Abstract
Background
A subset of patients hospitalized with acute heart failure experiences worsening clinical status and requires escalation of therapy. Worsening heart failure is an end point in many clinical trials, but little is known about its prevalence in clinical practice and its associated outcomes.
Methods and Results
We analyzed inpatient data from the Acute Decompensated Heart Failure National Registry linked to Medicare claims to examine the prevalence and outcomes of patients with worsening heart failure, defined as the need for escalation of therapy at least 12 hours after hospital presentation. We compared patients with worsening heart failure to patients with an uncomplicated hospital course and patients with a complicated presentation. Of 63 727 patients hospitalized with acute heart failure, 11% developed worsening heart failure. These patients had the highest observed rates of mortality, all‐cause readmission, and Medicare payments at 30 days and 1 year after hospitalization (P < 0.001 for all comparisons). The adjusted hazards of 30‐day mortality were 2.56 (99% CI, 2.34 to 2.80) compared with an uncomplicated course and 1.29 (99% CI, 1.17 to 1.42) compared with a complicated presentation. The adjusted cost ratios for postdischarge Medicare payments at 30 days were 1.35 (99% CI, 1.24 to 1.46) compared with an uncomplicated course and 1.11 (99% CI, 1.02 to 1.22) compared with a complicated presentation.
Conclusions
In‐hospital worsening heart failure was common and was associated with higher rates of mortality, all‐cause readmission, and postdischarge Medicare payments. Prevention and treatment of in‐hospital worsening heart failure represents an important goal for patients hospitalized with acute heart failure.
Keywords: healthcare costs, heart failure, mortality, patient outcome assessment, patient readmission
Introduction
Hospitalization for acute heart failure is common and is associated with substantial morbidity and mortality. In the United States, acute heart failure leads to over 1 million hospitalizations annually,1 and the 1‐year mortality rate after a heart failure hospitalization ranges from 20% to 30%.2–3 A subset of patients hospitalized with acute heart failure experience worsening heart failure during the hospitalization, typically defined as persistent or worsening signs or symptoms requiring an escalation of therapy. Worsening heart failure has been an end point in many clinical trials of acute heart failure therapies,4–8 but limited data exist regarding the prevalence of worsening heart failure in clinical practice and its associated outcomes.
We performed a retrospective, observational study using data from the Acute Decompensated Heart Failure National Registry (ADHERE) linked to fee‐for‐service Medicare administrative claims. Our objective was to describe the prevalence of in‐hospital worsening heart failure in this large, multicenter US registry and to describe the associated mortality, rates of readmission, and postdischarge Medicare payments.
Methods
Data Sources
Acute Decompensated Heart Failure National Registry was a large, multicenter registry of patients hospitalized with acute heart failure.9–10 More than 300 community and academic medical centers in the United States participated in the registry, and data were collected on more than 185 000 patients between January 2001 and March 2006. Registry data include demographic characteristics, comorbid conditions, medications, hospital course, laboratory test results, procedures, and discharge disposition. We obtained standard analytic files for fee‐for‐service Medicare beneficiaries from the US Centers for Medicare & Medicaid Services.
We identified registry patients in the Medicare claims data by first linking registry hospitalizations to Medicare inpatient claims. The process used to link the registry data and the Medicare claims data has been described previously.11 We obtained payment and health care utilization information from Medicare inpatient, outpatient facility, and professional claims and enrollment and mortality information from the Medicare denominator files. The institutional review board of the Duke University Health System approved the study.
Study Population
We included patients 65 years and older who had a registry hospitalization between January 1, 2001 and December 31, 2004 that was linked to fee‐for‐service Medicare claims data. We did not include registry hospitalizations from 2005 or 2006 because detailed information about inotrope use was not collected in those years. For patients with multiple linked hospitalizations, we selected the first as the index hospitalization. We excluded patients who were admitted on an elective basis for the index hospitalization. We also excluded patients who did not have fee‐for‐service Medicare coverage for at least 6 months before the index hospitalization.
Study Groups
We categorized patients into 3 groups according to their experience during the index hospitalization: patients with a complicated hospital presentation, patients with in‐hospital worsening heart failure, and patients with an uncomplicated hospital course. We classified patients as having a complicated hospital presentation if they met any of the following criteria: initiated inotropic medications or an intravenous vasodilator within 12 hours of presentation to the hospital, were admitted initially to the intensive care unit, or received advanced medical therapy (ie, mechanical circulatory support, mechanical ventilation, or hemodialysis) on the first inpatient day. We classified patients as having in‐hospital worsening heart failure if they met any of the following criteria: initiated inotropic medications or an intravenous vasodilator more than 12 hours after hospital presentation, were transferred to the intensive care unit, or received advanced medical therapy after the first inpatient day. We classified the remaining patients as having an uncomplicated hospital course.
Outcomes
The outcomes of interest were mortality, readmission, and postdischarge Medicare payments. Specifically, we estimated the unadjusted and adjusted associations between each study group and all‐cause mortality, all‐cause readmission, heart failure readmission, days alive and out of the hospital, and postdischarge Medicare payments at both 30 days and 1 year. We also measured hospital length of stay, in‐hospital mortality, and Medicare payments to the hospital for the index hospitalization for each study group.
We determined the index hospitalization date, length of stay, and in‐hospital mortality from the Medicare index hospitalization claims. We determined mortality during the follow‐up period using death dates in the Medicare denominator files, measuring from the date of admission for the index hospitalization. We identified readmissions from subsequent inpatient Medicare claims and measured time to readmission from the date of discharge for the index hospitalization. Readmission for heart failure was based on subsequent inpatient claims with a primary diagnosis of heart failure (International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis code 428.x, 402.x1, 404.x1, or 404.x3). We excluded patients who died in the hospital, left against medical advice, or were discharged or transferred to another short‐term hospital or hospice from the measurement and reporting of readmission, days alive and out of the hospital, and postdischarge Medicare payments. We determined total days alive and out of the hospital after discharge based on the death date, if present, and the duration of all subsequent hospitalizations during the follow‐up period. Medicare payments after discharge from the index hospitalization included payments for inpatient, outpatient, and professional claims. We report these payments in 2010 US dollars with inflation adjustment using the Consumer Price Index medical care component. We excluded patients who enrolled in Medicare managed care during the follow‐up period from the measurement and reporting of days alive and out of the hospital and postdischarge Medicare payments.
