Abstract
Objectives:
To assess the long term complications of JJ stent, the management of complications and the role of endoscopic approach to manage these complications.
Materials and Methods:
Nineteen patients with indwelling JJ stent for a duration of more than 6 months were included in this study. Patients were assessed with X-ray KUB, USG KUB, blood urea, creatinine and DTPA renogram. Data were analyzed by Microsoft excel 2007.
Results:
Out of 19 patients 12 (63.16%) were male and 7 (36.84%) were female. The mean age was 39.78 ± 13.69 years., Mean duration for which the stent was in situ was 29.56 months. The most common complication was broken stent, in 11 cases (57.89%). Other complications were migration in 5 (26.32%), encrustation in 2 (10.52%) and 1 case of (5.26%) stone formation. Eighteen cases were managed by endoscopic approaches. A total of 22 procedures were performed to treat the complications. Eleven cases were managed by a single procedure and 8 patients required multiple procedures. All were managed successfully with no death reported. Post-operative complications were seen in eight cases (42.11%).
Conclusions:
JJ stent related long-term complications are not uncommon and are usually seen after 6 months of indwelling time. Endourological procedure should be the initial approach with a high success rate. Coordinated use multimodality and technology helps in management of difficult cases. Open surgery is rarely required. Prevention of the complication by judicious use and early removal is the cornerstone.
Keywords: Complication, JJ stent, management, prevention
INTRODUCTION
JJ stent is widely used in urological practice. It was first described in 1967 by Zimskind et al.[1] Ureteric stents are not complication free. Stent related complications are primarily mechanical; including stent migration, encrustation, stone formation and fragmentation. Stents act as foreign bodes and may cause urinary tract infection, pyonephrosis that may lead to nonfunctioning kidney. Therefore, ureteral stent should be removed as early as possible after it serves its purpose or changed frequently as per the need to reduce stent related complication and morbidity. Managing complication itself has its own inherent consequences and that led understand urologist to prevent it by timely removal or change of the JJ stent. We studied the complications related to JJ stent, the possible etiologies, treatment options, role of endourological procedures and prevention of such problems. Our objective is to assess the long term complications and to assess the role of endoscopic approach to manage the complications. It will help in understanding the importance of prevention of complication by judicious use of JJ stent.
MATERIAL AND METHODS
This is a retrospective study which was conducted in Dept of Urology, IPGMER and SSKM Hospital, a tertiary centre of West Bengal, India from January 2008 to June 2013. Nineteen patients referred to our institution with more than 6 months of JJ stent placement were included in this study. We performed a plain X-ray KUB, USG KUB, blood urea, creatinine, and DTPA renogram if hydronephrosis or raised urea, creatinine was found. Data were collected from departmental register. Analysis was done by Microsoft office excels 2007.
RESULTS
Out of the 19 patients 12 (63.16%) were male and 7 (36.84%) were female. Table 1 summarizes the clinical parameters of the patients. The mean age was 39.9 years, with a range 10-58 years. Mean duration of the stent in situ was 29.89 months ranging from 7 months to 156 months. The most common complication was broken stent in 11 (57.89%). Other complications were migration in 5 (26.32%), encrustation in 2 (10.52%) and 1 case of (5.26%) stone formation. Eighteen 18 (94.74%) cases were managed by endoscopic approaches and only 1 case require open procedure. In the later case, the forgotten JJ stent fragmented and migrated down with knotting formation causing obstruction of right ureter and had to resorted open ureterotomy as attempt of ureteroscopic removal failed [Figure 1]. A total of 22 procedures were performed to treat the complications. In 57.89% (n = 11) cases single procedure was sufficient to effectively manage the complications, and 42.11% (n = 8) required multiple procedures. Cystoscopic removal of fragmented stent from the bladder was done in 9 cases, ureteroscopy was done in six cases for ureteric fragments of stent or ureteric migration of stent, ESWL in two encrusted stent followed by cystoscopic removal of those stents [Figure 2], and two cases of fragmented stent with stone formation in kidney removed by PCNL [Figure 3]. Antegrade removal of retained fragment in the pelvis or upper ureter was done in two cases. In one of them as there were reimplanted ureters for vesicoureteric reflux, the attempt of ureteroscopy was failed and upper fragment of stent removed through percutaneous nephrostomy [Figure 4]. All were managed successfully with no death reported. Although post-operative complications were seen in eight cases (42.11%). Infections were most common and was seen in 62.5% (n = 5). Sepsis was seen in 1 case.
