Abstract
Background:
Appropriate treatment of osteonecrosis of femoral head (ONFH) remains challenging.
Objectives:
Here, we report the results of treating these patients with auto-corticocancellous bone graft from iliac crest to overcome the need for early total hip arthroplasty (THA).
Patients and Methods:
There were 132 hips (96 patients) with ONFH. Association Research Circulation Osseous (ARCO) type II and III underwent auto-corticocancellous bone grafting from the iliac crest in the current prospective study. Before the operation and in the final postoperative visit, the pain intensity using visual analogue scale (VAS), range of hip motions and Harris hip score (HHS) were determined and compared. Patients were followed for 48.5 ± 17.9 months.
Results:
The shape of head and the joint space were preserved in 120 hips (90.9%). There were 12 hips in which the disease progressed to grade IV and resulted in THA in 10 of them. The pain intensity significantly decreased (6.3 ± 4.1 vs. 1.4 ± 2) and HHS (35.8 ± 15.3 vs. 79.5 ± 16.2) and range of motion (ROM) significantly improved after the operation (P < 0.001).
Conclusions:
Necrotic bone removal and filling the femoral head cavity with auto-corticocancellous bone graft from iliac crest is an effective femoral head preserving method in treating patients with precollapse stages of ONFH and preventing the need for early THA, especially in young active populations.
Keywords: Osteonecrosis, Femoral Head, Bone Graft
1. Background
Traumatic and atraumatic osteonecrosis of the femoral head (ONFH) has remained a challenging problem for orthopedic surgeons. In late stages of the disease, degenerative changes in the hip joint necessitate hip arthroplasty as the definite treatment. Although recent advances in arthroplasty technologies (design of implants, materials, surgical equipment and techniques) have resulted in increased prosthesis survival, since ONFH usually involves the young active population, it is possible that patients require more than one THA. To avoid early hip arthroplasty, several head preserving procedures such as core decompression (CD), proximal femoral osteotomy, vascularized and nonvascularized bone grafting and bone substitutes have been introduced (1-17); but to our knowledge, the efficacies of these methods are controversial and none of these treatment methods can effectively prevent the progression of the disease to femoral head collapse and subsequent degenerative changes of the hip joint (18). The light bulb technique was described by Rosenwasser et al. in 1994, in which dead and diseased bone was replaced by cancellous bone graft (19).
2. Objectives
In the current study, we investigated the midterm results of treating advanced ONFH Association Research Circulation Osseous (ARCO) type II and III using auto-corticocancellous bone graft from the iliac crest.
3. Patients and Methods
Between February 2003 and April 2008, we assessed 101 patients with ONFH ARCO type II and III who contributed to the current prospective study in Akhtar Hospital of Tehran. During the follow up, three patients relocated to a new address and two others refused to return for the final examination. Therefore, the study was completed with 96 patients (132 hips). The demographic and underlying data are presented in Table 1. Before the operation, the ethics committee approval was obtained and all the patients signed informed consents. Patients with previous histories of hip surgery, traumatic ONFH and infection were excluded. Diagnosis of ONFH was made based on the plain radiography anteroposterior (AP) and lateral frog leg views and magnetic resonance imaging (MRI) (sagittal and coronal views). The grade of ONFH was determined based on the ARCO classification system (20). In addition, the pain intensity was determined utilizing visual analogue scale (VAS). In this setting, zero was attributed to no pain, while 10 indicated the worst imaginable pain. Patients were followed up for 48.5 ± 17.9 months (ranging from 22 to 76). Before the operation, the hip motions were measured and Harris hip score (HHS) was completed for all the patients to investigate the hip joint function.
Table 1 . Demographic and Underlying Information of the Patients a.
| 132 Hips (n =96) | |
|---|---|
| Age, mean ± SD, y | 33.7 ± 5.3 |
| Gender | |
| Male | 57 |
| Female | 39 |
| Bilateral AVN patients, hip side | |
| Right | 36 |
| Left | 71 |
| ARCO classification, hip | |
| II A | 61 |
| II B | 27 |
| II C | 24 |
| III A | 26 |
| III B | 23 |
| III C | 17 |
| Etiology, patient | |
| Corticosteroids | 15 |
| Trauma | 48 |
| Drug | 12 |
| Alcohol | 19 |
| Idiopathic | 5 |
a Abbreviation: ARCO, Association Research Circulation Osseous; AVN, visual analogue scale.
