Abstract
Evidence-based assessment has received little attention despite its critical importance to the evidence-based practice movement. Given the limited resources in the public sector, it is necessary for evidence-based assessment to utilize tools with established reliability and validity metrics that are free, easily accessible, and brief. We review tools that meet these criteria for youth and adult mental health for the most prevalent mental health disorders to provide a clinical guide and reference for the selection of assessment tools for public sector settings. We also discuss recommendations for how to move forward the evidence-based assessment agenda.
Keywords: evidence-based practice, evidence-based assessment, public sector
The thorniest challenge facing the mental health field is the dissemination and implementation (DI) of evidence-based practices (EBPs) in community settings (McHugh & Barlow, 2010). EBPs refer to “the integration of the best available research with clinical expertise in the context of patient characteristics, culture, and preferences” (American Psychological Association, 2006, p. 1). Despite the proliferation of many EBPs for both children and adults suffering from psychosocial difficulties (Chambless & Hollon, 1998), these treatments are not widely available in community settings where the majority of individuals receive services (President's New Freedom Commission on Mental Health, 2003). Implementation science focuses on determining how to most effectively transmit knowledge about EBPs (i.e., dissemination) and how to use strategies that allow for increased adoption of such treatments (i.e., implementation; Lomas, 1993). The desired result of implementation science is to ensure that community clinicians are providing EBPs to youth and adults with the ultimate goal of improved quality of care. One aspect to this pursuit that has to date received little attention is evidence-based assessment (EBA), a critical foundational component of EBPs (American Psychological Association, 2006; Hunsley & Mash, 2007).
The scope of EBA is twofold, encompassing both the process through which assessment is conducted, and the instruments utilized for evaluation (Hunsley & Mash, 2007). The scope of this review will focus on the latter (i.e., instruments used for evaluation). We first briefly highlight the importance of EBA in the context of EBP. Assessment is inherently a decision-making task fraught with the biases that plague clinical decision-making (Dawes, Faust, & Meehl, 1989; Garb, 1998). For example, clinicians are subject to cognitive heuristics and biases such as confirmatory bias (i.e., preferentially seeking evidence consistent with an initial conceptualization at the cost of considering emerging contradictory information; Garb, 2005). These biases may be more avoidable with a systematic and empirically-based, research-driven approach to assessment. The importance of an accurate diagnosis is an implicit prerequisite to the selection of EBPs, which are largely organized by specific disorders. Moreover, diagnostic categories are the common language through which we think about, question, and communicate about research findings and clinical problems. Without accurate assessments yielding accurate diagnoses, we may widen the research-practice communication gap (Jensen & Weisz, 2002). There is also some evidence that accurate diagnosis is associated with better treatment outcomes (Jensen-Doss & Weisz, 2008; Pogge et al., 2001). Finally, emerging evidence suggests that simply tracking progress during treatment and providing feedback to clinicians results in better treatment outcomes (Bickman, Kelley, Breda, Vides de Andrade, & Riemer, 2011; Lambert, Hansen, & Finch, 2001). Therefore, EBA is critical to any evidence-based treatment approach. Given the importance of EBA, to date, two special issues of peer-reviewed journals have focused on EBA in both adult and youth populations: see special issues of Psychological Assessment (Hunsley & Mash, 2005) and the Journal of Clinical Child and Adolescent Psychology (Mash & Hunsley, 2005). These special issues have resulted in recommendations on EBA for a variety of disorders, including youth and adult anxiety (Antony & Rowa, 2005; Silverman & Ollendick, 2005), adult depression (Joiner, Walker, Pettit, Perez, & Cukrowicz, 2005), youth disruptive behavior disorders (McMahon & Frick, 2005), and youth bipolar disorder (Youngstrom, Findling, Kogos-Youngstrom, & Calabrese, 2005).
Although these reviews have resulted in important recognition of the importance of EBA and preliminary guidelines, they have not always been as applicable to low resource mental health settings such as those in the public sector because they have featured resource-intensive ways to engage in EBA. In the pages that follow, we identify and address issues related to the use of standardized tools in low resource mental health settings. The challenge of identifying which standardized instruments to use in the public sector is complicated by the sheer volume of assessment methods and processes and the many purposes of assessment compared to treatment (Hunsley & Mash, 2005). Treatment providers in agencies in public settings must often contend with high workload, poor financial compensation, limited time, and intense demand for resources (Nunno, 2006). Assessments must not add unnecessarily to the paperwork burden for providers and agencies, lest the cost, time, and resource requirements of EBA become barriers that outweigh the potential benefits (Bumbarger & Campbell, 2012). Given the known barriers to implementation of EBPs in community settings and our desire to increase EBA in the public sector, assessments must be brief, free or low cost, validated for use in multiple populations particularly ethnic minority and low socioeconomic status individuals, and straightforward and brief to administer, score and interpret (Jensen-Doss & Hawley, 2010). These recommendations are echoed by public health researchers who recommend that for standardized assessment instruments to be usable, they must be important to stakeholders in addition to researchers, low burden to administer, broadly applicable, sensitive to change, and represent constructs that are actionable (i.e., clinician or patient can do something about them; Glasgow & Riley, 2013).
Accordingly, the goal of this paper is to conduct a review of EBA instruments for the most prevalent mental health disorders in youths and adults that meet the criteria delineated above. We focus on instruments that can be used for screening (i.e., identifying those at risk for a disorder), diagnosis (i.e., identifying those who meet DSM criteria), and/or treatment monitoring and evaluation (i.e., evaluating the success of treatment or interim response to treatment (Hunsley & Mash, 2008). We hope this manuscript can serve as a clinical guide and reference for the selection of assessment instruments for low-resource mental health settings.
Methods
Search Methods
We searched PsycINFO, PubMed, and Google Scholar using this search term as our template: (“disorder name or type” or “mental health”) AND (instrument OR survey OR questionnaire OR measure OR assessment). For “disorder name or type”, we used the following terms: “trauma,” “trauma exposure,” “depression,” “anxiety,” “obsessive-compulsive disorder,” “panic,” “worry,” “generalized anxiety disorder,” “eating disorder,” “anorexia nervosa,” “bulimia nervosa,” “suicide,” “suicidality,” “self-injurious,” “schizophrenia,” “psychosis,” “personality disorders,” “borderline personality disorder,” “conduct disorder,” “oppositional defiant disorder,” “attention-deficit disorder,” “bipolar,” “mania,” “quality of life,” “functioning,” and “general functioning.” For disorders that could apply to both youth and adults (e.g., anxiety), we inserted “child,” “youth,” or “adolescent” in front of the disorder name or type when searching for youth-specific measures. We also searched for adolescent versions of all child and adult measures identified in our search. We employed a snowball sampling technique in which we searched the reference sections of located articles for potentially eligible measures. Also, due to its specific relevance, a textbook referencing EBA instruments was searched by hand for relevant measures (Hunsley & Mash, 2008). Finally, we reached out to experts to ensure that we did not miss any instruments. Specifically, the first author queried members of the Association for Behavioral and Cognitive Therapies (ABCT) via the ABCT members’ listserv and engaged in conversations with experts about measures they had used previously in studies. We also included measures we have used in previous studies in low-resource settings.
Inclusion and Exclusion Criteria
We utilized the following criteria when deciding whether or not to include measures: we required that the measures be free, easily accessible via the Internet or the author of the measure, brief (items < 50), have established reliability and validity, and be relevant for the most prevalent mental health disorders (e.g., anxiety, depression, trauma-associated disorders, oppositional behavior disorders; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Merikangas et al., 2010). We crafted these criteria based on a recent paper written by Glasgow & Riley (2013) encouraging the use of pragmatic measures. Specifically, Glasgow & Riley (2013) recommend that instruments be: important to stakeholders, low burden to administer, broadly applicable, sensitive to change, and measure actionable constructs. Our inclusion criteria map on these recommendations explicitly. The instruments we included are: (a) of importance for stakeholders in that they meet the needs for outcome assessment, a growing reality and requirement in many public systems, (b) are low burden to administer because they have fewer than 50 items, (c) are broadly applicable because they are appropriate for high prevalence conditions, (d) are sensitive to change when intended to be used as progress monitoring instruments, and (e) measure actionable constructs such as symptoms of a mental health disorder that are amenable to change through treatment.
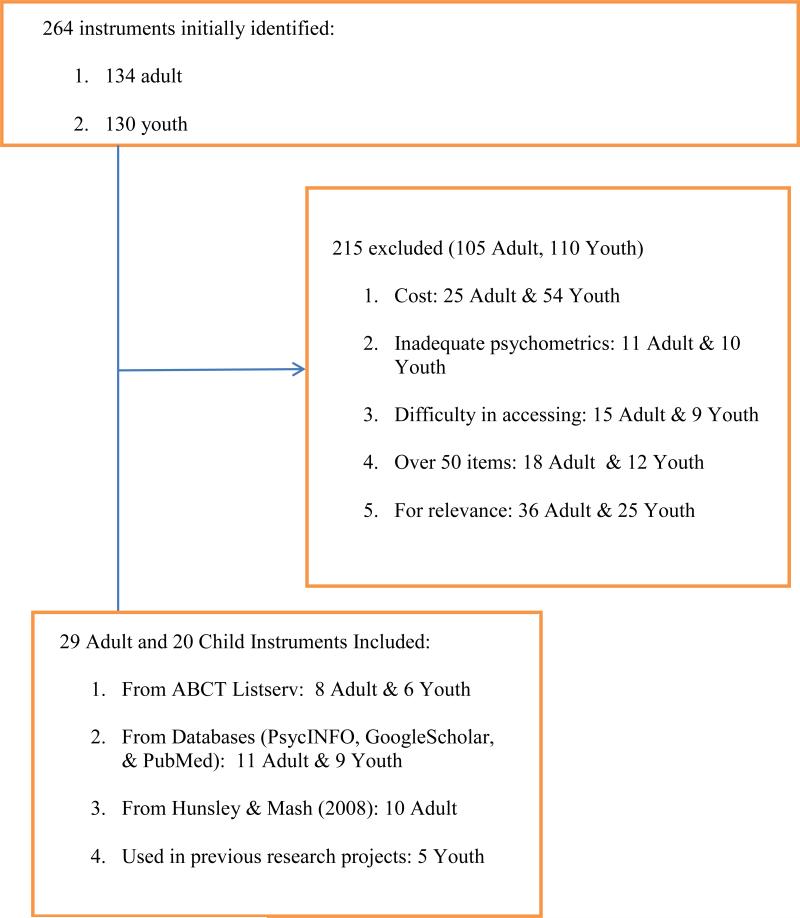
See Figure 1 for the number of instruments that were identified, reviewed, included, and excluded. Two hundred and sixty four instruments (134 adult, 130 youth) were initially located: 25 adult and 54 youth instruments were excluded because they had a financial cost associated with them, 15 adult and nine youth instruments were excluded because they could not be accessed (e.g., only available through journal articles which required a library subscription), 18 adult and 12 youth instruments were excluded due to number of items (i.e., >50 items), 11 adult and 10 youth instruments were excluded due to inadequate psychometrics (e.g., no information provided on reliability and/or validity) and 36 adult and 25 youth instruments were excluded due to being too specific or pertaining to a low base rate disorder (e.g., an instrument to diagnose personality disorders in incarcerated adolescent males; an instrument to rate trichotillomania symptoms). In all, 49 instruments (29 adult, 20 youth) were included.
Figure 1.
Instrument Classification
Given that instruments can serve multiple purposes (i.e., diagnosis, screening, and treatment monitoring/evaluation), we elected to classify the manner in which each instrument could be used. Instruments may be used for: (a) diagnosis: to determine “the nature and/or cause of the presenting problem”; (b) screening: to identify “those who are at risk...or who might be helped by further assessment or intervention”; and/or (c) treatment monitoring and evaluation: “track changes in symptoms and functioning” or determine “effectiveness...of the intervention.”(p. 6, Hunsley & Mash, 2008). An instrument could be designated as meeting all three criteria. We operationally defined instruments as appropriate for diagnosis if they were created to map on to DSM criteria. Sometimes, authors of instruments stated that it was explicitly not meant to be used for diagnosis (e.g., eating disorder instruments). However, to be consistent, we included any measure that mapped on to DSM criteria as meeting the “diagnosis” definition. Instruments met criteria for screening if the questions queried for symptoms of a mental health disorder or behavioral and/or emotional difficulties. Finally, instruments were classified as treatment monitoring and evaluation instruments if they could be used for screening or diagnosis, and data were available on the instrument's sensitivity to change following psychotherapy or psychotropic medication.
