Abstract
Background
The American Heart Association Get With the Guidelines (GWTG) program has improved care quality of acute myocardial infarction (AMI) with important implications for other countries in the world. This study evaluated the incidence and care of AMI in Taiwan and assessed the compliance of GWTG in Taiwan.
Methods and Results
We used the Taiwan National Health Insurance Research Database (1999–2008) to identify hospitalized patients ≥18 years of age presenting with AMI. The temporal trends of annual incidence and care quality of AMI were evaluated. The age‐adjusted incidence of AMI (/100 000 person‐years) increased from 28.0 in 1999 to 44.4 in 2008 (P<0.001). The use of guideline‐based medications for AMI was evaluated. The use of dual antiplatelet therapy (DAPT) increased from 65% in 2004 to 83.9% in 2008 (P<0.001). Angiotensin‐converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) was used in 72.6% in 2004 and 71.7% in 2008 (P=NS) and β‐blocker was used in 60% in 2004 and 59.7% in 2008 (P=NS). Statin use increased from 32.1% to 50.1% from 2004 to 2008 (P<0.001). The in‐hospital mortality decreased from 15.9% in 1999 to 12.3% in 2008 (P<0.0001). Multivariable analysis showed that DAPT, ACE inhibitor/ARB, β‐blocker, and statin use during hospitalization were all associated with reduced in‐hospital mortality in our AMI patients.
Conclusions
AMI incidence was increasing, but the guideline‐based medications for AMI were underutilized in Taiwan. Quality improvement programs, such as GWTG, should be promoted to improve AMI care and outcomes in Taiwan.
Keywords: epidemiology, incidence, myocardial infarction, population
Introduction
cute myocardial infarction (AMI) is a common cardiovascular disease that carries a high fatality rate. Important medical and interventional treatments with beneficial effects on reducing morbidity and mortality of AMI have been proved in randomized clinical trials and incorporated into clinical guidelines.1–2 Currently, AMI has been selected as a disease for performance monitoring in many Western countries. In the United States, the Get With the Guidelines (GWTG) program has been initiated by the American Heart Association to improve guideline adherence for patients hospitalized with AMI.3 Participation in GWTG could increase the use of evidence‐based treatments, enhance the adherence to practice guidelines, and improve the prognosis in patients.4 The success of the GWTG program has improved the quality of AMI care with important implications for other countries in the world. However, healthcare expenditures are different across countries around the world and could influence the compliance with GWTG standards in countries other than the United States. In Taiwan, healthcare expenditure constitutes about 6% of the gross domestic product and is about half of that in the United States.5 The mean cost of each AMI hospitalization in Taiwan is only about one third the mean cost of those in the United States.6–7 The overall incidence of AMI has declined over the past decade in the United States,8 but the temporal trend of AMI incidence in Taiwan is unknown. Since the implementation of National Health Insurance (NHI) in Taiwan in 1995, more than 98% of Taiwan's 23 million population has received healthcare coverage from this system.9 NHI data provide us an opportunity to evaluate the use of GWTG performance measures for AMI in Taiwan and assess whether they can become international standards in taking care of AMI patients across national and economic boundaries. In the present study, we used NHI data from 1999 through 2008 and sought to (1) analyze the secular trends in annual incidence of AMI in Taiwan, and (2) assess the use of evidence‐based therapies after AMI as compared with Asian American AMI patients during a similar study period.10
Methods
Database
This study used claims data from the 1999 to 2008 National Health Insurance Research Database provided by the National Health Research Institute in Taiwan. The National Health Insurance Research Database includes data on every inpatient admission covered under the NHI program, which has enrolled nearly 99% of the Taiwanese population (23 million residents) and contracted with 97% of hospitals and clinics throughout the nation.9 The databases used in this study included all inpatient and outpatient medical claims between January 1, 1999 and December 31, 2008. From the databases, we can retrieve medical information including disease diagnosis, prescription drugs, procedures, and surgery incurred during a hospitalization or at an outpatient visit. For electronic processing in the NHI in Taiwan, all the healthcare service providers are requested to submit the diagnosis information using International Classification of Disease‐Clinical Modification, ninth revision together with service claims.
Study Design
We selected all adult patients (≥18 years) who were admitted to hospitals for AMI from January 1, 1999 to December 31, 2008. AMI admission was defined as a hospitalization with a primary or secondary discharge diagnosis code of ICD9‐CM 410.x. We retained only those patients who were admitted at an acute‐care hospital. To avoid the possibility of wrongly selecting into the study patients who had not actually experienced an AMI (eg, prior AMI patients who were admitted for a diagnostic or therapeutic intervention and still coded for AMI), we excluded patients who were coded as AMI and survived but were hospitalized for < 2 days. For each patient, the comorbidities were retrieved from both the inpatient and outpatient claim databases for 12 months before the index date. We obtained information on each patient's age at the index MI admission, gender, days of hospitalization, and the use of AMI‐related interventional procedures, including percutaneous coronary interventions (PCI) and coronary artery bypass graft. We specifically looked at the 4 performance measures during hospitalization according to the current guideline1: (1) use of dual antiplatelet therapy (DAPT); (2) use of angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs); (3) use of β‐blockers; and (4) use of statins. The composite performance measure of “four‐combined care” was defined as the proportion of patients who received all the above 4 performance measures. During the same hospitalization, we also evaluated whether patients received other invasive procedures including ventilator support, intra‐aortic balloon pump, and extracorporeal membrane oxygenation. We respectively ascertained medication use in‐hospital and in the 180 days prior to the index date as proxies for several comorbidities using the anatomic therapeutic chemical classification system: oral antidiabetic drugs, insulin; several cardiovascular drug classes (α‐blockers, β‐blockers, calcium channel blockers, ACE inhibitors, ARBs, other antihypertensives, diuretics, nitrates, digitalis, vitamin K antagonist, statins, fibrates); medications indicated for asthma or chronic obstructive pulmonary disease (inhaled corticosteroids, β‐receptor agonists); drugs reducing gastroesophageal reflux or ulcer disease (H2‐blockers, proton pump inhibitors, sucralfate, antacids); pain medications (nonsteroidal anti‐inflammatory drugs, selective cyclo‐oxygenase‐2 inhibitors, opioids, and others); oral corticosteroids; and several psychoactive drug classes (benzodiazepines or anxiolytics, antidepressants, antipsychotics).
