Abstract
High concentrations of HDL cholesterol are considered to indicate efficient reverse cholesterol transport and to protect from atherosclerosis. However, HDL has been suggested to be dysfunctional in ESRD. Hence, our main objective was to investigate the effect of HDL cholesterol on outcomes in maintenance hemodialysis patients with diabetes. Moreover, we investigated the associations between the major protein components of HDL (apoA1, apoA2, and apoC3) and end points. We performed an exploratory, post hoc analysis with 1255 participants (677 men and 578 women) of the German Diabetes Dialysis study. The mean age was 66.3 years and the mean body mass index was 28.0 kg/m2. The primary end point was a composite of cardiac death, myocardial infarction, and stroke. The secondary end point included all-cause mortality. The mean duration of follow-up was 3.9 years. A total of 31.3% of the study participants reached the primary end point and 49.1% died from any cause. HDL cholesterol and apoA1 and apoC3 quartiles were not related to end points. However, there was a trend toward an inverse association between apoA2 and all-cause mortality. The hazard ratio for death from any cause in the fourth quartile compared with the first quartile of apoA2 was 0.63 (95% confidence interval, 0.40 to 0.89). The lack of an association between HDL cholesterol and cardiovascular risk may support the concept of dysfunctional HDL in hemodialysis. The possible beneficial effect of apoA2 on survival requires confirmation in future studies.
Keywords: lipids, cardiovascular disease, mortality risk, chronic dialysis
Reverse cholesterol transport is considered to protect from atherosclerosis.1,2 HDLs represent the major vehicle of reverse cholesterol transport.1,2 They primarily consist of phospholipids, cholesterol, and proteins.1,2 The two major protein constituents of HDL are apoA1 and apoA2.1,2 ApoC3 forms another component of HDL.3,4 Whereas apoA1 is regarded as beneficial to cardiovascular health, apoC3 is rather regarded as proatherogenic.3–6 The role of apoA2 has not been sufficiently examined.7,8 Nevertheless, recent data tend to support anti-atherogenic effects.7–9
High concentrations of HDL cholesterol are generally thought to reflect efficient reverse cholesterol transport.2,5 However, HDL composition and function are impaired in CKD.10,11 In addition, dysfunctional HDL has been observed in patients on hemodialysis.12 Hence, high HDL cholesterol does not necessarily indicate efficient reverse cholesterol transport in renal disease.
We conducted an exploratory, post hoc analysis of the German Diabetes Dialysis (4D) study to investigate whether HDL cholesterol predicts mortality and cardiovascular risk in patients on maintenance hemodialysis treatment.13,14 Moreover, we sought to analyze the relationships of the major protein components of HDL, namely apoA1, apoA2, and apoC3, with outcomes.
Results
Patient Characteristics at Baseline
The 1255 (677 men and 578 women) participants of the 4D study had a mean age of 66.3 years and a mean body mass index of 28.0 kg/m2.
Tables 1–4 show the baseline characteristics of the study participants according to the quartiles of HDL cholesterol and apoA1, apoA2, and apoC3. Supplemental Table 1 shows the baseline characteristics of the subgroups with HDL cholesterol levels ≤50 mg/dl and >50 mg/dl within the fourth quartile of HDL cholesterol. Supplemental Table 2 shows the baseline characteristics of the propensity score–matched cohort.
Table 1.