Reliability and Validity
Because methods and metrics to assess validity were not consistent across measures (e.g., concurrent validity, convergent validity, divergent validity), it was not possible to apply a validity coding scheme across instruments. Therefore, Appendices A and B summarize any evidence of validity as presented in the original psychometric papers. For reliability data, specifically internal consistency, inter-rater reliability, and test-retest reliability, we considered adequate, good and excellent reliabilities based on the criteria set forth by Hunsley & Mash (2008). These criteria are reviewed in Table 1.
Table 1.
Criteria at a Glance: Reproduced from Hunsley & Mash (2005)
| Criteria | Preponderance of evidence indicates: |
|---|---|
| Internal Consistency | |
| Adequate | α values of .70-.79 |
| Good | α values of .80-.89 |
| Excellent | α values ≥ .90 |
| Inter-rater reliability | |
| Adequate | k values of .60-.74, or Pearson correlation or intraclass correlation values of .70-.79 |
| Good | k values of .75-.84, or Pearson correlation or intraclass correlation values of .80-.89 |
| Excellent | k values ≥ .85, or Pearson correlation or intraclass correlation values ≥ .90 |
| Test-retest reliability | |
| Adequate | test-retest correlations of at least .70 over a period of several days to several weeks |
| Good | test-retest correlations of at least .70 over a period of several months |
| Excellent | test-retest correlations of at least .70 over a period of a year or longer |
Results
Twenty-nine adult and 20 youth instruments were identified. All instruments are free1, can be accessed through a website or by emailing the author, and contain less than 50 items. Additionally, all have reliability and validity information available. See Tables 2 and 3 for a list of all instruments and selected information (i.e., number of items, age range, sensitivity to change, reporter, and classification). More in-depth descriptions, including reliability and validity data, as available, are presented in the appendices (see Appendices A and B).
Table 2.
Adult Instruments
| Adult Instruments | ||||||||
|---|---|---|---|---|---|---|---|---|
| Measure | Where to obtain | Number of Items |
Ages | Reporter | Sensitive to change |
Screening | Diagnosis | Tx Monitoring & Evaluation |
| Anxiety | ||||||||
| The Clinically Useful Anxiety Outcome Scale (CUXOS) | http://www.outcometracker.org | 2Q | 18+ | S | X | X | X | |
| Generalized Anxiety Disorder Screener (GAD-7) | http://www.phqscreeners.com | 7 | 18+ | S | X | X | X | X |
| Hamilton Rating Scale for Anxiety (HAM-A) | http://www.outcometracker.org | 15 | 18+ | C | X | X | X | |
| Liebowitz Social Anxiety Scale Clinician-Report (LSAS-CR) | http://healthnet.umassmed.edu/mhealth/LiebowitzSocialAnxiet yScale.pdf | 24 | 18+ | S and C | X | X | X | |
| Liebowitz Social Anxiety Scale Self-Report (LSAS-SR) | http://asp.cumc.columbia.edu/S AD/ | |||||||
| Panic Disorder Severity Scale (PDSS) | http://www.outcometracker.org | 7 | 18+ | C | X | X | X | X |
| Fear Questionnaire (FQ) | http://www.outcometracker.org | 24 | 18+ | S | X | X | ||
| Penn State Worry Questionnaire (PSWQ) | http://www. outcometracker.org | 16 | 18+ | S | X | X | X | |
| Social Phobia Inventory (SPIN) | http://www.psychtoolkit.com | 17 | 18+ | S | X | X | X | |
| Worry and Anxiety Questionnaire (WAQ) | http://www.psychology.concor dia.ca/fac/dugas/downloads/en/ WAQ.pdf | 11 | 18+ | S | X | X | X | X |
| Depression | ||||||||
| The Clinically Useful Depression Outcome Scale (CUDOS) | http://www.outcometracker.org | 18 | 18+ | S | X | X | X | X |
| Hamilton Rating Scale for Depression (HAM-D) | http://www.outcometracker.org | 17 | 18+ | C | X | |||
| The Inventory of Depressive Symptoms and the Quick Inventory of Depressive Symptoms (IDS and QIDS) | http://www.ids-qids.org | 30 16 |
18+ | S and C | X | X | X | X |
| Patient Health Questionnaire-9 (PHQ-9) | http://www.phqscreeners.com/ | 9 | 18+ | S | X | X | X | X |
| Eating Disorders | ||||||||
| Eating Disorder Diagnostic Scale (EDDS) | http://homepage.psy.utexas.edu/homepage/group/sticelab/scales/#edds | 22 | 18+ | S | X | X | X | X |
| Sick, Control, One, Fat, Food Screening Tool (SCOFF) | http://www.marquette.edu/coun seling/documents/AQuickAssessmentforEatingConcerns.pdf | 5 | 18+ | S | X | |||
| Mania | ||||||||
| Altman Self-Rating Mania Scale (ASRM) | http://www.cqaimh.org/pdf/tool asrm.pdf | 5 | 18+ | S | X | X | X | |
| Bech-Rafaelsen Mania Scale (MAS) | http://opapc.com/images/pdfs/ MRS.pdf | 11 | 18+ | C | X | X | X | |
| Young Mania Rating Scale (YMRS) | http://dcf.psychiatry.ufl.edu/files/2011/05/Young-Mania-Rating-Scale-Measure-with-background.pdf | 11 | 18+ | C | X | X | X | |
| Overall Mental Health | ||||||||
| National Institutes of Health Patient Reported Outcomes Measurement Information System (PROMIS) | https://www.assessmentcenter.net/promisforms.aspx | 4-30 | 18+ | S | X | |||
| Patient Health Questionnaires (PHQ) | http://www.phqscreeners.com/ | 11 | 18+ | S | X | X | X | X |
| Recovery Assessment Scale (RAS) | http://www.power2u.org/downloads/pn-55.pdf | 41 | 18+ | S and C | X | X | ||
| Personality Disorders | ||||||||
| Borderline Evaluation of Severity over Time (BEST) | http://psychiatry.ucsd.edu/bord erlineServices.html | 15 | 18+ | S | X | X | X | X |
| Suicidality | ||||||||
| Columbia-Suicide Severity Rating Scale (C- SSRS) | http://www.cssrs.columbia.edu | 20 | 18+ | C | X | X | NA* | X |
| The Suicide Behaviors Questionnaire - Revised (SBQ-R) | http://www.integration.samhsa. gov/images/res/SBQ.pdf | 4 | 18+ | S | X | NA* | ||
| Trauma | ||||||||
| Impact of Event Scale-Revised (IES-R) | daniel.weiss@ucsf.edu | 22 | 18+ | S | X | |||
| Los Angeles Symptom Checklist (LASC) | dfoy@pepperdine.edu | 43 | 18+ | S | X | X | ||
| The Post-Traumatic Stress Disorder Checklist - Civilian Version (PCL-C) | http://www.ptsd.va.gov | 17 | 18+ | S | X | X | ||
| The Trauma History Screen (THS) | http://www.istss.org/AssessmentResources/5347.htm | 14 | 18+ | S | X | |||
| The Trauma History Questionnaire (THQ) | http://ctc.georgetown.edu/toolkit/ | 24 | 18+ | S and C | X | |||
Note.
S = self, C = clinician, * = not a diagnosable disorder; cannot be a diagnostic tool.
Table 3.
Youth Instruments
| Youth Instruments | ||||||||
|---|---|---|---|---|---|---|---|---|
| Measure | Where to obtain | Number of Items |
Ages | Reporter | Sensitive to Change |
Screening | Diagnosis | Tx Monitoring & Evaluation |
| Anxiety | ||||||||
| Children Yale-Brown Obsessive Compulsive Scale (CY-BOCS) | http://icahn.mssm.edu/research/centers/center-of-excellence-for-ocd/rating-scales | 10 | 6-17 | P | X | X | X | |
| Penn State Worry Questionnaire for Children (PSWQ-C) | http://www.childfirst.ucla.edu/Resources.html | 16 | 7-17 | S | X | |||
| Revised Children's Anxiety and Depression Scale Youth and Parent Versions (RCADS/RCADS-P) | http://www.childfirst.ucla.edu/Resources.html | 47 | 6-18 | S and P | X | X | X | X |
| Screen for Child Anxiety Related Emotion Disorders (SCARED) | http://psvchiatrv.pitt.edu/sites/default/files/Documents/assessments/SCARED%20Child.pdf | 41 | 6-18 | S and P | X | X | X | |
| Spence Children's Anxiety Scale (SCAS) | http://www.scaswebsite.com | 44 | 7-19 | S and P | X | X | X | X |
| Depression | ||||||||
| Center for Epidemiologic Studies Depression Scale for Children (CES-DC) | http://www.bri2htfutures.or2/rnentalhealth/pdf/professionals/bridges/cesdc.pdf | 20 | 6-23 | S | X | X | X | |
| Depression Self Rating Scale for Children (DSRSC) | http://www.scalesandmeasures.net/files/files/Birleson%20Self- Rating%20Scale%20for%20Child%20Depressive%20Disorder.pdf | 18 | 8-14 | S | X | |||
| Disruptive Behavior | ||||||||
| Child and Adolescent Disruptive Behavior Inventory-Parent & Teacher Version (CADBI) | http://measures.earlvadolescence.org/measures/view/40/ | 25 | Not specifi-ed | P and T | X | X | ||
| Eating Disorder | ||||||||
| Child Eating Attitudes Test (ChEAT) | http://www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/ChEAT.pdf | 26 | 8-13 | S | X | |||
| Eating Attitudes Test-26 (EAT-26) | http://eat-26.com | 26 | 16-18 | S and C | X | |||
| Mania | ||||||||
| Parent Version-Young Mania Rating Scale (P-YMRS) | http://dcf.psvchiatrv.ufl.edu/files/2011/05/Youna-Mania-Ratina-Scale-Measure-with- backaround.pdf | 11 | 5-17 | C | X | |||
| Child Mania Rating Scale - Parent (CMRS-P) | http://www.dbsalliance.ora/pdfs/ChildManiaSurvev.pdf | 21 | 5-17 | P | X | X | X | X |
| Overall Mental Health | ||||||||
| Brief Problem Checklist (BPC) | http://www.childfirst.ucla.edu/Resources.html | 12 | 7-13 | S and P | X | X | X | |
| The Ohio Scale-Youth, Parent, and Clinician versions | benoales@bvu.edu | 48 | 5-18 | S, P, and C | X | X | ||
| Peabody Treatment Progress Battery (PTPB) | http://peabodv.vanderbilt.edu/research/center-evaluation- proaram-improvement-cepi/rea/ptpb 2nd ed downloa ds.php | 11 | 11-18 | S, P, and C | X | X | X | |
| Pediatric Symptom Checklist and Pediatric Symptom Checklist-Youth Report (PSC & Y-PSC) | http://www.massaeneral.ora/psvchiatrv/services/pschome.aspx | 35 | 3-18 | S and P | X | X | X | |
| Strength and Difficulties Questionnaire (SDQ) | http://www.sdqinfo.ora/a0.html | 25 | 3-16 | S, P, and C | X | X | X | |
| Youth Top Problems (TP) | http://www.wih.harvard.edu/~iweisz/pdfs/2011c.pdf | 3 | 7-13 | S, P, and C | X | X | ||
| Trauma | ||||||||
| Child PTSD Symptom Scale (CPSS) | foa@mail.med.upenn.edu | 24 | 8-18 | S or C | X | X | X | X |
| Pediatric Emotional Distress Scale (PEDS) | conwav.savlor@citadel.edu | 21 | 2-10 | P | X | X | X | |
Note.
S = self, C = clinician, P = parent, T=teacher
Anxiety
Fourteen instruments were identified (9 adult, 5 youth) that assessed symptoms of anxiety.
Adult
Adult instruments ranged in length from 7-24 items. The majority of the adult instruments (7) were disorder specific (e.g., assessing for Generalized Anxiety Disorder; Generalized Anxiety Disorder Screener (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006)), although two instruments assessed general anxiety (The Clinically Useful Anxiety Outcome Scale (CUXOS; Zimmerman, Chelminski, Young, & Dalrymple, 2010); Hamilton Rating Scale for Anxiety (HAM-A; Hamilton, 1959)). All of the adult instruments could be used as screening and treatment monitoring/evaluation tools. Only three instruments could be used as diagnostic tools (GAD-7; Spitzer et al., 2006); Panic Disorder Severity Scale (PDSS; Shear et al., 1997); Social Phobia Inventory (SPIN; Connor et al., 2000)).