Comorbid Diseases
For each patient, the comorbidities for AMI were retrieved from both the inpatient and outpatient claims databases for 1 year before and during the index AMI hospitalization. Several proven diseases predisposing patients to AMI and other comorbidities were based on International Classification of Disease‐Clinical Modification, ninth revision codes (Table S1). Hormone therapy included hormone replacement therapy and oral contraceptive use indicating the use of estrogen and/or progesterone. Chronic lung disease included emphysema, chronic bronchitis, bronchiectasis, other obstructive pulmonary disease, and chronic respiratory failure. Serious neurologic diseases encompassed stroke or other central and peripheral nervous disease with associated extremity paresis or paralysis.
Statistical Analysis
The scale of the disease incidence for 10 years was examined by separation into attack and incidence, and the scale of disease incidence according to gender and age was also investigated. Age was classified into 4 groups (18 to 54, 55 to 64, 65 to 79, and ≥80) and the ages of patients in each year were also calculated. The attack rate was calculated by dividing the number of total episodes (total attacks) by the population number, and the same patients could produce several attacks. The incidence rates were determined by dividing the number of patients with first attacks throughout their entire lives by the population number every year. The estimates of Taiwan's civilian resident population from the Taiwan Department of Statistics for the years 1999 through 2008 were used to calculate the age‐ and gender‐specific attack and incidence of AMI per 100 000 population. This study evaluated the attack and incidence according to years and examined the trend of the disease incidence. By considering characteristics of population structure each year, age standardization was performed. The standardized population for age standardization was calculated by adding the population numbers from 1999 to 2008 according to age groups each year. A Poisson regression model was used to examine the temporal trends in the annual incidence of AMI, with categorical year variables. Trends in continuous variables and categorical data by calendar period were analyzed using Spearman nonparametric correlation analysis. We used a logistic regression model to quantify the effects on in‐hospital mortality of age, gender, comorbidity (respiratory disease, diabetes, cancer, cerebrovascular disease, peripheral arterial disease, hypertension, heart failure, atrial fibrillation, and renal failure), revascularization procedures (PCI or coronary artery bypass graft), and use of ventilator, intra‐aortic balloon pump, and extracorporeal membrane oxygenation. Men and women are considered separately in the models because gender was a significant predictor of outcome and because of an interaction previously seen between age and gender in the outcome after an AMI. All variables were entered simultaneously into the models. All of the tests were 2‐tailed, and a P<0.05 was considered statistically significant. We used SAS statistical software (version 9.1; SAS Institute, Cary, NC) for data collection and all statistical analyses.
Results
Baseline Characteristics
The study included 108 741 patients (78 779 male, 72.4%) enrolled from January 1, 1999 to December 31, 2008. The clinical characteristics and in‐hospital treatment of AMI between male and female patients are shown in Table 1. Compared with male patients, females were older and had a higher prevalence of hypertension, diabetes mellitus, and dyslipidemia. Female patients also had more comorbidities, including coronary artery disease, atrial fibrillation, stroke/transient ischemic attack, chronic lung disease, and chronic renal disease. However, for in‐hospital treatment of AMI, female patients received significantly less AMI standard therapies, including aspirin, β‐blocker, ACE inhibitor or ARB, statin, and PCI.
Table 1.
