Abstract
Objective:
Perioperative complications are one of the surrogate indicators of surgical outcomes. However, reporting these complications need a precise grading system. Our aim is to report and grade the complications of semirigid ureteroscopy in ureteral stone management according to the modified Clavien classification system.
Materials and Methods:
This is a prospective study conducted From January 2012 to June 2013. All patients with ureteral stones who were indicated for semirigid URS were evaluated. All procedures were performed by the same surgeon. The data recorded including patient demographics, clinical indication, stone size and location, operative time and complications were classified according to the modified Clavien classification system. The patients were followed for 8 weeks postoperatively.
Results:
148 patients included, Stone distribution was: 89 (60.1%) lower ureteral, 26 (17.6%) mid ureteral, and 33 (22.3%) upper ureteral. the mean stone size was 8.6 mm. Urgent URS done in 23% of patient. The overall stone free rate was 88.5%, the individual stone free rate for the upper, middle and lower ureter were 87.9%, 84.6%, and 89.9%, respectively. The mean operative time was 31.9 min (20-50 min.). Complications occurred in 26.35% of patients. Grade I complications occurred in 32 patients (26.1%), grade II in 9 (6.1%), grade IIIa in 7 (4.7%), grade IIIb in 8 (5.4%), grade IVa in two patient (1.35%), and grade IVb in one patient (0.7%). No grade V complication was encountered.
Conclusion:
Ureteroscopy becomes the vanguard interventional therapy for ureteral stones with well-established efficacy and safety. It is of paramount importance to adopt a precise structured classification system for reporting surgical complications, that should be flexible and comprehensive in order to accommodate the various and rapidly expanding surgical fields.
Keywords: Complications, clavien classification, lithotripsy, ureteroscopy, ureteral stone
INTRODUCTION
The escalating technical refinements in ureteroscopy (URS) greatly expand their uses and improved their safety. URS become a major technique and in-dispensable procedure for the diagnosis and treatment of upper urinary tract lesions.[1] Albeit its widely applicable diagnostic and therapeutic benefits, URS may be associated with noticeable complications ranging from mild flank pain to ureteral avulsion and sepsis.[2]
Perioperative complications are still in need of a succinct, widely acceptable definition, and a precise grading system for their severity. Therefore, a standardized classification system offering a common platform for communication among urologists is essential.[3] The Clavien classification system has been used initially to grade complications of general surgery[4] which had been modified and validated further.[5] Currently, its use is prevailing in most aspects of urology.[6]
MATERIALS AND METHODS
This is a prospective study conducted in the period between January 2012 and June 2013; all patients with ureteral stones admitted for semirigid URS by single surgeon were analyzed. All patients were assessed by urinalysis, complete blood counts, blood urea nitrogen (BUN), serum creatinine, urine culture (if indicated), plain abdominal X-ray (KUB), and renal ultrasonography. Non-contrasted urinary tract CT scan and/or intravenous urography (IVU) were requested upon certain indications.
Our inclusion criteria were: Age above 18 years with symptomatic ureteral stone(s) requiring endoscopic intervention. Patients with sepsis, pyonephrosis, indwelling ureteral stent, unfitness for general anesthesia, and/or lithotomy position and patients need bilateral ureteroscopy were excluded. The data recorded included patient demographics, stone size and location, operative time, auxiliary procedures, stone free rate, and complications which were graded according to the MCCS with their management. All enrolled patients signed an informed consent.
All the patients were given 1 gm of Ceftriaxone intravenously at the induction of anesthesia (or 500 mg Amikacin intravenously in Penicillin allergic patients); all procedures have been done under GA in lithotomy position (to avoid excessive kidney movement which may be bothersome especially in proximal ureteral stones). Rigid cystoscopy was performed initially to evaluate the lower urinary tract and ureteral orifice, followed by Safety wire insertion, and then semirigid ureteroscopy (9.5 and 8 Fr.) were used. The stones were removed by grasping forceps and/or fragmented with Holmium: Yttrium–aluminum–garnet (YAG) laser lithotripsy. No basket was used. Double J ureteral stent was inserted when indicated by the surgeon for migrated stones, ureteral perforations, ureteral stricture, and impacted stones. No indwelling urethral catheter was inserted routinely.
Following recovery from anesthesia, assessment of vital signs and KUB were done to ensure stone free status and double J stent position, then the patients were discharged on a day case basis unless otherwise there is an indication for keeping them in hospital. All patients scheduled to visit the clinic after 1 week unless there is uncontrolled pain, fever, hematuria, inability to pass urine or other complaints were they should attend our emergency department and were managed accordingly.