Youth
Youth instruments ranged in length from 10-47 items and were intended for administration with youths 6-19. The majority of the youth instruments (3) assessed general anxiety (Revised Children's Anxiety and Depression Scale Youth and Parent Versions (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000); Screen for Child Anxiety Related Emotion Disorders (SCARED; Birmaher et al., 1997), Spence Children's Anxiety Scale (SCAS; Spence, 1998)), although two instruments were disorder specific (Children Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997); Penn State Worry Questionnaire for Children (PSWQ-C; Chorpita, Tracey, Brown, Collica, & Barlow, 1997)). All of the youth instruments could be used as screening tools. Only two instruments could be used as diagnostic tools (RCADS; SCAS). Four instruments could be used for treatment monitoring/evaluation (CY-BOCS, RCADS, SCARED, SCAS).
Depression
Six instruments were identified (4 adult, 2 youth) that assessed symptoms of depression.
Adult
Adult instruments ranged in length from 9-30 items. All of the adult instruments could be used as screening tools. Three instruments could be used as diagnostic tools and treatment monitoring/evaluation tools (The Clinically Useful Depression Outcome Scale (CUDOS, Zimmerman, Chelminski, McGlinchey, & Posternak, 2008); The Inventory of Depressive Symptoms/Quick Inventory of Depressive Symptoms (IDS/QIDS; Rush et al., 1986; Rush, Gullion, Basco, Jarrett, & Trivedi, 1996; Rush et al., 2003); Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001)).
Youth
. Youth instruments ranged in length from 18-20 items and were intended for administration in youths 6-23. All of the youth instruments could be used as screening tools. None were appropriate for diagnostic purposes. Only one tool could be used for treatment monitoring and evaluation (Center for Epidemiologic Studies Depression Scale for Children (CES-DC; Fendrich, Weissman, & Warner, 1990)).
Disruptive Behavior Disorders
One instrument was identified that assessed symptoms of disruptive behavior disorders.
Adult
Not applicable.
Youth
One 25-item instrument, the Child and Adolescent Disruptive Behavior Inventory-Parent & Teacher Version (CADBI; Burns, Taylor, & Rusby, 2001a; 2001b), was identified. This tool can be used as a screening and diagnostic tool, but not for treatment monitoring and evaluation.
Eating disorders
Four instruments were identified (2 adult, 2 youth) that assessed symptoms of eating disorders.
Adult
Adult instruments ranged in length from 5-22 items. Both adult instruments could be used as screening tools; only the Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000) could be used as a diagnostic and treatment monitoring/evaluation tool.
Youth
Both youth instruments were 26 items and were intended for administration in youths 8-18. Both instruments could be used as screening tools. Neither was appropriate for diagnostic or treatment monitoring and evaluation.
Mania
Five instruments were identified (3 adult, 2 youth) that assessed symptoms of mania.
Adult
Adult instruments ranged in length from 5-11 items. All adult instruments could be used as screening and treatment monitoring/evaluation tools. None of the tools could be used for diagnostic purposes.
Youth
Youth instruments ranged from 11-21 items and were intended for administration in youths 5-17. Both youth instruments could be used as screening tools; only the Child Mania Rating Scale-Parent (CMRS-P; Pavuluri, Henry, Devineni, Carbray, & Birmaher, 2006) could be used for diagnostic and treatment monitoring/evaluation purposes.
Overall Mental Health
Nine instruments were identified (3 adult, 6 youth) that fell under the category of “overall mental health.”
Adult
Adult instruments ranged in length from 4-41 items. Two adult instruments could be used as screening tools (National Institutes of Health Patient Reported Outcomes Measurement Information System (PROMIS; NIH PROMIS, 2013); Patient Health Questionnaire (PHQ; Spitzer, Kroenke, & Williams, 1999)). The PHQ could also be used as a diagnostic tool. Two instruments could be used for treatment monitoring and evaluation (PHQ, Recovery Assessment Scale (RAS; Giffort, Schmook, Woody, Vollendorf, & Gervain, 1995)).
Youth
Youth instruments ranged from 11-48 items and were intended for administration in youths 3-18. Four of the instruments could be used as screening tools (Brief Problem Checklist (BPC; Chorpita et al., 2010), Peabody Treatment Progress Battery (PTPB; Bickman et al., 2010), Pediatric Symptom Checklist/Youth Report (PSC & Y-PSC; Jellinek et al., 1988), and the Strength and Difficulties Questionnaire (SDQ; Goodman, 1997)). None of the instruments were used as diagnostic tools. All instruments could be used for treatment monitoring and evaluation.
Personality Disorders
One measure was identified that assessed personality disorders in adults; no measures were identified for youths which is appropriate given that personality disorders are not diagnosed in those under 18 years.
Adult
The Borderline Evaluation of Severity over Time (BEST; Blum, Pfohl, St. John, Monahan, & Black, 2002) is a 15-item instrument that is a screening, diagnostic, and treatment monitoring/evaluation tool for borderline personality disorder. Tools for other personality disorders were not identified.
Youth
Not applicable.
Suicidality
Two adult instruments were identified that assessed suicidality; no child instruments were identified.
Adult
Adult instruments ranged in length from 4-20 items. All adult instruments could be used as screening tools. One instrument could be used for treatment monitoring and evaluation (The Suicide Behaviors Questionnaire-Revised (SBQ-R; Osman et al., 2001).
Youth
We were not able to identify any measures that met our criteria.
Trauma
Seven instruments were identified (5 adult, 2 youth) that assessed symptoms of trauma.
Adult
Adult instruments ranged in length from 14-43 items. All adult instruments could be used as screening tools. None of the tools could be used for treatment monitoring and evaluation. Two instruments could be used for diagnostic purposes (Los Angeles Symptom Checklist (LASC; King, King, Leskin, & Foy, 1995); The Post-Traumatic Stress Disorder Checklist-Civilian Version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993)).
Youth
Youth instruments ranged from 21-24 items and were intended for administration in youths 2-18. Both youth instruments could be used as screening tools; only the Child PTSD Symptom Scale (CPSS; Foa, Johnson, Feeny, & Treadwell, 2001) could be used for diagnostic purposes. Both instruments could be used for treatment monitoring/evaluation purposes.
Discussion
As evidenced by this review, there are multiple assessment tools that fit the needs of clinicians in low-resource mental health settings; these measures are free, easily accessible via the Internet or email, brief, have established psychometric properties, and are relevant for the most prevalent mental health disorders. It is our hope that community clinicians will use this compendium to select the most appropriate measure for their general population and specific clients. We have identified 29 adult and 20 youth measures that can be used as part of an EBA toolkit for a heterogeneous group of clients. We also believe that this manuscript can provide a valuable resource for implementation scientists interested in promoting the use of feasible EBA in community settings.
This review also provides important insights about where assessment tools are most sorely needed. Whereas instruments to measure anxiety symptoms in adults and youths were well represented, instruments to assist in diagnosis and treatment monitoring for youth with depressive symptoms were sparse. Only one instrument for disruptive behavior disorders was identified, and this instrument can be used only for screening and/or diagnosis; not treatment monitoring/evaluation, suggesting a need for instrument development and validation. Diagnostic and treatment monitoring and evaluation instruments for youth with eating disorders were also unavailable. Of great concern, tools assessing suicidality in youths were unavailable. Diagnostic tools of overall mental health were missing for youth. With regard to adult instruments, a need for treatment monitoring and evaluation instruments for trauma were identified as a needed area, as well as instruments that assess for personality disorders other than borderline personality disorder.
Some have suggested that providing a laundry list of psychometrically validated measures is not likely to be effective in encouraging use of EBA on a wider scale (Kazdin, 2005). However, the provision of this list helps lay a foundation in moving the agenda forward for increasing the use of EBA (Jensen-Doss & Hawley, 2010) through the necessary first step of providing access. A few studies have queried mental health clinicians about their use of assessment tools, finding that the primary assessment method used in clinical practice is the unstructured clinical interview (Anderson & Paulosky, 2004). Clinicians report that barriers to the use of standardized tools are measure access, time demands, and ease of administration and scoring (Garland, Kruse, & Aarons, 2003; Hatfield & Ogles, 2007; Jensen-Doss & Hawley, 2010). These practical concerns are particularly pressing for fee-for-service clinicians in the public sector. It is our hope that the publication of this collection of measures increases the opportunity for clinicians to quickly access a list of available, free, standardized instruments from which to select a battery for screening, diagnosis, and treatment monitoring and evaluation. Moreover, in concert with sophisticated guidelines in the process of EBA (See Youngstrom, Coukas-Bradley, Calhoun, & Jensen-Doss, this issue), this list has the potential to make an impact on clinicians, clients, and policy-makers in the public sector wishing to integrate assessment and monitoring tools in their toolkit, as well as highlighting areas of need for future research.
There are a number of important clinical issues that must be considered within the context of EBA, including: How does a clinician decide which standardized tool to use? Should the tools be general to mental well-being or specific to the presenting problem or disorder? How should these tools inform the diagnostic process and treatment monitoring? Which informants should be included? When is the best time to administer such tools? We have not made recommendations about which measure a clinician should select for a particular presenting problem, in large part because such guidelines will be necessarily complex and are beyond the scope of this manuscript. Several manuscripts are dedicated to exploring these issues for particular disorders in the referenced special issues. Hunsley and Mash (2005) present key themes and considerations in the development of EBA guidelines, and yet suggest that there is still much work to do in delineating EBA guidelines. Making an exciting stride forward, Youngstrom and colleagues (this issue) make recommendations on a twelve-step approach, using evidence-based medicine principles, that can be applied to streamline the assessment process.
There is a general consensus that prior to treatment, clinicians should select broader assessment tools to cast a wide net regarding the presenting problem of a client, and then using more specific tools as the presenting problem becomes more clear (Hunsley & Mash, 2005). To monitor progress over time, specific tools can be used to track client improvement or deterioration. This also speaks to the issue of assessment over time. As Kazdin (2005) states, “ongoing, continuous assessment is needed during the course of treatment.” (p. 554). For example, in the case of a youth presenting for treatment; a general screener such as the BPC (Chorpita et al., 2010) can be administered. If particular elevations suggesting anxiety become apparent, then an anxiety specific standardized tool such as the SCARED can then be administered (Birmaher et al., 1997). Subsequently, this tool can be used on a regular basis (e.g., every 2 weeks) to monitor treatment progress. At the end of treatment, the BPC and SCARED can be administered again to ensure that initial elevations are no longer present.
Beyond the question of which instrument to use and when to administer it, clinicians are confronted with the question of whom to ask to complete it (Achenbach, 2005). This topic has been explored in great depth in the youth assessment literature, but has received less recognition in the adult assessment literature, despite evidence that, similar to data in youths, there is low cross-informant (e.g., caregiver, spouses) agreement for adults (Achenbach, Krukowski, Dumenci, & Ivanova, 2005). Unfortunately, there is little guidance available to help clinicians decide how to weigh informant data in adults. In the youth assessment literature, a plethora of evidence suggests discrepancies among children, parents, and teachers when reporting on youths psychosocial difficulties (De Los Reyes & Kazdin, 2005). There are different methods to assess such divergence (see De Los Reyes & Kazdin, 2004). In the absence of EBA guidelines, clinicians are encouraged to use the “or rule.” If a youth or parent reports symptoms on a standardized tool, the clinician targets treatment towards those symptoms. The “or rule” increases sensitivity compared with the “and rule,” which requires that both the youth and parent report symptoms (Comer & Kendall, 2004).
There are also a number of ethical considerations to consider in the context of EBA. One important question is the appropriateness of standardized assessment tools for ethnic/racial minorities and the use of standardized rating scales to make diagnostic determinations. Many standardized assessment tools cited in this manuscript have not been tested in multiple ethnic/racial groups (Achenbach, 2005), and may not be equally valid in assessing psychopathology or diagnostic criteria. In the rare cases in which standardized tools have been compared across different cultures, similarities have been found in the prevalence and presentation of mental health difficulties (Ivanova et al., 2007; 2010). More research of this kind is needed given that many of the youth and adults seen in the public sector are ethnic and/or racial minorities. Another ethical issue concerns the use of rating scales as diagnostic tools. The gold-standard diagnostic process is the structured clinical interview (e.g., Structured Clinical Interview for DSM Disorders; SCID; First, Spitzer, Gibbon, & Williams, 1996). The standardized tools presented in this manuscript are not intended as diagnostic tools even if they map on to diagnostic criteria; they are all intended as screeners for potential disorders (sometimes necessitating further assessment) or symptom rating tools. However, the SCID and similar interviews are time-intensive, generally unbillable, and require intensive training for administration. Given these practical concerns, they are not feasible in the public sector. Clinicians in these settings need brief standardized tools that can be used as diagnostic aids (see Youngstrom et al., this issue). It is not clear from the literature how much EBA presently occurs in community mental health. Given the practical concerns, the answer is possibly very little. Although future research is necessary to examine this empirical question, it may be better overall for clinicians to be using some EBA tools rather than none at all, and this review will hopefully serve as a helpful resource.
