Abstract
Individuals with greater social capital have better health outcomes. Investment in social capital likely increases one’s own social capital, bearing great implications for disease prevention and health promotion. In this study, the authors developed and validated the Social Capital Investment Inventory (SCII). Direct effects of social capital investment on perceived stress, and indirect effects through social capital were examined. 397 Participants from Beijing and Wuhan, China completed surveys. Analyses demonstrated that the SCII has a single factor structure and strong internal consistency. Structural equation modeling showed that individuals who invested more in social capital had greater bonding social capital, and subsequently less perceived stress. Results suggest that disease prevention and health promotion programs should consider approaches to encourage social capital investment; individuals may be able to reduce stress by increasing their investment in social capital. Future research is needed to provide additional empirical support for the SCII and observed structural relationships.
Keywords: Social capital investment, Social capital, Perceived stress, Structural equation modeling
1 Introduction
Derived from economics and finance, social capital theory has successfully guided numerous researchers in advancing our understanding of the impact of social factors on health in both developed and developing countries across the globe (Murayama et al. 2012; Kaljee and Chen 2011). Converging evidence from diverse sources strongly suggests the existence of a positive relationship between social capital and health at the individual (Berkman et al. 2000; Chen et al. 2009a, 2011; Nieminen et al. 2010; Norstrand and Xu 2012; Poortinga 2006), community (Bartkowski and Xu 2007; Lochner et al. 2003; Miller et al. 2006; Poortinga 2006), national and global levels (Kawachi et al. 1997; Kennelly et al. 2003). Possession of more social capital is often associated with a number of positive health outcomes, including: longer life expectancy, lower infant mortality, lower total mortality, and better physical and psychosocial well-being (Miller et al. 2006; Norstrand and Xu 2012; Lazarus and Cohen 1977; Nieminen et al. 2010; Lin and Hsung 2001; Kawachi et al. 1997; Kennelly et al. 2003).
The observed associations of higher social capital with lower morbidity and mortality have encouraged researchers to explore approaches to foster social capital for health promotion and disease prevention. According to Lin (1999), social capital arises from “investment in social relationships with expected returns” (pg. 30). Therefore, to invest in one’s own social capital, an individual has to interact with others, such as talking together, working and playing together, visiting each other, joining social organizations, and participating in social events. Watching television alone at home does not produce social capital, but playing games as a team may produce social capital. Engaging in these types of activities may build trust and reciprocity in close relationships, resulting in the accumulation of social capital.
Reported studies have demonstrated positive effects of intervention programs aimed at building social capital (Harris et al. 2013; Michael et al. 2008; Ottesen et al. 2010; Pronyk et al. 2008). For example, the Poder es Salud/Power for Health program utilized community partnerships to develop a targeted social capital intervention program (Michael et al. 2008). This program included the development of health and education-based support groups, a public safety committee, and community sports teams (dance and soccer), among other components aimed at building social capital in the community. At the 8 month follow-up, participants reported having a greater number of social support providers, better physical health, and reduced depression and loneliness. Some of these positive outcomes may be linked to social capital investment behaviors that participants reported engaging in, such as helping others find jobs, providing food or housing, and increasing involvement in church activities (Michael et al. 2008).
The current study provides an initial investigation of the social capital investment construct, including a validation analysis of the construct by relating it with social capital and perceived stress. In the following sections, we first discuss the relevant literature regarding the concept of social capital, evidence of the linkage between social capital, psychological stress and health outcomes, and then discuss social capital investment and its potential structural relationship with perceived stress, including a direct path linking social capital investment to stress and an indirect path mediated through social capital (Fig. 1).
Fig. 1.
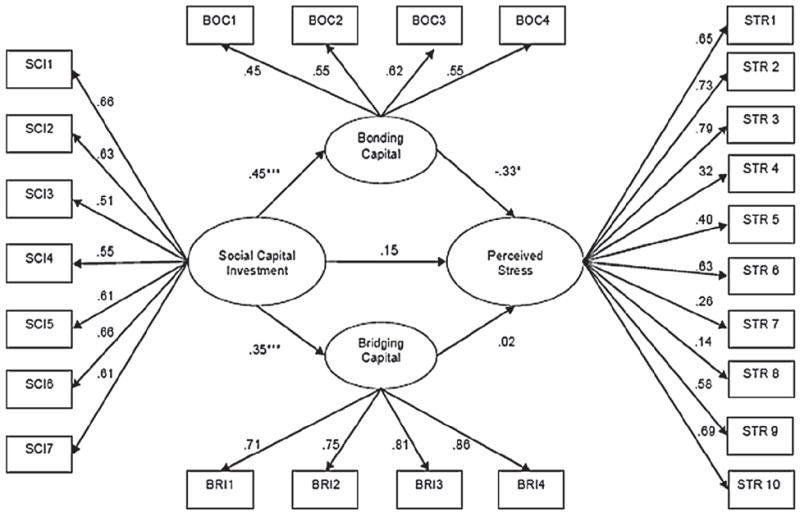
The relationship among social capital investment, social capital and perceived stress. Note Standardized path coefficient; *p < 0.05; **p < 0.01; ***p < 0.001. Data-model fit: GFI = 0.90, CFI = 0.93, RMSEA = 0.05, χ2/df = 1.92. The covariance (0.45) between the bonding and the bridging capital was not shown in the figure
1.1 Concept of Social Capital
In this study, we consider social capital as the direct outcome of social capital investment. Despite the considerable debate over the definition of social capital, a consensus has emerged that without network connections one cannot have social capital (Bourdieu 1986; Coleman 1988; Lin and Hsung 2001; Putnam 2001). In the current study, social capital is considered within a social-health framework (Kaljee and Chen 2011) and is examined at the individual level (Chen et al. 2009a, b). Based on our own research and the research of others, we defined social capital as part of the broad network connections that an individual accumulates in life that possess four fundamental characteristics: durability, trustworthiness, resource-rich and reciprocity (Chen et al. 2009a; Archuleta and Teasley 2013). As well, social capital is further discussed in terms of its bonding and bridging capabilities. Bonding social capital is preserved among an individual’s network ties with homogenous groups of people (e.g., same skin color, similar education), and is generated through free and uncharted mutual interactions with each other; whereas bridging capital is shared among heterogeneous groups of people (e.g., different races, reside in different countries/regions), and is generated through organized involvement in institutions and organizations (Putnam 2001; Szreter and Woolcock 2004).
1.1.1 Social Capital Contributes to Positive Health Outcomes
People who possess more social capital are more likely to have their health be impacted by their network members. Network members influence health behavior and knowledge via established social norms and the spread of health information, through monitoring and inhibiting negative health behaviors, and by fostering a sense of individual obligation to maintain health for the sake of others (Schwartz et al. 2003; Schwartz and Sendor 1999; Umberson and Montez 2010; Thoits 2011). Therefore, not only do sufficient levels of social capital allow already healthy people to maintain and promote health, but people who suffer from illness are also better equipped to obtain social, emotional and instrumental support for more effective treatment and recovery. Nieminen et al. (2010) examined how a variety of social capital measures related to self-rated health in a representative sample of Finnish adults. They found that (a) greater trust and reciprocity, (b) greater social participation and networks, and (c) greater social support were all related to better self-rated health, and greater psychological well-being, with trust and reciprocity as the strongest predictors.