3.1. Surgical Technique
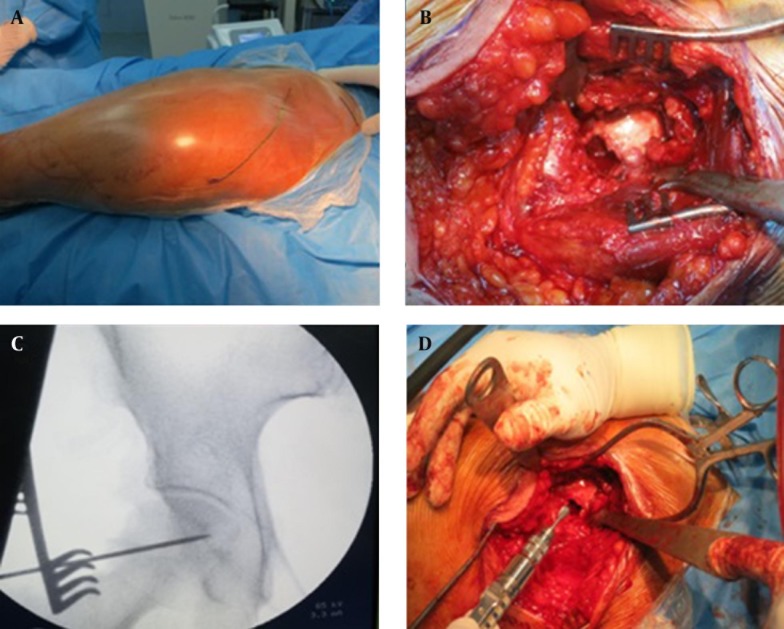
In the supine position, while a sandbag was placed beneath the affected hip, an 8-cm incision was made over the anterolateral aspect of the greater trochanter. After splitting the tensor fascia latae along the skin incision, we reached the articular capsule between the tensor fascia latae and gluteus medius and incised the capsule in a T-shape manner. Capsulotomy was performed with a vertical incision placed along the femoral neck and a transverse one along the acetabular attachment of the capsule. The anterior flap was retracted anteriorly to expose the anterior aspect of the proximal femoral. A small bone window (1.0-1.5 cm2) was made through the anterior aspect of femoral neck using drills and osteotomes. After removing the window, the area of osteonecrosis, which was determined pre- and intra-operatively using fluoroscopy, was then evacuated from the necrotic bone to the subchondral bone. The sclerotic bone was perforated with an electric drill until bleeding occurred. After measuring the volume of cavity, the cortico-cancellous matchstick-like autograft which was harvested from the ilium (using minimal incision over the anterior part of the iliac bone) was packed into the femoral cavity in a layered manner to fill the void space and support the subchondral bone. The cortical window was replaced and packed in place (Figure 1). After the operation, the patients were followed clinically and radiologically. The progression of AVN and the articular cartilage status were assessed using plain radiography and MRI. In the final visit, the range of hip motions was measured and HHS was completed for all the patients. In addition, the pain severity was determined using VAS. In our study, radiographic progression of AVN to ARCO grade IV or need for THA was defined as the failure end-point. Finally, all the parameters before and after the surgery were compared using SPSS version 16. The mean of hip ROM and HHS were compared using paired t-test. P < 0.05 was considered significant.
Figure 1. A) The outline of incision used in the current study; B) we made a window using drilling and osteotome in the anterior surface of the femoral neck; C) anteroposterior fluoroscopic image showing the pin inserted into the necrotic bone; D) the necrotic bone was removed through the window and the femoral head was filled in with corticocancellous bone grafts.
