Abstract
Persistent Mullerian duct syndrome (PMDS) is a rare form of Disorder of sex development in which Mullerian duct derivatives (fallopian tubes, uterus and the proximal vagina) are present in an otherwise normally differentiated 46 XY male. In the majority of cases, PMDS is a surprise finding either during orchidopexy or during inguinal hernia repair. We report a case of 4 year child with female type (Type III) PMDS. We are discussing the presentation, management and review of the literature.
Keywords: Anti Mullerian hormone, cryptorchidism, hernia uteri inguinale, persistent Mullerian duct syndrome
INTRODUCTION
Persistent Mullerian duct syndrome (PMDS), previously also known as hernia uteri inguinale is a relatively rare variety of Disorder of sex development. Patients are phenotypically male and have 46 XY karyotype. As the name suggests Mullerian remnants (fallopian tubes [F. T.], uterus and the proximal vagina) are present in an otherwise normal male. The rudimentary vagina ends by opening into the prostatic utricle. Anatomically PMDS [Table 1] is divided into three categories.[1] In our case, the PMDS variety was of female type with bilateral cryptorchid testis, uterus and F. T.
Table 1.
Anatomical classification of PMDS
CASE REPORT
This was a case of a 4-year-old child (reared as male) presented with bilateral undescended testis. On clinical examination, the phallus was normal and bilateral testes were not palpable. The child underwent laparoscopy for non-palpable testis. On laparoscopy, bilateral gonads were present at the ovarian position and there was a midline uterus present. We could identify vas like structure and vessels along with F. T. entering into the gonads. Due to discrepancies in gonadal morphology and the internal genitalia, a biopsy was taken. Subsequently the condition was explained to the parents and karyotyping was done which was suggestive of 46 XY male karyotype. The human chorionic gonadotropin (HCG) stimulation test was performed, which was suggestive of functional testicular tissue. The gonadal biopsy was suggestive of normal testicular tissue. All these findings confirmed the diagnosis of PMDS. Subsequently the child underwent a second surgery through a pfannenstiel incision [Figure 1] and excision of Mullerian structures (uterus, F. T. and proximal vagina) was performed [Figure 2]. The distal most part of the vagina was very close to the both vas deferens [Figure 1] so could not excised completely, we opened the vaginal cavity [Figure 3] and strip of the mucosa with preservation of the bilateral vas along with its vascular supply. After excision of the Mullerian structures, we obtained sufficient length to perform bilateral orchidopexy in subdartos pouch. The child was under follow-up.
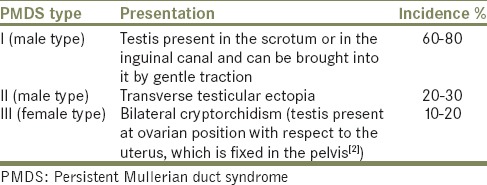
Figure 1.

Midline rudimentary uterus (black arrow) with fallopian tube on both sides. Both gonad at the two ends, vas can be identified (indicated by forceps tip) along the vascular pedicle. Line diagram (inset) showing the anatomical details of the case. (u = uterus, v = vagina, F. T. = fallopian tube, T = testis, dotted line showing vas deferens)
Figure 2.
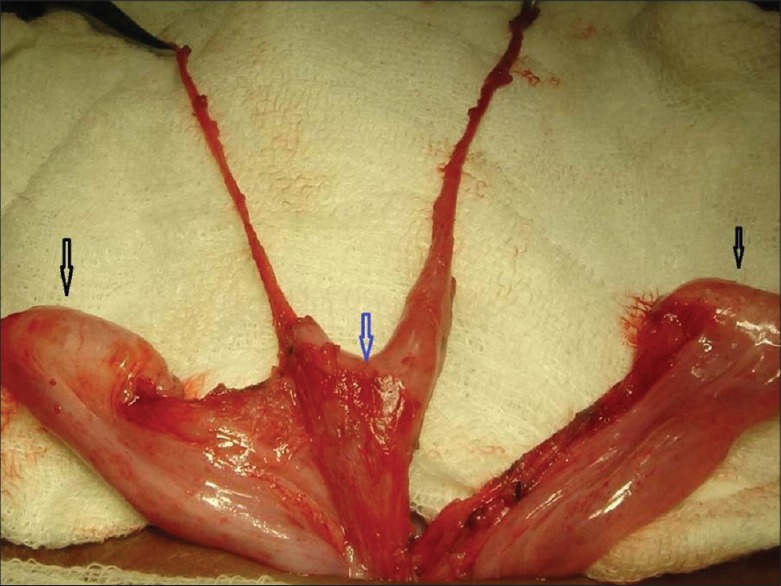
Excised uterus (blue arrow) along with the bilateral fallopian tube. Both testis separated (black arrows) from the Mullerian remnants
Figure 3.
