Abstract
Background:
High concentrations of triglyceride-rich lipoproteins, and apolipoprotein B in newborns with low gestational age may increase the risk of cardiovascular diseases in the future. We investigated the lipid profile in term, late preterm and preterm Iranian infants.
Materials and Methods:
A total number of 99 term (gestational age ≥37 weeks), preterm (gestational age <34 weeks), and late preterm (34≤ gestational age <37 weeks) newborns were studied. Total cholesterol, low-density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol (HDL-C), and triglycerides, as well as apolipoproteins A and B were analyzed using auto analyzer.
Results:
Significant differences existed between cord blood concentrations of triglycerides, total cholesterol, and LDL-C in the term, late preterm and preterm infants (P < 0.05). The highest (61.69 mg/dl) and lowest (47.03 mg/dl) concentrations of triglycerides were documented in term and preterm newborns, respectively. Late preterm infants had the highest concentration of cord blood cholesterol. The lowest amount of cholesterol was found in term newborns (72.51 mg/dl). No significant difference existed in the mean of HDL-C and apolipoproteins in the studied groups (P > 0.05).
Conclusion:
In this study, the cord blood concentrations of cholesterol, triglycerides, and LDL-C were lower in term than in preterm and late preterm infants. This finding should be considered in infant nutrition and preventive measures.
Keywords: Cord blood, gestational age, lipoprotein, newborns
INTRODUCTION
Dyslipidemia may cause complications such as stroke, kidney failure, coronary heart disease, and atherosclerosis.[1] Concentrations of the cord blood lipoprotein subtypes are influenced by fetal malnutrition and prematurity.[2,3,4] High concentrations of triglyceride-rich lipoproteins, and apolipoprotein B in infants with a low gestational age; and increase of apo c-1 rich in high-density lipoprotein (HDL) with low birth weight are potential risk factors for cardiovascular disease in the future.[5,6,7]
It is suggested that the decreasing activity of the lipoprotein lipase, hepatic lipase and lecithin-cholesterol acyltransferase enzymes in preterm infants might lead to high concentrations of lipoproteins.[8]
A study in Spain[9] reported that the cord blood HDL-cholesterol (HDL-C) level was lower in premature than in term newborns, but very low-density lipoprotein (VLDL) levels were higher in preterm than in term newborns. In a study in Japan,[10] cord blood samples of preterm newborns had higher concentrations of VLDL, LDL-cholesterol (LDL-C), and HDL-C subclasses compared with their term counterparts.
Donegá et al. reported that the concentrations of total cholesterol, LDL-C, HDL-C, and apolipoprotein-B were higher in preterm- than in full-term newborns. Whereas, triglycerides was lower in preterm- than in full-term newborns.[11]
A previous study in Iran showed that the total cholesterol and HDL-C of female newborns were higher than in male newborns.[12]
Limited experience exists on the difference of the cord blood concentrations according to the gestational age.
The aim of this investigation is to compare the cord blood lipid concentration in term, late preterm and preterm newborns in a sample of Iranian neonates.
MATERIALS AND METHODS
This cross-sectional study was conducted in 2013 among 100 neonates in Isfahan, Iran. Neonates with a gestational age of ≥37 weeks were considered as term, those with gestational age of <34 weeks as preterm, and those with 34≤ gestational age <37 weeks, as late preterm neonates.[13] Newborns were selected by simple sampling from the maternity ward of Shaheed Beheshti Teaching Hospital, affiliated to Isfahan University of Medical Sciences in Isfahan, the second large city in Iran. All mothers were healthy, and their pregnancies were without complications. Immediately after delivery, 2 ml of cord blood was collected from the fetal part of the umbilical cord. Cord blood was allowed clot and then stored at −20°C until analysis in <1 month. Lipid profile and apolipoproteins A and B were analyzed in Milad Laboratory by autoanalyzer (Hitachi 911, Japan). Statistical Package for the Social Science version 20.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis using one-way analysis of variance.
RESULTS
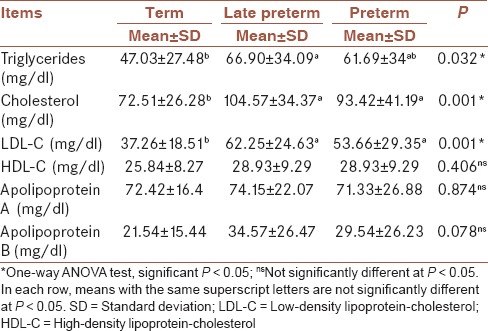
Cord blood concentrations of triglycerides, total cholesterol and LDL-C were significantly different in term, late preterm, and preterm newborns [Table 1]. Term infants had the highest level of triglycerides (47.03 mg/dl), whereas preterm infants had its lowest concentration (61.69 mg/dl). Our analysis showed that in each three groups under study, the difference of total cholesterol level was significant. Late preterm infants had the highest concentration of cholesterol in cord blood. The lowest amount of cholesterol content was documented in term infants (72.51 mg/dl). No significant difference existed in the mean level of HDL-C, apolipoprotein A and apolipoprotein B levels in the three studied groups (P > 0.05).
