention for childhood anxiety disorders and co-occurring depression symptoms. Cognitive and Behavioral Practice. 2012;19(1):41–55. doi:10.1016/j.cbpra.2011.02.003. [Google Scholar]
- Ehrenreich-May J, Queen AH, Bilek EL, Remmes CR. Marciel KK. The unified protocols for the treatment of emotional disorders in children and adolescents. In: Chu BC, editor; Ehrenreich-May J, editor. Transdiagnostic treatments for children and adolescents: Principles and practice. New York, NY: Guilford Press; 2013. pp. 267–292. [Google Scholar]
- Eisenberg N. Fabes RA. Mothers’ reactions to children's negative emotions: Relations to children's temperament and anger behaviour. Merrill-Palmer Quarterly. 1994;40(1):138–156. [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ. Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. doi:10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embregts P. van Nieuwenhuijzen M. Social information processing in boys with autistic spectrum disorder and mild to borderline intellectual disabilities. Journal of Intellectual Disability Research. 2009;53(11):922–931. doi: 10.1111/j.1365-2788.2009.01204.x. doi:10.1111/j.1365-2788.2009.01204.x. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thomson-Hollands J, Carl JR. Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behaviour Therapy. 2012;43(3):666–678. doi: 10.1016/j.beth.2012.01.001. doi:10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrugia S. Hudson J. Anxiety in adolescents with Asperger syndrome: Negative thoughts, behavioral problems, and life interference. Focus on Autism and Other Developmental Disabilities. 2006;21(1):25–35. doi:10.1177/10883576060210010401. [Google Scholar]
- Fitzgerald M. Bellgrove MA. The overlap between alexithymia and Asperger's syndrome. Journal of Autism and Developmental Disorders. 2006;36(4):573–576. doi: 10.1007/s10803-006-0096-z. doi:10.1007/s10803-006-0096-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein SE. Carbajal J. Commentary on Kerns and Kendall. Clinical Psychology: Science and Practice. 2012;19(4):356–357. doi:10.1111/cpsp.12015. [Google Scholar]
- Friedberg RD. McClure JM. Clinical practice of cognitive therapy with children and adolescents: The nuts and bolts. New York, NY: Guilford Press; 2002. [Google Scholar]
- Fujii C, Renno P, McLeod BD, Lin CE, Decker K, Zielinski K. Wood JJ. Intensive cognitive behavioural therapy for anxiety disorders in school-aged children with autism: A preliminary comparison with treatment-as-usual. School Mental Health. 2013;5(1):1–13. doi:10.1007/s12310-012-9090-0. [Google Scholar]
- Gadow KD, DeVincent CJ. Pomeroy J. ADHD symptom subtypes in children with pervasive developmental disorder. Journal of Autism and Developmental Disorders. 2006;36(2):271–283. doi: 10.1007/s10803-005-0060-3. doi:10.1007/s10803-005-0060-3. [DOI] [PubMed] [Google Scholar]
- Gallager HL. Frith C. Functional imaging of ‘theory of mind’. Trends in Cognitive Sciences. 2003;7(2):77–83. doi: 10.1016/s1364-6613(02)00025-6. doi:10.1016/S1364-6613(02)00025-6. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Rieffe C, Jellesma F, Terwogt MM. Kraaij V. Cognitive emotion regulation strategies and emotional problems in 9–11-year-old children. European Child & Adolescent Psychiatry. 2006;16(1):1–9. doi: 10.1007/s00787-006-0562-3. doi:10.1007/s00787-006-0562-3. [DOI] [PubMed] [Google Scholar]
- Geldhof GJ, Weiner M, Agans JP, Mueller MK. Lerner RM. Understanding entrepreneurial intent in late adolescence: The role of intentional self-regulation and innovation. Journal of Youth and Adolescence. 2014;43:81–91. doi: 10.1007/s10964-013-9930-8. doi:10.1007/s10964-013-9930-8. [DOI] [PubMed] [Google Scholar]
- Goldstein S. Schwebach AJ. The comorbidity of pervasive developmental disorder and attention deficit hyperactivity disorder: Results of a retrospective chart review. Journal of Autism and Developmental Disorders. 2004;34(3):329–339. doi: 10.1023/b:jadd.0000029554.46570.68. doi:10.1023/B:JADD.0000029554.46570.68. [DOI] [PubMed] [Google Scholar]
- Gomot M. Wicker B. A challenging, unpredictable world for people with autism spectrum disorder. International Journal of Psychophysiology. 2012;83(2):240–247. doi: 10.1016/j.ijpsycho.2011.09.017. doi:10.1016/j.ijpsycho.2011.09.017. [DOI] [PubMed] [Google Scholar]