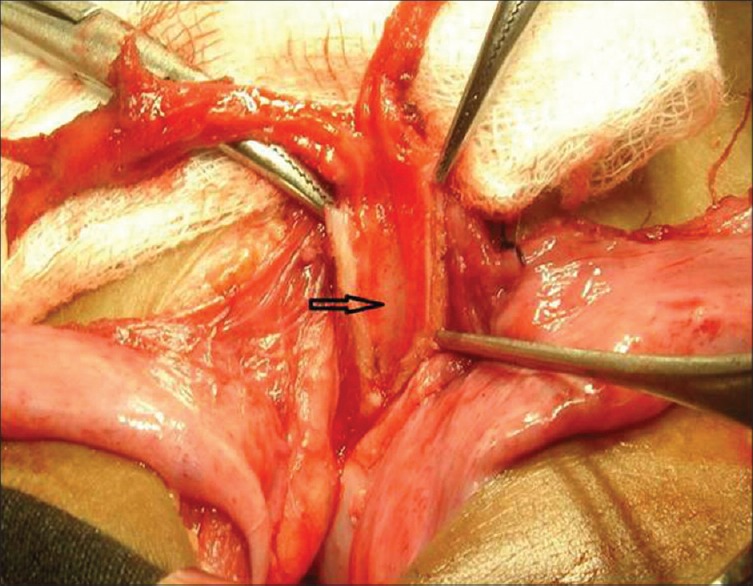
Distal most part of the rudimentary vagina, the vaginal cavity opened (black arrow) to remove the mucosa
DISCUSSION
The cause of PMDS is the absence of Anti Mullerian hormone (AMH), abnormal AMH or defects in its receptor.[3] The AMH (also known as Mullerian inhibiting substance) is a glycoprotein secreted by fetal Sertoli cells. AMH does not have a direct role in the descent of the testis, but in case of bilateral abdominal testes, Mullerian remnants prevent the mobilization of the testes. The human gene for AMH has been mapped on chromosome 19. In PMDS the testes are histologically normal and the overall incidence of malignant transformation in the testis is similar (18%) to the rate in otherwise intra-abdominal testis.[4]
Previously, it was advised that there is no need to remove the Mullerian structure (to preserve the vas and its vasculature) but subsequent malignancy of the Mullerian remnants has been reported and so at present, excision of these structures is recommended.[5,6,7,8] Complete excision of the Mullerian duct remnants can result in damage to the integrity or vascularity of the vas deferens because the vas deferens is usually found to be intimately adhering to the lateral walls of the uterus, F. T. and the vagina.[9]
In our case, for distal most part of the vagina we could only strip of the mucosa because of the close proximity with vas. As reported malignancies of Mullerian remnants originate from its mucosa, the removal of the mucosal lining should be sufficient to reduce the risk of malignancy. Retained Mullerian remnants also known to cause recurrent urinary tract infections (UTI), stones and voiding disturbances. Removal of the vaginal mucosa would obliterate the cavity also and so decrease the risk of UTI and stone formation.
For optimum management surgeon should be aware of this entity and recognition during operation (as most of the time, not suspected preoperatively) is most important. Once suspected, the confirmation of diagnosis is done with testicular biopsies and chromosomal studies. Assessment of testicular response to HCG stimulation is not essential in every case but verify the existence of functional testicular tissue. Subsequently the patient requires excision of Mullerian structure with bilateral orchidopexy or bilateral orchidectomy/unilateral orchidectomy and another side orchidopexy depend upon the age of the patient, HCG stimulation result and histology of gonad. In these patients generally virilisation remains unaffected and also normal development of external genitalia with secondary sexual characteristics but infertility is common because most patients have azoospermia.[7]
CONCLUSION
For proper management of PMDS, the excision of Mullerian derivatives is important at all ages to prevent malignant transformation. The management of testis (orchidopexy or orchidectomy) depends upon the age, presence of functional testicular tissue and histology of gonads.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Dekker HM, de Jong IJ, Sanders J, Wolf RF. Persistent Müllerian duct syndrome. Radiographics. 2003;23:309–13. doi: 10.1148/rg.232025141. [DOI] [PubMed] [Google Scholar]
- 2.Clemente A, Macchi V, Berretta M, Morra A. Female form of persistent müllerian duct syndrome: MDCT findings. Clin Imaging. 2008;32:314–7. doi: 10.1016/j.clinimag.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Rey RA, Grinspon RP. Normal male sexual differentiation and aetiology of disorders of sex development. Best Pract Res Clin Endocrinol Metab. 2011;25:221–38. doi: 10.1016/j.beem.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Aboutorabi R, Feiz Zadeh B, Rajabian R. Gynecomastia secondary to choriocarcinoma in a man with persistant Mullerian duct. Int J Endocrinol Metab. 2005;3:140–2. [Google Scholar]
- 5.Berkmen F. Persistent müllerian duct syndrome with or without transverse testicular ectopia and testis tumours. Br J Urol. 1997;79:122–6. doi: 10.1046/j.1464-410x.1997.27226.x. [DOI] [PubMed] [Google Scholar]
- 6.Vandersteen DR, Chaumeton AK, Ireland K, Tank ES. Surgical management of persistent müllerian duct syndrome. Urology. 1997;49:941–5. doi: 10.1016/s0090-4295(97)00104-0. [DOI] [PubMed] [Google Scholar]
- 7.Romero FR, Fucs M, Castro MG, Garcia CR, Fernandes Rde C, Perez MD. Adenocarcinoma of persistent müllerian duct remnants: Case report and differential diagnosis. Urology. 2005;66:194–5. doi: 10.1016/j.urology.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Manjunath BG, Shenoy VG, Raj P. Persistent müllerian duct syndrome: How to deal with the müllerian duct remnants - A review. Indian J Surg. 2010;72:16–9. doi: 10.1007/s12262-010-0003-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu HC, Chen JH, Lu HF, Shen WC. Persistent müllerian duct syndrome wtih seminoma: CT findings. AJR Am J Roentgenol. 2000;174:102–4. doi: 10.2214/ajr.174.1.1740102. [DOI] [PubMed] [Google Scholar]