Baseline patient characteristics according to quartiles of HDL cholesterol
| Characteristic | Quartile of HDL Cholesterol | P Value | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Participants (n) | 312 | 308 | 317 | 318 | |
| Range (mg/dl) | 17.3–33.4 | 33.5–39.3 | 39.4–46.9 | 47.0–115.5 | |
| Age (yr) | 65.3 (8.3) | 66.0 (8.6) | 67.2 (8.1) | 66.7 (8.0) | 0.03 |
| Men (%) | 205 (66) | 185 (60) | 156 (49) | 131 (41) | <0.001 |
| Ever smoking, n (%) | 146 (47) | 123 (40) | 120 (38) | 118 (37) | 0.06 |
| Body mass index (kg/m2) | 30.0 (4.7) | 28.2 (5.0) | 27.7 (5.0) | 26.2 (4.3) | <0.001 |
| BP (mmHg) | |||||
| Systolic | 145 (22) | 147 (22) | 144 (21) | 147 (22) | 0.19 |
| Diastolic | 75 (11) | 76 (12) | 76 (11) | 77 (11) | 0.13 |
| Time receiving dialysis (mo) | 8.9 (6.7) | 8.3 (7.2) | 8.1 (7.0) | 7.8 (6.6) | 0.24 |
| History of disease, n (%)a | |||||
| Arrhythmia | 76 (24) | 52 (17) | 49 (15) | 59 (19) | 0.03 |
| MI, CABG, PCI, or CHD | 103 (33) | 94 (31) | 79 (25) | 93 (29) | 0.16 |
| Congestive heart failureb | 132 (42) | 107 (35) | 102 (32) | 103 (32) | 0.03 |
| Stroke or TIA | 57 (18) | 63 (20) | 55 (17) | 49 (15) | 0.42 |
| Peripheral vascular disease | 148 (47) | 147 (48) | 125 (39) | 140 (44) | 0.13 |
| Hemoglobin (g/dl) | 10.8 (1.4) | 11.0 (1.3) | 10.8 (1.3) | 11.0 (1.4) | 0.08 |
| Glycated hemoglobin (%) | 6.84 (1.31) | 6.72 (1.24) | 6.61 (1.27) | 6.72 (1.21) | 0.15 |
| Phosphate (mg/dl) | 5.98 (1.72) | 6.07 (1.56) | 5.97 (1.51) | 6.09 (1.63) | 0.71 |
| Albumin (g/dl) | 3.83 (0.3) | 3.81 (0.26) | 3.80 (0.32) | 3.81 (0.31) | 0.47 |
| Cholesterol (mg/dl) | |||||
| LDL | 119.4 (26.9) | 125.0 (30.2) | 128.3 (30.4) | 129.5 (40.0) | <0.001 |
| HDL | 29.6 (3.0) | 36.1 (1.7) | 43.0 (2.2) | 56.9 (9.6) | <0.001 |
| Apolipoprotein (mg/dl) | |||||
| A1 | 107.9 (14.4) | 118.5 (16.8) | 129.0 (16.1) | 149.5 (23.2) | <0.001 |
| A2 | 24.5 (4.4) | 27.1 (4.5) | 29.1 (4.9) | 32.2 (6.1) | <0.001 |
| C3 | 22.3 (10.6) | 20.8 (10.0) | 19.5 (8.8) | 19.1 (8.1) | <0.001 |
| Triglycerides (mg/dl) | 349.0 (200.7) | 291.6 (170.1) | 236.2 (134.1) | 181.4 (95.6) | <0.001 |
| C-reactive protein (mg/L) | 11.0 (4.3–13.6) | 6.6 (2.8–12.0) | 5.7 (2.5–11.7) | 4.5 (1.9–11.1) | <0.001 |
| NT-pro-BNP (ng/L) | 3585 (1492–9949) | 3117 (1416–6842) | 2698 (1246–8375) | 3953 (1686–11,115) | 0.03 |
Data are presented as the mean (SD) or median (25th percentile to 75th percentile), unless otherwise specified. P values for comparison of groups were derived from an analysis of covariance model (for continuous variables) or logistic regression model (for categorical variables), both adjusted for age and sex. Q, quartile; MI, myocardial infarction; CABG, coronary artery bypass grafting surgery; PCI, percutaneous coronary intervention; CHD, coronary heart disease, documented by coronary angiography; TIA, transitory ischemic attack; NT-pro-BNP, N-terminal pro-brain natriuretic peptide.
Types of disease and intervention are not mutually exclusive.
Predominantly New York Heart Association II.
Table 4.
