Abstract
Artificial urinary sphincters (AUSs) are commonly used after radical prostatectomy for those who are incontinent of urine. However, they are associated with complications, the most common being reservoir uprising or migration. We present a unique case of occlusive external iliac and femoral vein obstruction by the AUS reservoir causing thrombosis. Deflation of the reservoir and anticoagulation has, thus far, not been successful at decreasing thrombus burden. We present this case as a rare, but significant surgical complication; explore the risk factors that may have contributed, and other potential endovascular therapies to address this previously unreported AUS complication.
Keywords: Artificial urinary sphincter, deep vein thrombosis, radical prostatectomy
INTRODUCTION
Urinary incontinence is common after radical retropubic prostatectomy, at a rate of approximately 5%, dependent on various factors.[1,2] Treatments include conservative physiotherapy to minimally invasive surgical techniques, which include urethral slings and artificial urinary sphincter (AUS) insertion. Although AUSs have proven successful and are growing in popularity, they are associated with complications including revision, replacement or explantations. Wang et al.[3] have indicated that more than half of AUS recipients require additional surgery within the first 2 years. The most common reason for surgical revision was reservoir uprising or migration, with a rare case of intravesical migration of the reservoir reported.[4] Other reasons for revision include recurrent incontinence (55%), mechanical malfunction (22%) and infection/erosion (18%).[3] We present a previously unreported case of deep vein thrombosis (DVT) caused by AUS reservoir migration and resultant external iliac vein compression.
CASE REPORT
We present a case of a 55-year-old man who suffered occlusive external iliac and femoral vein thrombosis secondary to AMS-800 AUS insertion. The reservoir component was found to be 100% occlusive of the vein, causing a 12 cm DVT below the groin crease.
Our patient was electively admitted for the insertion of AUS on a background of radical prostatectomy and adjuvant radiotherapy 7 years prior. A previous urethral sling procedure had been unsuccessful. The AUS reservoir was placed in the dissected retropubic space of Retzius. The dissection was difficult given his radiation history and subsequent scarring. He had an uneventful postoperative course. 40 mg of enoxaparin was given daily as DVT prophylaxis during his inpatient stay, in addition to anti-embolism compression stockings and early mobilization. He also received prophylactic intravenous antibiotics, which were continued orally on discharge. He was discharged 3 days postoperatively.
Two days later, he represented to the emergency department with right lower limb swelling and pain that limited mobility. Ultrasound confirmed extensive, completely occlusive DVT starting from the inactivated (full) reservoir, extending 12 cm distally in the external iliac and femoral vein [Figure 1]. He was therapeutically anticoagulated with enoxaparin and warfarin was commenced.
Figure 1.
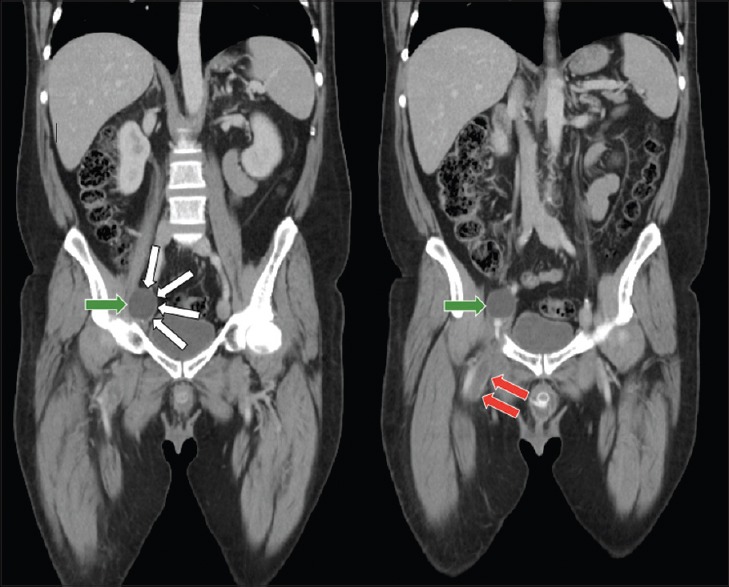
Computed tomography abdomen/pelvis showing inflated reservoir compressing external iliac vein and resultant occlusive thrombus distal to reservoir. Green arrows show the reservoir; white arrows on the left show external iliac vein wrapped around the reservoir; red arrows on the right show thrombus filled distal external iliac vein
After 3 weeks of anticoagulation, a repeat ultrasound showed no change in the thrombus size. After discussion with the interventional radiologist and vascular surgeons, the decision was made to insert an inferior vena cava filter, reverse anticoagulation, and then return to theater to remove the reservoir. However, intra-operatively, the external iliac vein was found wrapped tightly around the reservoir and thus it was unable to be removed safely. The reservoir was disconnected from the system, emptied of fluid, and clipped on negative pressure. A new reservoir was placed in the anterior abdominal wall superior to the rectus sheath on the ipsilateral side.