Table 1.
Patients characteristics
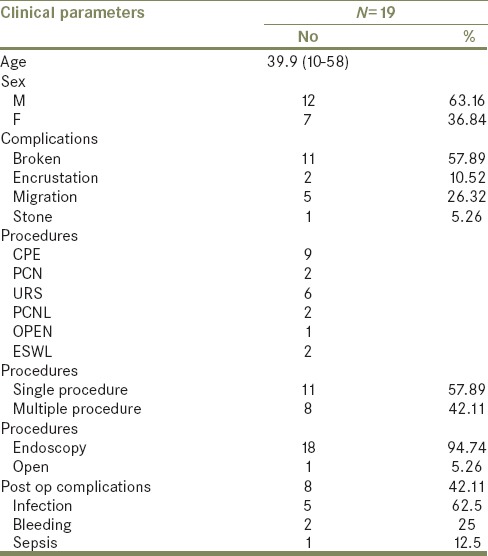
Figure 1.

Stent fragmented and migrated down with knotting causing obstruction of the right upper ureter
Figure 2.

Left over stent in patient with stone former for 2 years with encrustation
Figure 3.

Stone formation in retained small fragment of JJ stent for 3 years
Figure 4.

Forgotten bilateral stents for 13 years with fragmentation and migration
DISCUSSION
JJ stent is commonly used in urological practice since its first introduction. It is usually kept for (4-6 weeks) short term period to help in the healing of ureter, drainage of urine and prevent narrowing during healing. Short term use of JJ stent associated with short lived mild complications, whereas long term complications are more severe, particularly when it is placed for more than 6 months duration. Although Ideal stent should have many properties, with low complication rate and should not cause irritative symptoms, it is yet not be possible to manufacture.[2] Most common stent related complication is “stent syndrome”.[3] It is a constellation of clinical symptoms: Flank pain, frequency, urgency, suprapubic discomfort and sometime with hematuria or incontinence. Stent syndrome is primarily due to physical characteristics of stent and the improper size selection. Stent acts as a foreign body that irritates the ureteral and bladder wall. Extra length or coil may impinge on the trigone causing irritative voiding symptoms, hematuria or suprapubic pain. Ureteral peristalsis against the stent may cause flank pain or uereteric colic.[3,4] Although it is short lived but may cause of high morbidity in stented patients. Several tools have been described to assess the stent syndrome (International Prostatic Symptoms Score, IPSS; The Ureteral Stent Symptom Questionnaire, USSQ).[4,5,6] Although selection of the proper stent and the proper size is the prerequisite to reduce the complication, alpha1-blockers for treating these symptoms has been used with good results.[6]
Long-term complications are associated with prolonged indwelling times. Some time forgotten or overlooked stent may jeopardize the function of the kidney. With the passage of time all stents lose tensile strength, cracks are started at the holes resulting in fracture of the stents.[7] Zisman et al. found a decreased elongation at break of the retrieved polyurethane stents, and hypothesized that it is due to the accelerated aging process of stent material.[8] Although broken stent is a less commonly reported,[3] it is most common complication seen in our series. We found 57.89% cases with broken JJ stent. Breakage occurs in those who had JJ stent for long duration ranging from 15 to 156 months. In contrast, Damiano et al., found a relative lower incidence of fracture stent, only 1.3%.[9] Similar result was (4.79%) also shown by Ikram Ullah et al.[10] Monga et al. has shown a higher rate of fragmented JJ stent in their series. He counted 45% fragmented and another 14% fragmented and calcified. Mean duration of JJ stent was 22.7 months in their series.[11] Although broken JJ stent is relatively less common in most reported series, we found more than 50% presented with fragmented stent. It may be due to prolonged indwelling time (42.73 month) and also heterogeneity of JJ stent used in our area. Since all the cases were referred to our institution, the make and design of these stents were not known. It is seen that different types of JJ stent and of different manufacturer are being used in this eastern part of India. However, the definite reason of fragmentation is unclear. Although it does impact on rate and the type of complication. Silicone stent is resistant to biofilm formation and encrustation is less likely. Because of its softness and elasticity, patient feels more comfortable. On the other hand, polyurethane stents are rigid, easy manageable during placement but cause patient discomfort and may cause ureteral erosion.