Baseline patient characteristics according to quartiles of apoC3
| Characteristic | Quartile of Baseline ApoC3 | P Value | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Participants (n) | 321 | 306 | 307 | 317 | |
| Range (mg/dl) | 2–13 | 14–18 | 19–26 | 26–49 | |
| Age (yr) | 67.1 (7.8) | 67.7 (7.9) | 65.9 (8.4) | 64.6 (8.6) | <0.001 |
| Men (%) | 195 (61) | 169 (55) | 154 (50) | 159 (50) | 0.02 |
| Ever smoking, n (%) | 130 (41) | 132 (43) | 112 (36) | 133 (41) | 0.38 |
| Body mass index (kg/m2) | 26.4 (4.5) | 26.6 (4.3) | 28.2 (4.7) | 29.0 (5.1) | <0.001 |
| BP (mmHg) | |||||
| Systolic | 146 (23) | 146 (21) | 147 (22) | 143 (22) | 0.25 |
| Diastolic | 76 (11) | 75 (10) | 76 (11) | 75 (12) | 0.14 |
| Time receiving dialysis (mo) | 7.7 (7.1) | 7.8 (6.2) | 9.1 (7.2) | 8.6 (6.8) | 0.03 |
| History of disease, n (%)a | |||||
| Arrhythmia | 68 (21) | 63 (21) | 53 (17) | 52 (16) | 0.29 |
| MI, CABG, PCI, or CHD | 98 (31) | 82 (27) | 91 (30) | 98 (31) | 0.71 |
| Congestive heart failureb | 123 (38) | 114 (37) | 99 (32) | 108 (34) | 0.33 |
| Stroke or TIA | 45 (14) | 68 (22) | 54 (16) | 57 (18) | 0.07 |
| Peripheral vascular disease | 146 (45) | 145 (47) | 139 (45) | 130 (41) | 0.35 |
| Hemoglobin (g/dl) | 10.8 (1.3) | 11.0 (1.4) | 11.0 (1.4) | 10.8 (1.3) | 0.12 |
| Glycated hemoglobin (%) | 6.6 (1.2) | 6.5 (1.2) | 6.8 (1.1) | 7.0 (1.4) | <0.001 |
| Phosphate (mg/dl) | 5.75 (1.51) | 6.04 (1.53) | 6.19 (1.74) | 6.15 (1.63) | 0.002 |
| Albumin (g/dl) | 3.76 (0.32) | 3.83 (0.27) | 3.84 (0.30) | 3.85 (0.31) | 0.002 |
| Cholesterol (mg/dl) | |||||
| LDL | 114 (26) | 126 (28) | 133 (29) | 130 (33) | <0.001 |
| HDL | 38 (13) | 39 (12) | 36 (14) | 32 (133) | <0.001 |
| Apolipoprotein (mg/dl) | |||||
| A1 | 120.5 (23.1) | 127.7 (21.6) | 127.6 (23.1) | 129.6 (25.7) | <0.001 |
| A2 | 26.1 (5.5) | 28.8 (5.2) | 28.9 (5.5) | 29.3 (6.2) | <0.001 |
| C3 | 10.1 (2.3) | 15.9 (1.4) | 21.9 (2.2) | 33.9 (5.6) | <0.001 |
| Triglycerides (mg/dl) | 146.0 (61.0) | 201.7 (77.7) | 265.2 (102.1) | 440.1 (202.1) | <0.001 |
| C-reactive protein (mg/l) | 6.8 (2.7–11.8) | 5.0 (2.4–11.1) | 7.1 (3.0–11.1) | 7.4 (2.9–11.9) | 0.02 |
| NT-pro-BNP (ng/l) | 5325 (1974–138,794) | 3187 (1451–9503) | 2659 (1171–7670) | 2629 (1289–5207) | <0.001 |
Data are presented as the mean (SD) or median (25th percentile to 75th percentile), unless otherwise specified. P values for comparison of groups were derived from an analysis of covariance model (for continuous variables) or logistic regression model (for categorical variables), both adjusted for age and sex. Q, quartile; MI, myocardial infarction; CABG, coronary artery bypass grafting surgery; PCI, percutaneous coronary intervention; CHD, coronary heart disease, documented by coronary angiography; TIA, transitory ischemic attack; NT-pro-BNP, N-terminal pro-brain natriuretic peptide.