Patient Characteristics
We used information from the registry to describe patient demographic characteristics, medical history, findings from the initial evaluation, vital signs, laboratory test results, and admission and discharge medications. We used Medicare claims from the 6 months before the index admission to identify previous heart failure hospitalizations (International Classification of Diseases, Ninth Revision, Clinical Modification primary diagnosis code 428.x, 402.x1, 404.x1, or 404.x3).
Statistical Analysis
We describe baseline characteristics of the study population by study group, using frequencies with percentages for categorical variables and means with SDs for continuous variables. We tested for differences between the groups using χ2 tests for categorical variables and Kruskal–Wallis tests for continuous variables.
Most variables in the registry had few to no missing values. Exceptions included smoking status, B‐type natriuretic peptide level on presentation, and left ventricular ejection fraction. For those variables, we treated missing values as a separate category, labeled “unknown.” Missing data in other variables occurred <5% of the time. We imputed these missing values to the median value for continuous variables, to “no” for dichotomous variables, and to the modal value for other categorical variables.12
We present the observed outcomes by study group. We present in‐hospital mortality using frequencies and percentages, and we use χ2 tests to test for differences between the groups. We present length of stay, days alive out of the hospital, and Medicare payments using means with SDs or medians with interquartile ranges, and we used Kruskal–Wallis tests to test for differences between the groups. Calculations of the incidence of mortality at 30 days and 1 year were based on Kaplan–Meier estimates, and we used log‐rank tests to test for differences between the groups. For both readmission outcomes, we estimated incidence at 30 days and 1 year using the cumulative incidence function, which accounts for the competing risk of mortality, and we tested for differences between the groups using Gray tests.13
For estimates of unadjusted and adjusted hazard ratios for each study group comparison for mortality, all‐cause readmission, and heart failure readmission at 30 days and 1 year, we used Cox proportional hazards models. We used robust standard errors to account for clustering of patients within hospitals. We used linear mixed models to estimate the unadjusted and adjusted differences between the groups in the number of days alive and out of the hospital. We estimated unadjusted and adjusted ratios for average postdischarge Medicare payments between the groups using generalized linear mixed models with a log link and a Poisson error distribution that allowed for overdispersion. In all of the mixed models, we estimated hospital‐level random intercepts to account for clustering of patients within hospitals. All unadjusted models included only the study group indicators. The adjusted models also controlled for patient baseline demographic characteristics, medical history, findings from the initial evaluation, vital signs, laboratory test results, and medications. We performed sensitivity analyses that categorized patients receiving early intravenous vasodilators as uncomplicated (instead of complicated) and excluded from the analysis patients with secondary diagnoses of acute myocardial infarction, pneumonia, or sepsis/septicemia.
Because of the number of outcomes in the study, we used α=0.01 to establish statistical significance and we report 99% CIs. We used SAS version 9.3 (SAS Institute Inc., Cary, NC) for all analyses.
Results
The study population included 63 727 patients. Of these, 7032 (11.0%) developed in‐hospital worsening heart failure, 15 361 (24.1%) had a complicated hospital presentation, and 41 334 (64.9%) had an uncomplicated hospital course. Table 1 shows the baseline characteristics of the study population. Patients with worsening heart failure were younger and more likely to be male than patients in the other study groups. Some comorbid conditions were more common among patients with worsening heart failure, such as anemia, chronic kidney disease, diabetes mellitus, and peripheral vascular disease. Patients with worsening heart failure were also more likely to have a history of reduced left ventricular ejection fraction and a heart failure hospitalization in the preceding 6 months. On initial evaluation, patients with in‐hospital worsening heart failure tended to have lower systolic blood pressure, higher serum creatinine level, and higher B‐type natriuretic peptide level.
Table 1.
Baseline Characteristics of the Study Population
| Characteristic | Worsening Heart Failure (n=7032) | Complicated Hospital Presentation (n=15 361) | Uncomplicated Hospital Course (n=41 334) | P Value |
|---|---|---|---|---|
| Age, mean (SD), y | 78.0 (7.3) | 78.3 (7.4) | 80.3 (7.8) | <0.001 |
| Male, n (%) | 3515 (50.0) | 7224 (47.0) | 16 678 (40.3) | <0.001 |