Table 1.
Comparison of the mean levels of cord blood lipids in the studied groups
DISCUSSION
The present study demonstrated that the term infants had the highest concentration of cord blood triglycerides. The highest amount of cholesterol in cord blood was documented in late preterm infants. In the total study group, no significant difference existed in the mean of HDL, apolipoprotein A and apolipoprotein B levels. Lipid profile is a marker of an underlying cardiovascular status, and direct correlation exists between the abnormalities in lipid profile and incidence of many chronic diseases. Among various factors theorized in the development of atherosclerosis, increased plasma levels of cholesterol and or triglycerides are considered to be of most important factors. Atherosclerosis begins early in life, and the studies conducted on cord blood lipid profile had inconsistent findings.
Some findings of the current study are not consistent with a previous study on cord blood cholesterol, which found higher cholesterol in preterm than in term newborns.[9,10,11] In another study, preterm infants had a high level of cholesterol concentrations.[14] In this investigation, we did not document significant difference in the mean cord blood level of HDL-C, apolipoprotein A and apolipoprotein B levels in the total study group. Consistent with another investigation, the current study indicated that differences in the gestational age do not affect cord blood HDL-C level.[14]
A previous study[15] showed that LDL-C concentrations decline from 30-33 to 42 weeks of gestation. Our findings also demonstrated that term newborns had lower cord blood LDL-C concentration than preterm and late preterm infants, however the differences were not significant.
Haridas and Acharya in their study concluded that preterm infant have higher triglycerides and total cholesterol levels, but statically significant difference was found only for total cholesterol.[16] Mathur et al. concluded that in preterm neonates, total cholesterol was significantly high.[17] Donegá et al., reported that total cholesterol, LDL-C, and HDL-C levels of cord blood were significantly higher in preterm infants; also the triglycerides content was lower in preterm neonates.[11] Pardo et al., found that total cholesterl, LDL-C, and HDL-C of cord blood were higher in preterm neonates compared with term neonates, with statically significant difference in total cholesterol and LDL-C levels, but the corresponding figure was not significant for HDL-C.[18]
It is suggested that decrease of lipoprotein lipase, hepatic lipase, and lecithin cholesterol acyltransferase enzymes activity in preterm newborns might increase lipoprotein concentrations in preterm than in term infants.[8]
In addition to genetic factors that are of major determinants of lipid levels,[19] fetal growth retardation might also establish a lifelong irreversible atherogenic profile, and the history of low birth weight,[20] or preterm birth[21] are associated with various risk factors including increase in apolipoprotein B levels.[22] In our study, higher levels of triglycerides, total-cholesterol, and LDL-C in preterm and late preterm infants could be explained by the fact that preterm newborns lack both hepatic carbohydrate and subcutaneous adipose stores. Increase in cord blood cholesterol level may reflect the metabolic adaptation to provide adequate energy, especially to vital organs like brain. Given the early life origins of adult diseases,[23] primordial and primary prevention should be emphasized.
Study limitations
The main limitation of our study is its cross-sectional nature. Future longitudinal studies with long-term follow-up are necessary to verify the clinical implications of the current findings.
CONCLUSION
The present study assumes that cord blood lipid profile differs according to the gestational age. These findings should be considered in early life nutrition and preventive measures.
AUTHOR'S CONTRIBUTION
All authors contributed in the study design and conduct, as well as in drafting and revising the manuscript. All authors approved the final version of the paper, and take the responsibility for its content.