1.1.2 Social Capital Can Reduce Psychological Stress
The impact of a stressor depends on the individual’s appraisal of the stressor and the psychological, social, and cultural resources available to them (Astone et al. 1999; Cohen 2004; Bolin et al. 2003). Beliefs that one has the necessary resources to control, change, or cope with a stressor can mitigate the potential negative impact of the stressor (Avey et al. 2009; Cohen 2004; Bolin et al. 2003). Social capital can provide such resources to fight against stress. Greater social capital helps reduce psychological stress through a number of pathways, including: social support provision, access to information and other resources, enhancing self-confidence, and bolstering self-worth. Close and trusted others are likely to provide instrumental and emotional support and coping assistance strategies, which help buffer the effects of stress by reducing the situational and psychological demands of the stressor (Thoits 2011). Individuals’ sense of personal control subsequently increases and this also helps to counteract the potential deleterious effects of the stressor (Atienza et al. 2001). Consistent with these conclusions, individuals with higher levels of self-esteem and feelings of self control have lower levels of psychological stress (Symister 2003; Atienza et al. 2001).
1.2 Concept of Social Capital Investment
The significant role of social capital in health promotion and disease prevention has prompted researchers to consider approaches to develop new forms of social capital and to maintain and enhance existing social capital (Glaeser et al. 2002). These efforts have included the development and implementation of a variety of community-level programs, but there has been little research on building social capital through individual-level investment in social capital. We have conceptualized individual attempts to obtain social capital based on the concepts of economic and financial investment. In economics, investment means to save or defer consumption for future development (Case et al. 2012). Therefore, economic investment serves as a long-term strategy for future growth and development. In finance, investment refers to putting money into something with the expectation of calculated gain, including short-term gain (e.g., stock market speculation) and long-term gain (e.g., bonds, stocks), and with an awareness of risk (Thaler 2005). Parallel to the concept in economics and finance, in this study we define social capital investment as efforts and resources that are devoted to daily activities to build social capital for both short-term and long-term needs, including need for personal health promotion and disease prevention (Kaljee and Chen 2011; Chen et al. 2009a).
Although the definition of social capital investment parallels that of economic and financial investment, social capital investment differs in important ways. Economic and financial investments are purposeful behavior, and the investments are made based on a solid trust between the investor and a financial agency, involving calculated investment decisions; they require individual wealth to invest; and those investments are transferrable to others. Social capital investments are culturally based; they often occur naturally and involve little or no conscious calculation at all; and social capital investment is to build trust by “investment”. Furthermore, a person does not need to be wealthy to invest in social capital. In addition to money and materials, an individual can invest his or her time and effort, or specific talents and strengths, which can often be given freely. Finally, an individual’s social capital is unique to him or her and is the culmination of his/her investments in his/her own interpersonal relationships. The bonds formed from the time and effort put into a relationship cannot be easily transferred to someone new.
1.2.1 Socializing Activities and Measurement of Capital Investment
Social capital research has elucidated the many ways in which social capital can be destroyed, but there is remarkably little research on how to build or maintain social capital (Ng and Jeffery 2003; Glaeser et al. 2002). Important barriers to examining investment in social capital have been the need for a clear definition and operationalization of the construct and the development of validated and reliable tools to measure social capital investment. In the previous sections we provided a conceptual definition of social capital investment. To meet the urgent research needs, here we discuss in greater detail how to quantify social capital investment.
Living in the modern society, every one of us engages in certain interpersonal activities on a daily basis. Greeting each other in the morning, sharing a coffee break with colleagues, playing or walking together with friends or a neighbor after dinner, watching television with family members, and long-distance visits to relatives; these are all examples of how individuals invest in their social relationships (Chen et al. 2009a; Lin 2002; Putnam 2001; Villar and Albertin 2010). Since these activities may result in social capital accumulation, they can be considered as investments in social capital. Today’s technology provides new approaches for investment in social capital through social media, mobile phones, and texting (Ellison et al. 2011; Steinfield et al. 2008). When engaging in these activities naturally and voluntarily (often with little effort), network connections will be maintained, expanded and strengthened, mutual trust increased, and reciprocity enhanced, resulting in more social capital (Chen et al. 2009a; Kaljee and Chen 2011). The Social Capital Investment Inventory (SCII), developed in the current study, attempts to systematically quantify these activities using modern psychometric and sociometric techniques.
1.2.2 Costs of Investment in Social Capital
Based on the discussion in the previous two sections, any interpersonal interactions that lead to the generation, accumulation, and maintenance of social capital (e.g., trustworthy, resourceful, and reciprocal network connections) can be considered as investment in social capital. Certainly, some social capital investment activities can require significant time, effort or money. These investments may include, but are not limited to: preparations for parties or special gifts for important occasions and events (wedding, birthday parties, graduation, etc.), provision of direct assistance to solve time- or effort-intensive problems (e.g., fixing a broken car, searching for a relevant school, securing a relevant and well-paid job, etc.), and acknowledgment of significant others who have contributed to the completion of important tasks (Bian 2004; Putnam 2001; Van Der Gaag and Webber 2010).
The exact costs of social capital investment are often dictated by larger cultural norms. For example, reciprocity norms foster a sense of obligation to reciprocate social capital investment behaviors from others (e.g., taking someone out to dinner for their birthday). Such norms ensure that the individual who initially invested will eventually see returns on their investment, which is beneficial for them. However, the recipient might now feel obligated to reciprocate, even when they might not have the time or money to be able to return the favor (Woolcock and Narayan 2000). The group cohesion that accompanies social capital investment can have numerous positive effects on in-group members, but it can also increase the likelihood that individuals who violate group norms will be isolated by the group (Woolcock and Narayan 2000). Considering the potential costs and benefits related to social capital investment and social capital highlights the importance of considering their impact on individual health outcomes.
1.3 Structural Relationship Among Social Capital Investment, Social Capital and Stress
The inclusion of social capital investment within a social-health framework provides an opportunity to validate a newly developed instrument to assess social capital investment, to investigate potential structural relationships assessing the strength of the relationships between social capital investments, levels of social capital and psychological stress. Based on the previous discussion regarding the well-established relationship between social capital and health (including stress), and the hypothesized relationship between social capital investment and social capital, we further hypothesized the following structural relationships: Social capital investment will increase social capital, and it is this increase in social capital which will be related to decrements in perceived stress. Second, it is possible that by investing in our own social relationships through social support provision to others and group involvement, we can increase our own happiness, self-esteem, self-efficacy, and confidence in our ability to cope with a future stressor (Cohen 1988). Thus, in addition to enhancing social capital, engaging in activities for social capital investment may have a direct effect, reducing perceived stress. As can be seen in Fig. 1, the relationship between social capital investment and perceived stress may contain both direct and indirect pathways through bridging and bonding social capital.