| Race, n (%) | <0.001 | |||
| Black | 822 (11.7) | 1947 (12.7) | 4802 (11.6) | |
| White | 5948 (84.6) | 12 875 (83.8) | 35 343 (85.5) | |
| Other or unknown | 262 (3.7) | 539 (3.5) | 1189 (2.9) | |
| Medical history, n (%) | ||||
| Anemia | 4245 (60.4) | 7997 (52.1) | 22 165 (53.6) | <0.001 |
| Atrial fibrillation | 2480 (35.3) | 5117 (33.3) | 14 957 (36.2) | <0.001 |
| Chronic kidney disease | 3036 (43.2) | 5332 (34.7) | 9415 (22.8) | <0.001 |
| COPD or asthma | 2210 (31.4) | 4606 (30.0) | 12 358 (29.9) | 0.03 |
| Coronary artery disease | 4581 (65.1) | 10 123 (65.9) | 23 492 (56.8) | <0.001 |
| Devices, n (%) | ||||
| Any pacemaker | 1484 (21.1) | 3024 (19.7) | 7521 (18.2) | <0.001 |
| Biventricular pacemaker | 237 (3.4) | 500 (3.3) | 785 (1.9) | <0.001 |
| Implantable cardioverter‐defibrillator | 514 (7.3) | 1110 (7.2) | 1547 (3.7) | <0.001 |
| Diabetes mellitus | 3223 (45.8) | 6695 (43.6) | 15 921 (38.5) | <0.001 |
| Heart failure hospitalization, past 6 months | 1315 (18.7) | 2577 (16.8) | 5204 (12.6) | <0.001 |
| Hyperlipidemia | 2712 (38.6) | 5969 (38.9) | 14 031 (33.9) | <0.001 |
| Hypertension | 5233 (74.4) | 11 468 (74.7) | 30 343 (73.4) | 0.005 |
| Left ventricular ejection fraction | <0.001 | |||
| <40% | 3335 (47.4) | 6668 (43.4) | 13 045 (31.6) | |
| ≥40% | 2815 (40.0) | 6237 (40.6) | 19 955 (48.3) | |
| Unknown | 882 (12.5) | 2456 (16.0) | 8334 (20.2) | |
| Peripheral vascular disease | 1645 (23.4) | 3153 (20.5) | 7304 (17.7) | <0.001 |
| Prior myocardial infarction | 2381 (33.9) | 5459 (35.5) | 11 765 (28.5) | <0.001 |
| Prior stroke or transient ischemic attack | 1397 (19.9) | 2835 (18.5) | 7942 (19.2) | 0.03 |
| Smoking status | <0.001 | |||
| Never smoked | 2938 (41.8) | 6304 (41.0) | 18 565 (44.9) | |
| Former smoker | 2717 (38.6) | 5731 (37.3) | 14 459 (35.0) | |
| Initial evaluation and laboratory test results | ||||
| BNP level, mean (SD), pcg/mL | 1492.7 (1247.0) | 1401.7 (1212.9) | 991.0 (949.7) | <0.001 |
| Unknown BNP level, n. (%) | 3372 (48.0) | 7646 (49.8) | 21 298 (51.5) | |
| Dyspnea, n (%) | 6303 (89.6) | 14 033 (91.4) | 36 686 (88.8) | <0.001 |
| Fatigue, n (%) | 2499 (35.5) | 4892 (31.8) | 12 678 (30.7) | <0.001 |
| Hemoglobin level, mean (SD), g/dL | 12.0 (2.3) | 12.4 (2.5) | 12.2 (2.3) | <0.001 |
| Pulmonary edema, n (%) | 6122 (87.1) | 13 805 (89.9) | 35 738 (86.5) | <0.001 |
| Pulse mean (SD), bpm | 86.7 (21.7) | 90.6 (24.0) | 85.7 (21.0) | <0.001 |
| Rales, n (%) | 4832 (68.7) | 11 363 (74.0) | 28 454 (68.8) | <0.001 |
| Serum creatinine level, mean (SD), mg/dL | 2.2 (1.6) | 2.0 (1.6) | 1.4 (0.8) | <0.001 |
| Chronic kidney disease, n (%) | <0.001 | |||
| Stage 1 (eGFR ≥90 mL/min per 1.73 m2) | 235 (3.3) | 587 (3.8) | 2403 (5.8) | |
| Stage 2 (eGFR 60 to 89 mL/min per 1.73 m2) | 1213 (17.2) | 3173 (20.7) | 11 998 (29.0) | |
| Stage 3 (eGFR 30 to 59 mL/min per 1.73 m2) | 3134 (44.6) | 7443 (48.5) | 21 065 (51.0) | |
| Stage 4 (eGFR 15 to 29 mL/min per 1.73 m2) | 1606 (22.8) | 2729 (17.8) | 5128 (12.4) | |
| Stage 5 (eGFR <15 mL/min per 1.73 m2) | 844 (12.0) | 1429 (9.3) | 740 (1.8) | |
| Serum sodium level, mean (SD), mmol/L | 137.6 (5.1) | 138.0 (4.8) | 138.3 (4.7) | <0.001 |
| Systolic blood pressure, mean (SD), mm Hg | 137.7 (30.9) | 148.2 (37.5) | 145.8 (29.6) | <0.001 |
| Systolic blood pressure, n (%) | <0.001 | |||
| <140 mm Hg | 3924 (55.8) | 6817 (44.4) | 18 209 (44.1) | |
| ≥140 mm Hg | 3108 (44.2) | 8544 (55.6) | 23 125 (55.9) | |
| Admission medications, n (%) | ||||
| ACE inhibitor or ARB | 3348 (47.6) | 7829 (51.0) | 20 232 (48.9) | <0.001 |
| Aspirin | 2793 (39.7) | 6425 (41.8) | 16 125 (39.0) | <0.001 |
| β‐Blocker | 3484 (49.5) | 8194 (53.3) | 19 753 (47.8) | <0.001 |
| Clopidogrel | 825 (11.7) | 2036 (13.3) | 4432 (10.7) | <0.001 |
| Diuretic | 4897 (69.6) | 10 181 (66.3) | 28 358 (68.6) | <0.001 |
| Lipid‐lowering agent | 2419 (34.4) | 5572 (36.3) | 13 042 (31.6) | <0.001 |
| Warfarin | 1767 (25.1) | 3740 (24.3) | 10 515 (25.4) | 0.03 |
| Discharge medications, n (%)* | ||||
| ACE inhibitor or ARB | 3145 (56.7) | 8417 (63.2) | 24 506 (63.3) | <0.001 |
| Aspirin | 2746 (49.5) | 6961 (52.3) | 17 961 (46.4) | <0.001 |
| β‐Blocker | 3465 (62.5) | 8542 (64.2) | 22 056 (57.0) | <0.001 |
| Clopidogrel | 873 (15.7) | 2298 (17.3) | 4822 (12.5) | <0.001 |
| Diuretic | 4202 (75.8) | 10 771 (80.9) | 34 087 (88.1) | <0.001 |
| Lipid‐lowering agent | 2067 (37.3) | 5185 (38.9) | 12 706 (32.8) | <0.001 |
| Warfarin | 1657 (29.9) | 3593 (27.0) | 10 920 (28.2) | <0.001 |
| Year of hospitalization, n (%) | <0.001 | |||
| 2001 | 196 (2.8) | 449 (2.9) | 1300 (3.1) | |
| 2002 | 2269 (32.3) | 4735 (30.8) | 13 827 (33.5) | |
| 2003 | 2635 (37.5) | 5537 (36.0) | 15 387 (37.2) | |
| 2004 | 1932 (27.5) | 4640 (30.2) | 10 820 (26.2) |
ACE indicates angiotensin‐converting enzyme; ARB, angiotensin II receptor blocker; BNP, B‐type natriuretic peptide; COPD, chronic obstructive pulmonary disease; eGFR, estimated glomerular filtration rate according to the Modification of Diet in Renal Disease Study equation.