ACKNOWLEDGMENT
This research was done with support of Isfahan University of Medical Sciences, the project number was 391021.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Betteridge J, Illingworth DR, Shepherd J. London: Arnold Press; 1999. Poproteins in health and disease; p. 1302. [Google Scholar]
- 2.Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: A summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006;118:1207–14. doi: 10.1542/peds.2006-0018. [DOI] [PubMed] [Google Scholar]
- 3.Gray RF, Indurkhya A, McCormick MC. Prevalence, stability, and predictors of clinically significant behavior problems in low birth weight children at 3, 5, and 8 years of age. Pediatrics. 2004;114:736–43. doi: 10.1542/peds.2003-1150-L. [DOI] [PubMed] [Google Scholar]
- 4.Meas T. Fetal origins of insulin resistance and the metabolic syndrome: A key role for adipose tissue? Diabetes Metab. 2010;36:11–20. doi: 10.1016/j.diabet.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Yonezawa R, Okada T, Kitamura T, Fujita H, Inami I, Makimoto M, et al. Very low-density lipoprotein in the cord blood of preterm neonates. Metabolism. 2009;58:704–7. doi: 10.1016/j.metabol.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Kwiterovich PO, Jr, Cockrill SL, Virgil DG, Garrett ES, Otvos J, Knight-Gibson C, et al. A large high-density lipoprotein enriched in apolipoprotein C-I: A novel biochemical marker in infants of lower birth weight and younger gestational age. JAMA. 2005;293:1891–9. doi: 10.1001/jama.293.15.1891. [DOI] [PubMed] [Google Scholar]
- 7.Radunovic N, Kuczynski E, Rosen T, Dukanac J, Petkovic S, Lockwood CJ. Plasma apolipoprotein A-I and B concentrations in growth-retarded fetuses: A link between low birth weight and adult atherosclerosis. J Clin Endocrinol Metab. 2000;85:85–8. doi: 10.1210/jcem.85.1.6243. [DOI] [PubMed] [Google Scholar]
- 8.Hamosh M. Lipid metabolism in premature infants. Biol Neonate. 1987;52:50–64. doi: 10.1159/000242739. [DOI] [PubMed] [Google Scholar]
- 9.Morillas JM, Moltó L, Robles R, Gil A, Sánchez-Pozo A. Lipoproteins in preterm and small-for-gestational-age infants during the first week of life. Acta Paediatr. 1992;81:774–8. doi: 10.1111/j.1651-2227.1992.tb12101.x. [DOI] [PubMed] [Google Scholar]
- 10.Nagano N, Okada T, Yonezawa R, Yoshikawa K, Fujita H, Usukura Y, et al. Early postnatal changes of lipoprotein subclass profile in late preterm infants. Clin Chim Acta. 2012;413:109–12. doi: 10.1016/j.cca.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Donegá S, Oba J, Maranhão RC. Concentration of serum lipids and apolipoprotein B in newborns. Arq Bras Cardiol. 2006;86:419–24. doi: 10.1590/s0066-782x2006000600003. [DOI] [PubMed] [Google Scholar]
- 12.Badiee Z, Kelishadi R. Cord blood lipid profile in a population of Iranian term newborns. Pediatr Cardiol. 2008;29:574–9. doi: 10.1007/s00246-007-9149-0. [DOI] [PubMed] [Google Scholar]
- 13.Fowlie PW, McGuire W. Immediate care of the preterm infant. BMJ. 2004;329:845–8. doi: 10.1136/bmj.329.7470.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tohmaze RM. Cord blood lipid profile in premature, near-term and term newborn infants. Iran J Neonatol. 2014;5:8–10. [Google Scholar]
- 15.Forte TM, Genzel-Boroviczeny O, Austin MA, Kao LC, Scott C, Albers JJ, et al. Effect of total parenteral nutrition with intravenous fat on lipids and high density lipoprotein heterogeneity in neonates. JPEN J Parenter Enteral Nutr. 1989;13:490–500. doi: 10.1177/0148607189013005490. [DOI] [PubMed] [Google Scholar]
- 16.Haridas N, Acharya PT. Serum lipid status in neonates. Indian Pediatr. 1984;21:327–34. [PubMed] [Google Scholar]
- 17.Mathur PP, Prasad R, Jain SK, Pandey DN, Singh SP. Cord blood cholesterol in term and preterm new borns. Indian Pediatr. 1986;23:103–6. [PubMed] [Google Scholar]
- 18.Pardo IM, Geloneze B, Tambascia MA, Barros-Filho AA. Atherogenic lipid profile of Brazilian near-term newborns. Braz J Med Biol Res. 2005;38:755–60. doi: 10.1590/s0100-879x2005000500013. [DOI] [PubMed] [Google Scholar]
- 19.Kelishadi R, Haghjooy Javanmard S, Tajadini MH, Mansourian M, Motlagh ME, Ardalan G, et al. Genetic association with low concentrations of high density lipoprotein-cholesterol in a pediatric population of the Middle East and North Africa: The CASPIAN-III study. Atherosclerosis. 2014;237:273–78. doi: 10.1016/j.atherosclerosis.2014.08.043. [DOI] [PubMed] [Google Scholar]
- 20.Irving RJ, Belton NR, Elton RA, Walker BR. Adult cardiovascular risk factors in premature babies. Lancet. 2000;355:2135–6. doi: 10.1016/S0140-6736(00)02384-9. [DOI] [PubMed] [Google Scholar]
- 21.Lindsay RS, Dabelea D, Roumain J, Hanson RL, Bennett PH, Knowler WC. Type 2 diabetes and low birth weight: The role of paternal inheritance in the association of low birth weight and diabetes. Diabetes. 2000;49:445–9. doi: 10.2337/diabetes.49.3.445. [DOI] [PubMed] [Google Scholar]
- 22.Kharb S, Kaur R, Singh V, Sangwan K. Birth weight, cord blood lipoprotein and apolipoprotein levels in Indian newborns. Int J Prev Med. 2010;1:29–33. [PMC free article] [PubMed] [Google Scholar]
- 23.Kelishadi R, Poursafa P. A review on the genetic, environmental, and lifestyle aspects of the early-life origins of cardiovascular disease. Curr Probl Pediatr Adolesc Health Care. 2014;44:54–72. doi: 10.1016/j.cppeds.2013.12.005. [DOI] [PubMed] [Google Scholar]