Types of disease and intervention are not mutually exclusive.
Predominantly New York Heart Association II.
In the entire cohort, the HDL cholesterol quartiles were inversely related to the proportion of men, to body mass index, triglycerides, apoC3, and C-reactive protein and they were positively related to LDL cholesterol and apoA1 and apoA2 (Table 1). The apoA1 quartiles were inversely related to the proportion of men, triglycerides, and C-reactive protein and they were positively associated with albumin, LDL cholesterol, and apopliproteins (Table 2). The apoA2 quartiles were inversely related to C-reactive protein, N-terminal pro-brain natriuretic peptide, congestive heart failure, and arrhythmia and they were positively associated with hemoglobin, albumin, and LDL cholesterol (Table 3). The apoC3 quartiles were inversely related to age and N-terminal pro-brain natriuretic peptide and they were positively associated with body mass index, glycated hemoglobin, LDL cholesterol, and triglycerides (Table 4).
Table 2.
Baseline patient characteristics according to quartiles of apoA1
| Characteristic | Quartile of ApoA1 at Baseline | P Value | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Participants (n) | 312 | 311 | 301 | 327 | |
| Range (mg/dl) | 74–109 | 110–123 | 124–139 | 140–271 | |
| Age (yr) | 65.6 (8.6) | 66.3 (7.9) | 67.1 (7.7) | 66.2 (8.6) | 0.13 |
| Men (%) | 208 (67) | 188 (60) | 147 (48) | 134 (41) | <0.001 |
| Ever smoking, n (%) | 145 (46) | 130 (42) | 115 (38) | 117 (36) | 0.03 |
| Body mass index (kg/m2) | 27.5 (4.9) | 27.7 (4.7) | 27.6 (4.6) | 27.3 (5.1) | 0.66 |
| BP (mmHg) | |||||
| Systolic | 146 (22) | 145 (23) | 146 (22) | 145 (21) | 0.80 |
| Diastolic | 75 (10) | 76 (11) | 77 (11) | 76 (11) | 0.31 |
| Time receiving dialysis (mo) | 8.5 (7.1) | 8.2 (6.5) | 8.4 (7.2) | 8.1 (6.8) | 0.88 |
| History of disease, n (%)a | |||||
| Arrhythmia | 73 (23) | 63 (20) | 45 (15) | 55 (17) | 0.03 |
| MI, CABG, PCI, or CHD | 110 (35) | 88 (28) | 81 (27) | 90 (28) | 0.07 |
| Congestive heart failureb | 126 (40) | 120 (39) | 104 (34) | 94 (29) | 0.01 |
| Stroke or TIA | 61 (20) | 48 (15) | 59 (19) | 56 (17) | 0.49 |
| Peripheral vascular disease | 156 (50) | 140 (45) | 136 (45) | 128 (39) | 0.05 |
| Hemoglobin (g/dl) | 10.8 (1.5) | 10.9 (1.3) | 10.9 (1.3) | 11.0 (1.4) | 0.13 |