Data are presented for patients discharged alive only, including 5546 patients with worsening heart failure, 13 314 patients with complicated hospital presentation, and 38 708 patients with uncomplicated hospital course.
Table 2 shows the care received during the index hospitalization by patients with worsening heart failure and patients with a complicated hospital presentation. The use of inotropic medications and hemodialysis were more common among patients with worsening heart failure, whereas the use of intravenous vasodilators was more common among patients with a complicated hospital presentation.
Table 2.
Care Received During the Index Hospitalization*
| Resource | Worsening Heart Failure | Complicated Hospital Presentation | P Value |
|---|---|---|---|
| Hemodialysis, n (%) | 1239 (17.6) | 1448 (9.4) | <0.001 |
| Inotropic medication, n (%) | 2723 (38.7) | 3639 (23.7) | <0.001 |
| Intensive care unit, n (%) | 2871 (40.8) | 7623 (49.6) | <0.001 |
| Intra‐aortic balloon pump, n (%) | 77 (1.1) | 99 (0.6) | <0.001 |
| Intravenous vasodilator, n (%) | 3263 (46.4) | 9724 (63.3) | <0.001 |
| Mechanical ventilation, n (%) | 945 (13.4) | 1937 (12.6) | 0.09 |
Fewer than 10 patients in each group received a left ventricular assist device and were not included in the table. Patients with an uncomplicated hospital course did not receive any of the listed therapies during the hospital stay.
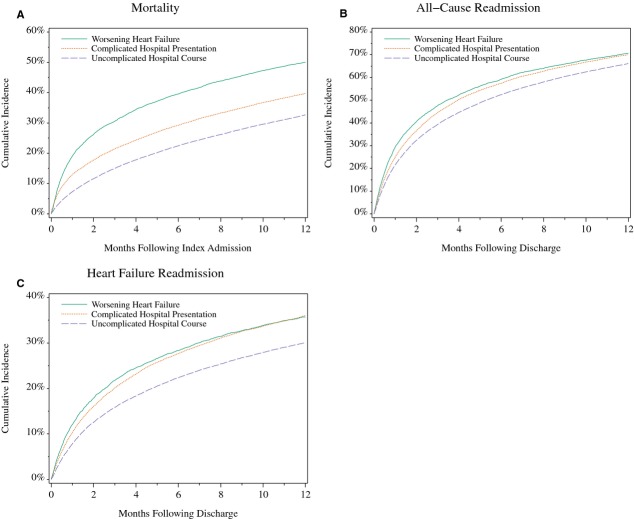
Table 3 presents the observed outcomes. For all measured variables, patients with worsening heart failure had the poorest outcomes at both 30 days and 1 year. The observed mortality rates for patients with worsening heart failure (19.0% at 30 days and 50.1% at 1 year) were higher than the rates for patients with an uncomplicated hospital course (7.3% and 32.7%, respectively) and patients with a complicated presentation (12.9% and 39.7%, respectively). Patients with worsening heart failure also had the highest rates of all‐cause readmission (29.2% at 30 days and 70.6% at 1 year), compared with patients with an uncomplicated hospital course (21.4% and 66.1%, respectively) and patients with a complicated presentation (24.8% and 70.1%, respectively). The mean hospital length of stay was longest for patients with worsening heart failure (10.0 days), compared with patients with an uncomplicated hospital course (4.8 days) and patients with a complicated presentation (6.3 days). The median Medicare payments after discharge (adjusted for inflation to 2010 US dollars) for patients with worsening heart failure were $1045 (interquartile range, 237 to 8026) at 30 days and $19 642 (interquartile range, 6609 to 49 013) at 1 year and were higher than those among patients with an uncomplicated hospital course and patients with a complicated presentation. Patients with worsening heart failure also had the highest rate of in‐hospital mortality, the highest Medicare facility payments for the index hospitalization, the highest rates of heart failure readmission at 30 days and 1 year, and the fewest days alive and out of the hospital at 30 days and 1 year. The Figure shows the Kaplan–Meier estimates of mortality, all‐cause readmission, and heart failure readmission at 1 year.
Table 3.
Observed Outcomes
| Outcome | Worsening Heart Failure (n=7032) | Complicated Hospital Presentation (n=15 361) | Uncomplicated Hospital Course (n=41 334) | P Value |
|---|---|---|---|---|
| Length of stay, mean (SD), days | 10.0 (8.5) | 6.3 (5.4) | 4.8 (3.5) | <0.001 |
| Medicare hospital payments, median (IQR), $* | 7581 (5946 to 13 534) | 6746 (5550 to 9309) | 6308 (5385 to 7934) | <0.001 |
| In‐hospital mortality, No. (%) | 893 (12.7) | 1090 (7.1) | 951 (2.3%) | <0.001 |
| Mortality, n (cumulative incidence) | ||||
| 30‐day | 1336 (19.0) | 1976 (12.9) | 3002 (7.3%) | <0.001 |
| 1‐year | 3514 (50.1) | 6084 (39.7) | 13 446 (32.7%) | <0.001 |
| Discharged alive, n* | 5546 | 13 314 | 38 708 | |
| All‐cause readmission, n (%)* | ||||
| 30‐day | 1620 (29.2) | 3301 (24.8) | 8264 (21.4%) | <0.001 |
| 1‐year | 3911 (70.6) | 9305 (70.1) | 25 502 (66.1%) | <0.001 |
| Heart failure readmission, n (%)* | ||||
| 30‐day | 665 (12.0) | 1355 (10.2) | 2997 (7.7%) | <0.001 |
| 1‐year | 1975 (35.7) | 4782 (36.0) | 11 585 (30.0%) | <0.001 |
| Discharged alive and not censored at 30 days, No.* | 5544 | 13 308 | 38 684 | |
| Days alive and out of the hospital, mean (SD) | 26.5 (6.8) | 27.4 (5.9) | 27.9 (5.3) | <0.001 |
| Total postdischarge Medicare payments* | ||||
| Mean (SD) | 6510 (15 317) | 5152 (12 456) | 3830 (10 932) | <0.001 |
| Median (IQR) | 1045 (237 to 8026) | 544 (173 to 6261) | 375 (145 to 2054) | |
| Patients discharged alive and not censored at 1 year, n* | 5494 | 13 173 | 38 182 | |
| Days alive and out of the hospital, mean (SD) | 252.1 (135.9) | 275.3 (125.2) | 285.7 (120.0) | <0.001 |
| Total postdischarge medicare payments* | ||||
| Mean (SD) | 35 159 (44 228) | 31 524 (41 371) | 24 456 (33 804) | <0.001 |
| Median (IQR) | 19 642 (6609 to 49 013) | 17 379 (5506 to 42 817) | 13 199 (3811 to 32 051) |
IQR, interquartile range.