Clinical Characteristics and Treatment of AMI in Taiwan From 1999 to 2008
| Overall N=108 741 | Male N=78 779 | Female N=29 962 | P Value | |
|---|---|---|---|---|
| Age, y (SD) | 66.3 (13.4) | 64.2 (13.5) | 71.9 (11.5) | <0.001 |
| Risk factors, % | ||||
| Hypertension | 64.4 | 59.4 | 77.8 | <0.001 |
| Diabetes mellitus | 37.8 | 32.3 | 52.1 | <0.001 |
| Dyslipidemia | 32.2 | 29.8 | 38.6 | <0.001 |
| Cardiovascular history, % | ||||
| Coronary artery disease | 47.5 | 45.4 | 52.9 | <0.001 |
| Atrial fibrillation | 3.2 | 2.7 | 4.8 | <0.001 |
| Peripheral artery disease | 2.6 | 2.1 | 3.7 | <0.001 |
| Stroke | 11.9 | 10.8 | 14.9 | <0.001 |
| Comorbidity, % | ||||
| Chronic lung disease | 32.2 | 31.3 | 34.6 | <0.001 |
| Chronic renal disease | 18.9 | 16.6 | 24.7 | <0.001 |
| Cancer | 15.5 | 14.9 | 17.2 | <0.001 |
| Peptic ulcers | 22.9 | 21.4 | 26.6 | <0.001 |
| In‐hospital drug use | ||||
| Aspirin | 94.7 | 95.2 | 93.5 | <0.001 |
| Clopidogrel | 63.2 | 63.3 | 62.8 | 0.1 |
| Ticlopidine | 11.4 | 12.0 | 9.7 | <0.001 |
| GP IIbIIa inhibitor | 14.4 | 15.9 | 10.6 | <0.001 |
| DAPT | 64.4 | 65.6 | 61.0 | <0.001 |
| β‐Blocker | 60.0 | 60.5 | 58.5 | <0.001 |
| ACEI or ARB | 73.1 | 73.2 | 72.6 | 0.056 |
| Statin | 33.3 | 33.9 | 31.9 | <0.001 |
| In‐hospital procedure or surgery | ||||
| Ventilator support | 8.0 | 6.8 | 11.1 | <0.001 |
| IABP | 4.8 | 5.1 | 4.3 | <0.001 |
| ECMO | 0.4 | 0.5 | 0.3 | <0.001 |
| PCI | 49.0 | 52.7 | 39.4 | <0.001 |
| CABG | 6.4 | 6.8 | 5.5 | <0.001 |
Data are presented as N (%) or mean values±SD. P value compared with male and female groups using a Student t test or χ2 test. ACEI indicates angiotensin‐converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft; DAPT, dual antiplatelet therapy; ECMO, extracorporeal membrane oxygenation; GP, Glycoprotein; IABP, intra‐aortic balloon pumping; PCI, percutaneous coronary intervention.
Attack Rate and Incidence of AMI
When the crude attack rate for AMI was investigated according to year, there was an increase by ≈2.1 times from 30.1 cases per 100 000 persons in 1999 to 62.4 cases per 100 000 persons in 2008. The crude incident rate for AMI increased by 2.0 times from 27.5 cases per 100 000 persons in 1999 to 55.7 cases per 100 000 persons in 2008. In comparing the attack rate and incidence for each year according to gender and age, males showed higher rates than females and both of the rates became higher with older ages. The overall age‐adjusted attack rate of AMI (/100 000 person‐years) increased 1.6‐fold, from 30.7 in 1999 to 48.3 in 2009 (P<0.001) (Figure 1). The overall age‐adjusted incidence of AMI (/100 000 person‐years) markedly increased 1.6‐fold, from 28.0 in 1999 to 44.4 in 2008 (P<0.001) (Figure 2). When age‐adjusted attack rates and incidences were compared according to year, there was also an increasing tendency during these years. This tendency was the same even after males and females were separated (Figures 1 and 2). The average age of the male and female AMI patients in the whole period was 64.2±13.5 and 71.9±11.5 years, respectively. In males, the age‐adjusted incidence of AMI (/100 000 person‐years) significantly increased 1.5‐fold, from 41.8 in 1999 to 62.5 in 2008 (P<0.001), while in females, it tended to similarly increase 1.8‐fold, from 13.5 in 1999 to 26.0 in 2008 (P<0.001). In men, the annual incidence of AMI drastically increased in patients older than 40 years. However, the significant increase in annual incidence of AMI in women occurred in patients older than 60 years (Figure 3). The overall increase in AMI incidence was predominantly driven by the increase of AMI in older individuals. Overall, AMI incidence per 100 000 young individuals (<65 years) increased 1.3% per year in men and 0.9% per year in women from 1999 to 2008, but it increased 3.2% per year in men and 3.5% per year in women in old individuals (>65 years) (Figure 4A and 4B).
Figure 1.
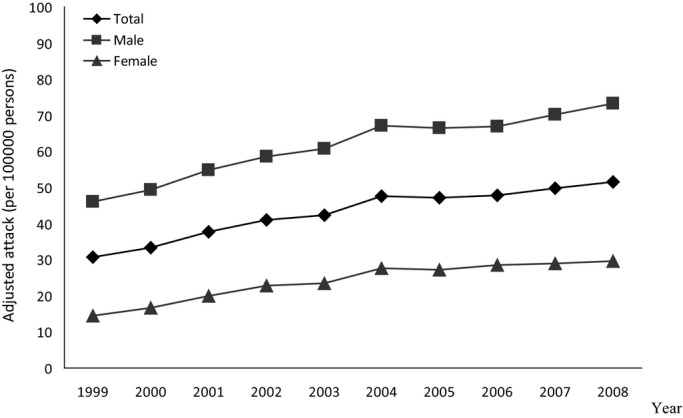
Age‐adjusted attack rates (/100 000 person‐years) of acute myocardial infarction has increased over the last 10 years by gender.
Figure 2.