| Glycated hemoglobin (%) | 6.8 (1.3) | 6.7 (1.2) | 6.6 (1.2) | 6.9 (1.3) | 0.06 |
| Phosphate (mg/dl) | 5.98 (1.70) | 5.96 (1.60) | 6.02 (1.53) | 6.16 (1.60) | 0.37 |
| Albumin (g/dl) | 3.76 (0.29) | 3.81 (0.31) | 3.86 (0.30) | 3.84 (0.29) | <0.001 |
| Cholesterol (mg/dl) | |||||
| LDL | 117 (26) | 124 (26) | 129 (30) | 132 (31) | <0.001 |
| HDL | 26 (6) | 32 (7) | 38 (9) | 49 (15) | <0.001 |
| Apolipoprotein (mg/dl) | |||||
| A1 | 99.8 (6.8) | 116.5 (4.0) | 130.6 (4.8) | 157.1 (18.4) | <0.001 |
| A2 | 23.3 (3.6) | 26.7 (3.5) | 29.4 (4.1) | 33.4 (5.8) | <0.001 |
| C3 | 18.6 (9.7) | 20.3 (9.4) | 20.9 (9.2) | 21.8 (9.5) | <0.001 |
| Triglycerides (mg/dl) | 292 (190) | 268 (155) | 263 (159) | 235 (158) | <0.001 |
| C-reactive protein (mg/L) | 10.0 (3.7–15.8) | 6.8 (3.1–11.2) | 6.1 (2.6–11.1) | 4.6 (1.9–11.1) | <0.001 |
| NT-pro-BNP (ng/L) | 4051 (1641–11,625) | 2926 (1460–8322) | 3076 (1351–7553) | 2975 (1288–8040) | 0.02 |
Data are presented as the mean (SD) or median (25th percentile to 75th percentile), unless otherwise specified. P values for comparison of groups were derived from an analysis of covariance model (for continuous variables) or logistic regression model (for categorical variables), both adjusted for age and sex. Q, quartile; MI, myocardial infarction; CABG, coronary artery bypass grafting surgery; PCI, percutaneous coronary intervention; CHD, coronary heart disease, documented by coronary angiography; TIA, transitory ischemic attack; NT-pro-BNP, N-terminal pro-brain natriuretic peptide.
Types of disease and intervention are not mutually exclusive.
Predominantly New York Heart Association II.
Table 3.
Baseline patient characteristics according to quartiles of apoA2
| Characteristic | Quartile of ApoA2 at Baseline | P Value | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Participants (n) | 232 | 314 | 338 | 367 | |
| Range (mg/dl) | 12–23 | 24–26 | 28–30 | 31–54 | |
| Age (yr) | 66.3 (7.8) | 66.7 (8.4) | 66.4 (8.0) | 65.9 (8.6) | 0.58 |
| Men (%) | 133 (57) | 176 (56) | 172 (51) | 193 (53) | 0.37 |
| Ever smoking, n (%) | 98 (42) | 131 (42) | 135 (40) | 140 (38) | 0.72 |
| Body mass index (kg/m2) | 27.4 (4.7) | 27.7 (4.8) | 27.6 (5.0) | 27.4 (4.6) | 0.74 |
| BP (mmHg) | |||||
| Systolic | 144 (23) | 147 (22) | 145 (21) | 146 (22) | 0.51 |
| Diastolic | 75 (11) | 75 (11) | 77 (11) | 76 (11) | 0.17 |