- Gotham K, Bishop SL, Hus V, Huerta M, Lund S, Buja A. Lord C. Exploring the relationship between anxiety and insistence on sameness in autism spectrum disorders. Autism Research. 2013;6(1):33–41. doi: 10.1002/aur.1263. doi:10.1002/aur.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groden J, Kantor A, Woodard CR. Lipsitt LP. How everyone on the autism spectrum, young and old, can become resilient, be more optimistic, enjoy humor, be kind, and increase self-efficacy—A positive psychology approach. London, UK: Jessica Kingsley; 2011. [Google Scholar]
- Grolnick WS, Kurowski CO. McMenamy JM. Mothers’ strategies for regulating their toddlers’ distress. Infant Behaviour and Development. 1998;21(3):437–450. doi:10.1016/S0163-6383(98)90018-2. [Google Scholar]
- Gross JJ. Thompson RA. Handbook of emotion regulation. New York, NY: Guilford Press; 2007. Emotion regulation: Conceptual foundations. In J. J. Gross (Ed.), (pp. 3–24) [Google Scholar]
- Gulsrud AC, Jahromi LB. Kasari C. The co-regulation of emotions between mothers and their children with autism. Journal of Autism and Developmental Disorders. 2010;40(2):227–237. doi: 10.1007/s10803-009-0861-x. doi:10.1007/s10803-009-0861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Wilson DM. Wilder DA. Assessment and treatment of problem behavior maintained by escape from attention and access to tangible items. Journal of Applied Behavior Analysis. 2001;34(2):229–232. doi: 10.1901/jaba.2001.34-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper JM, Iwata BA. Camp EM. Assessment and treatment of social avoidance. Journal of Applied Behavior Analysis. 2013;46(1):147–160. doi: 10.1002/jaba.18. doi:10.1002/jaba.18. [DOI] [PubMed] [Google Scholar]
- Harrop CE. Green J. 2012. Exploring the IMPACT of Vygotsky in pre-school autism. Poster session presented at the meeting of the International Meeting for Autism Research, Toronto, ON.
- Hepburn SL. Stone WL. Using Carey Temperament Scales to assess behavioral style in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2006;36(5):637–642. doi: 10.1007/s10803-006-0110-5. doi:10.1007/s10803-006-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill E, Berthoz S. Frith U. Brief report: Cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. Journal of Autism and Developmental Disorders. 2004;34(2):229–235. doi: 10.1023/b:jadd.0000022613.41399.14. doi:10.1023/B:JADD.0000022613.41399.14. [DOI] [PubMed] [Google Scholar]
- Hirstein W, Iversen P. Ramachandran VS. Autonomic responses of autistic children to people and objects. Proceedings of the Royal Society of London. Series B: Biological Sciences. 2001;268(1479):1883–1888. doi: 10.1098/rspb.2001.1724. doi:10.1098/rspb.2001.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgetts S, Nicolas D. Zwaigenbaum L. Home sweet home? Families’ experiences with aggression in children with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2013;28:166–174. doi:10.1177/1088357612472932. [Google Scholar]
- Howlin P. Autism and Asperger syndrome: Preparing for adulthood. 2nd ed. London, UK: Routledge; 2004. [Google Scholar]
- Humphrey N. Symes W. Responses to bullying and use of social support among pupils with autism spectrum disorders (ASDs) in mainstream schools: A qualitative study. Journal of Research in Special Educational Needs. 2010;10(2):82–90. doi:10.1111/j.1471-3802.2010.01146.x. [Google Scholar]
- Hurtig T, Kuusikko S, Mattila ML, Haapsamo H, Ebeling H, Jussila K. Moilanen I. Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism. 2009;13(6):583–598. doi: 10.1177/1362361309335719. doi:10.1177/1362361309335719. [DOI] [PubMed] [Google Scholar]
- Ivey ML, Heflin LJ. Alberto P. The use of social stories to promote independent behaviors in novel events for children with PDD-NOS. Focus on Autism and Other Developmental Disabilities. 2004;19(3):164–176. doi:10.1177/10883576040190030401. [Google Scholar]
- Jahromi LB, Bryce CI. Swanson J. The importance of self-regulation for the school and peer engagement of children with high-functioning autism. Research in Autism Spectrum Disorders. 2013;7(2):235–246. doi:10.1016/j.rasd.2012.08.012. [Google Scholar]