Postoperatively, the computed tomography venogram showed ongoing obstruction. The external iliac vein remained compressed by a fluid filled pseudo-capsule at the site of initial reservoir placement [Figure 2]. Warfarin anticoagulation was recommenced and a grade two graduated compression stocking was fitted in an attempt to prevent postthrombotic syndrome (PTS).
Figure 2.
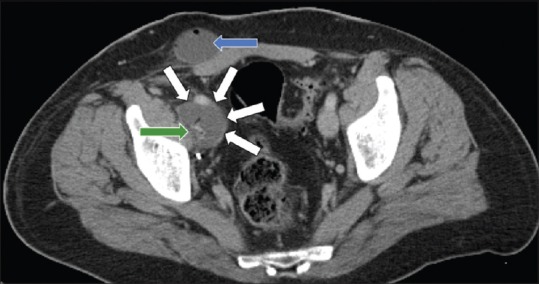
Computed tomography abdomen/pelvis after return to theatre. Green arrow shows the deflated initial reservoir; white arrows show the external iliac vein, still wrapped around fluid filled cystic structure; blue arrow shows the placement of new subcutaneous reservoir
Ten weeks post insertion of the original AUS, activation of the new sphincter was successful. It continues to operate satisfactorily 6 months later, although DVT remains occlusive of the external iliac vein. Prevention of PTS, thus far, has been successful. He is currently using the AUS successfully, and is fully continent of urine.
DISCUSSION
To the best of our knowledge, the complication described herein has not been previously reported in the literature. This case highlights the difficulties associated with deep reservoir insertion, especially with our patient's risk factor of irradiation. Interestingly, while radiation predisposes to a higher complication and revision risk, it does not have adverse long-term continence outcomes.[5]
The time frame of the return to surgery may have contributed to the formation of the pseudo-capsule that continues to compress the external iliac vein.
Morey et al.[6] described safe sub-muscular positioning of reservoir balloons between the transversalis fascia and rectus abdominus. Our patient can feel the new reservoir under his subcutaneous fat, but does not cause any discomfort.
The CaVenT study[7] describes the use of catheter directed lysis in iliofemoral thrombosis and has shown significant reduction in clot burden, DVT recurrence and rates of PTS at 24 months. Although early, our patient remains PTS free. However, a follow-up study has shown adversely effected quality of life if PTS does develop.[8] While the mechanical obstruction as a cause for thrombus, even after the deflation of the reservoir, may have prevented effective catheter directed thrombolysis (CDT), this should be considered as an alternative therapeutic option.