The patients were followed postoperatively with visits at 1, 4, and 8 weeks, in each visit a focused history, physical examination, serum creatinine (if indicated), and ultrasound examination done for all patients. If there is suspicion of residual stones or complications then KUB, IVU, and/or CT. Scan of the urinary tract were done accordingly. Clinically insignificant residual fragments (CIRFs) were defined as less than 2 mm, asymptomatic, noninfectious, and non-obstructive residual fragments. Indwelling Double J stent was removed within 2-4 weeks postoperatively.
Hematuria that persisted >6 h and had resolved spontaneously by 48 h was considered as “transient hematuria” and hematuria persisting for >48 h was considered as “persistent hematuria.”
All complications were classified according to the MCCS by the operating surgeon. In patients with more than one complication, each one was graded separately according to their levels. The study was approved by the authorities of department of Surgery.
RESULTS
Of the 169 patients with ureteral stones admitted for ureteroscopy, 148 included in the study and some of the parameters shown in Table 1. The excluded patients were 21: Of which six were unfit for GA and/or lithotomy position, five had pyonephrosis with impacted stone, four patients need bilateral URS, three had sepsis, and three patients had indwelling Double J stent. Patient need bilateral ureteroscopy were excluded from the study because this may cause confusion in the interpretation of the results.
Table 1.
Patients characteristics
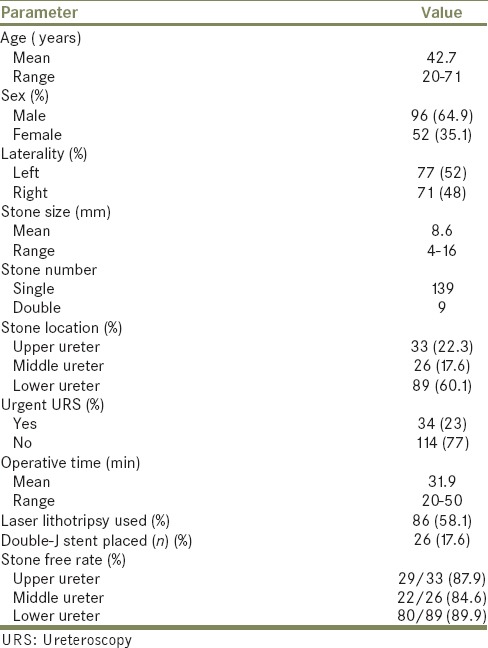
Urgent URS (within 72 h from presentation) was done in 34 (23%) patients because of severe pain and/or obstruction in a solitary functioning kidney. The mean operative time was 31.9 min (20-50 min). Laser lithotripsy used in 86 (58.1%) patients and 4.7 Fr./28 cm. Double J ureteral stent inserted in 26 patients (17.6%) and removed when it's indication is vanished at 2-4 weeks. The success rate was defined as the absence of residual stones/fragments following URS. The overall stone free rate was 131/148 (88.5%). The mean hospital stay was 12.9 h (8-120 h).
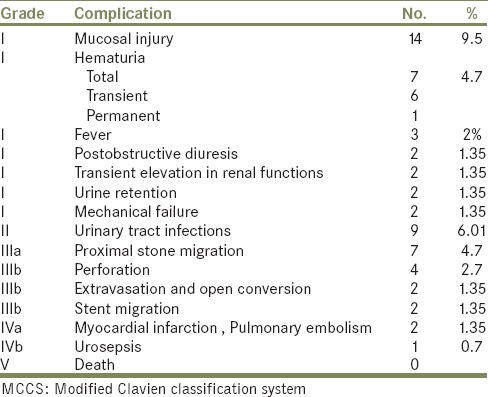
Fifty-nine complications occurred in 39 patients (26.35%). patients with more than one complication were graded separately, 3 patients had three complications, 14 had two complications, and 22 had one. Grade I complications occurred in 32 patients (26.1%), grade II in 9 (6.1%), grade IIIa in 7 (4.7%), grade IIIb in 8 (5.4%), grade IVa in two patient (1.35%), and grade IVb in one patient (0.7%). No grade V complication was encountered. The classification of the complications illustrated in Table 2.
Table 2.