- Jahromi LB, Meek SE. Ober-Reynolds S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry. 2012;53(12):1250–1258. doi: 10.1111/j.1469-7610.2012.02560.x. doi:10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- Janes J. 2001. Executive function, emotion regulation, and maternal report of child temperament in children with PDD. (Master's thesis). Retrieved from ProQuest Dissertations and Theses. (Accession Order No. AAT MQ61912)
- Jawaid A, Riby DM, Owens J, White SW, Tarar T. Schulz PE. ‘Too withdrawn’ or ‘too friendly’: Considering social vulnerability in two neuro- developmental disorders. Journal of Intellectual Disability Research. 2012;56(4):335–350. doi: 10.1111/j.1365-2788.2011.01452.x. doi:10.1111/j.1365-2788.2011.01452.x. [DOI] [PubMed] [Google Scholar]
- Johnston L, Titov N, Andrews G, Spence J. Dear BF. A RCT of a transdiagnostic internet-delivered treatment for three anxiety disorders: Examination of support roles and disorder-specific outcomes. PLoS ONE. 2011;6(11):e28079. doi: 10.1371/journal.pone.0028079. doi:10.1371/journal.pone.0028079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C, Sigman M, Mundy P. Yimiya N. Caregiver interactions with autistic children. Journal of Abnormal Child Psychology. 1988;16(1):45–56. doi: 10.1007/BF00910499. doi:10.1007/BF00910499. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Settipani CA. Cummings CM. No need to worry: The promising future of anxiety research. Journal of Clinical Child & Adolescent Psychology. 2012;41(1):103–115. doi: 10.1080/15374416.2012.632352. doi:10.1080/15374416.2012.632352. [DOI] [PubMed] [Google Scholar]
- Kennedy CH, Meyer KA, Knowles T. Shukla S. Analyzing the multiple functions of stereotypical behavior for students with autism: Implications for assessment and treatment. Journal of Applied Behavior Analysis. 2000;33(4):559–571. doi: 10.1901/jaba.2000.33-559. doi:10.1901/jaba.2000.33-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns CM. Kendall PC. The presentation and classification of anxiety in autism spectrum disorder. Clinical Psychology: Science and Practice. 2012;19(4):323–347. doi:10.1111/cpsp.12009. [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL. Wilson FJ. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4(2):117–132. doi:10.1177/1362361300004002002. [Google Scholar]
- Kleeberger V. Mirenda P. Teaching generalized imitation skills to a preschooler with autism using video modeling. Journal of Positive Behavior Interventions. 2010;12:116–127. doi:10.1177/1098300708329279. [Google Scholar]
- Koegel RL. Kern Koegel L. Pivotal response treatments for autism: Communication, social, and academic development. Baltimore, MD: Brookes; 2006. [Google Scholar]
- Konstantareas MM. Stewart K. Affect regulation and temperament in children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2006;36(2):143–154. doi: 10.1007/s10803-005-0051-4. doi:10.1007/s10803-005-0051-4. [DOI] [PubMed] [Google Scholar]
- Konstantareas MM, Zajdeman H, Homatidis S. McCabe A. Maternal speech to verbal and higher functioning versus nonverbal and lower functioning autistic children. Journal of Autism and Developmental Disorders. 1988;18(4):647–656. doi: 10.1007/BF02211882. doi:10.1007/BF02211882. [DOI] [PubMed] [Google Scholar]
- Koster EH, Verschuere B, Crombez G. Van Damme S. Time-course of attention for threatening pictures in high and low trait anxiety. Behaviour Research and Therapy. 2005;43(8):1087–1098. doi: 10.1016/j.brat.2004.08.004. doi:10.1016/j.brat.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Kross E, Davidson M, Weber J. Ochsner K. Coping with emotions past: The neural bases of regulating affect associated with negative autobiographical memories. Biological Psychiatry. 2009;65(5):361–366. doi: 10.1016/j.biopsych.2008.10.019. doi:10.1016/j.biopsych.2008.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kylliäinen A. Hietanen JK. Skin conductance responses to another person's gaze in children with autism. Journal of Autism and Developmental Disorders. 2006;36(4):517–525. doi: 10.1007/s10803-006-0091-4. doi:10.1007/s10803-006-0091-4. [DOI] [PubMed] [Google Scholar]
- Landry R, Bryson SE. Impaired disengagement of attention in young children with autism. Journal of Child Psychology and Psychiatry. 2004;45:1115–1122. doi: 10.1111/j.1469-7610.2004.00304.x. doi:10.1111/j.1469-7610.2004.00304.x. [DOI] [PubMed] [Google Scholar]