1.4 Purpose of This Study
The current study has three goals. First, the SCII was developed to assess investment in social capital. Based on our conceptualization, any interpersonal interactions that lead to the generation, accumulation, and maintenance of social capital (e.g., trustworthy, resourceful, and reciprocal network connections) can be considered as investment in social capital. The psychometric properties of this scale will be examined. Exploratory and confirmatory factor analyses will assess factor structure, and a reliability analysis will assess internal consistency.
Second, the relationship between social capital investment and social capital is examined. The Personal Social Capital Scale 16 (PSCS-16; Wang et al. 2013) is used to assess both bonding capital (e.g., horizontal ties between members of the same group) and bridging capital (e.g., ties across different groups; Putnam 2001). The current study examined bridging across two types of social organizations: (1) political, economic and governmental organizations, and (2) recreational, cultural, sports and other non-governmental organizations. A positive relationship between social capital investment and bonding and bridging social capital is anticipated. In general, relative to people who invest less in social capital, those who invest more will have a greater amount of social capital.
Finally, the relationships among social capital investment, levels of social capital and perceived stress (Cohen et al. 1983), were examined using a structural equation modeling approach. Both the direct and indirect effects of social capital investment on perceived stress are examined. The indirect pathways between both bonding capital and bridging capital are considered. The protective effects of social capital on health have been well documented (Chen et al. 2011; Murayama et al. 2012; O’Connor et al. 2011; Webber et al. 2011). However, bonding social capital, which reflects emotional support and access to resources provided by close family and friends, has been shown in the previous literature to have stronger and more positive effects on health outcomes (Cohen et al. 2003). Therefore, we expected a stronger effect of bonding capital, compared to bridging capital on perceived stress.
2 Data and Methods
2.1 Participants and Data Collection
Data used for this study were derived from a survey study jointly conducted by Wayne State University (WSU), Detroit MI, USA, and Beijing Normal University (BNU) and Wuhan Centers for Disease Prevention and Control (Wuhan CDC), China. The study protocol was approved by the relevant IRBs at BNU, the Wuhan CDC and the Human Investigation Committee at WSU. Survey data were collected during 2010–2011 in Beijing and Wuhan, including the urban areas and rural counties. Beijing, the capital of China has an estimated population of 20 million and per capita GDP of 12,643 dollars. Wuhan is the capital of Hubei Province, located in central China with a population of 9.1 million and per capita GDP of 10,960 dollars.
Participants (N = 387, 18–50 years of age) consisted of three subgroups: rural residents, urban residents, and rural-to-urban migrants. Non-migrant participants from rural and urban areas were recruited at their residential homes. One person per household was recruited to participate in the study. For households with more than one eligible participant, only one was selected using the random digits table method. Rural-to-urban migrants were recruited in workplaces with limitation to one person per type of occupation in each workplace. Among the eligible candidates we approached, approximately 90–95 % agreed to participate by signing the informed consent. We purposefully included participants with diverse backgrounds to enhance external validity of the study.
The survey was conducted using a paper-and-pencil questionnaire. The questionnaire was derived based on our previous research on HIV risk behaviors among rural-to-urban migrants in China (Chen et al. 2009b, 2011). The questionnaire covers general and demographic information, social capital investment and social capital, health and behavior measures and other influential factors. It took approximately 45 min for a typical participant to complete the survey. Trained data collectors from Beijing Normal University (graduate students in Psychology) and Wuhan CDC (staff with a college degree and three or more years of experience in field data collection) were dispatched to the field to recruit participants, and to administer the survey after obtaining the signed informed consent form. The survey was conducted following the protocol we established and previously used in Chinese settings for other projects (Chen et al. 2009b, 2011).
2.2 Measures
2.2.1 Measurement of Social Capital Investment
Social capital investment was the key predictor variable of this study. Since there was no ready-to-use instrument available in the published literature to assess the level of social capital investment at the individual level, we developed the SCII. The SCII is based on (1) our previous research on social capital and health risk behavior with data collected among rural-to-urban migrants in China (Chen et al. 2009a); (2) a thorough analysis of the characteristics of social capital investment, including a comparative analysis with the concept of investment in economics and finance and theoretical characterization of social capital investment as previously described in detail in the Introduction section of this paper; and (3) rigorous psychometric assessment.
The finalized SCII consists of seven items assessing seven activities commonly practiced by people for social networking in daily life (Table 2). A 5-point Likert scale was used to assess the frequency of each activity with 1 = “never,” 2 = “rarely,” 3 = “sometimes,” 4 = “often,” and 5 = “every day”. Cronbach’s alpha = 0.81. Measurement modeling analysis indicated that the data fit a one-factor model well (χ2/df = 1.83, GFI = 0.99, RMSEA = 0.05, CFI = 0.99). Individual items were used in structural equation modeling analysis and mean scores were computed and used in descriptive and bivariate analysis.
Table 2.
The Social Capital Investment Inventory (SCII)
| Scale item | N | Mean ± SD | r with total | Alpha if deleted |
|---|---|---|---|---|
| How often do you interact with others through the following? (1 = never, 5 = every day) | ||||
| 1. Talking and chatting together with others | 304 | 3.35 ± 0.82 | 0.55 | 0.77 |
| 2. Gift giving or gift exchanging | 304 | 2.57 ± 0.87 | 0.53 | 0.77 |
| 3. Working or doing things together | 297 | 3.03 ± 0.90 | 0.44 | 0.79 |
| 4. Entertaining, playing or traveling together | 304 | 2.39 ± 0.86 | 0.52 | 0.78 |
| 5. Communicating through telephone or internet | 304 | 3.21 ± 0.94 | 0.51 | 0.78 |
| 6. Offering assistance to others | 304 | 2.95 ± 0.86 | 0.57 | 0.77 |
| 7. Participating in parties and gathering | 304 | 2.76 ± 0.87 | 0.60 | 0.76 |
| Total scale | 297 | 2.90 ± 0.59 | 1.00 | 0.81 |
(1) Cronbach’s alpha = 0.81 for the SCII, data fit a one-factor model well (χ2/df = 1.83, GFI = 0.99, RMSEA = 0.05, CFI = 0.99). (2)The sample size N varied across items because of missing data. Pair-wise deletion was used in computing alpha coefficients
2.2.2 Measurement of Social Capital
Levels of social capital for individual participants were assessed using the Personal Social Capital Scale 16 (PSCS-16; Wang et al. 2013). The PSCS-16 was derived from the full version of the Personal Social Capital Scale. Cronbach’s alpha varied from 0.87 to 0.89 among different participant subgroups in China (Chen et al. 2009a). The scale was then validated independently by investigators in the United States (alpha = 0.85, Archuleta and Miller 2011). The PSCS-16 consists of 16 items with eight items assessing the bonding capital (network size, trustworthy, resource ownership, and reciprocity) and eight items assessing bridging capital, embedded in two types of social organizations (political, economic and governmental organizations/group; and creational, cultural, sports and other non-governmental organizations/groups). A 5-point Likert scale was used for item assessment. Correlation analysis indicated that alpha coefficients for the PSCS-16 were 0.88 and 0.90 for men and women respectively. Mean scores for the bonding and bridging subscales, as well as the total scale, were computed and used in descriptive and bivariate analysis.