4. Results
Interestingly, we found that after a mean of 48.5 months, the shape of head and the joint space were preserved in 110 hips (90.9%) (Figure 2). Unfortunately, in 12 hips, the disease progressed to more severe grade of AVN (grade IV) and the total hip arthroplasty was performed for 10 of these hips. The failure rate in the ARCO stages IIB, IIC, IIIA, IIIB and IIIC were 8.7%, 4.5%, 5%, 12.5% and 40%, respectively. The procedure was associated with successful outcomes in all the patients with ARCO stage IIA of ONFH. Table 2 compares pre- and postoperative pain, hip ROM, and HHS. The pain based on VAS significantly decreased and HHS and ROM significantly increased after the operation (P < 0.001).
Figure 2. A 27-Year-Old Female with Bilateral ONFH, Resulting From Corticosteroid Use. A) Preoperative anteroposterior X-ray, showing ONFH ARCO type II b in left and II in right sides; B and C) AP X-ray and MRI after 24 months showing arrested progression of AVN. This patient was pain free at the last visit with nearly full range of hip motions.
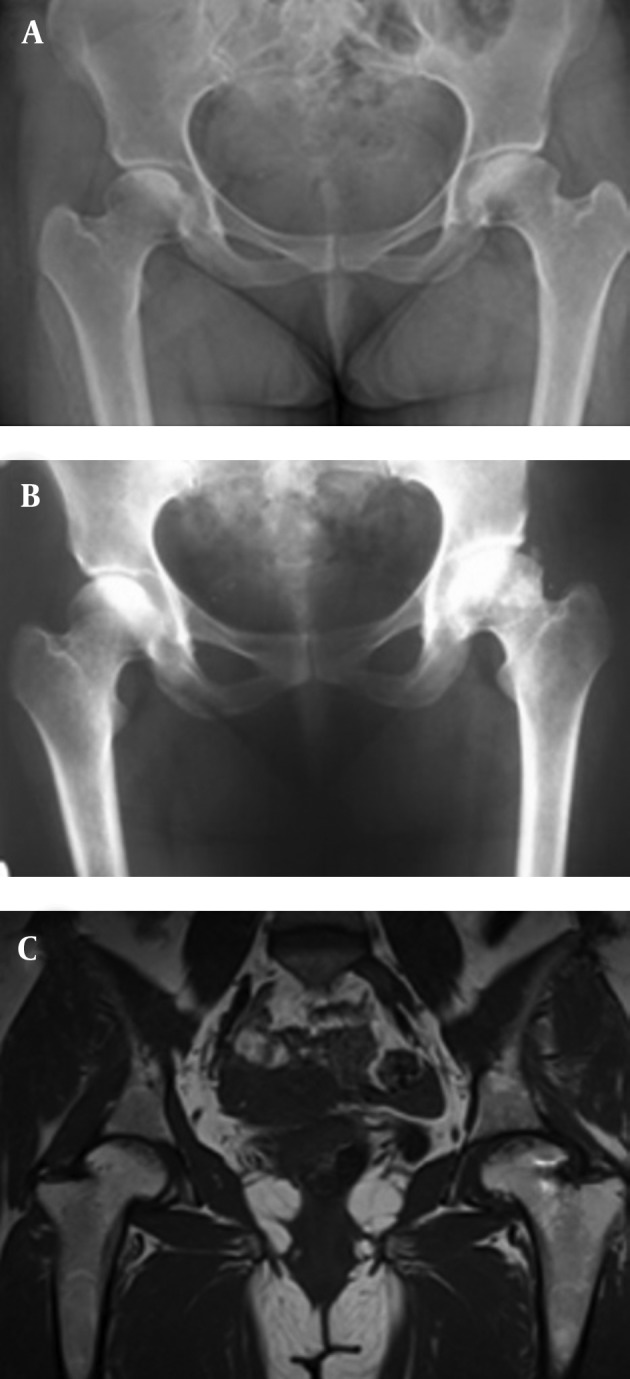
Table 2. Comparison of the ARCO Classification, Range of Motion, Visual Analogue Scale and Harris Hip Score Before and After the Operation a,b.