- Lawson J, Baron-Cohen S. Wheelwright S. Empathising and systemising in adults with and without Asperger syndrome. Journal of Autism and Developmental Disorders. 2004;34(3):301–310. doi: 10.1023/b:jadd.0000029552.42724.1b. doi:10.1023/B:JADD.0000029552.42724.1b. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Gadow KD, DeVincent CJ. Edwards MC. Validation of DSM-IV model of psychiatric syndromes in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;39(2):278–289. doi: 10.1007/s10803-008-0622-2. doi:10.1007/s10803-008-0622-2. [DOI] [PubMed] [Google Scholar]
- Lee SH, Simpson RL. Shogren KA. Effects and implications of self management for students with autism: A meta-analysis. Focus on Autism and Other Developmental Disabilities. 2007;22(1):2–13. doi:10.1177/10883576070220010101. [Google Scholar]
- Lerner RM. Promoting positive youth development: Theoretical and empirical bases. Washington, DC: National Academies of Science; 2005. . White paper prepared for the Workshop on the Science of Adolescent Health and Development, National Research Council/Institute of Medicine. [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J. Lainhart JE. Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36(7):849–861. doi: 10.1007/s10803-006-0123-0. . doi:10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Loveland KA, Pearson DA, Tunali-Kotoski B, Ortegon J. Gibbs MC. Judgments of social appropriateness by children and adolescents with autism. Journal of Autism and Developmental Disorders. 2001;31(4):367–376. doi: 10.1023/a:1010608518060. doi:10.1023/A:1010608518060. [DOI] [PubMed] [Google Scholar]
- Loveland KA. Tunali-Kotoski B. The school age child with autism. In: Volkmar FR, editor; Cohen DJ, editor. Handbook of autism and pervasive developmental disorders. 2nd ed. New York, NY: Wiley; 1997. pp. 283–308. [Google Scholar]
- Magyar CI. Pandolfi V. Considerations for establishing a multi-tiered problem-solving model for students with autism spectrum disorders and comorbid emotional-behavioral disorders. Psychology in the Schools. 2012;49(10):975–987. doi:10.1002/pits.21645. [Google Scholar]
- Mash EJ. Wolfe DA. Abnormal child psychology. Belmont, CA: Wadsworth; 2002. [Google Scholar]
- Matson JL. Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities. 2007;28(4):341–352. doi: 10.1016/j.ridd.2005.12.004. doi:10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L. White SW. The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(7):679–688. doi: 10.1016/j.jaac.2013.05.006. doi:10.1016/j.jaac.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Oswald DP, Day TN, Eack SM, Michshew NJ. Lainhart JE. ASD, a psychiatric disorder, or both? Psychiatric diagnoses in adolescents with high-functioning ASD. Journal of Clinical Child and Adolescent Psychology. 2012;41(4):516–523. doi: 10.1080/15374416.2012.686102. doi:10.1080/15374416.2012.686102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Pelphrey KA. Dahl RE. The need for a broader approach to emotion regulation research in atusim. Child Development Perspectives. 2012;6(1):92–97. doi: 10.1111/j.1750-8606.2011.00229.x. doi:10.1111/j.1750-8606.2011.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA. White SW. Emotion regulation: Concepts & practice in autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America. 2014;23(1):15–24. doi: 10.1016/j.chc.2013.07.002. doi:10.1016/j.chc.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS. Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy. 2011;49(9):544–554. doi: 10.1016/j.brat.2011.06.003. doi:10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA. Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011;49(3):186–193. doi: 10.1016/j.brat.2010.12.006. doi:10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally Keehn RHM, Lincoln AJ, Brown MZ. Chavira DA. The Coping Cat Program for children with anxiety and autism spectrum disorder: A pilot randomized controlled trial. Journal of Autism and Developmental Disorders. 2013;43(1):57–67. doi: 10.1007/s10803-012-1541-9. doi:10.1007/s10803-012-1541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesibov GB. Shea V. Full inclusion and students with autism. Journal of Autism and Developmental Disorders. 1996;26(3):337–346. doi: 10.1007/BF02172478. doi:10.1007/BF02172478. [DOI] [PubMed] [Google Scholar]