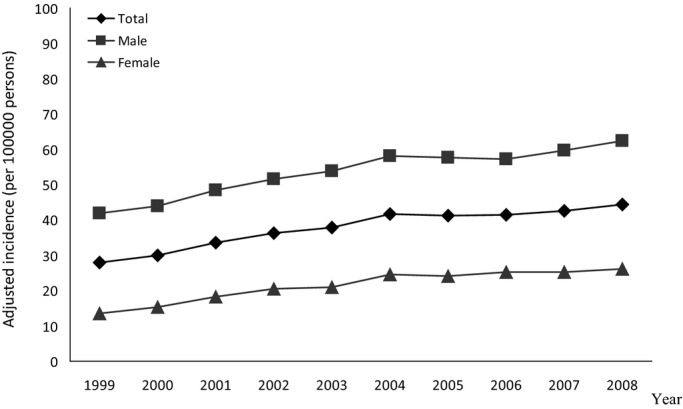
Age‐adjusted incidence (/100 000 person‐years) of acute myocardial infarction has increased over the last 10 years by gender.
Figure 3.
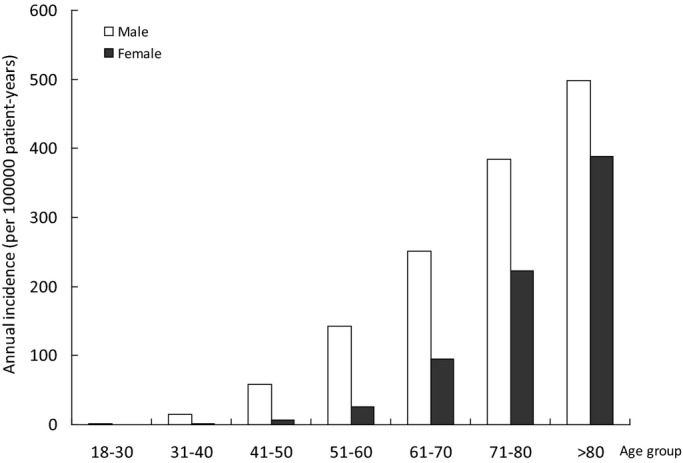
Age‐ and gender‐specific incidence of acute myocardial infarction over the last 10 years.
Figure 4.
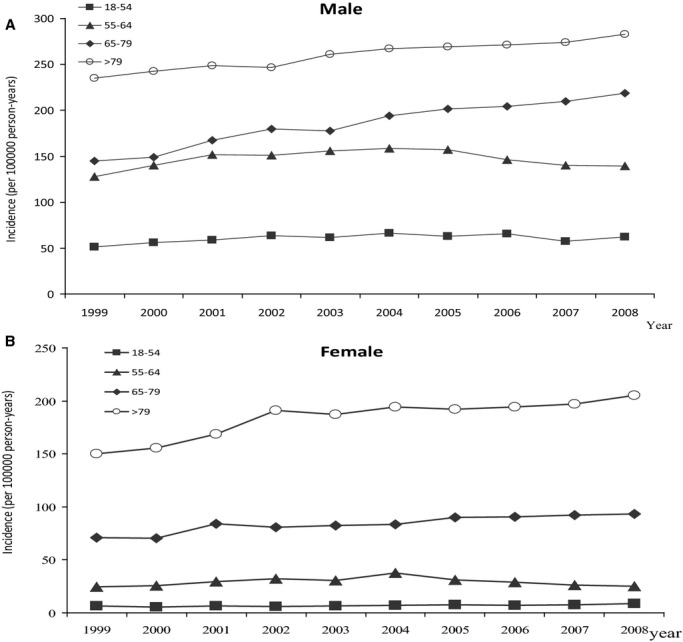
Serial changes in the age distribution of patients with acute myocardial infarction by gender: (A) male and (B) female.
Temporal Trends of Clinical Characteristics
We separated the study period into 3 periods and observed the temporal trends of AMI clinical features in Taiwan. During the study periods, there was an increase of the mean age for AMI hospitalization. The percentage of female AMI patients was also increasing. The prevalence of risk factors for AMI including hypertension, diabetes mellitus, and dyslipidemia increased markedly. Atrial fibrillation and chronic renal disease also increased significantly (Table 2).
Table 2.
Temporal Trends of Clinical Characteristics for AMI Patients From 1999 to 2008
| Period 1 (1999–2002) N=32 356 | Period 2 (2003–2005) N=34 561 | Period 3 (2006–2008) N=41 824 | |
|---|---|---|---|
| Age, y | 65.5 (12.9) | 66.5 (13.3)* | 66.9 (13.8)** |
| Male | 74.6 | 72.0* | 71.2** |
| Risk factors, % | |||
| Hypertension | 55.2 | 67.7* | 68.8** |
| Diabetes mellitus | 30.5 | 39.8* | 41.6** |
| Dyslipidemia | 22.3 | 33.3* | 36.8** |
| Cardiovascular history, % | |||
| Coronary artery disease | 34.3 | 39.9* | 37.8** |
| Atrial fibrillation | 2.0 | 3.6* | 4.0** |
| Peripheral artery disease | 1.4 | 2.7* | 3.3** |
| Stroke | 9.1 | 13.1* | 13.2* |
| Comorbidity, % | |||
| Chronic lung disease | 38.9 | 48.3* | 43.9** |
| Chronic renal disease | 11.5 | 17.0* | 18.1** |
| Cancer | 10.7 | 15.5* | 15.8* |
| Peptic ulcers | 17.8 | 25.7* | 24.5** |
Data are presented as N (%) or mean values±SD. AMI indicates acute myocardial infarction.
P value (<0.05) compared with Period 2 and Period 1 groups or Period 3 and Period 1 groups using a Student t test or χ2 test.
P value (<0.05) compared with Period 3 and Period 2 groups using a Student t test or χ2 test.