Adjusted for inflation to 2010 US dollars.
Excludes patients who died in the hospital, left against medical advice, or were discharged or transferred to another short‐term hospital or hospice.
Presented as the number of patients (cumulative incidence per 100 patients at risk) who were readmitted within 30 days after discharge from the index hospitalization.
Excludes patients who died in the hospital, left against medical advice, were discharged or transferred to another short‐term hospital or hospice, or enrolled in Medicare managed care during the follow‐up period.
Figure 1.
Observed all‐cause mortality, all‐cause readmission, and heart failure readmission among patients hospitalized with acute heart failure. A, Kaplan–Meier estimates of all‐cause mortality at 1 year after admission from the index hospitalization for patients with a complicated hospital presentation, patients with in‐hospital worsening heart failure, and patients with an uncomplicated hospital course. P < 0.001 for all comparisons. B, Kaplan–Meier estimates of all‐cause readmission at 1 year after discharge from the index hospitalization for patients with a complicated hospital presentation, patients with in‐hospital worsening heart failure, and patients with an uncomplicated hospital course. P < 0.001 for the comparison between worsening heart failure and uncomplicated hospital course. P = 0.009 for the comparison between worsening heart failure and complicated hospital presentation. C, Kaplan–Meier estimates for heart failure readmission at 1 year after discharge from the index hospitalization for patients with a complicated hospital presentation, patients with in‐hospital worsening heart failure, and patients with an uncomplicated hospital course. P < 0.001 for the comparison between worsening heart failure and uncomplicated hospital course. P = 0.86 for the comparison between worsening heart failure and complicated hospital presentation.
Table 4 shows the unadjusted and adjusted associations between the study groups and the observed outcomes. Compared with an uncomplicated hospital course, worsening heart failure was associated with higher mortality at 30 days (adjusted hazard ratio [HR], 2.56; 99% CI, 2.34 to 2.80) and 1 year (adjusted HR, 1.66; 99% CI, 1.58 to 1.74) and higher risks of all‐cause readmission at 30 days (adjusted HR, 1.24; 99% CI, 1.14 to 1.35) and 1 year (adjusted HR, 1.11; 99% CI, 1.05 to 1.16). Worsening heart failure was also independently associated with higher postdischarge Medicare payments at 30 days (adjusted cost ratio, 1.35; 99% CI, 1.24 to 1.46) and 1 year (adjusted cost ratio, 1.13; 99% CI, 1.08 to 1.18), compared with an uncomplicated hospital course. When we compared worsening heart failure with a complicated presentation, we found that worsening heart failure was associated with higher mortality at 30 days (adjusted HR, 1.29; 99% CI, 1.17 to 1.42) and 1 year (adjusted HR, 1.22; 99% CI, 1.14 to 1.30) and higher risks of all‐cause readmission at 30 days (adjusted HR, 1.11; 99% CI, 1.03 to 1.21) but not at 1 year. Compared with a complicated presentation, worsening heart failure was also associated with higher total Medicare payments at 30 days (adjusted cost ratio, 1.11; 99% CI, 1.02 to 1.22) but not at 1 year.
Table 4.
Unadjusted and Adjusted Associations of Study Group and 30‐Day and 1‐Year Outcomes
| Outcome | Unadjusted | Adjusted* | ||
|---|---|---|---|---|
| Hazard Ratio (99% CI) | P Value | Hazard Ratio (99% CI) | P Value | |
| Mortality at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 2.78 (2.55 to 3.04) | <0.001 | 2.56 (2.34 to 2.80) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.84 (1.67 to 2.02) | <0.001 | 1.98 (1.81 to 2.17) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.51 (1.37 to 1.67) | <0.001 | 1.29 (1.17 to 1.42) | <0.001 |
| Mortality at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.84 (1.75 to 1.93) | <0.001 | 1.66 (1.58 to 1.74) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.31 (1.24 to 1.38) | <0.001 | 1.36 (1.29 to 1.43) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.41 (1.32 to 1.50) | <0.001 | 1.22 (1.14 to 1.30) | <0.001 |
| All‐cause readmission at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 1.47 (1.35 to 1.59) | <0.001 | 1.24 (1.14 to 1.35) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.20 (1.13 to 1.27) | <0.001 | 1.12 (1.05 to 1.19) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.23 (1.13 to 1.33) | <0.001 | 1.11 (1.03 to 1.21) | <0.001 |
| All‐cause readmission at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.27 (1.21 to 1.34) | <0.001 | 1.11 (1.05 to 1.16) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.16 (1.12 to 1.20) | <0.001 | 1.09 (1.05 to 1.13) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.10 (1.04 to 1.17) | <0.001 | 1.02 (0.96 to 1.08) | 0.47 |
| Heart failure readmission at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 1.62 (1.43 to 1.84) | <0.001 | 1.26 (1.10 to 1.45) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.34 (1.22 to 1.48) | <0.001 | 1.17 (1.06 to 1.30) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.21 (1.06 to 1.37) | <0.001 | 1.08 (0.95 to 1.22) | 0.13 |
| Heart failure readmission at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.36 (1.26 to 1.47) | <0.001 | 1.14 (1.06 to 1.23) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.28 (1.22 to 1.35) | <0.001 | 1.16 (1.11 to 1.22) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.06 (0.98 to 1.14) | 0.04 | 0.98 (0.92 to 1.06) | 0.53 |
| Days alive and out of the hospital at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | −0.64 (−0.80 to −0.49) | <0.001 | −0.51 (−0.66 to −0.35) | <0.001 |
| Complicated presentation vs uncomplicated course | −0.21 (−0.32 to −0.10) | <0.001 | −0.29 (−0.40 to −0.17) | <0.001 |
| Worsening heart failure vs complicated presentation | −0.43 (−0.61 to −0.26) | <0.001 | −0.22 (−0.39 to −0.05) | 0.001 |
| Days alive and out of the hospital at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | −31.31 (−35.86 to −26.77) | <0.001 | −22.20 (−26.63 to −17.77) | <0.001 |