2.2.3 Measurement of Perceived Stress
A translated and validated Chinese version (Wang et al. 2011) of the Perceived Stress Scale (PSS, Cohen et al. 1983) was used to measure global stress. As a proxy of mental health status, PSS uses 10 items to assess the frequencies (1 = never to 5 = always) of 10 different feelings/events that occurred in the past 30 days. Typical examples include: “felt upset because of unexpected things”, “unable to cope with all the things a person has to do”, and “felt angry because things are out of control”. The PSS is an empirically established scale that assesses an individual’s general stress level with adequate cross-cultural reliability (with Cronbach alpha >0.8) and validity (Almadi et al. 2012; Andreou et al. 2011; Lesage et al. 2012; Mimura and Griffiths 2008; Ramírez and Hernández 2007; Reis et al. 2010; Remor 2006; Wang et al. 2011). Cronbach’s alpha = 0.87 for the current study sample. Measurement modeling analysis indicated a good fit of the data to a one-factor model (GFI = 0.98, RMSEA = 0.06, and CFI = 0.99, χ2/df = 1.88). A mean score was computed and used in descriptive and bivariate analysis.
2.2.4 Socio-Demographic Variables
In addition to social capital investment, social capital and perceived stress, other variables included in the analysis were chronological age (in years), gender (male and female), residential status (rural residents, urban residents, rural-to-urban migrants), educational attainment (primary school or less, middle school, high school, college or more), and marital status (single, married and other). In addition to describing the study sample, these variables were included as covariates in modeling analysis.
2.3 Data Processing and Statistical Analysis
Descriptive statistics (e.g., mean, standard deviation, and proportion) were used to summarize the characteristics of the study sample. Following the protocol for structural equation modeling (SEM) analysis (Hays et al. 2005; Yanuar et al. 2010), correlational analysis (including Cronbach alpha coefficients), exploratory factor analyses (EFA) and confirmatory factor analyses (CFA) were used to assess the psychometric characteristics of the three primary measurement instruments: SCII, PSCS-16 and PSS. Pearson product-moment correlation coefficients were then computed to provide preliminary data supporting the hypothesized structural relationships among SCII, PSCS and PSS. Finally, structural equation modeling was used to examine the hypothesized direct and indirect relationships between social capital investment and perceived stress, through social capital (Kline 2011).
SEM and CFA were conducted using the procedure PROC CALIS. Four commonly used goodness of fit indices were examined to assess data-model fit: Goodness-of-fit index (GFI, >0.9); comparative fit index (CFI, >0.90); the residual mean square of error approximation (RMSEA, <0.05); and the ratio of Chi square to degree of freedom (χ2/df < 2.0) (Bentler 1990; Browne and Cudeck 1992). In conducting the correlational analysis to compute the Cronbach alpha, the method of pairwise deletion was used for subjects with missing data. All statistical analyses were conducted using the software SAS version 9.23 (SAS Institute, Cary, NC).
3 Results
3.1 Characteristics of the Study Sample
The characteristics of the study sample are summarized in Table 1. Among the total 387 participants (mean age = 30.20, SD = 8.54), 124 were from urban areas, 129 were from rural areas, and 134 were rural-to-urban migrants; 18 with primary or less education and 104 with college or higher education. There were significantly more females than males (235 vs. 152, p < 0.01). Since this was an in-home survey, there were more females available at the time than males. The mean score (SD) for total social capital and perceived stress were 2.90 (0.59) and 2.66 (0.52) respectively.
Table 1.
Characteristics of the study sample
| Variable | Male [n (%)] | Female [n (%)] | Total [n (%)] |
|---|---|---|---|
| Sample size N | 152 (39.28 %) | 235 (60.72 %) | 387 (100 %) |
| Residential status | |||
| Urban residents | 50 (32.89 %) | 74 (31.49 %) | 124 (32.04 %) |
| Rural residents | 49 (32.24 %) | 80 (34.04 %) | 129 (33.33 %) |
| Rural-to-urban migrants | 53 (34.87 %) | 81 (34.47 %) | 134 (34.63 %) |
| Age in years | |||
| Mean (SD) | 29.75 (8.17) | 30.48 (8.77) | 30.20 (8.54) |
| Marital status [n (%)] | |||
| Single | 73 (48.03 %) | 90 (38.30 %) | 163 (42.12 %) |
| Married | 77 (50.66 %) | 144 (61.28 %) | 221 (57.11 %) |
| Others | 2 (1.32 %) | 1 (0.43 %) | 3 (0.78 %) |
| Educational attainment [n (%)] | |||
| Primary school or less | 6 (3.95 %) | 12 (5.11 %) | 18 (4.65 %) |
| Middle school | 48 (31.58 %) | 80 (34.04 %) | 128 (33.07 %) |
| High school | 54 (35.53 %) | 83 (35.32 %) | 137 (35.40 %) |
| College or more | 44 (28.95 %) | 60 (25.53 %) | 104 (26.87 %) |
| Social capital [mean (SD)] | |||
| Total PSCS score | 2.76 (0.57) | 2.68 (0.59) | 2.90 (0.59) |
| Bonding capital | 3.13 (0.55) | 3.06 (0.59) | 3.10 (0.57) |
| Bridging capital | 2.39 (0.75) | 2.27 (0.72) | 2.33 (0.74) |
| Levels of perceived stress | |||
| Mean (SD) | 2.63 (0.53) | 2.67 (0.52) | 2.66 (0.52) |
Table 2 lists the seven SCII items, their means scores (SD), correlations with total scale scores and potential improvements in Cronbach’s alpha with removal of an item. The mean scores of the seven items varied in a narrow range around 3. The Cronbach’s alpha = 0.81 for the scale, and this alpha could not be further improved by removing any item(s).
3.2 Correlations Among Social Capital Investment, Social Capital, Perceived Stress and Demographic Factors
Table 3 includes the correlations between social capital investment, levels of social capital (including bonding and bridging), perceived stress and the four demographic factors included as covariates. The results indicate that investment in social capital was significantly positively associated with bonding social capital (r = 0.29, p < 0.01), bridging capital (r = 0.31, p < 0.01), and total social capital (r = 0.35, p < 0.01); while total social capital (r = −0.17, p < 0.01), bonding capital (r = −0.16, p < 0.01) and bridging capital (r = −0.15, p < 0.01) were significantly negatively associated with perceived stress scores. The correlation between social capital investment and perceived stress was nonsignificant, but given the other correlations, an indirect relationship between social capital investment and perceived stress through accumulation of social capital was considered likely.