Stent migration is a recognized complication. It is related to JJ stent design and faulty technique of insertion. Double pigtail stents are less likely to migrate as opposed to J loop stent. Migration can occur either way but upward migration is more common.[3] Upward migration is primarily due to placement of stent too short for the ureter.[12,13] Other causes of migration are renal ureteric dynamics, peristalsis and incorrect size selection.[14] The incidence of stent migration in our study is much higher than it is reported. Damiano et al. reported stent migration 9.5%.[9] We found a high incidence of 26.32% with mean duration was 9 months. Nawaz et al. and Ikram Ullah et al. also reported low incidence of stent migration at rate of 3.5% and 6.84%, respectively.[10] The high incidence in our study population possibly due to incorrect positioning and improper size selection. This complication can be avoided by pulling the stent cystoscopicaly keeping the full loop into the bladder[3] and stent should be in the pelvis not into the calyx.[15]
Stone encrustation is another problem in long term use. Polyurethane stent are more prone to encrustation. Encrustation is more common where stent use for stone disease, but it may also occur due to biofilm formation by the bacteria. Because of their rigidity poly urethane stents tend to encourage stasis with formation of encrustation. These encrustations consist mainly of calcium oxalate, calcium phosphate and ammonium magnesium phosphate.[16] Risk factors are chronic recurrent stone formers with a lithogenic history, uricosuria, chronic renal failure, congenital anomalies, urinary tract infection, stasis, dehydration and long indwelling times.[14] El-Faqih et al. reported stent encrustation rate increases with indwelling time and it is 9.2% for an indwelling time of less than 6 weeks to 47.5% at 6 to 12 weeks to 76.3% at more than 12 weeks.[17] We found only 2 (10.52%) of our study patient presented with this complication. In both the cases JJ stent were used for stone disease. Although others reported higher incidence rate, ranging from 10.5 to 15%.[10] It is seen that Silicone stent is more resistant to biofilm formation and so encrustation is less likely. Stent replacement prior to the time of expected encrustation is the only effective method of preventing encrustation.
Stone formation in a left over stent or fragment is also a common complication. Stone formation primarily seen in patients who are increase risk for stone formation and also with long indwelling time. Dehydration, stent blockage, urinary tract infection, chronic renal failure may also contribute stone formation. We found 1 case, where stone formed in small retained fragment of JJ stent after 36 months.
Management of complicated stents requires coordinated use of medical, lithotripsy and endourological techniques or open surgery. JJ stent related complications are primarily managed by endoscopic procedure with a high success rate. PCNL and URS are often necessary in cases of encrusted stent or stone formation over JJ stent. Open or laparoscopic procedure is only required if endoscopic procedure is failed. Nephrectomy is resorted to cases with non-functioning kidney. 94.74% of our cases were managed endoscopically with 57.89% success rate by single procedure and requiring multiple procedures in rest of the cases (42.11%). Open procedure was required in one case following failed attempted URS, where there was fragmentation with knotting of stent in ureter. Rabani has shown similar result.[18]
Although successful management of these complications done by endourological means in majority of cases with minimal complications, the best treatment would be prevention from this complication. It can easily be done by recognizing the fact that basic factor is forgotten or long term placement of JJ stent. So it is always advisable not to use JJ stent when unnecessary, and to remove or replace at earliest.
The following measures can be adopted to increase the compliance of the patient:[14]
Counseling of the patient about JJ stent and its potential complication if left indwelling for a prolonged interval
Selection of the appropriate stent size
Giving Post procedure X-ray to the patient to show the stent left in the body
Maintaining log of the patients with JJ stent to ensure timely replace or removal[19]
Further imaging was necessary both medically and legally to exclude a retained stent or part of a stent.