There is a critical need to include EBA as part of the process of implementing EBP in community settings. Initial evaluation and ongoing progress monitoring are foundational components of the EBP process; both are expected and routine in other areas of healthcare (Goodman, McKay, & DePhilippis, in press). Use of standardized tools prior to treatment initiation for screening and diagnostic purposes allows clinicians to target treatment and identify appropriate EBPs. The use of standardized tools to monitor and evaluate treatment and provide feedback over the course of treatment can result in improved outcomes in both youths (Bickman et al., 2011) and adults (Carlier et al., 2012; Lambert et al., 2001). Having inexpensive, brief and easily accessible screening and progress-monitor tools is an important first – but by no means the only necessary – step in increasing the use of EBA in community mental health settings.
Several exciting national initiatives will make it easier for clinicians to use standardized tools as part of ongoing practice. The National Institutes of Health (NIH) has developed PROMIS, a set of freely available validated measures of patient–reported health status for physical, mental, and social well–being (http://www.nihpromise.org). Although promising, more work must be conducted on the use of these measures in clinical populations (e.g., youth with anxiety and/or depression) given that they have been primarily used in pediatric populations (e.g., oncology). The National Cancer Institute has sponsored a separate, free repository of available standardized tools to assess various mental and physical conditions (https://www.gem-beta.org/). Further, the NIH now requires that articles published from NIH-funded research be freely available to the public, which increases the likelihood of any new measures created through public funding becoming available to practitioners and consumers.
In the following paragraphs, we suggest some important next steps to increase the extent to which EBA is used.
Develop guidelines
While assessment guidelines are available for some disorders, these guidelines often do not take into account the practical constraints facing clinicians working in low resource mental health settings. Guidelines are needed for general practice and for specific disorders, with consideration of the limited time and other resources available to community clinicians. Specifically, guidelines are needed to help guide clinicians through the decision making process of which instrument to use, when to use it (e.g., screening, diagnosis, treatment monitoring and evaluation), how often to administer (i.e., frequency), and how to integrate information across instruments in a clinically meaningful manner. For example, the work of Ebesutani and colleagues (2012) provides a significant step forward in developing a standardized assessment protocol that is of low burden to clinicians that can inform treatment need for youth in public sector settings. More work of this kind is needed.
Develop training protocols to increase expertise in EBA
Another largely ignored issue is the need for clinician training in the use of standardized tools. Without understanding how standardized tools can be useful clinically, they become another administrative burden with little clinical payoff (Garland et al., 2003). One of the largest challenges in the EBP movement has been training the existing workforce in treatments with which they have little familiarity (McHugh & Barlow, 2010). Such efforts to train clinicians in EBP to date have been largely disappointing (Beidas & Kendall, 2010). As efforts are made to improve trainings and understand how the public sector context impacts clinician behavior (e.g., Beidas et al., 2013), an additional consideration will be the provision of training on how to administer standardized tools and use the data in meaningful ways (Kazdin, 2005). An exploration of implementation strategies (Powell et al., 2012) that increase the use of standardized tools is an important area of future research.
Develop a frequently updated databank of EBA
The status of standardized assessment tools is constantly in flux, with new tools created and old tools updated on a regular basis. Future efforts to document such tools in a web-based repository such as the American Psychological Association (APA) PracticeOUTCOMES website are ideal; however this service requires an APA membership. Other websites exists but none of them offer a comprehensive overview of screening, diagnostic, and treatment monitoring and evaluation instruments for youths and adults (e.g., http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures; http://outcometracker.org). A free website similar to this effort that provides an ongoing resource with updated standardized assessment tools by problem area would greatly move the EBA field forward.
Take advantage of new digital technologies
Most measures are administered using paper-and-pencil and require time to score and interpret. Current technology makes it easy to develop software that scores and provide interpretations for clinicians to reduce clinician burden and increase standardization of interpretation. As these technologies become less expensive, clinics could use tablet technology or kiosks to administer measures while clients wait for their appointments. This information then could be transmitted to the clinician in a seamless manner that greatly enhances the accessibility and uniformity of EBA. This may require negotiation with instrument developers as incorporation of instruments into digital data-collection systems may not be covered under usage terms.
Conclusion
This manuscript provides a clinical guide and reference for the selection of free, brief, and validated evidence-based assessment tools for public sector mental health settings. Relative to many other areas of health, mental health research has been greatly hampered by lack of consistent and universal measurement of presenting problems, progress over time, and outcomes. Even among highly trained professionals, there is a tremendous lack both of diagnostic agreement and concordance regarding treatment approach, especially among the clinically complex individuals presenting for treatment in the public sector. Successful implementation of EBA holds the potential to place the emphasis of our treatment and associated research on patient-centered outcomes. Standardized measurement is a necessary first step in comparative effectiveness research, a focus of the most recent National Institute of Mental Health Strategic Plan (United States Department of Health and Human Services, National Institutes of Health, 2008) and the recently created Patient Centered Outcomes Research Institute (PCORI). Applied to the population as a whole, implementation of EBA has the potential to provide a much better understanding of which treatments work for which patient, thereby reshaping the way care is provided in the public sector.
Supplementary Material
Footnotes
1 The Ohio Scales (Youth, Parent, and Clinician versions; Ogles, Melendez, Davis, & Lunnen, 2001) have a very nominal fee for clinicians not living in the state of Ohio.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile.Burlington. University of Vermont, Department of Psychiatry; VT: 1991a. [Google Scholar]
- Achenbach TM. Manual for the Youth-Self Report and 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991b. [Google Scholar]
- Achenbach TM. Advancing assessment of children and adolescents: Commentary on evidence-based assessment of child and adolescent disorders. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):541–547. doi: 10.1207/s15374424jccp3403_9. doi: 10.1207/s15374424jccp3403_9. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Krukowski RA, Dumenci L, Ivanova MY. Assessment of adult psychopathology: Meta-analyses and implications of cross-informant correlations. Psychological Bulletin. 2005;131(3):361–382. doi: 10.1037/0033-2909.131.3.361. doi: 10.1037/0033-2909.131.3.361. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms &Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Adler-Nevo G, Manassis K. An adaptation of prolonged exposure therapy for pediatric single incident trauma: A case series. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2011;20(2):127–133. [PMC free article] [PubMed] [Google Scholar]
- Altman EG, Hedeker DR, Janicak PG, Peterson JL, Davis JM. The Clinician-Administered Rating Scale for Mania (CARS-M): Development, reliability, and validity. Biological Psychiatry. 1994;36(2):124–134. doi: 10.1016/0006-3223(94)91193-2. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM. The Altman Self-Rating Mania Scale. Biological Psychiatry. 1997;42(10):948–955. doi: 10.1016/S0006-3223(96)00548-3. doi: 10.1016/S0006-3223(96)00548-3. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM. A comparative evaluation of three self-rating scales for acute mania. Biological Psychiatry. 2001;50(6):468–471. doi: 10.1016/s0006-3223(01)01065-4. [DOI] [PubMed] [Google Scholar]
- American Psychological Association Evidence-based practice in psychology. AmericanPsychology. 2006;61(4):271–285. doi: 10.1037/0003-066X.61.4.271. doi: 10.1037/0003-066X.61.4.271. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statisic Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, D.C.: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistic Manual of Mental Disorders. 4th ed., text rev. American Psychiatric Association; Washington, D.C.: 2010. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Anderson DA, Paulosky CA. A survey of the use of assessment instruments by eating disorder professionals in clinical practice. Eating and Weight Disorders. 2004;9(3):238–241. doi: 10.1007/BF03325075. [DOI] [PubMed] [Google Scholar]
- Antony MM, Rowa K. Evidence-based assessment of anxiety disorders in adults. Psychological Assessment. 2005;17(3):256–266. doi: 10.1037/1040-3590.17.3.256. doi: 10.1037/1040-3590.17.3.256. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for school-age children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmachology. 2003;13(4):463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Baczwaski BJ. A measure of interest to logotherapy researchers: Suicidal Behaviors Questionnaire-Revised. International Forum for Logotherapy. 2012;35(1):41–42. Retrieved from http://search.proquest.com/docview/1312430562?accountid=14707. [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, Hofmann SG. The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40(6):701–715. doi: 10.1016/s0005-7967(01)00060-2. doi: 10.1016/S0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: Has the gold standard become a lead weight? The American Journal of Psychiatry. 2004;161(12):2163–2177. doi: 10.1176/appi.ajp.161.12.2163. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- Bech P. The Bech-Rafaelsen Mania Scale in clinical trials of therapies for bipolar disorder: A 20-year review of its use as an outcome measure. CNS Drugs. 2002;16(1):47–63. doi: 10.2165/00023210-200216010-00004. doi: 10.2165/00023210-200216010-00004. [DOI] [PubMed] [Google Scholar]
- Bech P, Rafaelsen OJ, Kramp P, Bolwig TG. The Mania Rating Scale: Scale construction and inter-observer agreement. Neuropharmacology. 1978;17(6):430–431. doi: 10.1016/0028-3908(78)90022-9. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47(2):343. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Aarons G, Barg F, Evans A, Hadley T, Hoagwood K, Mandell DS. Policy to implementation: Evidence-based practice in community mental health--Study protocol. Implementation Science. 2013;8:38. doi: 10.1186/1748-5908-8-38. doi: 10.1186/1748-5908-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidas RS, Kendall PC. Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: Science and Practice. 2010;17(1):1–30. doi: 10.1111/j.1468-2850.2009.01187.x. doi: 10.1111/j.1468-2850.2009.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz S, Stover CS. Trauma History Questionnaire Parent and Child Version. Unpublished questionnaire. Yale Child Study Center Trauma Section. 2005 [Google Scholar]
- Bickman L, Athay MM. Practical multi-informant measurement of youth mental health treatment progress [Special issue]. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39(1-2):1–145. doi: 10.1007/s10488-012-0404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickman L, Athay MM, Riemer M, Lambert EW, Kelley SD, Breda C, Vides de Andrade AR, editors. 2nd ed. Vanderbilt University; Nashville, TN: 2010. Manual of the Peabody Treatment Progress Battery. Electronic version. Retrieved from: http://peabody.vanderbilt.edu/ptpb\. [Google Scholar]
- Bickman L, Kelley SD, Breda C, Vides de Andrade AR, Riemer M. Effects of routine feedback to clinicians on mental health outcomes of youths: Results of a randomized trial. Psychiatric Services. 2011;62(12):1423–1429. doi: 10.1176/appi.ps.002052011. doi:10.1176/appi.ps.00205201. [DOI] [PubMed] [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. Journal of Child Psychology and Psychiatry. 1981;22:68–73. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Birleson P, Hudson I, Buchanan DG, Wolff S. Clinical evaluation of a self-rating scale for depressive disorder in childhood. Journal of Child Psychology and Psychiatry. 1987;28(1):43–60. doi: 10.1111/j.1469-7610.1987.tb00651.x. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders(SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blum N, Pfohl B, St. John D, Monahan P, Black DW. STEPPS: A cognitive-behavioral systems-based group treatment for outpatients with borderline personality disorder--A preliminary report. Comprehensive Psychiatry. 2002;43(4):301–310. doi: 10.1053/comp.2002.33497. doi: 10.1053/comp.2002.33497. [DOI] [PubMed] [Google Scholar]
- Bollinger AR, Cuevas CA, Vielhauer MJ, Morgan EE, Keane TM. The operating characteristics of the PTSD Checklist in detecting PTSD in HIV+ substance abusers. Journal of Psychological Trauma. 2008;7(4):213–234. doi: 10.1080/19322880802384251. [Google Scholar]
- Boysan M, Keskin S, Besiroglu L. Assessment of hierarchical factor structure, reliability and validity of Penn State Worry Questionnaire Turkish version. Klinik Psikofarmakoloji Bulteni-Bulletin of Clinical Psychopharmacology. 2008;18(3):174–182. [Google Scholar]
- Bright Futures: Tool for Professionals . Instructions for use. Center for EpidemiologicalStudies Depression Scale for Children (CES-DC); 2013. Retrieved from http://www.brightfutures.org/mentalhealth/pdf/professionals/bridges/ces_dc.pdf. [Google Scholar]
- Broderick JE, DeWitt EM, Rothrock N, Crane PK, Forrest CB. Advances in patient reported outcomes: The NIH PROMIS measures. Generating Evidence & Methods to Improve Patient Outcomes. 2013;1(1):12. doi: 10.13063/2327-9214.1015. doi: 10.13063/2327-9214.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhr K, Dugas MJ. The Intolerance of Uncertainty Scale: Psychometric properties of the English version. Behaviour Research and Therapy. 2002;40(8):931–945. doi: 10.1016/s0005-7967(01)00092-4. doi: 10.1016/S0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Bumbarger BK, Campbell EM. A state agency-university partnership for translational research and the dissemination of evidence-based prevention and intervention. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39(4):268–277. doi: 10.1007/s10488-011-0372-x. doi: 10.1007/s10488-011-0372-x. [DOI] [PubMed] [Google Scholar]
- Burns GL, Boe B, Walsh JA, Sommers-Flanagan R, Teegarden LA. A confimatory factor analysis on the DSM-IV ADHD and ODD symptoms: What is the best model for the organization of these symptoms? Journal of Abnormal Psychology. 2001;29:339–349. doi: 10.1023/a:1010314030025. [DOI] [PubMed] [Google Scholar]
- Burns GL, Taylor TK, Rusby JC. Child and Adolescent Disruptive Behavior Inventory 2.3: Parent version. Washington State University, Department of Psychology; Pullman: 2001a. [Google Scholar]
- Burns GL, Taylor TK, Rusby JC. Child and Adolescent Disruptive Behavior Inventory 2.3: Teacher Version. Washington State University, Department of Psychology; Pullman: 2001b. [Google Scholar]
- Calderoni ME, Alderman EM, Silver EJ, Bauman LJ. The mental health impact of 9/11 on inner-city high school students 20 miles north of ground zero. Journal of Adolescent Health. 2006;39(1):57–65. doi: 10.1016/j.jadohealth.2005.08.012. doi: 10.1016/j.jadohealth.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Campbell KA, Rohlman DS, Storzbach D, Binder LM, Anger WK, Kovera CA, Grossmann SJ. Test-retest reliability of psychological and neurobehavioral tests self-administered by computer. Assessment. 1999;6(1):21–32. doi: 10.1177/107319119900600103. [DOI] [PubMed] [Google Scholar]
- Carlier IV, Meuldijk D, Van Vliet IM, Van Fenema E, Van der Wee NJ, Zitman FG. Routine outcome monitoring and feedback on physical or mental health status: Evidence and theory. Journal of Evaluation in Clinical Practice. 2012;18(1):104–110. doi: 10.1111/j.1365-2753.2010.01543.x. doi: 10.1111/j.1365-2753.2010.01543.x. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, Spain DA. Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment. 2011;23(2):463–477. doi: 10.1037/a0022294. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for School Mental Health Summary of free assessment measures. 2012 Retrieved from http://csmh.umaryland.edu/Resources/ClinicianTools/Summmary%20of%20Free%20Assessment%20Measures%2012.12.12.pdf.