Table 3.
Correlation coefficients of manifest bonding variables and bridging variables
| Variable | Age | Gender | Education | Marital status | Social capital investment | Total social capital | Bonding social capital | Bridging social capital | Perceived stress |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | 0.04 | −0.26** | 0.65** | −0.18** | 0.09 | 0.10* | 0.05 | −0.04 |
| 2. Gender (male = 1) | – | −0.05 | 0.09 | −0.02 | −0.07 | −0.08 | −0.04 | 0.04 | |
| 3. Education | – | −0.24** | 0.25** | −0.01 | −0.05 | 0.01 | 0.12* | ||
| 4. Marital status | – | −0.08 | 0.14** | 0.17** | 0.09 | −0.02 | |||
| 5. Social capital investment | – | 0.35** | 0.29** | 0.31** | 0.07 | ||||
| 6. Total social capital | – | 0.84** | 0.91** | −0.17** | |||||
| 7. Bonding social capital | – | 0.54** | −0.16** | ||||||
| 8. Bridging social capital | – | −0.15** | |||||||
| 9. Perceived stress | – |
p <0.05;
p < 0.01.
Residential status (rural resident, urban resident and migrant) was not included because a correlation coefficient cannot be calculated for this variable
3.3 Structural Relationship Among Social Capital Investment, Social Capital, Perceived Stress
Figure 1 presents the results from the SEM analysis that tested the structural relationship among the three key variables, while controlling for age, gender, educational attainment, residential status, and marital status. First of all, the data satisfactorily fit the constructed model (GFI = 0.90, CFI = 0.93, RMSEA = 0.05, χ2/df = 1.92). Social capital investment scores were positively associated with the bonding (standard coefficient = 0.45, p < 0.01) and the bridging (standard coefficient = 0.35, p < 0.01) capital; the bonding capital was in turn negatively associated with the perceived stress (standard coefficient = −0.33, p < 0.05). The association between the bridging social capital and perceived stress was not significantly different from zero (standard coefficient = 0.02, p > 0.05).
4 Discussion
Since the pioneer work by Durkheim on social capital and suicide in 1889–91 (Cohen and McKay 1984), much progress has been made in understanding the role of and the mechanisms through which social capital can directly and indirectly affect health and well-being. In this study, we reported the SCII, a validated tool to measure social capital investment; we then examined the relationship between social capital investment, social capital, and perceived stress. The study was conducted using data from a random adult sample of 387 participants with diverse geographic (Beijing and Wuhan), residential (rural, urban and rural-to-urban migrants) and demographic backgrounds.
Based on theoretical support from the economics and finance literatures, we developed the SCII and provided detailed psychometric assessment of the instrument. Exploratory and confirmatory factor analyses confirmed a single factor structure and the scale demonstrated high internal consistency. With this new instrument and data, we found a structural association from social capital investment to social capital (including bonding and bridging capital), also demonstrating the concurrent predictive validity of the scale.
4.1 Social Capital Investment
Results indicated social capital investment was greater among younger individuals and individuals with higher educational attainment. Gender and marital status were unrelated to social capital investment. Consistent with theories and models in economics and finance (Case et al. 2012; Thaler 2005), more social capital investment was associated with greater social capital, including the total, bonding and bridging capital. This relationship was revealed through correlation analysis and further verified through SEM analysis, after controlling for covariates. In addition to documenting the relationship between social capital investment and levels of social capital, the positive association between the two provides empirical evidence supporting the validity of the SCII we developed for future use.
4.2 Direct Effects of Social Capital Investment on Perceived Stress
Social capital investment was not directly related to perceived stress at the bivariate level, as well as in the structural equation model. Further research is needed to better understand this relationship and if social capital investment has positive effects on other health outcomes. It could be that for some individuals the time and effort put into forming social bonds with others is stressful because it requires considerable resources that they might not have, or because they feel like their investments are not being reciprocated (Coleman 1988). For others, their social investments might be incredibly fulfilling, and therefore, they experience reduced stress.
4.3 Indirect Effect of Social Capital Investment on Perceived Stress
Findings of this study indicate that the influence of social capital investment on perceived stress is indirect through social capital, particularly bonding capital. Stress can lead to poor coping strategies that involve risky health behaviors, such as increased smoking, consuming a higher fat diet and reduced exercise (De Silva et al. 2005), which negatively impact health. Stress also impacts individual health through its activation of the sympathetic nervous system and hypothalamic-pituitary adrenal cortical axis (Durkheim 1951). Thus understanding the specific links between social capital investment, social capital and perceived stress are important for understanding any downstream effects on health behaviors. A number of mechanisms and models are proposed to explain the relationship between social capital and health, including personal empowerment to access scarce resources in the wider community and the creation of a harmonic social and cultural environment (Berkman et al. 2000; Chen et al. 2009a, 2011; Poortinga 2012; Putnam 2001; Lin 2002; Veenstra et al. 2005). Our study is the first to bring social capital investment into this line of research.
4.4 Social Capital and Perceived Stress
Findings from published research have documented the protective role of social capital on health at the micro, meso and macro levels (Mohnen et al. 2013; Kaljee and Chen 2011; Verhaeghe et al. 2012; Verhaeghe and Tampubolon 2012). In the current study, bridging capital was related to significantly less perceived stress at the bivariate level, but not significantly related to perceived stress in the structural equation model. Given the strong relationship between bonding and bridging capital, it is likely that once bonding capital was accounted for in the model, the effect of bridging capital on perceived stress was attenuated. Bridging capital has been referred to as ‘weak ties’ that link individuals through organizations (Putnam 2001). Thus, these relationships are acknowledged as playing a less central role in building social capital, compared to bonding capital.
4.5 Implications for Health Promotion and Disease Prevention
Enhancement of social capital represents an emerging area in social capital and health research (Onyx and Leonard 2010; Ottesen et al. 2010; Shan et al. 2012; Harris et al. 2013). Intervention studies report positive effects of enhancing social capital through organized activities (Michael et al. 2008; Ottesen et al. 2010). The findings of this study support the reported interventions to enhance social capital. Our study findings further imply that social capital can be enhanced by promoting many interpersonal activities on a daily basis as reflected by the SCII. Since these social capital investment behaviors are often culturally inherited and socially desirable, encouraging cross-cultural and cross-racial exchange through social programs and policies may also help enhance social capital investment.
Intervention programs promoting group activities, both in young children and older adults, have demonstrated positive effects on social capital and individual health. For example, in a study from Ottesen et al. (2010), women who took part in a 16 week physical activity intervention (learned how to play football or joined a running group), frequently reported sharing their personal stories in order to create similarities and forms bonds with other members of the intervention. The new relationships that were formed were related to increased enjoyment and commitment to the physical activity. The SCII we reported in this study will add a new tool for further research to devise new intervention programs to enhance social capital for health promotion, disease prevention, and treatment recovery.