Combining CDT with percutaneous mechanical thrombectomy (PMT) ± stent placement is another option. This approach has been shown to be safe and effective in removing acute thrombus,[5,9] although long-term data regarding the development of PTS is lacking. Igari et al.[10] published a case series of successful mechanical thrombectomy and stenting for DVT secondary to (congential) mechanical obstruction. The ATTRACT multi-centre RCT, currently underway, has been designed to compare treatment of acute DVT using all mechanical thrombectomy devices (including use of stents with catheter directed lysis) with standard therapy. This will hopefully provide useful and definitive data regarding the merits of combined endovascular therapies in reducing the risk of PTS.
This is a clinically challenging complication of AUS not previously reported. Our patient was in the high-risk category with previous irradiation and failed urethral sling. In such cases, it would be worthwhile considering sub-muscular or subcutaneous reservoir placement, avoiding difficult and unnecessary dissection. A multidisciplinary approach to such complex cases is vital to optimise patient outcomes. This patient continues to undergo surveillance to monitor thrombus occlusion and development of PTS.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Nam RK, Herschorn S, Loblaw DA, Liu Y, Klotz LH, Carr LK, et al. Population based study of long-term rates of surgery for urinary incontinence after radical prostatectomy for prostate cancer. J Urol. 2012;188:502–6. doi: 10.1016/j.juro.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Eastham JA, Kattan MW, Rogers E, Goad JR, Ohori M, Boone TB, et al. Risk factors for urinary incontinence after radical prostatectomy. J Urol. 1996;156:1707–13. [PubMed] [Google Scholar]
- 3.Wang R, McGuire EJ, He C, Faerber GJ, Latini JM. Long-term outcomes after primary failures of artificial urinary sphincter implantation. Urology. 2012;79:922–8. doi: 10.1016/j.urology.2011.11.051. [DOI] [PubMed] [Google Scholar]
- 4.Bartoletti R, Gacci M, Travaglini F, Sarti E, Selli C. Intravesical migration of AMS 800 artificial urinary sphincter and stone formation in a patient who underwent radical prostatectomy. Urol Int. 2000;64:167–8. doi: 10.1159/000030521. [DOI] [PubMed] [Google Scholar]
- 5.Vedantham S, Vesely TM, Sicard GA, Brown D, Rubin B, Sanchez LA, et al. Pharmacomechanical thrombolysis and early stent placement for iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2004;15:565–74. doi: 10.1097/01.rvi.0000127894.00553.02. [DOI] [PubMed] [Google Scholar]
- 6.Morey AF, Cefalu CA, Hudak SJ. High submuscular placement of urologic prosthetic balloons and reservoirs via transscrotal approach. J Sex Med. 2013;10:603–10. doi: 10.1111/jsm.12000. [DOI] [PubMed] [Google Scholar]
- 7.Enden T, Haig Y, Kløw NE, Slagsvold CE, Sandvik L, Ghanima W, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): A randomised controlled trial. Lancet. 2012;379:31–8. doi: 10.1016/S0140-6736(11)61753-4. [DOI] [PubMed] [Google Scholar]
- 8.Enden T, Wik HS, Kvam AK, Haig Y, Kløw NE, Sandset PM. Health-related quality of life after catheter-directed thrombolysis for deep vein thrombosis: secondary outcomes of the randomised, non-blinded, parallel-group CaVenT study. BMJ Open. 2013;3:e002984. doi: 10.1136/bmjopen-2013-002984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meissner MH, Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, et al. Early thrombus removal strategies for acute deep venous thrombosis: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2012;55:1449–62. doi: 10.1016/j.jvs.2011.12.081. [DOI] [PubMed] [Google Scholar]
- 10.Igari K, Kudo T, Toyofuku T, Jibiki M, Inoue Y. Surgical thrombectomy and simultaneous stenting for deep venous thrombosis caused by iliac vein compression syndrome (May-Thurner Syndrome) Ann Thorac Cardiovasc Surg. 2013 Nov 27;:13–00213. doi: 10.5761/atcs.oa.13-00213. doi: 10.5761/atcs.oa. [DOI] [PubMed] [Google Scholar]