- Mineka S, Rafaeli E. Yovel I. Cognitive biases in emotional disorders: Information processing and social-cognitive perspectives. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Minshew NJ, Meyer J. Goldstein G. Abstract reasoning in autism: A dissociation between concept formation and concept identification. Neuropsychology. 2002;16(3):327–334. doi: 10.1037//0894-4105.16.3.327. doi:10.1037//0894-4105.16.3.327. [DOI] [PubMed] [Google Scholar]
- Mullins JL. Christian LA. The effects of progressive relaxation training on the disruptive behavior of a boy with autism. Research in Developmental Disabilities. 2001;22:449–462. doi: 10.1016/s0891-4222(01)00083-x. doi:10.1016/S0891-4222(01)00083-X. [DOI] [PubMed] [Google Scholar]
- Munoz-Solomando A, Kendall T. Whittington CJ. Cognitive behavioural therapy for children and adolescents. Current Opinion in Psychiatry. 2008;21(4):332–337. doi: 10.1097/YCO.0b013e328305097c. doi:10.1097/YCO.0b013e328305097c. [DOI] [PubMed] [Google Scholar]
- Norton PJ. A randomized clinical trial of transdiagnostic cognitve-behavioral treatments for anxiety disorder by comparison to relaxation training. Behavior Therapy. 2012;43(3):506–517. doi: 10.1016/j.beth.2010.08.011. . doi:10.1016/j.beth.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ. Barrera TL. Transdiagnostic versus diagnosis-specific CBT for anxiety disorders: A preliminary randomized controlled noninferiority trial. Depression and Anxiety. 2012;10:874–882. doi: 10.1002/da.21974. doi:10.1002/da.21974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, Barrera AR, Chamberlain LD, Szafranski DD, Reddy R. Smith A. Effect of transdiagnostic CBT for anxiety disorders on comorbid diagnoses. Depression and Anxiety. 2013;30(2):168–173. doi: 10.1002/da.22018. doi:10.1002/da.22018. [DOI] [PubMed] [Google Scholar]
- Ochsner KN. Gross JJ. The cognitive control of emotion. Trends in Cognitive Sciences. 2005;9(5):242–249. doi: 10.1016/j.tics.2005.03.010. doi:10.1016/j.tics.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Ollendick TH. White SW. The presentation and classification of anxiety in autism spectrum disorder: Where to from here? Clinical Psychology: Science and Practice. 2012;19(4):352–355. doi:10.1111/cpsp.12013. [Google Scholar]
- O'Riordan MA, Plaisted KC, Driver J. Baron-Cohen S. Superior visual search in autism. Journal of Experimental Psychology: Human Perception and Performance. 2001;27(3):719–730. doi: 10.1037//0096-1523.27.3.719. doi:10.1037/0096-1523.27.3.719. [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Krauss MW. Seltzer MM. Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders. 2004;34(3):245–256. doi: 10.1023/b:jadd.0000029547.96610.df. doi:10.1023/B:JADD.0000029547.96610.df. [DOI] [PubMed] [Google Scholar]
- Ozonoff S. Strayer DL. Inhibitory function in nonretarded children with autism. Journal of Autism and Developmental Disorders. 1997;27(1):59–77. doi: 10.1023/a:1025821222046. doi:10.1023/A:1025821222046. [DOI] [PubMed] [Google Scholar]
- Ozonoff S, Strayer DL, McMahon WM. Filloux F. Executive function abilities in autism and Tourette syndrome: An information processing approach. Journal of Child Psychology and Psychiatry. 1994;35(6):1015–1032. doi: 10.1111/j.1469-7610.1994.tb01807.x. doi:10.1111/j.1469-7610.1994.tb01807.x. [DOI] [PubMed] [Google Scholar]
- Pennington BF. Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37(1):51–58. doi: 10.1111/j.1469-7610.1996.tb01380.x. doi:10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Pierce K. Schreibman L. Increasing complex social behaviors in children with autism: Effects of peer-implemented pivotal response training. Journal of Applied Behavior Analysis. 2013;28(3):285–295. doi: 10.1901/jaba.1995.28-285. doi:10.1901/jaba.1995.28-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Pol J, Volman M. Beishuizen J. Scaffolding in teacher-student interaction: A decade of research. Educational Psychology Review. 2010;22(3):271–296. doi:10.1007/s10648-010-9127-6. [Google Scholar]
- Puleo CM. Kendall PC. Cognitive-behavioral therapy for typically developing youth with anxiety: Autism spectrum symptoms as a predictor of treatment outcome. Journal of Autism and Developmental Disorders. 2011;41:275–286. doi: 10.1007/s10803-010-1047-2. doi:10.1007s10803-010-1047-2. [DOI] [PubMed] [Google Scholar]