Modernization and urbanization in the past resulted in social capital collapse (Putnam 2001; Ferlander 2007; Halpern 2005). In the new information era, new technologies, such as social media, provide new methods through which people make connections and invest in their social capital (Ellison et al. 2011; Steinfield et al. 2008). However, not all online interactions produce the same levels or the same types of social capital. Burke et al. (2010) found that engaging in directed communication with ‘actual friends’ on Facebook is related to increased bonding social capital, but having a large friend count on Facebook is related more strongly to bridging social capital. As well, face-to-face interactions are still the strongest predictor of individual perceptions that one has someone they can rely on for tangible assistance, as well as social support (Vitak et al. 2011). Although online interactions appear to account for additional variation in perceptions of support from others, above and beyond that accounted for by face-to-face interaction (Vitak et al. 2011).
Whether the adaptation of these modern communication technologies will result in another social capital collapse is an unanswered question. The SCII developed in this study provides a reliable and valid measurement tool for researchers to quantitatively investigate the role of these technologies in social capital construction.
4.6 Suggested Future Research
Social capital investment can be considered as a culturally and socially based daily, as well as lifelong, interpersonal strategy. Some people may actively invest in a relationship for a long time and rarely need assistance in return; others may frequently receive assistance from others but invest little or do not come to the point to invest. Different from economics and financing, short-term returns on investment in social relationships are less predictable. When in a time of need, social network members or support providers may provide less assistance than one needs, provide the wrong type or level of assistance or at the wrong time, or may not be able to provide assistance at all (Bourdieu 1986; Harpham et al. 2006; House et al. 1985). However, over the long-term, reciprocity of investment is the norm. Long-term returns from social capital investment are therefore predictable and sometimes such returns are priceless. As we pointed our earlier in this paper, it is difficult to place a value on securing a dream job, finding a lifetime lover, or saving a life with the assistance of a friend.
Future research is however needed to broaden our understanding of the nuances in social capital investment returns. Barrowing the concept from anthropology, returns from social capital investment could be categorized into generalized, balanced and negative (House et al. 1988; Hyyppä and Mäki 2001). Generalized returns are returns from putatively altruistic or culturally mandated actions. Balanced returns are a direct exchange, or the anticipation of a specific return, within a given time frame. Negative returns are an attempt to “get something for nothing”. Social relationships with negative returns might be especially stressful, as one person is always giving, and the other is always taking. Future research is needed to understand how returns on investments contribute to perceived levels of stress.
4.7 Limitations
There are several limitations to this study. First, data used for this analysis are cross-sectional in nature. Therefore, we cannot draw any causal conclusions about the strengths and direction of the relationships in the structural equation model. Future research is needed that utilizes longitudinal data in order to draw such causal conclusions. In the Introduction, we discussed the similarities and differences between social capital investment and investment in economics and finance. Additional theoretical and empirical support for the characteristics of social capital investment is needed. Research is also needed that examines how social capital investment behaviors could be used in health promotion interventions. Finally, data collected for this study represents the conditions in China where collectivism is the traditional culture. Caution is needed when generalizing the findings of this study to other cultures with different value systems.
Despite these limitations, this is the first study to document social capital investment and its role with social capital and mental health status. Data used for the study is derived from a diverse sample. The study provides an efficient and simple new tool to assess social capital investment at the individual level. The findings from the study also provide new information on social capital and health with important implications for health promotion, disease prevention and treatment interventions through enhancement of personal investment in social capital.
Acknowledgments
This research was supported by research funding from the National Institute of Health through a research Grant (R01 MH200396). We thank research staff at Wuhan Centers for Disease Prevention and Control and the graduate students from Beijing Normal University who devoted their effort to complete data collection in the field and to help clean and process the collected data.
Contributor Information
Xinguang Chen, Email: jimax.chen@phhp.ufl.edu, Wuhan University Global Health Center, Wuhan, China; School of Medicine, Wayne State University, Detroit, MI, USA; Wuhan Centers for Disease Prevention and Control, Wuhan, China; Department of Epidemiology, University of Florida, Gainesville, FL, USA.
Peigang Wang, Email: pwang@med.wayne.edu, Wuhan University Global Health Center, Wuhan, China; School of Medicine, Wayne State University, Detroit, MI, USA.
Rhiana Wegner, Email: rhiana@wayne.edu, School of Medicine, Wayne State University, Detroit, MI, USA; Psychology Department, Wayne State University, Detroit, MI, USA.
Jie Gong, Email: jiegong322@hotmail.com, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Xiaoyi Fang, Email: fangxy@bnu.edu.cn, Beijing Normal University Developmental Institute, Beijing, China.
Linda Kaljee, Email: lkaljee@med.wayne.edu, School of Medicine, Wayne State University, Detroit, MI, USA.
References
- Almadi T, Cathers I, Hamdan Mansour AM, Chow CM. An Arabic version of the Perceived Stress Scale: Translation and validation study. International Journal of Nursing Studies. 2012;49(1):84–89. doi: 10.1016/j.ijnurstu.2011.07.012. [DOI] [PubMed] [Google Scholar]
- Andreou E, Alexopoulos EC, Lionis C, Varvogli L, Gnardellis C, Chrousos GP, et al. Perceived Stress Scale: Reliability and validity study in Greece. International Journal of Environmental Research and Public Health. 2011;8(8):3287–3298. doi: 10.3390/ijerph8083287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archuleta AJ, Miller CR. Validity evidence for the translated version of the personal social capital scale. Journal of the Society for Social Work and Research. 2011;2(2):39–53. [Google Scholar]
- Archuleta AJ, Teasley M. Acculturative stress among people of Mexican descent: The role of acculturation, social capital, and family role expectations. Social Work in Mental Health. 2013;11(4):311–333. [Google Scholar]
- Astone NM, Nathanson CA, Schoen R, Kim YJ. Family demography, social theory, and investment in social capital. Population and Development Review. 1999;25(1):1–31. [Google Scholar]
- Atienza AA, Collins R, King AC. The mediating effects of situational control on social support and mood following a stressor a prospective study of dementia caregivers in their natural environments. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2001;56(3):S129–S139. doi: 10.1093/geronb/56.3.s129. [DOI] [PubMed] [Google Scholar]