| Time receiving dialysis (mo) | 8.4 (7.1) | 8.3 (6.5) | 8.7 (7.6) | 7.8 (6.4) | 0.47 |
| History of disease, n (%)a | |||||
| Arrhythmia | 64 (28) | 66 (21) | 48 (14) | 57 (16) | <0.001 |
| MI, CABG, PCI, or CHD | 80 (34) | 99 (31) | 90 (27) | 100 (27) | 0.13 |
| Congestive heart failureb | 113 (49) | 125 (40) | 102 (30) | 102 (28) | <0.001 |
| Stroke or TIA | 42 (18) | 62 (20) | 53 (16) | 67 (18) | 0.59 |
| Peripheral vascular disease | 121 (52) | 151 (48) | 146 (43) | 141 (38) | 0.01 |
| Hemoglobin (g/dl) | 10.6 (1.4) | 10.9 (1.4) | 11.0 (1.3) | 11.1 (1.3) | <0.001 |
| Glycated hemoglobin (%) | 6.8 (1.2) | 6.8 (1.3) | 6.7 (1.2) | 6.7 (1.2) | 0.77 |
| Phosphate (mg/dl) | 6.00 (1.83) | 6.00 (1.57) | 6.09 (1.51) | 6.02 (1.60) | 0.86 |
| Albumin (g/dl) | 3.73 (0.31) | 3.81 (0.30) | 3.83 (0.29) | 3.86 (0.30) | <0.001 |
| Cholesterol (mg/dl) | |||||
| LDL | 117 (29) | 126 (27) | 126 (29) | 130 (32) | <0.001 |
| HDL | 28 (9) | 32 (10) | 37 (12) | 44 (15) | <0.001 |
| Apolipoprotein (mg/dl) | |||||
| A1 | 105.8 (13.6) | 115.9 (15.6) | 127.9 (16.9) | 146.8 (23.4) | <0.001 |
| A2 | 20.8 (2.1) | 25.2 (1.0) | 28.7 (1.0) | 35.2 (4.1) | <0.001 |
| C3 | 17.6 (10.2) | 19.8 (9.3) | 20.8 (9.1) | 22.4 (9.1) | <0.001 |
| Triglycerides (mg/dl) | 291 (209) | 271 (162) | 264 (157) | 241 (147) | 0.004 |
| C-reactive protein (mg/L) | 11.1 (5.8–18.9) | 8.4 (3.5–12.9) | 5.1 (2.1–11.1) | 4.4 (1.9–11.1) | <0.001 |
| NT-pro-BNP (ng/L) | 5713 (2558–13,735) | 3415 (1402–8652) | 2510 (1118–6649) | 2742 (1310–6473) | <0.001 |
Data are presented as the mean (SD) or median (25th percentile to 75th percentile), unless otherwise specified. P values for comparison of groups were derived from an analysis of covariance model (for continuous variables) or logistic regression model (for categorical variables), both adjusted for age and sex. Q, quartile; MI, myocardial infarction; CABG, coronary artery bypass grafting surgery; PCI, percutaneous coronary intervention; CHD, coronary heart disease, documented by coronary angiography; TIA, transitory ischemic attack; NT-pro-BNP, N-terminal pro-brain natriuretic peptide.
Types of disease and intervention are not mutually exclusive.
Predominantly New York Heart Association II.
Effect of Baseline HDL Cholesterol and Apolipoprotein Concentrations on Outcomes