| Complicated presentation vs uncomplicated course | −9.51 (−12.73 to −6.29) | <0.001 | −11.09 (−14.25 to −7.92) | <0.001 |
| Worsening heart failure vs complicated presentation | −21.80 (−26.86 to −16.75) | <0.001 | −11.11 (−15.92 to −6.30) | <0.001 |
| Cost Ratio (99% CI) | P Value | Cost Ratio (99% CI) | P Value | |
| Total postdischarge Medicare payments at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 1.70 (1.57 to 1.84) | <0.001 | 1.35 (1.24 to 1.46) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.39 (1.31 to 1.49) | <0.001 | 1.21 (1.13 to 1.29) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.22 (1.12 to 1.33) | <0.001 | 1.11 (1.02 to 1.22) | 0.001 |
| Total postdischarge Medicare payments at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.43 (1.37 to 1.49) | <0.001 | 1.13 (1.08 to 1.18) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.33 (1.29 to 1.38) | <0.001 | 1.11 (1.08 to 1.15) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.07 (1.02 to 1.12) | <0.001 | 1.01 (0.97 to 1.06) | 0.45 |
Covariates in the adjusted regression models included demographic characteristics (age, sex, and race); medical history (anemia, atrial fibrillation, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease or asthma, diabetes mellitus, heart failure hospitalization in the past 6 months, hyperlipidemia, hypertension, peripheral vascular disease, prior myocardial infarction, prior stroke or transient ischemic attack, smoking status, pacemaker type, and implantable cardioverter defibrillator); initial evaluation results, vital signs, and laboratory test results (dyspnea, ejection fraction, fatigue, hemoglobin level, pulmonary edema, pulse, rales, serum creatinine level, serum sodium level, and systolic blood pressure); medications (angiotensin‐converting inhibitor or angiotensin II receptor blocker, aspirin, β‐blocker, clopidogrel, diuretic, lipid‐lowering agent, warfarin); and the year of the index hospitalization. The mortality models included medication information from admission; the other models included medication information from discharge.
Includes all patients.
Excludes patients who died in the hospital, left against medical advice, were discharged, or transferred to another short‐term hospital or hospice.
Excludes patients who died in the hospital, left against medical advice, were discharged, or transferred to another short‐term hospital or hospice, or enrolled in Medicare managed care during the follow‐up period.
Sensitivity analyses using different study definitions reclassified a subset of patients from 1 study group to another but did not significantly change the primary outcomes. Table 5 shows the adjusted rates of all‐cause mortality and all‐cause readmission at both 30 days and 1 year when patients who received early intravenous nitroglycerin or any intravenous vasodilator (ie, nitroglycerin, nitroprusside, or nesiritide) were categorized as uncomplicated instead of complicated. Similar findings were observed when patients who had secondary diagnoses of acute myocardial infarction, pneumonia, or sepsis/septicemia (results not shown) were excluded from study.
Table 5.
Adjusted Associations* of Study Group With Modified Study Group Definitions and 30‐Day and 1‐Year Outcomes
| Outcome | Modified Definition 1 (Early IV Nitroglycerin Use Not Considered a Complicated Presentation) | Modified Definition 2 (Any Early IV Vasodilator Use Not Considered a Complicated Presentation) | ||
|---|---|---|---|---|
| Hazard Ratio (99% CI) | P Value | Hazard Ratio (99% CI) | P Value | |
| Mortality at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 2.61 (2.39 to 2.85) | <0.001 | 2.70 (2.48 to 2.94) | <0.001 |
| Complicated presentation vs uncomplicated course | 2.07 (1.90 to 2.26) | <0.001 | 2.20 (1.99 to 2.43) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.26 (1.14 to 1.39) | <0.001 | 1.23 (1.10 to 1.37) | <0.001 |
| Mortality at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.67 (1.59 to 1.75) | <0.001 | 1.69 (1.62 to 1.76) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.39 (1.33 to 1.46) | <0.001 | 1.43 (1.35 to 1.52) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.20 (1.13 to 1.27) | <0.001 | 1.18 (1.10 to 1.27) | <0.001 |
| All‐cause readmission at 30 days* | ||||
| Worsening heart failure vs uncomplicated course | 1.24 (1.15 to 1.35) | <0.001 | 1.24 (1.15 to 1.34) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.10 (1.04 to 1.17) | <0.001 | 1.12 (1.05 to 1.19) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.13 (1.04 to 1.22) | <0.001 | 1.11 (1.02 to 1.21) | <0.001 |
| All‐cause readmission at 1 year* | ||||
| Worsening heart failure vs uncomplicated course | 1.11 (1.06 to 1.17) | <0.001 | 1.11 (1.06 to 1.16) | <0.001 |
| Complicated presentation vs uncomplicated course | 1.07 (1.04 to 1.11) | <0.001 | 1.07 (1.02 to 1.11) | <0.001 |
| Worsening heart failure vs complicated presentation | 1.03 (0.98 to 1.09) | 0.47 | 1.04 (0.98 to 1.10) | 0.07 |
Covariates in the adjusted regression models are the same as in Table 4 and included demographic characteristics (age, sex, and race); medical history (anemia, atrial fibrillation, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease or asthma, diabetes mellitus, heart failure hospitalization in the past 6 months, hyperlipidemia, hypertension, peripheral vascular disease, prior myocardial infarction prior stroke or transient ischemic attack, smoking status, pacemaker type, and implantable cardioverter defibrillator); initial evaluation results, vital signs, and laboratory test results (dyspnea, ejection fraction, fatigue, hemoglobin level, pulmonary edema, pulse, rales, serum creatinine level, serum sodium level, and systolic blood pressure); medications (angiotensin‐converting inhibitor or angiotensin II receptor blocker, aspirin, β‐blocker, clopidogrel, diuretic, lipid‐lowering agent, warfarin); and the year of the index hospitalization. The mortality models included medication information from admission; the other models included medication information from discharge.