Temporal Trends of Care Quality and Clinical Outcome
For the 4 performance measures during hospitalization according to the current guideline, only the use of DAPT and statin increased significantly. There were no significant changes for the use of ACE inhibitor or ARB and β‐blocker (Table 3). From 2004 to 2008, DAPT increased from 65% in 2004 to 83.9% in 2008 (P<0.001). ACE inhibitors or ARB were used in 72.6% in 2004 and 71.7% in 2008 (P=NS) and β‐blocker was used in 60% in 2004 and 59.7% in 2008 (P=NS). Statin use increased from 32.1% to 50.1% from 2004 to 2008 (P<0.001). The proportion of patients who received “four‐combined care” increased from 2004 to 2008 (Figure 5). In 2008, the 4 major performance measures for AMI during hospitalization in Taiwan significantly fell behind those reported in Asian Americans (aspirin, 93.7% versus 96.5%; ACE inhibitor or ARB, 72.3% versus 91.9%; β‐blocker, 60.2% versus 96.0%; and statin 46.1% versus 93.1%).10 For in‐hospital procedure or surgery, there was an increased use of PCI for AMI during hospitalization in Taiwan, but the coronary artery bypass graft rate did not decrease significantly. In addition, more AMI patients received the support of a ventilator, intra‐aortic balloon pump, or extracorporeal membrane oxygenation during hospitalization (Table 3). The duration of hospital stay was significantly shortened over the 10‐year study period; the prevalence of discharge within 7 days after the onset of AMI significantly increased from 48.5% in 1999 to 57.2% in 2008 (P<0.0001).
Table 3.
Temporal Trends of Treatments for AMI Patients From 1999 to 2008
| Period 1 (1999–2002) N=32 356 | Period 2 (2003–2005) N=34 561 | Period 3 (2006–2008) N=41 824 | |
|---|---|---|---|
| In‐hospital drug use, % | |||
| Aspirin | 97.4 | 93.6* | 93.7* |
| Clopidogrel | 11.5 | 69.2* | 88.0** |
| Ticlopidine | 31.3 | 4.7* | 1.5** |
| GP IIbIIIa inhibitor | 8.8 | 17.5* | 16.3** |
| DAPT | 39.3 | 66.1* | 82.4** |
| β‐Blocker | 59.0 | 60.7* | 60.1* |
| ACEI or ARB | 73.2 | 74.0* | 72.2** |
| Statin | 18.0 | 32.7* | 45.7** |
| Four‐combined care | 10.4 | 19.3* | 26.5** |
| In‐hospital procedure or surgery | |||
| Ventilator support | 4.3 | 9.5* | 9.6** |
| IABP | 3.4 | 4.8* | 6.0** |
| ECMO | 0.1 | 0.3* | 0.7** |
| PCI | 40.6 | 48.3* | 56.2** |
| CABG | 5.9 | 6.9* | 6.4** |
Data are presented as N (%). ACEI indicates angiotensin‐converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft; DAPT, dual antiplatelet therapy; ECMO, extracorporeal membrane oxygenation; GP, Glycoprotein; IABP, intra‐aortic balloon pumping; PCI, percutaneous coronary intervention.
P value (<0.05) compared with Period 2 and Period 1 groups or Period 3 and Period 1 groups using a Student t test or χ2 test.
P value (<0.05) compared with Period 3 and Period 2 groups using a Student t test or χ2 test.
Figure 5.
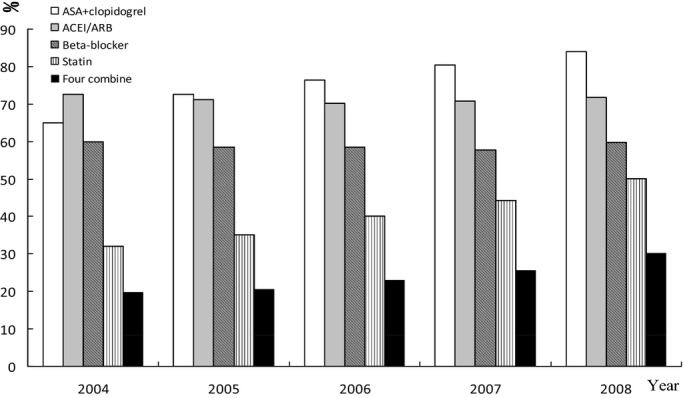
Serial changes in the use of guideline‐based medications for acute myocardial infarction: 2004–2008. ACEI indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; ASA, acetylsalicylic acid.
The overall in‐hospital mortality rate has markedly decreased from 20% in 1999 to 8% in 2008 (P<0.0001) (Figure 6). However, the mortality of female patients was always significantly higher than male patients over the 10‐year study period. In 2008, the in‐hospital mortality was 10.6% for males and 17.2% for females. Multivariable logistic regression analysis demonstrated that the determinants of in‐hospital death in AMI patients in Taiwan included old age, female gender, hypertension, diabetes mellitus, old MI, and old stroke (Table 4). We also found that in‐hospital use of DAPT (odds ratio [OR] 0.75, 95% CI 0.70 to 0.80), ACE inhibitor/ARB (OR 0.44, 95% CI 0.41 to 0.46), β‐ blocker (OR 0.69, 95% CI 0.66 to 0.74), statin (OR 0.62, 95% CI 0.58 to 0.66), and PCI (OR 0.61, 95% CI 0.57 to 0.65) were associated with significantly lower in‐hospital mortality.