- Quek L-H, Sofronoff K, Sheffield J, White A. Kelly A. Co-occurring anger in young people with Asperger's syndrome. Journal of Clinical Psychology. 2012;68(10):1142–1148. doi: 10.1002/jclp.21888. doi:10.1002/jclp.21888. [DOI] [PubMed] [Google Scholar]
- Rapee RM. The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety. Biological Psychiatry. 2002;52(10):947–957. doi: 10.1016/s0006-3223(02)01572-x. . doi:10.1016/S0006-3223(02)01572-X. [DOI] [PubMed] [Google Scholar]
- Raver CC. Relations between social contingency in mother-child interaction and 2-year-olds’ social competence. Developmental Psychology. 1996;32(5):850–859. . doi:10.1037/0012-1649.32.5.850. [Google Scholar]
- Reaven J. The treatment of anxiety symptoms in youth with high-functioning autism spectrum disorders: Developmental considerations for parents. Brain Research. 2011;1380:255–263. doi: 10.1016/j.brainres.2010.09.075. . doi:10.1016/j.brainres.2010.09.075. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K. Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2012;53(4):410–419. doi: 10.1111/j.1469-7610.2011.02486.x. doi:10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven J. Hepburn S. The parent's role in the treatment of anxiety symptoms in children with high-functioning autism spectrum disorders. Mental Health Aspects of Developmental Disabilities. 2006;9(3):73–80. [Google Scholar]
- Rieffe C, Oosterveld P, Terwogt MM, Mootz S, van Leeuwen E. Stockmann L. Emotion regulation and internalizing symptoms in children with autism spectrum disorders. Autism. 2011;15(6):655–670. doi: 10.1177/1362361310366571. doi:10.1177/1362361310366571. [DOI] [PubMed] [Google Scholar]
- Rohde P. Applying transdiagnostic approaches to treatments with children and adolescents: Innovative models that are ready for more systematic evaluation. Cognitive and Behavioral Practice. 2012;19(1):83–86. . doi:10.1016/j.cbpra.2011.06.006. [Google Scholar]
- Rubin KH, Hastings P, Chen X, Stewart S. McNichol K. Intrapersonal and maternal correlates of aggression, conflict, and externalizing problems in toddlers. Child Development. 1998;69(6):1614–1629. doi:10.1111/j.1467-8624.1998.tb06180.x. [PubMed] [Google Scholar]
- Scahill L. Commentary on Kerns and Kendall. Clinical Psychology: Science and Practice. 2012;19(4):348–351. . doi:10.1111/cpsp.12018. [Google Scholar]
- Scarpa A. Reyes NM. Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: A pilot study. Behavioural and Cognitive Psychotherapy. 2011;39(4):495–500. doi: 10.1017/S1352465811000063. doi:10.1017/S1352465811000063. [DOI] [PubMed] [Google Scholar]
- Schreibman L. Koegel RL. Fostering self-management: Parent-delivered pivotal response training for children with autistic disorder. In: Jensen PS, editor; Hibbs ED, editor. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association; 1996. pp. 525–552. doi:10.1037/10196-020. [Google Scholar]
- Schreibman L, Whalen C. Stahmer AC. The use of video priming to reduce disruptive transition behavior in children with autism. Journal of Positive Behavior Interventions. 2000;2:3–11. doi:10.1177/109830070000200102. [Google Scholar]
- Siller M. Sigman M. The behaviours of parents of children with autism predict the subsequent development of their children's communication. Journal of Autism and Developmental Disorders. 2002;32(2):77–89. doi: 10.1023/a:1014884404276. doi:10.1023/A:1014884404276. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T. Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. doi:10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Manikam R, Winton ASW, Singh ANA, Singh J. Singh ADA. A mindfulness-based strategy for self-management of aggressive behavior in adolescents with autism. Research in Autism Spectrum Disorders. 2011;5(3):1153–1158. doi:10.1016/j.rasd.2010.12.012. [Google Scholar]
- Smith T. Outcome of early intervention for children with autism. Clinical Psychology: Science and Practice. 2006;6(1):33–49. . doi:10.1093/clipsy.6.1.33. [Google Scholar]
- Snyder CM. 2010. The effect of task difficulty on preschoolers' problem solving and emotion-regulation strategy use (Master's thesis). Retrieved from http://etd.lsu.edu/docs/available/etd-04122010-114839/unrestricted/Thesis_pdf.pdf.