| Preoperation | Postoperation | P Value | |
|---|---|---|---|
| Pain, VAS | 6.3 ± 4.1 | 1.4 ± 2 | < 0.001 |
| [range] | [4-9] | [1-5] | |
| ROM, degree | |||
| Flexion | 53.2 ± 16.3 | 113 ± 22 | < 0.001 |
| Extension | 6.5 ± 3 | 9.4 ± 2.1 | < 0.001 |
| Abduction | 12.5 ± 5.7 | 37.3 ± 11 | < 0.001 |
| Adduction | 11.2 ± 8.2 | 28.3 ± 8.1 | < 0.001 |
| External rotation | 15.2 ± 5.1 | 38.6 ± 9 | < 0.001 |
| Internal rotation | 12.3 ± 4 | 24.6 ± 7.3 | < 0.001 |
| HHS | 35.8 ± 15.3 | 79.5 ± 16.2 | < 0.001 |
| [range] | [28-51] | [67-95] |
a Abbreviations: ARCO, Association Research Circulation Osseous; HHS, Harris hip score; ROM, range of motion; VAS, visual analogue scale.
b Data are presented as mean ± SD.
5. Discussion
Our study demonstrated that removing the necrotic bone and filling the femoral head space using auto-corticocancellous bone grafts derived from iliac crest was an appropriate treatment method for precollapse stages of ONFH, associated with favorable results and improved function. We found that this method can effectively overcome the pain and disability of ONFH by avoiding the progression of AVN and femoral head collapse and preserving the joint space. Traumatic or atraumatic ONFH is a challenging and complicated problem for hip surgeons. It can involve young active populations as a consequence of traumatic hip dislocation or femoral neck fracture or atraumatic events. Although THA can effectively relieve symptoms, because of the probable need for more THAs, this technique seems to be unfavorable. Currently, in many countries such as Iran, anabolic steroids are greatly used by many athletes, especially in body building, which is associated with substantial increase of ONFH risk. For this reason, many surgeons try to delay THA as much as possible. Nonoperative treatments of ONFH such as extracorporeal shock wave therapy, electromagnetic pulsed fields, hyperbaric oxygen therapy, drugs, physical therapy, and regenerative medicine have had disappointing outcomes (21-24). In addition, some authors have suggested cell therapy using autologous bone marrow grafting (25, 26). Mao et al. treated 78 hips with ONFH using targeted intra-arterial delivery of concentrated autologous bone marrow containing mononuclear cells and after five years found satisfactory outcomes in 92.3% of the hips. However, 7.7% of the hips required THA and radiological progression was observed in 43.6%. In addition, they demonstrated that this technique was useful for early precollapse stages of the disease (25). Therefore, to delay THA, several femoral head preserving procedures were introduced with their own advantages and a disadvantages; however, the success of these procedures has been under question (1-17). Core decompression with and without inserting a tantalum implant is an old simple femoral-head preserving method which is currently used in some orthopedic centers. Veillette et al. investigated two years of survivorship and clinical and radiographic outcomes of core decompression and a porous tantalum implant in treatment of ONFH in 58 hips. Most of these hips (84%) were in stage II of the disease based on the Steinberg classification system. They found that nine hips (15.5%) required THA. In addition, the survival rates were 91.8% after one year, 81.7% after two years, and 68.1% after four years (7). As Veillette et al. demonstrated (7), the failure rate after core decompression and inserting a tantalum implant was high and after four years, about one third of hips needed THA. In addition, removing a tantalum implant for hip arthroplasty is very devastating and difficult. Smith et al. treated 114 hips with ONFH with core decompression and found that after an average of three years and four months, 64 hips (56%) failed clinically and needed further surgery (6). Recently, some authors introduced arthroscopic-assisted core decompression for treatment of ONFH and believed that the technique had several advantages such as evaluating the presence of articular cartilage and subchondral collapse and possibility of treating other bony or soft tissue injuries (27, 28). However, to our knowledge, there is no study reporting the clinical or radiological outcomes of the technique and some studies in this field are required. Some surgeons suggested that using vascularized fibular grafts can be an appropriate treatment method for ONFH. In a retrospective study, Aldridge et al. assessed the outcomes of treatment of ONFH with free vascularized fibular grafting in 224 hips after an average of 4.3 years. In these patients, osteonecrosis led to collapse of the femoral head, but not to arthrosis. They found that the