Includes all patients.
Excludes patients who died in the hospital, left against medical advice, were discharged, or transferred to another short‐term hospital or hospice.
Discussion
We examined the prevalence and outcomes of in‐hospital worsening heart failure, defined as the need for escalation of therapy at least 12 hours after hospital presentation. Using data from a large clinical registry, we found that worsening heart failure was common among Medicare beneficiaries, affecting 11% of patients hospitalized with acute heart failure. These patients had more complicated and costly hospitalizations, as evidenced by the highest observed rates of in‐hospital mortality, longest lengths of stay, and highest Medicare hospital payments. In‐hospital worsening heart failure was also associated with worse postdischarge outcomes and higher costs, compared with patients with an uncomplicated hospital course and with patients with a complicated presentation. Compared with an uncomplicated hospital course, worsening heart failure was associated with more than a 2‐fold greater risk of mortality at 30 days, a 24% greater risk of all‐cause readmission at 30 days, 35% higher postdischarge Medicare payments at 30 days, and 22 fewer days alive and out of the hospital at 1 year. In addition, compared with a complicated presentation, worsening heart failure was independently associated with a 29% greater risk of mortality at 30 days, an 11% greater risk of all‐cause readmission at 30 days, 11% higher postdischarge Medicare payments at 30 days, and 11 fewer days alive and out of the hospital at 1 year.
In randomized controlled trials of acute heart failure therapies, the prevalence of in‐hospital worsening heart failure in the placebo groups ranged from 5% to 42%.4–8,14 Despite differences in the definitions of worsening heart failure in those studies, worsening heart failure was a consistent marker of greater risk for readmission and mortality.14–15 Our findings represent the first report of a large‐scale, real‐world analysis of the prevalence and outcomes of patients with in‐hospital worsening heart failure. The only other study to assess the prevalence of in‐hospital worsening heart failure outside of clinical trial settings came from a single‐center analysis of 337 patients in Israel.16 That study found in‐hospital worsening heart failure in 29% of patients but used a definition that included escalation of therapy after 6 hours of presentation to the hospital. Similar to our analysis, the study found that in‐hospital worsening heart failure was associated with greater early and late mortality.
Our findings suggest that worsening heart failure during an acute heart failure hospitalization has a strong association with worse in‐hospital and postdischarge outcomes. These findings have important implications for patients hospitalized with acute heart failure. Prevention or early recognition of in‐hospital worsening heart failure may improve patient outcomes and reduce healthcare resource use. Prevention of worsening heart failure has also been reported in acute heart failure clinical trials without a detailed understanding of its implications. Our findings suggest that prevention of in‐hospital worsening heart failure may be an important end point in acute heart failure trials.
On the basis of our findings, we believe that worsening heart failure should be considered in the design of acute heart failure trials. However, a standard definition based on objective criteria is needed. Recent clinical trials have used varying definitions. For example, in the RELAX‐AHF trial, worsening heart failure was defined as the presence of worsening signs or symptoms of heart failure requiring escalation of any intravenous therapy or mechanical support after study drug initiation within 16 hours of presentation.8,17 In the Value of Endothelin Receptor Inhibition With Tezosentan in Acute Heart Failure Study, worsening heart failure was defined as the presence of persistent or worsening signs or symptoms requiring escalation of therapy, or restarting previous therapies, or readmission after discharge, from the initiation of the study drug to 7 days.4,18 Our definition focused on the timing of the initiation of specific medications and advanced medical therapies or transfer to an intensive care unit. This definition may be more reproducible than physician‐ or investigator‐based assessments of worsening heart failure15 and may also be incorporated into clinical trials or quality‐improvement initiatives that use electronic health records for data collection.
Our study has limitations. First, the study population was limited to patients who were enrolled in the Acute Decompensated Heart Failure National Registry from 2001 through 2004 and who were 65 years or older and could be linked to Medicare claims data. The findings may not be generalizable to other patient populations, including younger patients and patients hospitalized during other time periods. Second, our definition of worsening heart failure included evidence for escalation of therapy while hospitalized for heart failure; we were unable to describe the reason for escalation of therapy and cannot be certain all escalation of care was for worsening heart failure. For example, while some patients were hospitalized for acute heart failure, they may have received advanced medical therapies such as mechanical ventilation for a concomitant condition such as pneumonia. Third, we were only able to adjust for variables collected in the registry. Associations between worsening heart failure and poor outcomes may be confounded by measured or unmeasured variables.
Conclusions
In a large, multicenter registry, in‐hospital worsening heart failure was common and was associated with high rates of mortality, readmission, and Medicare payments. Providers should consider the impact of in‐hospital worsening heart failure on prognosis in the hospital and after discharge. In‐hospital worsening heart failure is a target for new treatment strategies and may represent an important end point in clinical trials of acute heart failure therapies.
Sources of Funding
The Acute Decompensated Heart Failure National Registry registry was originally sponsored by Scios, Inc. This project was supported by a research agreement between Novartis Pharmaceuticals Corporation and Duke University. Dr Mentz was supported by grant T32GM086330 from the National Institute of General Medical Sciences.