- Sofronoff K, Attwood T. Hinton S. A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2005;46(11):1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. doi:10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. Levin I. A randomized controlled trial of a cognitive behavioural intervention for anger management in children diagnosed with Asperger syndrome. Journal of Autism and Developmental Disorders. 2007;37(7):1203–1214. doi: 10.1007/s10803-006-0262-3. doi:10.1007/s10803-006-0262-3. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Beaumont R. Weiss JA. Treating transdiagnostic processes in ASD: Going beyond anxiety. In: Ollendick TH, editor; Davis TE III, White SW, editors. Handbook of autism and anxiety. New York, NY: Springer; 2014. pp. 171–183. , & (Eds.), In ( [Google Scholar]
- Spek AA, van Ham NC. Nyklíček I. Mindfulness-based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Research in Developmental Disabilities. 2013;34(1):246–253. doi: 10.1016/j.ridd.2012.08.009. doi:10.1016/j.ridd.2012.08.009. [DOI] [PubMed] [Google Scholar]
- Spering M, Wagener D. Funke J. The role of emotions in complex problem-solving. Cognition and Emotion. 2005;19(8):1252–1261. doi:10.1080/02699930500304886. [Google Scholar]
- Szatmari P, Georgiades S, Duku E, Zwaigenbaum L, Goldberg J. Bennett T. Alexithymia in parents of children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2008;38(10):1859–1865. doi: 10.1007/s10803-008-0576-4. doi:10.1007/s10803-008-0576-4. [DOI] [PubMed] [Google Scholar]
- Tanaka JW, Wolf JM, Klaiman C, Koenig K, Cockburn J, Herlihy L. Schultz RT. The perception and identification of facial emotions in individuals with autism spectrum disorders using the Let's Face It! Emotion Skills Battery. Journal of Child Psychology and Psychiatry. 2012;53(12):1259–1267. doi: 10.1111/j.1469-7610.2012.02571.x. doi:10.1111/j.1469-7610.2012.02571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantum D. Psychological disorders in adolescents and adults with Asperger's syndrome. Autism. 2000;4(1):47–62. . doi:10.1177/1362361300004001004. [Google Scholar]
- Titov N, Dear BF, Johnston L, Lorian C, Zou J, Wootton B. Rapee RM. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: Randomized controlled trial. PLoS ONE. 2013;8(7):e62873. doi: 10.1371/journal.pone.0062873. doi:10.1371/journal.pone.0062873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totsika V, Hastings RP, Emerson E, Berridge DM. Lancaster GA. Behavior problems at 5 years of age and maternal mental health in autism and intellectual disability. Journal of Abnormal Child Psychology. 2011;39(8):1137–1147. doi: 10.1007/s10802-011-9534-2. doi:10.1007/s10802-011-9534-2. [DOI] [PubMed] [Google Scholar]
- Totsika V, Hastings RP, Emerson E, Lancaster GA. Berridge DM. A population-based investigation of behavioural and emotional problems and maternal mental health: Associations with autism spectrum disorder and intellectual disability. Journal of Child Psychology and Psychiatry. 2011;52(1):91–99. doi: 10.1111/j.1469-7610.2010.02295.x. doi:10.1111/j.1469-7610.2010.02295.x. [DOI] [PubMed] [Google Scholar]
- Trosper SE, Buzzella BA, Bennett SM. Ehrenreich JT. Emotion regulation in youth with emotion disorders: Implications for a unified treatment approach. Clinical Child and Family Psychology Review. 2009;12(3):234–254. doi: 10.1007/s10567-009-0043-6. doi:10.1007/s10567-009-0043-6. [DOI] [PubMed] [Google Scholar]
- Valiente C, Lemery-Chalfant K. Castro KS. Children's effortful control and academic competence: Mediation through school liking. Merrill-Palmer Quarterly. 2007;53(1):1–25. doi:10.1353/mpq.2007.0006. [Google Scholar]