survival rate was 67.4% for the hips, which were followed for a minimum of two years, and 64.5% for those which were followed for a minimum of five years. The mean HHS increased from 54.5 to 81 after the operation, in whom the surgery was successful (1). In a systematic review, Fang et al. evaluated the outcomes of treating ONFH with vascularized fibular graft. They found that vascularized fibular graft resulted in good to excellent clinical outcomes in 69% of patients. The conversion rate to THA, collapse rate and complication rates were 16.5%, 16.7% and 23.8%, respectively. They concluded that vascularized fibular graft was an effective method in prevention of ONFH progression and collapse and can retard or avoid hip replacement (4). Fang et al. (4) concluded that vascularized fibular grafting was an effective method for treatment of ONFH, but it was associated with high complication rate. Further, when the necrotic bone is removed, a large space emerges which cannot be completely filled with fibular graft, especially in those with extensive lesion. Rosenwasser et al. described a technique in which the necrotic bone curettage was performed through a window in the femoral head-neck junction and the head was filled with cancellous bone grafts in patients with Ficat stages II and III. They followed the patients for a mean of 12 years and found that 87% remained essentially symptom-free with minimal progression of osteoarthritis (19). Wang et al. treated nontraumatic ONFH (stage II and III-A based on the ARCO classification) with bone impaction grafting through a window made in femoral neck (light bulb procedures) in 138 hips. The necrotic bone was replaced using demineralized bone matrix and auto-iliac bone. Patients were followed for 25.37 months. They found that mean HHS increased significantly from 62 to 79. At the latest follow-up, the treatment was successful in 94 hips (68%). They found radiologic improvement in 100% of patients with stage IIA, 76.67% with stage IIB, and 50.96% with stage IIC and IIIA. HHSs showed that excellent and good results were obtained in 100%, 93.33% and 59.62% of cases with stages IIA, IIB, and IIC and IIIA, respectively. The survival rate was 85% in stages IIA and IIB and 60% in stages IIC and IIIA. There were patients with ectopic ossification, infection and lateral femoral cutaneous injuries. Finally, Wang et al. concluded that this procedure can be effective in treating patients with early to mediate stages of ONFH (9). Furthermore, Zhang et al. evaluated the indications for vascularized iliac bone grafting for treating the osteonecrosis of femoral head and operative result of surgical treatment in 23 hips with osteonecrosis of femoral head who underwent vascularized iliac bone grafting after 31.5 months on average. They demonstrated that vascularized iliac bone grafting was efficient for treatment of ONFH in short and middle term. They recommended the procedure for patients with ONFH in ARCO stages I, IIA, IIB medial and central, and IIC medial (8). In another study, Chen et al. retrospectively analyzed the results of vascularized iliac grafting on ONFH with segmental collapse in 33 hips with ARCO stage IIIA or IIIB. Only 8 (24%) of the 33 hips were preserved. The survival time for all the cases averaged 74 months after the operation. Eighteen of the 26 ARCO stage-IIIA hips required THA, and the survival time for the hips of stage IIIA averaged 85 months. THA was performed for all the seven ARCO stage-IIIB hips and the mean survival time for the stage-IIIB hips was 35 months. Finally, Chen et al. demonstrated that vascularized grafting with the technique described in their study was not appropriate for treatment of ONFH with segmental collapse (3). In spite of other techniques, in the light bulb technique the necrotic bone can be removed nearly completely with visualization of the interior volume of the femoral head using fluoroscopy. In addition, we can completely fill the space of the femoral head with auto-corticocancellous bone graft from the iliac crest. In techniques using the grafts from the fibula, the volume of the graft is not suitable to completely fill the femoral head space. In addition, it is not necessary to perform surgical dislocation of the femoral head which significantly decrease AVN and the invasive nature of the surgery. However, we found that similar to previous studies using the light bulb technique, patients with more advanced stages of ONFH benefited less from the technique and a great percentage of them failed to response to the surgery (35.7%), while the procedure resulted in satisfactory outcomes in earlier stages of ONFH.