Figure 6.
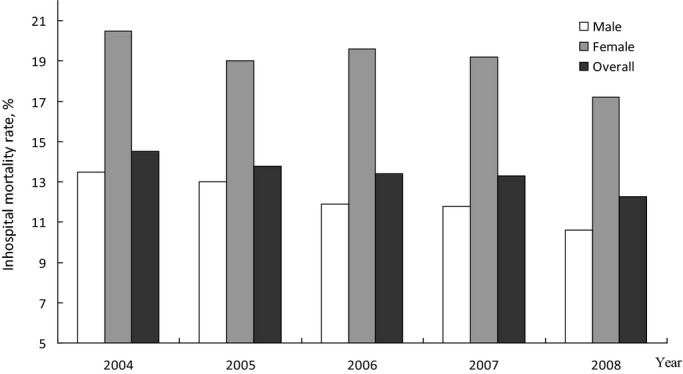
In‐hospital mortality rate of acute myocardial infarction by gender: 2004–2008.
Table 4.
Multivariable Logistic Regression Analysis of Variables Associated With In‐Hospital Mortality
| Clinical Characteristics | Odds Ratio (95% CI) |
|---|---|
| Male | 0.86 (0.81 to 0.91) |
| Age, y | |
| 45 to 54 vs Ref (<45) | 1.27 (1.01 to 1.59) |
| 55 to 64 vs Ref | 1.85 (1.50 to 2.29) |
| 65 to 69 vs Ref | 3.56 (2.90 to 4.36) |
| >69 vs Ref | 6.20 (5.05 to 7.63) |
| Hypertension | 1.10 (1.02 to 1.18) |
| Diabetes mellitus | 1.33 (1.25 to 1.40) |
| Old myocardial infarction | 1.10 (1.03 to 1.18) |
| Old stroke | 1.29 (1.21 to 1.39) |
| In‐hospital medical therapy | |
| Dual antiplatelet use | 0.75 (0.70 to 0.80) |
| ACEI/ARB | 0.44 (0.41 to 0.46) |
| β‐Bblocker | 0.69 (0.66 to 0.74) |
| Statin | 0.62 (0.58 to 0.66) |
| In‐hospital procedures | |
| Ventilator | 6.66 (6.23 to 7.11) |
| IABP | 4.74 (4.32 to 5.20) |
| ECMO | 12.15 (9.39 to 15.72) |
| Percutaneous coronary intervention | 0.61 (0.57 to 0.65) |
| Coronary artery bypass graft | 1.21 (1.09 to 1.34) |
ACEI indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; ECMO, extracorporeal membrane oxygenation; IABP, intra‐aortic balloon pumping.
Discussion
The major findings of this study were the following: (1) AMI attack rates and incidence were still rising in the 10‐year study period in Taiwan, and the AMI incidence was higher in men than women in all age groups; (2) guideline‐based medications for AMI were underused in Taiwan; (3) female patients had higher in‐hospital mortality rates and received less guideline‐based treatment for AMI; and (4) the improvement of AMI mortality with guideline‐based treatment in Taiwan reflects that GWTG performance measures can also be applied in Taiwan to improve AMI care quality.
The epidemiological characteristics and real‐world practice for AMI have not been well studied in Asian countries despite its importance in public health. Most of the available information comes from the data in highly selected medical centers or from AMI treatment networks rather than in an unselected nationwide database. Our study is a 10‐year nationwide population‐based cohort study that clearly demonstrates the temporal trends of epidemiological features and management of AMI in Taiwan. The overall age‐adjusted incidence of AMI (/100 000 person‐years) increased from 28.0 in 1999 to 41.3 in 2008, indicating a steady trend of increased AMI incidence in Taiwan. The rising incidence of AMI in Taiwan is completely different from that reported from Western countries and Japan. Data from the Unites States,8,11 Sweden,12 and the Netherlands13 with study periods similar to our study demonstrated a significant decline of AMI incidence after the year 2000. In Japan, data from the MIYAGI‐AMI study demonstrated that AMI incidence progressively increased from 1979, but after 2000, AMI incidence reached a stable state and there was no further increase of AMI incidence in Miyagi Prefecture.14 In Kumamoto Prefecture in Japan, a steady trend of decreasing incidence of AMI after 2004 was observed in the Kumamoto Acute Coronary Events study.15 Although the AMI incidence in Taiwan is still lower than that in Western countries, it is already higher than the incidence in Japan (40.7 versus 27.0/100 000 person‐years in 2008).14
The rising incidence of AMI in Taiwan is related to the aging population,16 as demonstrated by the increased trend of AMI incidence being most obvious in the old‐age group. However, the increased prevalence of risk factors in Taiwan, such as diabetes mellitus17 and cholesterol18 and the low hypertension control rate,19 also plays an important role. The link between control of major coronary risk factors and the reduction of AMI incidence has been reported in previous studies.20–21 More effort should be put into risk‐factor control in our population to attenuate the rising incidence of AMI in Taiwan.