The complications and their grades according to the MCCS
DISCUSSION
For many decades, reporting the surgical outcome gained an utmost importance in surgical armamentarium. It contributes efficiently in improving health care quality control, helps in evaluating certain maneuvers and/or techniques and assessing the learning curve for them and finally boosts surgical research. Morbidity rate is a key parameter in the evaluation of any medical intervention.[7]
There is a considerable overlap and lack of specification in reporting surgical outcomes which may be termed as complications, morbidity and/or mortality, mishaps, unfavorable incidents, and the need for further treatment. A semantic definition of postoperative complications is “any deviation from the ideal postoperative course that is not inherent in the procedure and does not comprise a failure to cure.”[8]
Despite the tremendous advances in evidence-based medical practice, inconsistency in reporting perioperative adverse events was still observed both in hospital records and clinical research. Severity grading was used in only one-third of large (over 100 patients) randomized controlled studies in surgery from 1990 to 2001.[9] The MCCS had been applied to grade complications of many urological procedures such as Percutaneous Nephrolithotomy,[10] TURP,[11] and radical prostatectomy.[12]
Options for ureteral stones management include wide array of medical and surgical modalities. Medical expulsive therapy proved to facilitate passage for stones less than 10 mm along the whole ureter.[13] On the other hand, URS and SWL are currently the main interventional treatment options for symptomatic ureteral stones. Although URS is a more invasive option than SWL, it has a better success rate with an overall success rate extending from 85.6%[14] to 95.7%.[15]
According to the European urology association (EUA) guidelines, the SFR for proximal ureteral stones with flexible and semirigid URS is 87% and 77%, respectively, for mid and lower ureteral stones: Semirigid URS achieves a SFR of 86% and 94%, respectively.[16] In our study, we achieved an overall SFR of 88.5%.
Ureteroscopic complications had been reported extensively in the literatures but these complications were traditionally classified as minor versus major or acute versus chronic and such classifications are subjective and not agreed upon by all urologist. Moreover, most of them were reported retrospectively and they lack a standard structured classification system. Only two prospective studies (up to our modest knowledge) used the MCCS to grade URS complications.[14,17] Another study reported URS complications using a different structured grading system which is the modified Satava classification.[18]
The complications of URS in general are minor and self-limiting, only few major complications require surgical management or result in mortality had been reported. Overall complication rate ranging from 3.5%[14] to 30%,[17] 13.1% for emergency URS[19] and 27.5% for impacted stones URS.[20] In our series, we reported 59 complications in 39 patients (26.35%), this relatively high complications rate attributed to some factors: Firstly, the prospective nature of the study and the use of a structured, objective, clearly defined classification system. Secondly, some of the minor or self-limiting complications may be underreported in the previous studies and finally, most of the large studies with low complication rates came from the centers of excellence with long experience.[14] Mandal et al. study which has a similar design to our study showed a complication rate of 30%.[17]
According to the MCCS, we have five grades for complications, Grade 1 and 2 equivalents to minor complications while grades 3-5 are regarded as major. Our use of this system was straight forward, rapid and easy to assign each complication to its appropriate grade [Table 2]. Minor complications represent about 14.2% while major ones were about 12.2% in our study.
Grade 1 complications were the most common in our patients (26.1%) and represent 32/59 (54.2%) of all complications. Mucosal abrasion and superficial false passage which are closely related to each other were regarded as one entity which was the most common complication 14/59 (23.7%) occurring in 14/148 (9.5%) of all patients. The rate of this complication in other studies fluctuating widely from 2.8%[18] to 24%.[21] Those patients need no further therapy.
The next complication was transient hematuria in six patients (4.1%) and persistent hematuria in one patient (0.7%), all of them had indwelling Double J stent and all resolved spontaneously. Elashry[2] reported transient hematuria of 2.2% while in Mandal study[17] it reached to 19%. Regarding persistent hematuria, it ranged from 0.1% to 2%.[22]
Fever was noticed in three patients (2%). The lowest reported rate was 1%[22] but it may reach up to 20%.[23] Those patients had transient fever and graded separately from other complications associated with fever such as urinary tract infection (UTI) (n = 9), extravasation (n = 2), and urosepsis in one patient. A rare but potentially serious complication, post-obstructive diuresis, occurs in two patients (1.4%) who initially presented with obstructed solitary kidney, although this complication was classified as grade I but both patients required hospital admission for 4 days each with daily monitoring and laboratory investigations. This sort of inconsistency between the grade of the complication and its impact raise the need for further modification of MCCS to incorporate hospital stay and management cost in it.
Proximal stone migration observed in 7/148 (4.7%) of patients (4 upper, 1 middle and 2 lower ureteral stones), Arıdogan et al.[24] showed that proximal stone migration was more likely when the stone was located in the proximal ureter (29%) than in the middle or distal ureter (6%). Similarly, El-Nahas et al.[23] reported a high incidence (35%) of secondary procedures to manage upward stone migration or complications after URS for proximal ureteral stones. our patients were managed with ESWL, no baskets and/or cones were used because they are costly and unavailable.