CONCLUSION
Serious complication of JJ stent is related to indwelling time and commonly seen in forgotten stent, particularly in poor compliant patients. Although majority can be managed by endourological procedure, prevention from this complication should be the goal. Patient's education regarding the stent and its complication and compliance may play a great role.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Zimskind PD, Fetter TR, Wilkerson JL. Clinical use of long-term indwelling silicone rubber ureteral splints inserted cystoscopically. J Urol. 1967;97:840–4. doi: 10.1016/S0022-5347(17)63130-6. [DOI] [PubMed] [Google Scholar]
- 2.Denstedt JD, Reid G, Sofer M. Advances in ureteral stent technology. World J Urol. 2000;18:237–42. doi: 10.1007/pl00007074. [DOI] [PubMed] [Google Scholar]
- 3.Lawrentschuk N, Russel JM. Ureteric stenting 25 years on: Routine or risky? ANZ J Surg. 2004;74:243–7. doi: 10.1111/j.1445-2197.2004.02947.x. [DOI] [PubMed] [Google Scholar]
- 4.Miyaoka R, Monga M. Ureteral stent discomfort: Etiology and management. Indian J Urol. 2009;25:455–60. doi: 10.4103/0970-1591.57910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joshi HB, Stainthorpe A, Keeley FX, Macdonagh R, Timoney AG. Indwelling ureteral stents: Evaluation of quality of life to aid outcome analysis. J Endourol. 2001;15:151–4. doi: 10.1089/089277901750134421. [DOI] [PubMed] [Google Scholar]
- 6.Deliveliotis C, Chrisofos M, Gougousis E, Papatsoris A, Dellis A, Varkarakis IM. Is there a role for alpha1-blockers in treating double-J stent-related symptoms? Urology. 2006;67:35–9. doi: 10.1016/j.urology.2005.07.038. [DOI] [PubMed] [Google Scholar]
- 7.Kumar M, Aron M, Aggarwal AK, Gupta NP. Stenturia: An unusual manifestation of spontaneous ureteral stent fragmentation. Urol Int. 1999;62:114–6. doi: 10.1159/000030370. [DOI] [PubMed] [Google Scholar]
- 8.Zisman A, Siegel YI, Siegmann A, Lindner A. Spontaneous ureteral stent fragmentation. J Urol. 1995;153:718–21. doi: 10.1097/00005392-199503000-00049. [DOI] [PubMed] [Google Scholar]
- 9.Damiano R, Oliva A, Esposito C, De Sio M, Autorino R, D’Armiento M. Early and late complications of double pigtail ureteral stent. Urol Int. 2002;69:136–40. doi: 10.1159/000065563. [DOI] [PubMed] [Google Scholar]
- 10.Ullah I, Alam K, Wazir BG, Shah F, Nawaz A, Malik A. Indications and Morbidity of Indwelling Ureteral Stenting. Ann Pak Inst Med Sci. 2011;7:173–5. [Google Scholar]
- 11.Monga M, Klein E, Castañeda-Zúñiga WR, Thomas R. The forgotten indwelling ureteral stent: A urological dilemma. J Urol. 1995;153:1817–9. [PubMed] [Google Scholar]
- 12.Bhatia V, Biyani CS. Pan proximal migration of ureteral stent: Case report. East Afr Med J. 1993;70:531. [PubMed] [Google Scholar]
- 13.Breau RH, Norman RW. Optimal prevention and management of proximal ureteral stent migration and remigration. J Urol. 2001;166:890–3. [PubMed] [Google Scholar]
- 14.Singh I. Indwelling JJ ureteral stents - a current perspective and review of literature. Indian J Surg. 2003;65:405–12. [Google Scholar]
- 15.Oswalt GC, Jr, Bueschen AJ, Lloyd IK. Upward migration of indwelling ureteral stents. J Urol. 1979;122:249–50. doi: 10.1016/s0022-5347(17)56350-8. [DOI] [PubMed] [Google Scholar]
- 16.Robert M, Boularan AM, El Sandid M, Grasset D. Double-J ureteric stent encrustations: Clinical study on crystal formation on polyurethane stents. Urol Int. 1997;58:100–4. doi: 10.1159/000282959. [DOI] [PubMed] [Google Scholar]
- 17.el-Faqih SR, Shamsuddin AB, Chakrabarti A, Atassi R, Kardar AH, Osman MK, et al. Polyurethane internal stents in treatment of stone patients: Morbidity related to indwelling times. J Urol. 1991;146:1487–91. doi: 10.1016/s0022-5347(17)38146-6. [DOI] [PubMed] [Google Scholar]
- 18.Rabani SM. Combined percutaneous and transurethral lithotripsy for forgotten ureteral stents with giant encrustation. Nephrourol Mon. 2012;4:633–5. doi: 10.5812/numonthly.4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finney RP. Experience with new double J ureteral catheter stent. J Urol. 1978;120:678–81. doi: 10.1016/s0022-5347(17)57326-7. [DOI] [PubMed] [Google Scholar]