- Center for Suicide Risk Assessment About the C-SSRS: Clinical practice. 2013 Retrieved from http://www.cssrs.columbia.edu/clinical_practice.html.
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal ofConsulting and Clinical Psychology. 1998;66(1):7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised ChildAnxiety and Depression Scale in a clinical sample. Behaviour Research and Therapy. 2005;43:309–322. doi: 10.1016/j.brat.2004.02.004. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Reise S, Weisz JR, Grubbs K, Becker KD, Krull JL, ResearchNetwork on Youth Mental Health Evaluation of the Brief Problem Checklist:Child and caregiver interviews to measure clinical progress. Journal of Consulting and Clinical Psychology. 2010;78(4):526–536. doi: 10.1037/a0019602. doi: 10.1037/a0019602. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH. Assessment of worry in children and adolescents: An adaptation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1997;35(6):569–581. doi: 10.1016/s0005-7967(96)00116-7. doi: 10.1016/S0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38(8):835–855. doi: 10.1016/s0005-7967(99)00130-8. doi: 10.1016/S0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Cole DA. Hopelessness, social desirability, depression, and parasuicide in two college student samples. Journal of Consulting and Clinical Psychology. 1988;56(1):131–136. doi: 10.1037//0022-006x.56.1.131. [DOI] [PubMed] [Google Scholar]
- Collaborative Research Team to Study Psychosocial Issues in Bipolar Disorder Assessment and Rating Scales: Young Mania Rating Scale (YMRS) 2013 Retrieved from: http://www.crestbd.ca/wp-content/uploads/YMRS.pdf.
- Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(7):878–886. doi: 10.1097/01.chi.0000125092.35109.c5. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN). New self-rating scale. The British Journal of Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JR. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depression and Anxiety. 2001;14(2):137–140. doi: 10.1002/da.1055. doi: 10.1002/da.1055. [DOI] [PubMed] [Google Scholar]
- Cooper J. The Leyton obsessional inventory. Psychological Medicine. 1970;1(1):48–64. doi: 10.1017/s0033291700040010. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Giffort D, Rashid F, Leary M, Okeke I. Recovery as a psychological construct. Community Mental Health Journal. 1999;35(3):231–239. doi: 10.1023/a:1018741302682. doi: 10.1023/A:1018741302682. [DOI] [PubMed] [Google Scholar]
- Cotton CR, Peters DK, Range LM. Psychometric properties of the Suicidal Behaviors Questionnaire. Death Studies. 1995;19(4):391–397. doi: 10.1080/07481189508252740. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Ross L, Swinson RP, Direnfeld DM. A comparison of social phobia outcome measures in cognitive behavioral group therapy. Behavior Modification. 1998;22:285–297. doi: 10.1177/01454455980223004. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behaviour Research and Therapy. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Crittendon J, Hopko DR. Assessing worry in older and younger adults:Psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A). Journal of Anxiety Disorders. 2006;20(8):1036–1054. doi: 10.1016/j.janxdis.2005.11.006. doi: 10.1016/j.janxdis.2005.11.006. [DOI] [PubMed] [Google Scholar]
- Cusin C, Yang H, Yeung A, Fava M. Rating scales for depression. In: Baer L, Blaid MA, editors. Handbook of clinical rating scales and assessment in psychiatry and mental health. Humana Press; Totowa, NJ: 2010. pp. 7–35. [Google Scholar]
- Daig I, Herschbach P, Lehmann A, Knoll N, Decker O. Gender and age differences in domain-specific life satisfaction and the impact of depressive and anxietysymptoms: A general population survey from Germany. Quality of Life Research. 2009;18(6):669–678. doi: 10.1007/s11136-009-9481-3. doi: http://dx.doi.org/10.1007/s11136-009-9481-3. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Potts NL, Richichi EA, Ford SM, Krishnan KR, Smith RD, Wilson W. The Brief Social Phobia Scale. The Journal of Clinical Psychiatry. 1991;52(Suppl):48–51. doi: 10.1037/t07672-000. [DOI] [PubMed] [Google Scholar]
- Dawes RM, Faust D, Meehl PE. Clinical versus actuarial judgment. Science. 1989;243(4899):1668–1674. doi: 10.1126/science.2648573. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Measuring informant discrepancies in clinical child research. Psychological Assessment. 2004;16(3):330–334. doi: 10.1037/1040-3590.16.3.330. doi: 10.1037/1040-3590.16.3.330. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131(4):485–509. doi: 10.1037/0033-2909.131.4.483. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Chang K, Welge JA, Adler CM, Rana M, Howe M, Strakowski SM. A double-blind, placebo-controlled pilot study of quetiapine for depressed adolescents with bipolar disorder. Bipolar Disorders. 2009;11(5):483–493. doi: 10.1111/j.1399-5618.2009.00728.x. doi: 10.1111/j.1399-5618.2009.00728.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Modern Problems of Pharmacopsychiatry. 1974;7(0):79–110. doi: 10.1159/000395070. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV) Pyschological Corporation; San Antonio, TX: 1994. [Google Scholar]
- Dugas MS, Freeston MH, Lachance S, Provencher M, Ladouceur R. Poster presned at the world congress of behavioral and cognitive therapies. Copenhagen, Denmark: 1995. Worry and Anxiety Questionnaire: Initial validation in non clinical and clinical samples. [Google Scholar]
- Dugas MJ, Freeston MH, Provencher MD, Lachance S, Ladouceur R, Gosselin P. Worry and Anxiety Questionnaire. Journal de Thérapie Comportementale et Cognitive. 2001;11(1):31–36. [Google Scholar]
- Dugas MJ, Ladouceur R, Léger E, Freeston MH, Langolis F, Provencher MD, Boisvert JM. Group cognitive-behavioral therapy for generalized anxiety disorder: Treatment outcome and long-term follow-up. Journal of Consulting and Clinical Psychology. 2003;71(4):821–825. doi: 10.1037/0022-006x.71.4.821. doi:10.1037/0022-006X.71.4.821. [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Weisz JR. A psychometric analysis of the revised child anxiety and depression scale--Parent version in a clinical sample. Journal of Abnormal Child Psychology. 2010;38(2):249–260. doi: 10.1007/s10802-009-9363-8. doi: 10.1007/s10802-009-9363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Chorpita BF, Weisz JR. A transportable assessment protocol for prescribing youth psychosocial treatments in real-world settings: Reducing assessment burden via self-report scales. Psychological Assessment. 2012;24(1):141–155. doi: 10.1037/a0025176. doi: 10.1037/a0025176. [DOI] [PubMed] [Google Scholar]
- Elkins RM, Pincus DB, Comer JS. A psychometric evaluation of the Panic Disorder Severity Scale for Children and Adolescents. Psychological Assessment. 2013 Dec 2; doi: 10.1037/a0035283. advance online publication. doi: 10.1037/a0035283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg SM, Ross AW. Assessment of child behavior problems: The validation of a new inventory. Journal of Clinical Child Psychology. 1978;7(2):113–116. [Google Scholar]
- Fairbum CG, Cooper Z. The Eating Disorder Examination. In: Fairbum CG, editor. Binge eating: Nature, assessment, and treatment. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- Farrand P, Woodford J. Measurement of individualised quality of life amongst young people with indicated personality disorder during emerging adulthood using the SEIQoL-DW. Quality of Life Research. 2013;22(4):829–838. doi: 10.1007/s11136-012-0210-y. doi: 10.1007/s11136-012-0210-y. [DOI] [PubMed] [Google Scholar]
- Fendrich M, Weissman MM, Warner V. Screening for depressive disorder in children and adolescents: Validating the Center for Epidemiologic Studies Depression Scale for Children. American Journal of Epidemiology. 1990;131(3):538–551. doi: 10.1093/oxfordjournals.aje.a115529. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSMIV Axis I Disorders, Clinician Version (SCID-CV) American Psychiatric Press, Inc.; Washington, D.C.: 1996. [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KR. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child & Adolescent Psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Ford JD, Racusin R, Ellis CG, Daviss WB, Reiser J, Fleischer A, Thomas J. Child maltreatment, other trauma exposure and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment. 2000;5(3):205–217. doi: 10.1177/1077559500005003001. Retrieved from http://search.proquest.com/docview/619464325?accountid=14707. [DOI] [PubMed] [Google Scholar]
- Foy DW, Wood JL, King DW, King LA, Resnick HS. Los AngelesSymptom Checklist: Psychometric evidence with an adolescent sample. Assessment. 1997;4(4):377–384. doi: 10.1177/107319119700400408. [Google Scholar]
- Fredrick CJ, Pynoos RS, Nader K. Childhood Posttraumatic Stress ReactionIndex. Copyrighted Instrument. 1992 [Google Scholar]
- Garb HN. Studying the clincian: Judgement research and psychological assessment. American Psychological Association; Washington, DC: 1998. [Google Scholar]
- Garb HN. Clinical judgement and decision making. Annual Review of ClinicalPsychology. 2005;1:67–89. doi: 10.1146/annurev.clinpsy.1.102803.143810. doi: 10.1146/annurev.clinpsy.1.102803.143810. [DOI] [PubMed] [Google Scholar]
- Garcia-Campayo J, Zamorano E, Ruiz MA, Pardo A, Perez-Paramo M, Lopez-Gomez V, Rejas J. Cultural adaptation into Spanish of the Generalized Anxiety Disorder-7 (GAD-7) scale as a screening tool. Health and Quality of Life Outcomes. 2010;8:8. doi: 10.1186/1477-7525-8-8. doi: 10.1186/1477-7525-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Kruse M, Aarons GA. Clinicians and outcome measurement:What's the use? Journal of Behavioral Health Services & Research. 2003;30(4):393–405. doi: 10.1007/BF02287427. [DOI] [PubMed] [Google Scholar]
- Garner DM. Eating Attitudes Test (EAT-26): Scoring and interpretation. 2010 Retrieved from http://www.eat-26.com/Docs/EAT-26IntpretScoring-Test-3-20-10.pdf.
- Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The Eating Attitudes Test:Psychometric features and clinical correlates. Psychological Medicine. 1982;12(4):871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- George D, Mallery P. SPSS for windows step by step: A simple guide and reference 12.0 update. 15th ed. Pearson Education New Zealand; Auckland, New Zealand: 2005. [Google Scholar]
- Giffort D, Schmook A, Woody C, Vollendorf C, Gervain M. RecoveryAssessment Scale. Illinois Department of Mental Health; Chicago, IL: 1995. [Google Scholar]
- Glasgow RE, Riley WT. Pragmatic measures: What they are and why we need them. American Journal of Preventative Medicine. 2013;45(2):237–243. doi: 10.1016/j.amepre.2013.03.010. doi: 10.1016/j.amepre.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman R. What is the SDQ? 2012 Retrieved from http://www.sdqinfo.org/a0.html.
- Goodman J, McKay J, DePhilippis D. Progress monitoring in mental health and addiction treatment: A means of improving care. Professional Psychology: Research and Practice. in press. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Charney DS. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Gosselin P, Dugas MJ, Ladouceur R, Freeston MH. Evaluation of worry: Validation of a French translation of the Penn State Worry Questionnaire. L'Encéphale. 2001;27(5):475–484. [PubMed] [Google Scholar]
- Gracious BL, Holmes WD, Ruppar N, Burke KC, Hurt J. Mania Rating Scale reliability in children and adolescents.. Presented at the First Annual International Conference on Bipolar Disorders; Pittsburgh. 1994. [Google Scholar]
- Gracious BL, Youngstrom EA, Findling RL, Calabrese JR. Discriminative validity of a parent version of the Young Mania Rating Scale. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(11):1350–1359. doi: 10.1097/00004583-200211000-00017. doi: 10.1097/00004583-200211000-00017. [DOI] [PubMed] [Google Scholar]
- Green B. Trauma History Questionnaire. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Sidran Press; Lutherville, MD: 1996. pp. 366–369. [Google Scholar]
- Greenhill LL, Pine D, March J, Birmaher B, Riddle M. Assessment issues in treatment research of pediatric anxiety disorders: What is working, what is not working, what is missing, and what needs improvement. Psychopharmacology Bulletin. 1998;34(2):155–164. [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of MedicalPsychology. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, andPsychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Hamilton rating scale for Depression (Ham-D). In: American Psychiatric Association; Rush AJ, editor. Handbook of psychiatric measures. American Psychogical Association; Washington, D.C.: 2000. pp. 526–528. [Google Scholar]
- Hancock N, Bundy A, Honey A, Tamsett S, Helich S. Sydney eScholarship Repository. University of Sydney; Sydney, Austrailia: 2013. Recovery Assessment Scale: Domains and stages (RAS-DS). [Google Scholar]
- Hatfield DR, Ogles BM. Why some clinicians use outcome measures and others do not. Administration and Policy in Mental Health and Mental Health Services Research. 2007;34(3):283–291. doi: 10.1007/s10488-006-0110-y. doi: 10.1007/s10488-006-0110-y. [DOI] [PubMed] [Google Scholar]
- Hautala L, Junnila J, Helenius H, Väänänen A, Liuksila P, Räihä H, Saarijärvi S. Adolescents with fluctuating symptoms of eating disorders: A 1-year prospective study. Journal of Advanced Nursing. 2008;62(6):674–680. doi: 10.1111/j.1365-2648.2008.04697.x. doi: 10.1111/j.1365-2648.2008.04697.x. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Horber KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, Liebowitz MR. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine. 1999;29:199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Helmreich I, Wagner S, Mergl R, Allgaier AK, Hautzinger M, Henkel V, Tadíc A. Sensitivity to changes during antidepressant treatment: A comparison of unidimensional subscales of the Inventory of Depressive Symptomatology (IDS-C) and the Hamilton Depression Rating Scale (HAMD) in patients with mild major, minor, or subsyndromal depresssion. European Archives of Psychiatry and Clinical Neuroscience. 2011;262(4):291–304. doi: 10.1007/s00406-011-0263-x. doi: 10.1007/s00406-011-0263-x. [DOI] [PubMed] [Google Scholar]
- Hill LS, Reid F, Morgan JF, Lacey JH. SCOFF, the development of an eating disorder screening questionnaire. International Journal of Eating Disorders. 2010;43(4):344–351. doi: 10.1002/eat.20679. doi: 10.1002/eat.20679. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Dibartolo PM. An instrument to assess self-statements during public speaking: Scale development and preliminary psychometric properties. Behavior Therapy. 2000;31(3):499–515. doi: 10.1016/s0005-7894(00)80027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper LM, Stockton P, Krupnick JL, Green BL. The development, use, and psychometric properties of the Trauma History Questionnaire. Journal of Loss and Trauma. 2011;16(3):258–283. doi:10.1080/15325024.2011.572035. [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the panic disorder severity scale. Depression and Anxiety. 2002;15(4):183–185. doi: 10.1002/da.10049. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized control trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(5):533–544. doi: 10.1097/CHI.0b013e31819c2401. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- Hunsley J, Mash E, editors. Introduction to the special section on developing guidelines for the evidence-based assessment of adult disorders [Special Issue]. Psychological Assessment. 2005;17(3):251–255. doi: 10.1037/1040-3590.17.3.251. doi:10.1037/1040-3590.17.3.251. [DOI] [PubMed] [Google Scholar]
- Hunsley J, Mash EJ. Evidence-based assessment. Annual Review of ClinicalPsychology. 2007;3:29–51. doi: 10.1146/annurev.clinpsy.3.022806.091419. doi: 10.1146/annurev.clinpsy.3.022806.091419. [DOI] [PubMed] [Google Scholar]
- Hunsley J, Mash EJ. A guide to assessments that work. 1st ed. Oxford University Press; New York: 2008. [Google Scholar]
- IDS-QUIDS.org. Inventory of Depressive Symptomatology (IDS) & Quick Inventory ofDepressive Symptomatology (QIDS) 2013 Retrieved from http://www.idsqids.org/index2.html#VALIDITY.
- International Society for Traumatic Stress Studies Assessing trauma: Child PTSDSymptom Scale. 2013 Retrieved from http://www.istss.org/ChildPTSDSymptomScale.htm.
- Ivanova MY, Achenbach TM, Rescorla LA, Dumenci L, Almqvist F, Bilenberg N, Verhulst FC. The generalizability of the Youth Self-Report syndrome structurein 23 societies. Journal of Consulting and Clinical Psychology. 2007;75(5):729–738. doi: 10.1037/0022-006X.75.5.729. doi: 10.1037/0022-006X.75.5.729. [DOI] [PubMed] [Google Scholar]
- Ivanova MY, Achenbach TM, Rescorla LA, Harder VS, Ang RP, Bilenberg N, Verhulst FC. Syndromes of preschool psychopathology reported by parents in 23 societies. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(12):1215–1224. doi: 10.1016/j.jaac.2010.08.019. doi: 10.1016/j.jaac.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivarsson T, Lidberg A, Gillberg C. The Birleson Depression Self-Rating Scale(DSRS): Clinical evaluation in an adolescent inpatient population. Journal of Affective Disorders. 1994;32(2):115–125. doi: 10.1016/0165-0327(94)90069-8. [DOI] [PubMed] [Google Scholar]
- Jellinek MS, Murphy JM, Robinson J, Feins A, Lamb S, Fenton T. ThePediatric Symptom Checklist: Screening school-age children for psychological dysfunction. Journal of Pediatrics. 1988;112(2):201–209. doi: 10.1016/s0022-3476(88)80056-8. doi: 10.1016/S0022-3476(88)80056-8. [DOI] [PubMed] [Google Scholar]
- Jensen-Doss A, Hawley KM. Understanding barriers to evidence-based assessment:Clinician attitudes toward standardized assessment tools. Journal of Clinical Child & Adolescent Psychology. 2010;39(6):885–896. doi: 10.1080/15374416.2010.517169. doi: 10.1080/15374416.2010.517169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen AL, Weisz JR. Assessing match and mismatch between practitioner-generated and standardized interview-generated diagnoses for clinic-referred children and adolescents. Journal of Consulting and Clinical Psychology. 2002;70(1):158–168. doi: 10.1037//0022-006X.70.1.158. [PubMed] [Google Scholar]
- Jensen-Doss A, Weisz JR. Diagnostic agreement predicts treatment process and outcomes in youth mental health clinics. Journal of Consulting and Clinical Psychology. 2008;76(5):711–722. doi: 10.1037/0022-006X.76.5.711. doi: 10.1037/0022-006X.76.5.711. [DOI] [PubMed] [Google Scholar]
- Johnson HS, Inderbitzen-Nolan HM, Anderson ER. The Social PhobiaInventory: Validity and reliability in an adolescent community sample. Psychological Assessment. 2006;18:269–277. doi: 10.1037/1040-3590.18.3.269. doi:101037/1040-3590183269. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Harris ES, Spitzer RL, Williams JBW. The Patient HealthQuestionnaire for Adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. Journal of Adolescent Health. 2002;30(3):196–204. doi: 10.1016/s1054-139x(01)00333-0. doi: http://dx.doi.org/10.1016/S1054-139X(01)00333-0. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Walker RL, Pettit JW, Perez M, Cukrowicz KC. Evidence-based assessment of depression in adults. Psychological Assessment. 2005;17(3):267–277. doi: 10.1037/1040-3590.17.3.267. doi: 10.1037/1040-3590.17.3.267. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based assessment for children and adolescents: Issues in measurement development and clinical application. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):548–558. doi: 10.1207/s15374424jccp3403_10. doi: 10.1207/s15374424jccp3403_10. [DOI] [PubMed] [Google Scholar]
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-RelatedPosttraumatic Stress Disorder: Three studies in reliability and validity. Journal of Consulting and Clinical Psychology. 1988;56(1):85–90. doi: 10.1037//0022-006x.56.1.85. doi: 10.1037/0022-006X.56.1.85. [DOI] [PubMed] [Google Scholar]
- Keller MB, Ryan ND, Strober M, Klein RG, Kutcher SP, Birmaher B, McCafferty JP. Efficacy of paroxetine in the treatment of adolescent major depression: A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(7):762–772. doi: 10.1097/00004583-200107000-00010. doi: 10.1097/00004583-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Kertz S, Bigda-Peyton J, Bjorgvinsson T. Validity of the Generalized AnxietyDisorder-7 Scale in an acute psychiatric sample. Clinical Psychology & Psychotherapy. 2013;20(5):456–464. doi: 10.1002/cpp.1802. doi: 10.1002/cpp.1802. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Leskin G, Foy DW. The Los Angeles SymptomChecklist: A self-report measure of posttraumatic stress disorder. Assessment. 1995;2(1):1–17. doi: 10.1177/1073191195002001001. [Google Scholar]
- Kovacs M. The Children's Depression Inventory (CDI). PsychopharmacologicalBulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kroenke K S, Spitzer RL, Williams B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12(2):210–224. doi: 10.1037//1040-3590.12.2.210. doi:10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Hansen N, Finch E. Patient-focused research: Using patient outcome data to enhance treatment effects. Journal of Consulting and Clinical Psychology. 2001;69:159–172. [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Lim YJ, Yu BH, Kim JH. Korean panic disorder severity scale: Construct validity by confirmatory factor analysis. Depression and Anxiety. 2007;24(2):95–102. doi: 10.1002/da.20206. doi: 10.1002/da.20206. [DOI] [PubMed] [Google Scholar]
- Lomas J. Diffusion, dissemination, and implementation: Who should do what? Annals of the New York Academy of Sciences. 1993;703:226–235. doi: 10.1111/j.1749-6632.1993.tb26351.x. doi: 10.1111/j.1749-6632.1993.tb26351.x. [DOI] [PubMed] [Google Scholar]
- Los Angeles County Department of Mental Health RCADS quick guide – Child. 2011 Retrieved from http://lausdsmh.net/wp-content/uploads/2012/03/RCADS-Child-Quick-Guide1.pdf.