Ureteral perforation occur in 4/148 (2.7%), all of them underwent 9.5 Fr. URS for stones larger than 10 mm in diameter. They were subsequently treated by JJ insertion and antibiotic cover and all recovered with uneventful course previous literatures showed rates from 1.6%[17] to 6.25% and it seems to be related to the stone size.[25]
Two patients (1.35%) had big ureteral perforation with urinary extravasation which was discovered immediately and dealt with at the same session by open conversion, drainage of the extravasation and ureteral stent insertion. Such complication rates ranging from less than 1%[26] to 3.2%.[27] No ureteral avulsion was reported; a recent study showed low avulsion rate of 0.16%[18] while the older studies showed rates up to 0.5%.[28]
Regarding concurrent pharmacotherapy, 11 patients were on anticoagulant therapy: Two on Warfarin who were asked to stop their medications and nine on low dose salicylate who underwent URS without stopping their medications and none of them showed significant hematuria. Of the 106 elective cases, 85 (80.2%) were on medical expulsive therapy (Tamsulosin 0.4 mg or alfuzosin 10 mg at bed time).
MCCS was proved to be precise, practical, and easy to use classification system. On the other hand, it needs to be more comprehensive and to include other vital parameters such as hospital stay, management cost, and readmission rate. There is a need to incorporate the intervention setting, whether at bedside or theater, into the classification system as well.
The limitations of this study include: Firstly, it is a single surgeon and single center study and it would be more representative if it involves multiple centers. Secondly, the MCSS preferably be assigned by another observing surgeon rather than the operating surgeon to avoid any bias.
CONCLUSION
Ureteroscopy become the prevailing surgical therapy for ureteral stones with well-established efficacy and safety. It is of paramount importance to adopt a precise structured classification system for reporting surgical complications which should be convenient and updated in order to accommodate various and rapidly expanding surgical fields.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Isen K. Single-session ureteroscopic pneumatic lithotripsy for the management of bilateral ureteric stones. Int Braz J Urol. 2012;38:63–8. doi: 10.1590/s1677-55382012000100009. [DOI] [PubMed] [Google Scholar]
- 2.Elashry OM, Elgamasy AK, Sabaa MA, Abo-Elenien M, Omar MA, Eltatawy HH, et al. Ureteroscopic management of lower ureteric calculi: A 15-year single-center experience. BJU Int. 2008;102:1010–7. doi: 10.1111/j.1464-410X.2008.07747.x. [DOI] [PubMed] [Google Scholar]
- 3.Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: A standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011;29:205–10. doi: 10.1007/s00345-010-0566-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- 5.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of a 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan M, Smith N, Thomas K, Murphy D. Is Clavien the new standard for reporting urological complications? BJU Int. 2009;4:434–9. doi: 10.1111/j.1464-410X.2009.08516.x. [DOI] [PubMed] [Google Scholar]
- 7.Jaques DP. Measuring morbidity. Ann Surg. 2004;240:214–5. doi: 10.1097/01.sla.0000133124.62619.1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dindo D, Clavien A. What is a surgical complication? World J Surg. 2008;32:939–41. doi: 10.1007/s00268-008-9584-y. [DOI] [PubMed] [Google Scholar]
- 9.Martin G, Brennan F, Jaques P. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–13. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin TS, Cho HJ, Hong SH, Lee JY, Kim SW, Hwang TK. Complications of percutaneous nephrolithotomy classified by the modified clavien grading system: A single center's experience over 16 years. Korean J Urol. 2011;52:769–75. doi: 10.4111/kju.2011.52.11.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: A standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011;29:205–10. doi: 10.1007/s00345-010-0566-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rabbani F, Yunis LH, Pinochet R, Nogueira L, Vora KC, Eastham JA, et al. Comprehensive standardized report of complications of retropubic and laparoscopic radical prostatectomy. Eur Urol. 2010;57:371–86. doi: 10.1016/j.eururo.