Concerning guideline‐based medications for AMI, our study shows that there was continued improvement in the temporal use of DAPT and statins from 1999 to 2008 in Taiwan, but there was no further improvement in the use of ACE inhibitors or ARB and β‐blockers. In 2008, 83.9% of patients received DAPT, 71.7% received an ACE inhibitor or ARB, 59.7% received β‐blockers, 50.1% received statins, and 30.3% received the 4‐combination therapy during hospitalization for AMI in Taiwan. Overall, the guideline‐based medications for AMI were significantly underused in Taiwan when compared with the data reported from the United States, especially for β‐blockers and statins. In 2006, data from the National Registry of Myocardial Infarction in the United States demonstrated that 94% of patients received aspirin, 74% received an ACE inhibitor or ARB, 92% received β‐blockers, and 88% received lipid‐lowering agents.22 In another survey of 4412 Asian Americans in the GWTG program in 2008, the use of guideline‐based medications for AMI was even higher: 94% of patients received aspirin, 78% received an ACE inhibitor or ARB, 94% received β‐blockers, and 91% received lipid‐lowering agents.10 In other Asian countries, β‐blockers and statins are also less prescribed than in the United States. In Japan,23 49.5% received β‐blockers and 77.8% received statins, and in Korea,24 72.7% received β‐blockers and 77.2% received statins for AMI treatment. According to the Taiwan NHI regulation before August 2013, statins were indicated in AMI patients with serum low‐density lipoprotein levels >130 mg/dL or total cholesterol >200 mg/dL. We thought that this regulation could be an important factor in the low use of statins in Taiwan's AMI patients. The Taiwan Acute Coronary Syndrome registry study reviewed 2744 AMI patients from October 2008 to January 2010 and found there was also no evident improvement in using guideline‐based medications for AMI after 2008. Only 77.2% of AMI patients received DAPT, 64.7% received ACE inhibitor or ARB, 55.2% received β‐blockers, and 62.5% received statins during hospitalization.25 Our study clearly demonstrated the benefit of using guideline‐based medications to reduce the in‐hospital mortality rate of AMI in Taiwan. Increasing the prescription rate of guideline‐based medications through quality‐improvement programs such as GWTG and revision of regulations regarding statin use are necessary to enhance adherence to the guidelines in the treatment of AMI in Taiwan.
The major strength of our study is that the nationwide population‐based data we used could provide more accurate assessment of incidence and treatment conditions of AMI in Taiwan. Currently, we are trying to differentiate ST‐segment elevation and non‐ST‐segment elevation MI in our database. Therefore, the differences of incidence and guideline‐based therapies between ST‐segment elevation and non‐ST‐segment elevation MI in Taiwan need further studies. In our database, only revascularization procedures were recorded and there was no detailed information of door‐to‐balloon time for primary PCI. The Taiwan Acute Coronary Syndrome registry study reported that 95.4% of our patients with ST‐segment elevation MI received primary PCI and the median door‐to‐balloon time was 96 minutes at that time.25 Whether there is any improvement of this performance measure for AMI care will require future registry study in Taiwan.
In conclusion, there was a progressive increase of AMI incidence in Taiwan from 1999 to 2008. Underutilization of the guideline‐based medications for AMI is a major problem in Taiwan. The influences of guideline‐based medications on in‐hospital mortality of AMI in Taiwan present an important clinical implication that quality‐improvement programs, such as GWTG, are necessary to enhance adherence to the guidelines in the treatment of AMI in Taiwan.
Supplementary Material
Appendix World Health Organization International Classification of Diseases, Ninth Revision.
Sources of Funding
This study was funded by AstraZeneca, Taiwan and National Cheng Kung University Hospital, Tainan, Taiwan (NCKUH‐10101002). The funding organizations had no role in the design, performance, or analysis of this study or decision to submit the manuscript for publication.
Disclosures
None.
Acknowledgments
We are grateful for the generosity of the Taiwan Bureau of National Health Insurance, Department of Health for giving us access to the National Health Insurance Research Database.
References
- 1.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DXCF/AHA Task Force. ACCF/AHA Guideline for the Management of ST‐Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart 7 Association Task Force on Practice Guidelines. Circulation. 2013; 127:529-555. [DOI] [PubMed] [Google Scholar]
- 2.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, II, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Jneid H, Ettinger SM, Ganiats TG, Lincoff AM, Philippides GJ, Zidar JPAmerican College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e663-e828. [DOI] [PubMed] [Google Scholar]
- 3.Somma KA, Bhatt DL, Fonarow GC, Cannon CP, Cox M, Laskey W, Peacock WF, Hernandez AF, Peterson ED, Schwamm L, Saxon LA. Guideline adherence after ST‐segment elevation versus non‐ST segment elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012; 5:654-661. [DOI] [PubMed] [Google Scholar]
- 4.Peterson ED, Shah BR, Parsons L, Pollack CV, Jr, French WJ, Canto JG, Gibson CM, Rogers WJ. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008; 156:1045-1055. [DOI] [PubMed] [Google Scholar]