- Avey JB, Luthans F, Jensen SM. Psychological capital: A positive resource for combating employee stress and turnover. Human Resource Management. 2009;48(5):677–693. [Google Scholar]
- Bartkowski JP, Xu X. Religiosity and teen drug use reconsidered: A social capital perspective. American Journal of Preventive Medicine. 2007;32(6):S182–S194. doi: 10.1016/j.amepre.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science and Medicine. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bian Y. Source and functions of urbanites social capital: A network approach. Social Sciences in China. 2004;25(3):136–146. [Google Scholar]
- Bolin K, Lindgren B, Lindström M, Nystedt P. Investments in social capital—Implications of social interactions for the production of health. Social Science and Medicine. 2003;56(12):2379–2390. doi: 10.1016/s0277-9536(02)00242-3. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson JG, editor. Handbook of theory and research for the sociology of education. New York: Greenwood; 1986. pp. 241–258. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1992;21(2):230–258. [Google Scholar]
- Burke M, Marlow C, Lento T. Social network activity and social well-being. Paper presented at the Conference on Human Factors in Computing Systems; Atlanta. 2010. [Google Scholar]
- Case KE, Fair RC, Oster SM. Principles of economics. Boston: Pearson Education, Limited; 2012. [Google Scholar]
- Chen X, Stanton B, Gong J, Fang X, Li X. Personal social capital scale: An instrument for health and behavioral research. Health Education Research. 2009a;24(2):306–317. doi: 10.1093/her/cyn020. [DOI] [PubMed] [Google Scholar]
- Chen X, Stanton B, Kaljee LM, Fang X, Xiong Q, Lin D, et al. Social stigma, social capital reconstruction, and rural migrants in urban China: A population health perspective. Human Organization. 2011;70(1):22–32. doi: 10.17730/humo.70.1.k76047734m703500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Stanton B, Li X, Fang X, Lin D, Xiong Q. A comparison of health-risk behaviors of rural migrants with rural residents and urban residents in China. American Journal of Health Behavior. 2009b;33(1):15–25. doi: 10.5993/ajhb.33.1.2. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7(3):269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59(8):676. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen DA, Farley TA, Mason K. Why is poverty unhealthy? Social and physical mediators. Social Science and Medicine. 2003;57(9):1631–1641. doi: 10.1016/s0277-9536(03)00015-7. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cohen S, McKay G. Social support, stress, and the buffering hypothesis: A theoretical analysis. Handbook of Psychology and Health. 1984;4:253–267. [Google Scholar]
- Coleman JS. Social capital in the creation of human capital. American Journal of Sociology. 1988;94:S95–S120. Supplement: Organizations and Institutions: Sociological and Economic Approaches to the Analysis of Social Structure. [Google Scholar]
- De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: A systematic review. Journal of Epidemiology and Community Health. 2005;59(8):619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim E. Suicide. New York: Free Press; 1951. [Google Scholar]
- Ellison NB, Steinfield C, Lampe C. Connection strategies: Social capital implications of Facebook-enabled communication practices. New Media & Society. 2011;13(6):873–892. [Google Scholar]
- Ferlander S. The importance of different forms of social capital for health. Acta Sociologica. 2007;50(2):115–128. [Google Scholar]
- Glaeser EL, Laibson D, Sacerdote B. An economic approach to social capital*. The Economic Journal. 2002;112(483):F437–F458. [Google Scholar]
- Halpern D. Social capital. Cambridge: Polity Press; 2005. [Google Scholar]
- Harpham T, McKenzie K, Wilkinson R. Social capital and mental health. Philadelphia, PA: Jessica Kingsley Publishers; 2006. [Google Scholar]
- Harris FM, Maxwell M, O’Connor RC, Coyne J, Arensman E, Székely A, et al. Developing social capital in implementing a complex intervention: A process evaluation of the early implementation of a suicide prevention intervention in four European countries. BMC Public Health. 2013;13(1):1–12. doi: 10.1186/1471-2458-13-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Revicki D, Coyne KS. Application of structural equation modeling to health outcomes research. Evaluation and the Health Professions. 2005;28(3):295–309. doi: 10.1177/0163278705278277. [DOI] [PubMed] [Google Scholar]
- House JS, Kahn RL, McLeod JD, Williams D. Measures and concepts of social support. In: Cohen S, Syme SL, editors. Social support and health. San Diego, CA: Academic Press; 1985. pp. 83–108. [Google Scholar]
- House JS, Umberson D, Landis KR. Structures and processes of social support. Annual Review of Sociology. 1988;14(1):293–318. [Google Scholar]
- Hyyppä MT, Mäki J. Individual-level relationships between social capital and self-rated health in a bilingual community. Preventive Medicine. 2001;32(2):148–155. doi: 10.1006/pmed.2000.0782. [DOI] [PubMed] [Google Scholar]
- Kaljee LM, Chen X. Social capital and risk and protective behaviors: A global health perspective. Adolescent Health, Medicine and Therapeutics. 2011;2011(2):113–122. doi: 10.2147/AHMT.S26560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennelly B, O’Shea E, Garvey E. Social capital, life expectancy and mortality: A cross-national examination. Social Science and Medicine. 2003;56(12):2367–2377. doi: 10.1016/s0277-9536(02)00241-1. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford Press; 2011. [Google Scholar]
- Lazarus RS, Cohen JB. Environmental stress. In: Altman I, Wohlwill JF, editors. Human behavior and environment. New York, NY: Plenum Press; 1977. pp. 89–127. [Google Scholar]
- Lesage F-X, Berjot S, Deschamps F. Psychometric properties of the French versions of the Perceived Stress Scale. International Journal of Occupational Medicine and Environmental Health. 2012;25(2):178–184. doi: 10.2478/S13382-012-0024-8. [DOI] [PubMed] [Google Scholar]
- Lin N. Building a network theory of social capital. Connections. 1999;22(1):28–51. [Google Scholar]
- Lin N. Social capital: A theory of social structure and action. Vol. 19. Cambridge, MA: Cambridge University Press; 2002. [Google Scholar]
- Lin N, Fu Y-C, Hsung R-M. The position generator: Measurement techniques for investigations of social capital. Paper presented at the Conference on Social Networks and Social Capital, Duke University; October 30–31.2001. [Google Scholar]
- Lochner KA, Kawachi I, Brennan RT, Buka SL. Social capital and neighborhood mortality rates in Chicago. Social Science and Medicine. 2003;56(8):1797–1805. doi: 10.1016/s0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- Michael YL, Farquhar SA, Wiggins N, Green MK. Findings from a community-based participatory prevention research intervention designed to increase social capital in Latino and African American communities. Journal of Immigrant and Minority Health. 2008;10(3):281–289. doi: 10.1007/s10903-007-9078-2. [DOI] [PubMed] [Google Scholar]
- Miller DL, Scheffler R, Lam S, Rosenberg R, Rupp A. Social capital and health in Indonesia. World Development. 2006;34(6):1084–1098. [Google Scholar]
- Mimura C, Griffiths P. A Japanese version of the Perceived Stress Scale: Cross-cultural translation and equivalence assessment. BMC Psychiatry. 2008;8(1):85. doi: 10.1186/1471-244X-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohnen SM, Völker B, Flap H, Subramanian S, Groenewegen PP. You have to be there to enjoy it? Neighbourhood social capital and health. The European Journal of Public Health. 2013;23(1):33–39. doi: 10.1093/eurpub/cks039. [DOI] [PubMed] [Google Scholar]