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 13.Ibrahim A, Mahmood I, Mahmood N. Efficacy and safety of tamsulosin vs. alfuzosin as medical expulsive therapy for ureteric stones. Arab J Urol. 2013;11:142–7. doi: 10.1016/j.aju.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de la Rosette J, Denstedt J, Geavlete P, Keeley F, Matsuda T, Pearle M, et al. The clinical research office of the endourological society ureteroscopy global study: Indications, complications, and outcomes in 11,885 patients. J Endourol. 2014;28:131–9. doi: 10.1089/end.2013.0436. [DOI] [PubMed] [Google Scholar]
- 15.Gunlusoy B, Degirmenci T, Kozacioglu Z, Arslan M, Ceylan Y, Nergiz N, et al. Factors affecting the complications of pneumatic lithotripsy for the treatment of ureteral Stones with different localizations: A multivariate analysis of complications. Urol Int. 2013;91:357–62. doi: 10.1159/000350243. [DOI] [PubMed] [Google Scholar]
- 16.Turk C, Knoll T, Petrik A, Sarica K, Straub M, Seitz C. Guidelines on Urolithiasis. Arnheim, the Netherlands: European Association of Urology. 2013:33–53. [Google Scholar]
- 17.Mandal S, Goel A, Singh MK, Kathpalia R, Nagathan DS, Sankhwar SN, et al. Clavien classification of semirigid ureteroscopy complications: A prospective study. Urology. 2012;80:995–1001. doi: 10.1016/j.urology.2012.05.047. [DOI] [PubMed] [Google Scholar]
- 18.Tepeler A, Resorlu B, Sahin T, Sarikaya S, Bayindir M, Oguz U, et al. Categorization of intraoperative ureteroscopy complications using modified Satava classification system. World J Urol. 2014;32:131–6. doi: 10.1007/s00345-013-1054-y. [DOI] [PubMed] [Google Scholar]
- 19.Al-Ghazo MA, Ghalayini IF, Al-Azab RS, Bani Hani O, Bani-Hani I, Abuharfil M, et al. Emergency ureteroscopic lithotripsy in acute renal colic caused by ureteral calculi: A retrospective study. Urol Res. 2011;39:497–501. doi: 10.1007/s00240-011-0381-y. [DOI] [PubMed] [Google Scholar]
- 20.Degirmenci T, Gunlusoy B, Kozacioglu Z, Arslan M, Kara C, Koras O, et al. Outcomes of ureteroscopy for the management of impacted ureteral calculi with different localizations. Urology. 2012;80:811–5. doi: 10.1016/j.urology.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Francesca F, Scattoni V, Nava L, Pompa P, Grasso M, Rigatti P. Failures and complications of transurethral ureteroscopy in 297 cases: Conventional rigid instruments vs. small caliber semirigid ureteroscopes. Eur Urol. 1995;28:112–5. doi: 10.1159/000475032. [DOI] [PubMed] [Google Scholar]
- 22.Yaycioglu O, Guvel S, Kilinc F, Egilmez T, Ozkardes H. Results with 7.5F versus 10F rigid ureteroscopes in treatment of ureteral calculi. Urology. 2004;64:643–6. doi: 10.1016/j.urology.2004.05.050. [DOI] [PubMed] [Google Scholar]
- 23.El-Nahas AR, El-Tabey NA, Eraky I, Shoma AM, El-Hefnawy AS, El-Assmy AM, et al. Semirigid ureteroscopy for ureteral stones: A multivariate analysis of unfavorable results. J Urol. 2009;181:1158–62. doi: 10.1016/j.juro.2008.10.167. [DOI] [PubMed] [Google Scholar]
- 24.Arıdogan IA, Zeren S, Bayazit Y, Soyupak B, Doran S. Complications of pneumatic ureterolithotripsy in the early postoperative period. J Endourol. 2005;19:50–3. doi: 10.1089/end.2005.19.50. [DOI] [PubMed] [Google Scholar]
- 25.Kassem A, Elfayoumy H, Elsaied W, Elgammal M, Bedair A. Laser and pneumatic lithotripsy in the endoscopic management of large ureteric stones: A comparative study. Urol Int. 2012;88:311–5. doi: 10.1159/000336254. [DOI] [PubMed] [Google Scholar]
- 26.Geavlete P, Georgescu D, Niţă G, Mirciulescu V, Cauni V. Complications of 2735 retrograde semirigid ureteroscopy procedures: A single-center experience. J Endourol. 2006;20:179–85. doi: 10.1089/end.2006.20.179. [DOI] [PubMed] [Google Scholar]
- 27.Mursi K, Elsheemy M, Morsi H, Ghaleb A, Abdel-Razzak O. Semi-rigid ureteroscopy for ureteric and renal pelvic calculi: Predictive factors for complications and success. Arab J Urol. 2013;11:136–41. doi: 10.1016/j.aju.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weinberg JJ, Ansong K, Smith AD. Complications of ureteroscopy in relation to experience: Report of survey and author experience. J Urol. 1987;137:384–85. doi: 10.1016/s0022-5347(17)44040-7. [DOI] [PubMed] [Google Scholar]