Disclosures
Drs Sharma and Johnson are employees of Novartis. Dr Fonarow reported serving as a consultant for Bayer, Gambro, Medtronic, and Novartis. Dr Curtis reported receiving research support from Boston Scientific, Bristol‐Myers Squibb, GE Healthcare, GlaxoSmithKline, Johnson & Johnson, Medtronic, Merck, and Novartis. Dr Hernandez reported receiving research support from the American Heart Association, Amgen, and Novartis.
Acknowledgments
Damon M. Seils, MA, Duke University, provided editorial assistance and prepared the manuscript. He did not receive compensation for his assistance apart from his employment at the institution where the study was conducted.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013; 127:e6-e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011; 306:1669-1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities Study). Am J Cardiol. 2008; 101:1016-1022. [DOI] [PubMed] [Google Scholar]
- 4.McMurray JJ, Teerlink JR, Cotter G, Bourge RC, Cleland JG, Jondeau G, Krum H, Metra M, O'Connor CM, Parker JD, Torre‐Amione G, van Veldhuisen DJ, Lewsey J, Frey A, Rainisio M, Kobrin I. Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials. JAMA. 2007; 298:2009-2019. [DOI] [PubMed] [Google Scholar]
- 5.Massie BM, O'Connor CM, Metra M, Ponikowski P, Teerlink JR, Cotter G, Weatherley BD, Cleland JG, Givertz MM, Voors A, DeLucca P, Mansoor GA, Salerno CM, Bloomfield DM, Dittrich HC. Rolofylline, an adenosine A1‐receptor antagonist, in acute heart failure. N Engl J Med. 2010; 363:1419-1428. [DOI] [PubMed] [Google Scholar]
- 6.O'Connor CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, Heizer GM, Komajda M, Massie BM, McMurray JJV, Nieminen MS, Reist CJ, Rouleau JL, Swedberg K, Adams KF, Anker SD, Atar D, Battler A, Botero R, Bohidar NR, Butler J, Clausell N, Corbalán R, Costanzo MR, Dahlstrom U, Deckelbaum LI, Diaz R, Dunlap ME, Ezekowitz JA, Feldman D, Felker GM, Fonarow GC, Gennevois D, Gottlieb SS, Hill JA, Hollander JE, Howlett JG, Hudson MP, Kociol RD, Krum H, Laucevicius A, Levy WC, Méndez GF, Metra M, Mittal S, Oh B‐H, Pereira NL, Ponikowski P, Tang WHW, Tanomsup S, Teerlink JR, Triposkiadis F, Troughton RW, Voors AA, Whellan DJ, Zannad F, Califf RM. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011; 365:32-43. [DOI] [PubMed] [Google Scholar]
- 7.Packer M, Colucci W, Fisher L, Massie BM, Teerlink JR, Young J, Padley RJ, Thakkar R, Delgado‐Herrera L, Salon J, Garratt C, Huang B, Sarapohja T. Effect of levosimendan on the short‐term clinical course of patients with acutely decompensated heart failure. JACC Heart Fail. 2013; 1:103-111. [DOI] [PubMed] [Google Scholar]
- 8.Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, Unemori E, Voors AA, Adams KF, Jr, Dorobantu MI, Grinfeld LR, Jondeau G, Marmor A, Masip J, Pang PS, Werdan K, Teichman SL, Trapani A, Bush CA, Saini R, Schumacher C, Severin TM, Metra M. Serelaxin, recombinant human relaxin‐2, for treatment of acute heart failure (RELAX‐AHF): a randomised, placebo‐controlled trial. Lancet. 2013; 381:29-39. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC. The Acute Decompensated Heart Failure National Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure. Rev Cardiovasc Med. 2003; 4suppl 7:S21-S30. [PubMed] [Google Scholar]
- 10.Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100 000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005; 149:209-216. [DOI] [PubMed] [Google Scholar]
- 11.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009; 157:995-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. 2001New York, NY: Springer‐Verlag [Google Scholar]
- 13.Gray RJ. A class of K‐sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988; 16:1141-1154. [Google Scholar]
- 14.Torre‐Amione G, Milo‐Cotter O, Kaluski E, Perchenet L, Kobrin I, Frey A, Rund MM, Weatherley BD, Cotter G. Early worsening heart failure in patients admitted for acute heart failure: time course, hemodynamic predictors, and outcome. J Card Fail. 2009; 15:639-644. [DOI] [PubMed] [Google Scholar]
- 15.Cotter G, Metra M, Weatherley BD, Dittrich HC, Massie BM, Ponikowski P, Bloomfield DM, O'Connor CM. Physician‐determined worsening heart failure: a novel definition for early worsening heart failure in patients hospitalized for acute heart failure–association with signs and symptoms, hospitalization duration, and 60‐day outcomes. Cardiology. 2010; 115:29-36. [DOI] [PubMed] [Google Scholar]
- 16.Weatherley BD, Milo‐Cotter O, Felker GM, Uriel N, Kaluski E, Vered Z, O'Connor CM, Adams KF, Cotter G. Early worsening heart failure in patients admitted with acute heart failure–a new outcome measure associated with long‐term prognosis? Fundam Clin Pharmacol. 2009; 23:633-639. [DOI] [PubMed] [Google Scholar]
- 17.Ponikowski P, Metra M, Teerlink JR, Unemori E, Felker GM, Voors AA, Filippatos G, Greenberg B, Teichman SL, Severin T, Mueller‐Velten G, Cotter G, Davison BA. Design of the RELAXin in acute heart failure study. Am Heart J. 2012; 163:149-155.e141. [DOI] [PubMed] [Google Scholar]
- 18.Teerlink JR, McMurray JJ, Bourge RC, Cleland JG, Cotter G, Jondeau G, Krum H, Metra M, O'Connor CM, Parker JD, Torre‐Amione G, Van Veldhuisen DJ, Frey A, Rainisio M, Kobrin I. Tezosentan in patients with acute heart failure: design of the value of endothelin receptor inhibition with tezosentan in acute heart failure study (VERITAS). Am Heart J. 2005; 150:46-53. [DOI] [PubMed] [Google Scholar]