Similar to other studies, there were some limitations in our study. We did not compare the results of our technique with those of other techniques. Precollapse stages of ONFH can be successfully treated with removing the necrotic bone and corticocancellous bone grafting through a window made in the anterior surface of femoral neck. This technique is a useful surgical method to overcome the need to early THA, especially in young active populations.
Footnotes
Authors’ Contributions:Study concept and design: Manouchehr Vahid Farahmandi; acquisition of data: Manouchehr Vahid Farahmandi, Mohammadreza Abbasian, Farshad Safdari and Mohammad Emami Moghaddam Tehrani; analysis and interpretation of data: Manouchehr Vahid Farahmandi and Mohammad Emami Moghaddam Tehrani; drafting of the manuscript: Mohammadreza Abbasian and Farshad Safdari; critical revision of the manuscript for important intellectual content: Manouchehr Vahid Farahmandi and Mohammad Emami Moghaddam Tehrani; statistical analysis: Farshad Safdari; administrative, technical, and material support: Manouchehr Vahid Farahmandi, Mohammad Emami Moghaddam Tehrani and Mohammadreza Abbasian; study supervision: Manouchehr Vahid Farahmandi, Mohammadreza Abbasian, Farshad Safdari and Mohammad Emami Moghaddam Tehrani.
References
- 1.Aldridge JM, 3rd, Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. Surgical technique. J Bone Joint Surg Am. 2004;86-A Suppl 1:87–101. doi: 10.2106/00004623-200403001-00012. [DOI] [PubMed] [Google Scholar]
- 2.Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85-A(6):987–93. doi: 10.2106/00004623-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Chen CC, Lin CL, Chen WC, Shih HN, Ueng SW, Lee MS. Vascularized iliac bone-grafting for osteonecrosis with segmental collapse of the femoral head. J Bone Joint Surg Am. 2009;91(10):2390–4. doi: 10.2106/JBJS.H.01814. [DOI] [PubMed] [Google Scholar]
- 4.Fang T, Zhang EW, Sailes FC, McGuire RA, Lineaweaver WC, Zhang F. Vascularized fibular grafts in patients with avascular necrosis of femoral head: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2013;133(1):1–10. doi: 10.1007/s00402-012-1627-z. [DOI] [PubMed] [Google Scholar]
- 5.Roush TF, Olson SA, Pietrobon R, Braga L, Urbaniak JR. Influence of acetabular coverage on hip survival after free vascularized fibular grafting for femoral head osteonecrosis. J Bone Joint Surg Am. 2006;88(10):2152–8. doi: 10.2106/JBJS.E.00469. [DOI] [PubMed] [Google Scholar]
- 6.Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77(5):674–80. doi: 10.2106/00004623-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Veillette CJ, Mehdian H, Schemitsch EH, McKee MD. Survivorship analysis and radiographic outcome following tantalum rod insertion for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88 Suppl 3:48–55. doi: 10.2106/JBJS.F.00538. [DOI] [PubMed] [Google Scholar]
- 8.Zhang NF, Li ZR, Zhang XZ, Wang W. [Vascularized iliac bone grafting for avascular necrosis of the femoral head]. Zhonghua Wai Ke Za Zhi. 2003;41(2):125–9. [PubMed] [Google Scholar]
- 9.Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, et al. Treatment of nontraumatic osteonecrosis of the femoral head using bone impaction grafting through a femoral neck window. Int Orthop. 2010;34(5):635–9. doi: 10.1007/s00264-009-0822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baksi DP, Pal AK, Baksi DD. Long-term results of decompression and muscle-pedicle bone grafting for osteonecrosis of the femoral head. Int Orthop. 2009;33(1):41–7. doi: 10.1007/s00264-007-0455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999;81(2):200–9. doi: 10.2106/00004623-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Cao B, Liu YH, Wang Y, Zhang SP, Wang JG, Yang ZL. [Clinical application of minimally invasive core decompression combined with impaction bone grafting to the treatment of femoral head necrosis]. Zhongguo Gu Shang. 2010;23(2):111–3. [PubMed] [Google Scholar]