- Valiente C, Lemery-Chalfant K, Swanson J. Reiser M. Prediction of children's academic competence from their effortful control, relationships, and classroom participation. Journal of Educational Psychology. 2008;100(1):67. doi: 10.1037/0022-0663.100.1.67. doi:10.1037/0022-0663.100.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valiente C, Swanson J. Lemery-Chalfant K. Kindergartners’ temperament, classroom engagement, and student-teacher relationship: Moderation by effortful control. Social Development. 2012;21(3):558–576. doi:10.1111/j.14679507.2011.00640.x. [Google Scholar]
- Vygotsky LS. Mind in society: The development of higher psychological processes. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- Watson LR. Following the child's lead: Mothers’ interactions with children with autism. Journal of Autism and Developmental Disorders. 1998;28(1):51–59. doi: 10.1023/a:1026063003289. . doi:10.1023/A:1026063003289. [DOI] [PubMed] [Google Scholar]
- Weersing VR, Rozenman MS, Maher-Bridge M. Campo JV. Anxiety, depression, and somatic distress: Developing a transdiagnostic internalizing toolbox for pediatric practice. Cognitive and Behavioral Practice. 2012;19(1):68–82. doi: 10.1016/j.cbpra.2011.06.002. doi:10.1016/j.cbpra.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ. Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of Child & Adolescent Psychopharmacology. 2005;15(3):477–496. doi: 10.1089/cap.2005.15.477. doi:10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- White SW, Ollendick T, Albano AM, Oswald D, Johnson C, Southam-Gerow MA. Scahill L. Randomized controlled trial: Multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(2):382–394. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Ollendick T, Scahill L, Oswald D. Albano AM. Preliminary efficacy of cognitive-behavioural treatment program for anxious youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(12):1652–1662. doi: 10.1007/s10803-009-0801-9. doi:10.1007/s10803-009-0801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams BT, Gray KM. Tonge BJ. Teaching emotion recognition skills to young children with autism: A randomised controlled trial of an emotion training programme. Journal of Child Psychology and Psychiatry. 2012;53(12):1268–1276. doi: 10.1111/j.1469-7610.2012.02593.x. doi:10.1111/j.1469-7610.2012.02593.x. [DOI] [PubMed] [Google Scholar]
- Williams D. Happé F. Representing intentions in self and other: Studies of autism and typical development. Developmental Science. 2010;13(2):307–319. doi: 10.1111/j.1467-7687.2009.00885.x. doi:10.1111/j.1467-7687.2009.00885.x. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Mathews A. MacLeod C. The emotional Stroop task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. doi:10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A. Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. doi:10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ. Gadow KD. Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Science and Practice. 2010;17(4):281–292. doi:10.1111/j.1468-2850.2010.01220.x. [Google Scholar]
- Yovel I. Mineka S. Emotion-congruent attentional biases: The perspective of hierarchical models of emotional disorders. Personality and Individual Differences. 2005;38(4):785–795. doi:10.1016/j.paid.2004.06.003. [Google Scholar]
- Zeman J. Shipman K. Influence of social context on children's affect regulation: A functionalist perspective. Journal of Nonverbal Behavior. 1998;22(3):141–165. doi:10.1023/A:1022900704563. [Google Scholar]
- Zeman J, Shipman K. Suveg C. Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):393–398. doi: 10.1207/S15374424JCCP3103_11. doi:10.1207/S15374424JCCP3103_11. [DOI] [PubMed] [Google Scholar]