- Löwe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Medical Care. 2004;42(12):1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- Luck AJ, Morgan JF, Reid F, O'Brien A, Brunton J, Price C, Lacy JH. The SCOFF questionnaire and clinical interview for eating disorders in general practice: Comparitive study. British Medical Journal. 2002;325:755. doi: 10.1136/bmj.325.7367.755. doi: 10.1136/bmj.325.7367.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disorders. Journal of Affective Disorders. 1988;14(1):61–68. doi: 10.1016/0165-0327(88)90072-9. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- Maloney MJ, McGuire JB, Daniels SR. Reliability testing of a children's version of the Eating Attitude Test. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27(5):541–543. doi: 10.1097/00004583-198809000-00004. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. TheMultidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, andvalidity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Marks IM, Mathews AM. Brief standard self-rating for phobic patients. BehaviourResearch and Therapy. 1979;17(3):263–267. doi: 10.1016/0005-7967(79)90041-x. doi: 0005-7967(79)90041-X. [DOI] [PubMed] [Google Scholar]
- Mash E, Hunsley J, editors. Evidence-based assessment of child and adolescent disorders: Issues and challenges [Special Issue]. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):1537–4416. doi: 10.1207/s15374424jccp3403_1. [DOI] [PubMed] [Google Scholar]
- Masia-Warner C, Storch EA, Pincus DB, Klein RG, Heimberg RG, Liebowitz MR. The Liebowitz Social Anxiety Scale for Children and Adolescents: An initial psychometric investigation. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(9):1076–1084. doi: 10.1097/01.CHI.0000070249.24125.89. [DOI] [PubMed] [Google Scholar]
- MassHealth PSD-Pediatric Symptom Checklist, Y-PSC-Pediatric Symptom Checklist-Youth Report. 2013 Retrieved from http://www.mass.gov/eohhs/gov/commissions-and-initiatives/cbhi/screening-for-behavioral-health-conditions/the-masshealth-approved-screening-tools/y-psc.html.
- Mathai J, Anderson P, Bourne A. Use of the Strengths and DifficultiesQuestionnaire as an outcome measure in a child and adolescent mental health service. Australasian Psychiatry. 2003;11:334–337. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36(4):455–470. doi: 10.1016/s0005-7967(97)10031-6. doi: S0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Mazure CM, Halmi KA, Sunday SR, Romano SJ, Einhorn AM. Yale-Brown-Cornell Eating Disorder Scale: Development, use, reliability, and validity. Journal of Psychiatric Research. 1994;28(5):425–445. doi: 10.1016/0022-3956(94)90002-7. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments. A review of current efforts. The American Psychologist. 2010;65(2):73–84. doi: 10.1037/a0018121. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Mancini DA, Srinivasan J, McCann S, Konarski JZ, Kennedy SH. The antidepressant effects of risperidone and olanzapine in bipolar disorder. Canadian Journal of Clinical Pharmacology. 2004;11:218–226. [PubMed] [Google Scholar]
- McMahon RJ, Frick PJ. Evidence-based assessment of conduct problems in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):477–505. doi: 10.1207/s15374424jccp3403_6. doi: 10.1207/s15374424jccp3403_6. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Michelson L, Mavissakalian M. Temporal stability of self-report measures in agoraphobia research. Behaviour Research and Therapy. 1983;21(6):695–698. doi: 10.1016/0005-7967(83)90089-x. doi: 10.1016/0005-7967(83)90089-X. [DOI] [PubMed] [Google Scholar]
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. doi: 10.1001/jama.290.1.57 290/1/57. [DOI] [PubMed] [Google Scholar]
- Moberg PJ, Lazarus LW, Mesholam RI, Bilker W, Chuy IL, Neyman I, Markvart V. Comparison of the standard and structured interview guide for the Hamilton Depression Rating Scale in depressed geriatric inpatients. The American Journal of Geriatric Psychiatry. 2001;9(1):35–40. [PubMed] [Google Scholar]
- Monga S, Birmaher B, Chiappetta L, Brent D, Kaufman J, Bridge J, Cully M. Screen for Child Anxiety-Related Emotional Disorders (SCARED): Covergent and divergent validity. Depression and Anxiety. 2000;12(2):85–91. doi: 10.1002/1520-6394(2000)12:2<85::AID-DA4>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Monkul ES, Tural U, Onur E, Fidaner H, Alkin T, Shear MK. Panic DisorderSeverity Scale: Reliability and validity of the Turkish version. Depression and Anxiety. 2004;20(1):8–16. doi: 10.1002/da.20011. doi: 10.1002/da.20011. [DOI] [PubMed] [Google Scholar]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychological Assessment. 2008;20(2):131–138. doi: 10.1037/1040-3590.20.2.131. doi: 10.1037/1040-3590.20.2.131 2008-06771-005. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: Assessment of a new screening tool for eating disorders. British Medical Journal. 1999;319(7223):1467–1468. doi: 10.1136/bmj.319.7223.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motooka H, Tanaka-Matsumi J, Hayashi K. The reliability and validity of a Japanese version of the Penn State Worry Questionnaire (PSWQ): A self-report inventory of “worry”. Japanese Journal of Counseling Science. 2009;42(3):247–255. [Google Scholar]
- Mueser KT, Rosenberg SD, Fox L, Salyers MP, Ford JD, Carty P. Psychometric evaluation of trauma and posttraumtic stress disorder assessments in persons with severe mental illness. Psychological Assessment. 2001;13(1):110–117. doi: 10.1037//1040-3590.13.1.110. doi: 10.1037/1040-3590.13.1.110. [DOI] [PubMed] [Google Scholar]
- Muris P, Mayer B, Bartelds E, Tierney S, Bogie N. The revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R): Treatment sensitivity in an early intervention trial for childhood anxiety disorders. British Journal of Clinical Psychology. 2001;40(3):323–36. doi: 10.1348/014466501163724. [DOI] [PubMed] [Google Scholar]
- Murphy JM, Jellinek MS. Screening for psychological dysfunction in economically disadvangted and minority group children: Further validation of the Pediatric Symptom Checklist. American Journal of Orthopsychiatry. 1988;58(3):450–456. doi: 10.1111/j.1939-0025.1988.tb01605.x. [DOI] [PubMed] [Google Scholar]
- Murphy JM, Kamin H, Masek B, Vogeli C, Caggiano R, Sklar K, Jellinek MS. Using brief clinician and parent measures to track outcomes in outpatient child psychiatry: Longer term follow-up and comparative effectiveness. Child and Adolescent Mental Health. 2012;17(4):222–230. doi: 10.1111/j.1475-3588.2011.00642.x. doi: 10.1111/j.1475-3588.2011.00642.x. [DOI] [PubMed] [Google Scholar]
- Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children's anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behaviour Research and Therapy. 2004;42(7):813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- NIH-PROMIS PROMIS: Dynamic tools to measure health outcomes from the patient perspective. 2013 Retrieved from http://nihpromis.org.
- Nunno M. The effects of the ARC organizational intervention on caseworker turnover, climate, and culture in children's services systems: Commentary. Child Abuse and Neglect. 2006;30(8):849–854. doi: 10.1016/j.chiabu.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Oei TP, Moylan A, Evans L. Validity and clinical utility of the Fear Questionnaire for anxiety-disorder patients. Psychological Assessment. 1991;3(3):391–397. doi: 10.1037/1040-3590.3.3.391. [Google Scholar]
- Ogles B, Melendez G, Davis DC, Lunnen KM. The Ohio Scales: Practical outcome assessment. Journal of Child and Family Studies. 2001;10(2):199–212. doi:10.1023/A:1016651508801. [Google Scholar]
- Orsillo SM. Measures for acute stress disorder and posttraumatic stress disorder. In: Antony MM, Orsillo SM, Roemer L, editors. Practitioner's guide to empirically based measures of anxiety. Springer; New York: 2001. pp. 255–307. [Google Scholar]
- Osman A, Bagge CL, Guitierrez PM, Konick LC, Kooper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and non clinical samples. Assessment. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Osman JR, Markway K. Further psychometric evaluation of the Fear Questionnaire: Responses of college-students. Psychological Reports. 1993;73(3 Pt. 2):1259–1266. doi: 10.2466/pr0.1993.73.3f.1259. [DOI] [PubMed] [Google Scholar]
- Pavot W, Diener E. Review of the Satisfaction with Life Scale. Psychological Assessment. 1993;5(2):164–172. [Google Scholar]
- Pavuluri MN, Henry DB, Devineni B, Carbray JA, Birmaher B. Child Mania Rating Scale: Development, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):550–560. doi: 10.1097/01.chi.0000205700.40700.50. doi: 10.1097/01.chi.0000205700.40700.50. [DOI] [PubMed] [Google Scholar]
- Perry L, Morgan J, Reid F, Brunton J, O'Brien A, Luck A, Lacey H. Screening for symptoms of eating disorders: Reliability of the SCOFF screening tool with written compared to oral delivery. International Journal of Eating Disorders. 2002;32(4):466–472. doi: 10.1002/eat.10093. doi: 10.1002/eat.10093. [DOI] [PubMed] [Google Scholar]
- Pestle SL, Chorpita BF, Schiffman J. Psychometric properties of the Penn StateWorry Questionnaire for Children in a large clinical sample. Journal of Clinical Child and Adolescent Psychology. 2008;37(2):465–471. doi: 10.1080/15374410801955896. doi: 10.1080/15374410801955896. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, St John D, McCormick B, Allen J, Black DW. Reliability and validity of the Borderline Evaluation of Severity over Time (BEST): A self-rated scale to measure severity and change in persons with borderline personality disorder. Journal of Personality Disorders. 2009;23(3):281–293. doi: 10.1521/pedi.2009.23.3.281. doi: 10.1521/pedi.2009.23.3.281 10.1521/pedi.2009.23.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PHQ Screeners PHQ-9 and GAD-7 Instruction Manual. 2010 Retrieved from: http://www.phqscreeners.com/instructions/instructions.pdf.
- Pogge DL, Wayland-Smith D, Zaccario M, Borgaro S, Stokes J, Harvey PD. Diagnosis of manic episodes in adolescent inpatients: Structured diagnostic procedures compared to clinical chart diagnoses. Psychiatry Research. 2001;101(1):47–54. doi: 10.1016/s0165-1781(00)00248-1. doi: 10.1016/S0165-1781(00)00248-1. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Mann JJ. The Columbia-Suicide Severity Rating Scale (C-SSRS): Initial validity and internal consistency findings from three multi-site studies with adolescents and adults. American Journal of Psychiatry. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, York JL. A compilation of strategies for implementing clinical innovations in health and mental health. Medical Care Research and Review. 2012;69(2):123–157. doi: 10.1177/1077558711430690. doi:10.1177/10775587114306901077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- President's New Freedom Commission on Mental Health . Report of the President's NewFreedom Commission on Mental Health. Washington, DC.: 2003. [Google Scholar]
- Psych Congress Network Hamilton Depression Rating Scale (HAM-D) 2013 Retrieved from: http://www.psychcongress.com/saundras-corner/scales-screeners/depression/hamilton-depression-rating-scale-ham-d.
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Ranta K, Kaltiala-Heino R, Rantanen P, Marttunen M. The Mini-Social PhobiaInventory: Psychometric properties in an adolescent general population sample. Comprehensive Psychiatry. 2012;53(5):630–637. doi: 10.1016/j.comppsych.2011.07.007. doi: 10.1016/j.comppsych.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children's manifest anxiety. Journal of Abnormal Child Psychology. 1978;6(2):271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Riemer M, Athay MM, Bickman L, Breda C, Kelley SD, Vides de Andrade AR. The Peabody Treatment Progress Battery: History and methods for developing a comprehensive measurement battery for youth mental health. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39(1-2):3–12. doi: 10.1007/s10488-012-0404-1. doi: 10.1007/s10488-012-0404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riemer M, Kearns MA. Description and psychometric evaluation of the Youth Counseling Impact Scale. Psychological Assessment. 2010;22(2):259–268. doi: 10.1037/a0018507. doi: 10.1037/a0018507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C. The Inventory for Depressive Symptomatology (IDS): Preliminary findings. Psychiatry Research. 1986;18(1):65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine. 1996;26(3):477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi M, Carmody TJ, Biggs MM, Shores-Wilson K, Ibrahim H, Crismon ML. One-year clinical outcomes of depressed public sector outpatients: A benchmark for subsequent studies. Biological Psychiatry. 2004;56(1):46–53. doi: 10.1016/j.biopsych.2004.04.005. doi: 10.1016/j.biopsych.2004.04.005S0006322304004779. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Keller MB. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician rating (QIDS-C), and Self-Report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Stable Resource Toolkit SAMHSA. The Patient Health Questionnaire (PHQ-9)-Overview. 1999 Retrieved from: http://www.cqaimh.org/pdf/tool_phq9.pdf.