- 13.Gangji V, Hauzeur JP. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells. Surgical technique. J Bone Joint Surg Am. 2005;87 Suppl 1(Pt 1):106–12. doi: 10.2106/JBJS.D.02662. [DOI] [PubMed] [Google Scholar]
- 14.Guerra-Vélez P, Cano-Egea JM, García-F. D. Trapdoor technique in femoral head osteonecrosis. Rev esp cir ortop traumatol. 2010;54(4):248–50. [Google Scholar]
- 15.Korompilias AV, Beris AE, Lykissas MG, Kostas-Agnantis IP, Soucacos PN. Femoral head osteonecrosis: why choose free vascularized fibula grafting. Microsurgery. 2011;31(3):223–8. doi: 10.1002/micr.20837. [DOI] [PubMed] [Google Scholar]
- 16.Shuler MS, Rooks MD, Roberson JR. Porous tantalum implant in early osteonecrosis of the hip: preliminary report on operative, survival, and outcomes results. J Arthroplasty. 2007;22(1):26–31. doi: 10.1016/j.arth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Zhao D, Wang B, Guo L, Yang L, Tian F. Will a vascularized greater trochanter graft preserve the necrotic femoral head? Clin Orthop Relat Res. 2010;468(5):1316–24. doi: 10.1007/s11999-009-1159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canale Terry S, Beaty JH, editors. Campbell's operative orthopaedics. Hip pain in the young adult and hip preservative surgery. 12th ed. Vol. 3. Philadelphia, USA: Elsevier Mosby; 2013. pp. 333–73. [Google Scholar]
- 19.Rosenwasser MP, Garino JP, Kiernan HA, Michelsen CB. Long term followup of thorough debridement and cancellous bone grafting of the femoral head for avascular necrosis. Clin Orthop Relat Res. 1994;(306):17–27. [PubMed] [Google Scholar]
- 20.Gardeniers JWM. Report of the Committee of Staging and Nomenclature. ARCO News Letter. 1993;5(2):79–82. [Google Scholar]
- 21.Gomez-Garcia F. [Review of non-surgical treatment of avascular necrosis of the femoral head]. Acta Ortop Mex. 2013;27(4):265–72. [PubMed] [Google Scholar]
- 22.Alves EM, Angrisani AT, Santiago MB. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol. 2009;28(11):1247–51. doi: 10.1007/s10067-009-1231-y. [DOI] [PubMed] [Google Scholar]
- 23.Rajpura A, Wright AC, Board TN. Medical management of osteonecrosis of the hip: a review. Hip Int. 2011;21(4):385–92. doi: 10.5301/HIP.2011.8538. [DOI] [PubMed] [Google Scholar]
- 24.Windisch C, Kolb W, Rohner E, Wagner M, Roth A, Matziolis G, et al. Invasive electromagnetic field treatment in osteonecrosis of the femoral head: a prospective cohort study. Open Orthop J. 2014;8:125–9. doi: 10.2174/1874325020140515001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mao Q, Jin H, Liao F, Xiao L, Chen D, Tong P. The efficacy of targeted intraarterial delivery of concentrated autologous bone marrow containing mononuclear cells in the treatment of osteonecrosis of the femoral head: a five year follow-up study. Bone. 2013;57(2):509–16. doi: 10.1016/j.bone.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernigou P, Poignard A, Zilber S, Rouard H. Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop. 2009;43(1):40–5. doi: 10.4103/0019-5413.45322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta AK, Frank RM, Harris JD, McCormick F, Mather RC, Nho SJ. Arthroscopic-assisted core decompression for osteonecrosis of the femoral head. Arthrosc Tech. 2014;3(1):e7–e11. doi: 10.1016/j.eats.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck DM, Park BK, Youm T, Wolfson TS. Arthroscopic treatment of labral tears and concurrent avascular necrosis of the femoral head in young adults. Arthrosc Tech. 2013;2(4):e367–71. doi: 10.1016/j.eats.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]