- Murayama H, Fujiwara Y, Kawachi I. Social capital and health: A review of prospective multilevel studies. Journal of Epidemiology. 2012;22(3):179–187. doi: 10.2188/jea.JE20110128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22(6):638. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Nieminen T, Martelin T, Koskinen S, Aro H, Alanen E, Hyyppä MT. Social capital as a determinant of self-rated health and psychological well-being. International Journal of Public Health. 2010;55(6):531–542. doi: 10.1007/s00038-010-0138-3. [DOI] [PubMed] [Google Scholar]
- Norstrand JA, Xu Q. Social capital and health outcomes among older adults in China: The urban–rural dimension. The Gerontologist. 2012;52(3):325–334. doi: 10.1093/geront/gnr072. [DOI] [PubMed] [Google Scholar]
- O’Connor M, Hawkins MT, Toumbourou JW, Sanson A, Letcher P, Olsson CA. The relationship between social capital and depression during the transition to adulthood. Australian Journal of Psychology. 2011;63(1):26–35. [Google Scholar]
- Onyx J, Leonard R. The conversion of social capital into community development: An intervention in Australia’s outback. International Journal of Urban and Regional Research. 2010;34(2):381–397. doi: 10.1111/j.1468-2427.2009.00897.x. [DOI] [PubMed] [Google Scholar]
- Ottesen L, Jeppesen RS, Krustrup BR. The development of social capital through football and running: Studying an intervention program for inactive women. Scandinavian Journal of Medicine and Science in Sports. 2010;20(s1):118–131. doi: 10.1111/j.1600-0838.2010.01123.x. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Social relations or social capital? Individual and community health effects of bonding social capital. Social Science and Medicine. 2006;63(1):255–270. doi: 10.1016/j.socscimed.2005.11.039. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Community resilience and health: The role of bonding, bridging, and linking aspects of social capital. Health & Place. 2012;18(2):286–295. doi: 10.1016/j.healthplace.2011.09.017. [DOI] [PubMed] [Google Scholar]
- Pronyk PM, Harpham T, Busza J, Phetla G, Morison LA, Hargreaves JR, et al. Can social capital be intentionally generated? A randomized trial from rural South Africa. Social Science and Medicine. 2008;67(10):1559–1570. doi: 10.1016/j.socscimed.2008.07.022. [DOI] [PubMed] [Google Scholar]
- Putnam RD. Bowling alone: The collapse and revival of American community. New York, NY: Simon and Schuster; 2001. [Google Scholar]
- Ramírez MTG, Hernández RL. Factor structure of the Perceived Stress Scale (PSS) in a sample from Mexico. The Spanish Journal of Psychology. 2007;10(1):199–206. doi: 10.1017/s1138741600006466. [DOI] [PubMed] [Google Scholar]
- Reis RS, Hino AAF, Añez CRR. Perceived Stress Scale reliability and validity study in Brazil. Journal of Health Psychology. 2010;15(1):107–114. doi: 10.1177/1359105309346343. [DOI] [PubMed] [Google Scholar]
- Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) The Spanish Journal of Psychology. 2006;9(1):86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- Schwartz C, Meisenhelder JB, Ma Y, Reed G. Altruistic social interest behaviors are associated with better mental health. Psychosomatic Medicine. 2003;65(5):778–785. doi: 10.1097/01.psy.0000079378.39062.d4. [DOI] [PubMed] [Google Scholar]
- Schwartz CE, Sendor RM. Helping others helps oneself: Response shift effects in peer support. Social Science and Medicine. 1999;48(11):1563–1575. doi: 10.1016/s0277-9536(99)00049-0. [DOI] [PubMed] [Google Scholar]
- Shan H, Muhajarine N, Loptson K, Jeffery B. Building social capital as a pathway to success: Community development practices of an early childhood intervention program in Canada. Health Promotion International. 2012 doi: 10.1093/heapro/das063. [DOI] [PubMed] [Google Scholar]
- Steinfield C, Ellison NB, Lampe C. Social capital, self-esteem, and use of online social network sites: A longitudinal analysis. Journal of Applied Developmental Psychology. 2008;29(6):434–445. [Google Scholar]
- Symister P. The influence of social support and problematic support on optimism and depression in chronic illness: A prospective study evaluating self-esteem as a mediator. Health Psychology. 2003;22(2):123–129. doi: 10.1037/0278-6133.22.2.123. [DOI] [PubMed] [Google Scholar]
- Szreter S, Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. International Journal of Epidemiology. 2004;33(4):650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Thaler RH. Advances in behavioral finance. Vol. 2. Princeton: Princeton University Press; 2005. [Google Scholar]
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Umberson D, Montez JK. Social relationships and health A flashpoint for health policy. Journal of Health and Social Behavior. 2010;51(1 suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Gaag M, Webber M. Measurement of individual social capital: Questions, instruments, and measures. In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York, NY: Springer; 2010. pp. 29–50. [Google Scholar]
- Veenstra G, Luginaah I, Wakefield S, Birch S, Eyles J, Elliott S. Who you know, where you live: Social capital, neighbourhood and health. Social Science and Medicine. 2005;60(12):2799–2818. doi: 10.1016/j.socscimed.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Verhaeghe P–P, Pattyn E, Bracke P, Verhaeghe M, Van De Putte B. The association between network social capital and self-rated health: Pouring old wine in new bottles? Health & Place. 2012;18(2):358–365. doi: 10.1016/j.healthplace.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Verhaeghe P–P, Tampubolon G. Individual social capital, neighbourhood deprivation, and self-rated health in England. Social Science and Medicine. 2012;75(2):349–357. doi: 10.1016/j.socscimed.2012.02.057. [DOI] [PubMed] [Google Scholar]
- Villar E, Albertin P. ‘It is who knows you’. The positions of university students regarding intentional investment in social capital. Studies in Higher Education. 2010;35(2):137–154. [Google Scholar]
- Vitak J, Ellison NB, Steinfield C. The ties that bond: Re-examining the relationship between Facebook use and bonding social capital. System Sciences (HICSS), 2011 44th Hawaii International Conference on; IEEE; 2011. pp. 1–10. [Google Scholar]
- Wang P, Chen X, Gong J, Jacques-Tiura AJ. Reliability and validity of the personal social capital scale 16 and personal social capital scale 8: Two short instruments for survey studies. Social Indicators Research. 2013 doi: 10.1007/s11205-013-0540-3. [DOI] [Google Scholar]
- Wang Z, Chen J, Boyd JE, Zhang H, Jia X, Qiu J, et al. Psychometric properties of the Chinese version of the Perceived Stress Scale in policewomen. PLoS ONE. 2011;6(12):e28610. doi: 10.1371/journal.pone.0028610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber M, Huxley P, Harris T. Social capital and the course of depression: Six-month prospective cohort study. Journal of Affective Disorders. 2011;129(1):149–157. doi: 10.1016/j.jad.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Woolcock M, Narayan D. Social capital: Implications for development theory, research, and policy. The World Bank Research Observer. 2000;15(2):225–249. [Google Scholar]
- Yanuar F, Ibrahim K, Jemain AA. On the application of structural equation modeling for the construction of a health index. Environmental Health and Preventive Medicine. 2010;15(5):285–291. doi: 10.1007/s12199-010-0140-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