- Saylor CF, Swenson CC, Reynolds SS, Taylor M. The Pediatric EmotionalDistress Scale: A brief screening measure for young children exposed to traumatic events. Journal of Clinical Child Psychology. 1999;28(1):70–81. doi: 10.1207/s15374424jccp2801_6. [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Leckman JF. Children's Yale-Brown Obsessive Compulsive Scale: Reliability and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(6):844–852. doi: 10.1097/00004583-199706000-00023. http://dx.doi.org/10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Seligson JE, Huebner ES, Valois RF. Preliminary validation of the BriefMultidimensional Students' Life Satisfaction Scale (BMSLSS). Social Indicators Research. 2003;61(2):121–145. [Google Scholar]
- Shachar I, Aderka IM, Gilboa-Schechtman E. The factor structure of theLiebowitz Social Anxiety Scale for children and adolescents: Development of a brief version. Child Psychiatry and Human Development. 2013 doi: 10.1007/s10578-013-0398-2. doi: 10.1007/s10578-013-0398-2. [DOI] [PubMed] [Google Scholar]
- Sharp LK, Lipsky MS. Screening for depression across the lifespan: A review of measures for use in primary care settings. American Family Physician. 2002;66(6):1001–1008. [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Papp LA. Multicenter collaborative Panic Disorder Severity Scale. The American Journal of Psychiatry. 1997;154(11):1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, Wang T. Reliability and validity of the Panic Disorder Severity Scale: Replication andextenstion. Journal of Psychiatric Research. 2001;35(5):293–296. doi: 10.1016/s0022-3956(01)00028-0. doi: 10.1016/S0022-3956(01)00028-0. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and Parent Version. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):380–411. doi: 10.1207/s15374424jccp3403_2. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Smith P, Perrin S, Dyregrov A, Yule W. Principal components analysis of theImpact of Event Scale with children in war. Personality and Individual Differences. 2003;34:315–322. doi:10.1016/S0191-8869(02)00047-8. [Google Scholar]
- Smolak L, Levine MP. Psychometric properties of the Children's Eating AttitudesTest. International Journal of Eating Disorders. 1994;16(3):275–282. doi: 10.1002/1098-108x(199411)16:3<275::aid-eat2260160308>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Hoza B, Pelham WE, Rapoff M, Ware L, Danovsky M, Stahl KJ. The development and validation of the Children's Hope Scale. Journal of Pediatr Psychology. 1997;22(3):399–421. doi: 10.1093/jpepsy/22.3.399. [DOI] [PubMed] [Google Scholar]
- Spence SH. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36(5):545–566. doi: 10.1016/s0005-7967(98)00034-5. doi: S0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Spence SH, Rapee R, McDonald C, Ingram M. The structure of anxiety symptoms among preschoolers. Behaviour Research and Therapy. 2001;39:1293–1316. doi: 10.1016/s0005-7967(00)00098-x. [DOI] [PubMed] [Google Scholar]
- Spence Children's Anxiety Scale Website Overview: Use of the scale. 2013 Retrieved from: http://www.scaswebsite.com/index.php?p=1_12.
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-Ill-R (SCID) American Psychiatric Press; Washington, D.C.: 1990. [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating Disorder Diagnostic Scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16(1):60–71. doi: 10.1037/1040-3590.16.1.60. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Stice E, Hayward C, Cameron R, Killen JD, Taylor CB. Body image and eating related factors predict onset of depression in female adolescents: A longitudinal study. Journal of Abnormal Psychology. 2000;109:438–444. [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating DisorderDiagnostic Scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment. 2000;12(2):123–131. doi: 10.1037//1040-3590.12.2.123. doi: 10.1037/1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Stöber J, Bittencourt J. Weekly assessment of worry: An adaptation of the PennState Worry Questionnaire for monitoring changes during treatment. Behaviour Research and Therapy. 1998;36:645–656. doi: 10.1016/s0005-7967(98)00031-x. [DOI] [PubMed] [Google Scholar]
- Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P, Goodman WK. Psychometric evaluation of the Children's Yale-Brown Obsessive-Compulsive Scale. Psychiatry Research. 2004;129(1):91–98. doi: 10.1016/j.psychres.2004.06.009. doi: 10.1016/j.psychres.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Strober M, DeAntonio M, Schmidt-Lackner S, Freeman R, Lampert C, Diamond J. Early childhood attention deficit hyperactivity disorder predicts poorer response to acute lithium therapy in adolescent mania. Journal of Affective Disorders. 1998;51(2):145–151. doi: 10.1016/s0165-0327(98)00213-4. Retrieved from http://search.proquest.com/docview/619416075?accountid=14707. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition, and hunger. Journal of Psychosomatic Research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Stable Resource Toolkit. 1999 Retrieved from: http://www.integration.samhsa.gov/images/res/STABLE_toolkit.pdf.
- Swenson CC, Brown EJ, Sheidow AJ. Medical, legal, and mental health service utilization by physically abused children and their caregivers. Child Maltreatment. 2003;8(2):138–144. doi: 10.1177/1077559502250813. [DOI] [PubMed] [Google Scholar]
- Tangen Haug T, Blomhoff S, Hellstrom K, Holme I, Humble M, Petter Madsu H, Egil Wood J. Exposure therapy and sertraline in social phobia: I-year follow-up of a randomised controlled trial. The British Journal of Psychiatry. 2003;182:312–318. doi: 10.1192/bjp.182.4.312. doi: 10.1192/bjp.02.229. [DOI] [PubMed] [Google Scholar]
- Taylor TK, Burns GL, Rusby JC, Foster EM. Oppositional defiant disorders towards adults and oppositional defiant disorders towards peers: Initial evdience for two separate constructs. Psychological Assessment. 2006;18(4):439–443. doi: 10.1037/1040-3590.18.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Child Traumatic Stress Network Pediatric Emotional Distress Scale. 2012 Retrieved from http://www.nctsn.org/content/pediatric-emotional-distress-scale.
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Kashner TM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), the Quick Inventory of Depressive Symtomatology,Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: A psychometric evaluation. Psychological Medicine. 2004;34(1):73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Hillerbrand E. Psychometric properties and factor structure of the FearQuestionnaire phobia subscale items in two normative samples. Journal of Psychopathology and Behavioral Assessment. 1990;12(4):285–297. [Google Scholar]
- United States Department of Health and Human Services, National Institutes of Health . The National Institute of Mental Health Strategic Plan. National Institutes of Health; Rockville, MD: 2008. (NIH Publication No. 08–6368. Retrieved from http://www.nimh.nih.gov/about/ [Google Scholar]
- Verhulst FC, van der Ende J. Assessment Scales in Child and Adolescent Psychiatry. Taylor & Francis; Boca Raton, FL: 2006. [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement. 1993;1(2):165–178. [PubMed] [Google Scholar]
- Wang R, Su J, Bi X, Wei Y, Mo L, You Y. Application of the chinesePosttraumatic Stress Disorder Checklist to adolescent earthquake survivors in China. Social Behavior and Personality. 2012;40(3):415–424. doi: 10.2224/sbp.2012.40.3.415. [Google Scholar]
- Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Watson D, Clark AL. The Mood and Anxiety Symptom Questionnaire (MASQ).Unpublished manuscript. University of Iowa, Department of Psychology; Iowa City, IA: 1991. [Google Scholar]
- Watson D, Friend R. Measurement of social-evaluative anxiety. Journal ofConsulting and Clinical Psychology. 1969;33(4):448–457. doi: 10.1037/h0027806. doi: 10.1037/h0027806. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility.. Paper presented at the 9th Annual Conference of the International Society for Traumatic Stress Studies; San Antonio, TX.: 1993. [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale—Revised. In: Wilson JPK, Keane TM, editors. Assessing psychological trauma and PTSD: A handbook for practitioners. Guilford Press; New York: 1997. pp. 399–411. [Google Scholar]
- Weisz JR, Chorpita BF, Frye A, Ng MY, Lau N, Bearman SK, Hoagwood KE. Youth Top Problems: Using idiographic, consumer-guided assessment to identify treatment needs and to track change during psychotherapy. Journal of Consulting and Clinical Psychology. 2001;79(3):369–380. doi: 10.1037/a0023307. doi: 10.1037/a0023307. [DOI] [PubMed] [Google Scholar]
- West AE, Ceilo CI, Henry DB, Pavuluri MN. Child Mania Rating Scale-Parent Version: A valid measure of symptom change due to pharmacotherapy. Journal of Affective Disorders. 2011;128(1-2):112–119. doi: 10.1016/j.jad.2010.06.013. doi: 10.1016/j.jad.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety. 2011;28(7):596–606. doi: 10.1002/da.20837. doi: 10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JBW. A structured interview guide for the Hamilton Depression RatingScale. Archives of General Psychiatry. 1988;45(8):742–747. doi: 10.1001/archpsyc.1988.01800320058007. doi:10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Prather RC, McKenzie SJ, Blouin DC. Behavioral assessment procedures can differentiate bulimia nervosa, compulsive overeater, obese, and normal. Behavioral Assessment. 1990;12:239–252. [Google Scholar]
- Wilson KA, Hayward C. Unique contributions of anxiety sensitivity to avoidance:A prospective study in adolescents. Behaviour Research and Therapy. 2006;44(4):601–609. doi: 10.1016/j.brat.2005.04.005. doi: 10.1016/j.brat.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: A systematic review. General Hospital Psychiatry. 2007;29(5):388–395. doi: 10.1016/j.genhosppsych.2007.06.004. doi: 10.1016/j.genhosppsych.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Yamamoto I, Nakano Y, Watanabe N, Noda Y, Furukawa TA, Kanai T, Kamijima K. Cross-cultural evaluation of the Panic Disorder Severity Scale in Japan. Depression and Anxiety. 2004;20(1):17–22. doi: 10.1002/da.20029. doi: 10.1002/da.20029. [DOI] [PubMed] [Google Scholar]
- Xia L, Ding C. The relationship between interpersonal traits and posttraumatic stress disorder symptoms: Analyses from wenchuan earthquake adolescent survivors in China. Journal of Traumatic Stress. 2011;24(4):487–490. doi: 10.1002/jts.20655. doi: 10.1002/jts.20655. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania:Reliability, validity and sensitivity. The British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Young SL, Bullock WA. The Mental Health Recovery Measure. Department of Psychology, University of Toledo; Toledo, Ohio: 2003. [Google Scholar]
- Youngstrom EA, Findling RL, Youngstrom JK, Calabrese JR. Toward an evidence-based assessment of pediatric bipolar disorder. Journal of Clinical Child & Adolescent Psychology. 2005;34(3):433–448. doi: 10.1207/s15374424jccp3403_4. doi: 10.1207/s15374424jccp3403_4. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Choukas-Bradley S, Calhoun C, Jensen-Doss A. Clinical guide to the evidence-based medicine approach to diagnosis. Cognitive and Behavioral Practice. this issue. [Google Scholar]
- Zanarini MC. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): A continuous measure of DSM-IV borderline psychopathology. Journal of Personality Disorders. 2003;17(3):233–242. doi: 10.1521/pedi.17.3.233.22147. [DOI] [PubMed] [Google Scholar]
- Zhong J, Wang C, Li J, Liu J. Penn State Worry Questionnaire: Structure and psychometric properties of the Chinese version. Journal of Zhejiang University Science B. 2009;10(3):211–218. doi: 10.1631/jzus.B0820189. doi: 10.1631/jzus.B0820189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, McGlinchey JB, Posternak MA. A clinically useful depression outcome scale. Comprehensive Psychiatry. 2008;49(2):131–140. doi: 10.1016/j.comppsych.2007.10.006. doi: 10.1016/j.comppsych.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, McGlinchey JB, Chelminski I. An inadequate community stand of care: Lack of measurement of outcome when treating depression in clinical practice. Primary Psychiatry. 2008;13(6):67–75. [Google Scholar]
- Zimmerman M, Chelminski I, Young D, Dalrymple K. A clinically useful anxiety outcome scale. The Journal of Clinical Psychiatry. 2010;71(5):534–542. doi: 10.4088/JCP.09m05264blu. doi:10.4088/JCP.09m05264blu. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.