- 5.Lu JF, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff (Millwood). 2003; 22:77-88. [DOI] [PubMed] [Google Scholar]
- 6.Kauf TL, Velazquez EJ, Crosslin DR, Weaver WD, Diaz R, Granger CB, McMurray JJ, Rouleau JL, Aylward PE, White HD, Califf RM, Schulman KA. The cost of acute myocardial infarction in the new millennium: evidence from a multinational registry. Am Heart J. 2006; 151:206-212. [DOI] [PubMed] [Google Scholar]
- 7.Chen CS, Liu TC, Chiu WT, Lin HC. Impact of hospital and physician characteristics on medical expenditures for acute myocardial infarction hospitalization. Int J Cardiol. 2007; 121:127-129. [DOI] [PubMed] [Google Scholar]
- 8.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010; 362:2155-2165. [DOI] [PubMed] [Google Scholar]
- 9.Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, Nolte E. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010; 10:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qian F, Ling FS, Deedwania P, Hernandez AF, Fonarow GC, Cannon CP, Peterson ED, Peacock WF, Kaltenbach LA, Laskey WK, Schwamm LH, Bhatt DLGet With The Guidelines Steering Committee and Investigators. Care and outcomes of Asian‐American acute myocardial infarction patients: findings from the American Heart Association Get With The Guidelines‐Coronary Artery Disease program. Circ Cardiovasc Qual Outcomes. 2012; 5:126-133. [DOI] [PubMed] [Google Scholar]
- 11.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010; 123:259-266. [DOI] [PubMed] [Google Scholar]
- 12.Dudas K, Lappas G, Stewart S, Rosengren A. Trends in out‐of‐hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation. 2011; 123:46-52. [DOI] [PubMed] [Google Scholar]
- 13.Koopman C, Bots ML, van Oeffelen AA, van Dis I, Verschuren WM, Engelfriet PM, Capewell S, Vaartjes I. Population trends and inequalities in incidence and short‐term outcome of acute myocardial infarction between 1998 and 2007. Int J Cardiol. 2013; 168:993-998. [DOI] [PubMed] [Google Scholar]
- 14.Takii T, Yasuda S, Takahashi J, Ito K, Shiba N, Shirato K, Shimokawa HMIYAGI‐AMI Study Investigators. Trends in acute myocardial infarction incidence and mortality over 30 years in Japan: report from the MIYAGI‐AMI Registry Study. Circ J. 2010; 74:93-100. [DOI] [PubMed] [Google Scholar]
- 15.Kojima S, Matsui K, Ogawa HKumamoto Acute Coronary Events (KACE) Study Group. Temporal trends in hospitalization for acute myocardial infarction between 2004 and 2011 in Kumamoto, Japan. Circ J. 2013; 77:2841-2843. [DOI] [PubMed] [Google Scholar]
- 16.Lin MH, Chou MY, Liang CK, Peng LN, Chen LK. Population aging and its impacts: strategies of the health‐care system in Taipei. Ageing Res Rev. 2010; 9suppl 1:S23-S27. [DOI] [PubMed] [Google Scholar]
- 17.Lin CC, Li CI, Hsiao CY, Liu CS, Yang SY, Lee CC, Li TC. Time trend analysis of the prevalence and incidence of diagnosed type 2 diabetes among adults in Taiwan from 2000 to 2007: a population‐based study. BMC Public Health. 2013; 9:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, Watanabe M, Kadota A, Okuda N, Kadowaki T, Nakamura Y, Okamura T. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702-2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Su TC, Bai CH, Chang HY, You SL, Chien KL, Chen MF, Chen HJ, Pan WH, Tseng CH, Cheng SH, Hurng BS, Hwang LC, Chen CJ. Evidence for improved control of hypertension in Taiwan: 1993‐2002. J Hypertens. 2008; 26:600-606. [DOI] [PubMed] [Google Scholar]
- 20.Hardoon SL, Whincup PH, Lennon LT, Wannamethee SG, Capewell S, Morris RW. How much of the recent decline in the incidence of myocardial infarction in British men can be explained by changes in cardiovascular risk factors? Evidence from a prospective population‐based study. Circulation. 2008; 117:598-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nedkoff LJ, Briffa TG, Preen DB, Sanfilippo FM, Hung J, Ridout SC, Knuiman M, Hobbs M. Age‐ and sex‐specific trends in the incidence of hospitalized acute coronary syndromes in Western Australia. Circ Cardiovasc Qual Outcomes. 2011; 4:557-564. [DOI] [PubMed] [Google Scholar]
- 22.Peterson ED, Shah BR, Parsons L, Pollack CV, Jr, French WJ, Canto JG, Gibson CM, Rogers WJ. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008; 156:1045-1055. [DOI] [PubMed] [Google Scholar]
- 23.Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, Kimura T, Matsubara T, Ikari Y, Kimura K, Tsukahara K, Origasa H, Morino Y, Tsutsui H, Kobayashi M, Isshiki TPACIFIC investigators. Management and two‐year long‐term clinical outcome of acute coronary syndrome in Japan: prevention of atherothrombotic incidents following ischemic coronary attack (PACIFIC) registry. Circ J. 2013; 77:934-943. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Yang DH, Park HS, Cho Y, Jeong MH, Kim YJ, Kim KS, Hur SH, Seong IW, Hong TJ, Cho MC, Kim CJ, Jun JE, Park WH, Chae SCKorea Acute Myocardial Infarction Registry Investigators. Suboptimal use of evidence‐based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010; 159:1012-1019. [DOI] [PubMed] [Google Scholar]
- 25.Shyu KG, Wu CJ, Mar GY, Hou JC, Li AH, Wen MS, Lai WT, Lin SJ, Kuo CT, Hwang JJ, Chiang FT. Clinical characteristics, management and in‐hospital outcomes of patients with acute coronary syndrome: observations from the Taiwan ACS Full Spectrum Registry. Acta Cardiol Sin. 2011; 27:135-144. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix World Health Organization International Classification of Diseases, Ninth Revision.