A total of 31.3% of the study participants reached the composite vascular end point and 49.1% died from any cause. The different end points according to HDL cholesterol and apolipoprotein quartiles are shown in Supplemental Tables 3–6. The interaction terms between components of HDL and randomization group were not significant for any end point in pooled analyses. These findings were corroborated by analyses stratified by randomization group (data not shown).
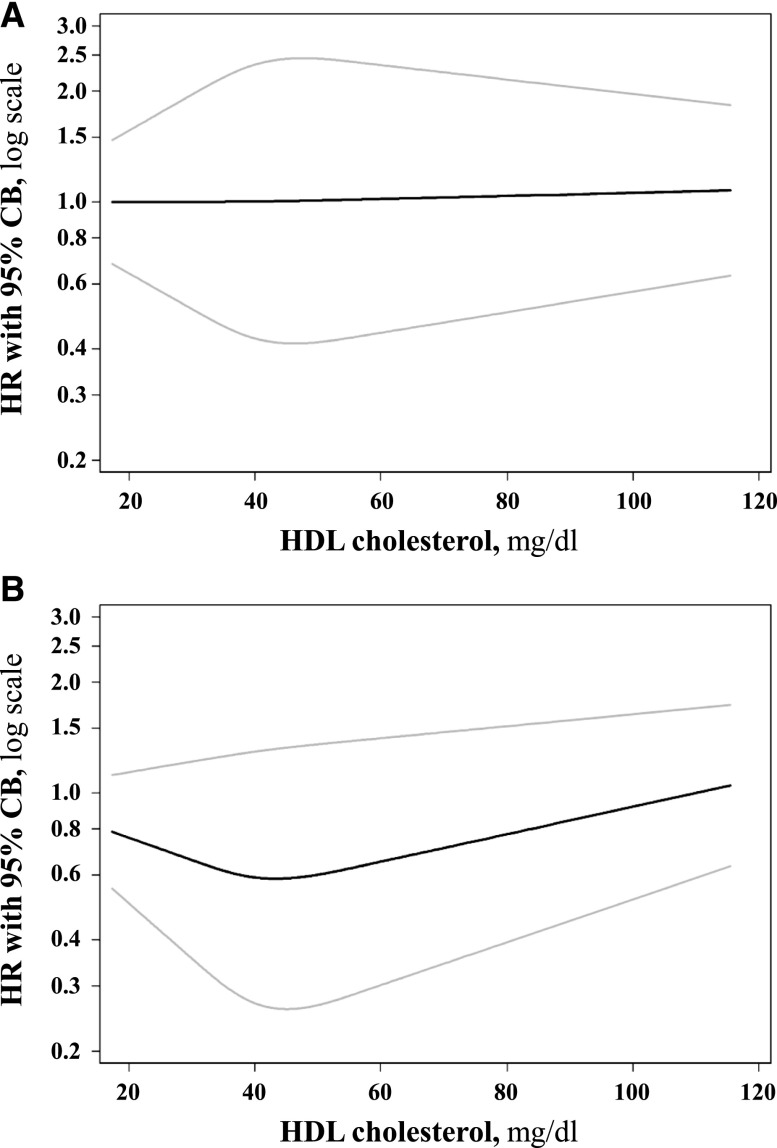
Table 5 shows a summary of the pooled time-to-event analyses. The quartiles of HDL cholesterol were not associated with any end point (Table 5). Further stratification of the fourth quartile in patients with HDL cholesterol ≤50 mg/dl and in those with HDL cholesterol >50 mg/dl did not reveal significant associations (Supplemental Table 7). Adjustment for HDL cholesterol measurements during the follow-up did not change the results (Supplemental Table 8). The cubic spline models corroborated the absence of any significant effect of HDL cholesterol on both cardiovascular risk and all-cause death (Figure 1).
Table 5.
Prognostic value of baseline lipid concentrations on risk of end point occurrence obtained by recurrent events time-to-event analysis
| End point | HDL Cholesterol | ApoA1 | ApoA2 | ApoC3 | ||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI)a | P Valueb | HR (95% CI)a | P Valueb | HR (95% CI)a | P Valueb | HR (95% CI)a | P Valueb | |
| Combined vascular end pointc | ||||||||
| Q2 | 1.02 (0.80 to 1.31) | 0.85 | 1.14 (0.90 to 1.44) | 0.29 | 0.78 (0.61 to 1.00) | 0.05 | 0.94 (0.74 to 1.19) | 0.60 |
| Q3 | 0.96 (0.75 to 1.23) | 0.75 | 0.93 (0.72 to 1.20) | 0.58 | 0.94 (0.74 to 1.20) | 0.61 | 0.98 (0.77 to 1.24) | 0.87 |
| Q4 | 1.06 (0.83 to 1.35) | 0.65 | 0.93 (0.73 to 1.19) | 0.57 | 0.74 (0.58 to 0.96) | 0.02 | 0.93 (0.73 to 1.19) | 0.58 |
| Overalld | 0.88 | 0.33 | 0.05 | 0.93 | ||||
| Cardiac death | ||||||||
| Q2 | 0.99 (0.71 to 1.39) | 0.97 | 1.16 (0.84 to 1.62) | 0.37 | 0.76 (0.54 to 1.07) | 0.12 | 0.95 (0.67 to 1.35) | 0.78 |
| Q3 | 0.82 (0.58 to 1.18) | 0.29 | 0.96 (0.67 to 1.31) | 0.80 | 0.84 (0.59 to 1.18) | 0.31 | 1.21 (0.87 to 1.70) | 0.26 |
| Q4 | 1.03 (0.74 to 1.43) | 0.88 | 0.92 (0.65 to 1.31) | 0.65 | 0.64 (0.45 to 0.93) | 0.02 | 0.85 (0.59 to 1.23) | 0.39 |
| Overall | 0.62 | 0.54 | 0.11 | 0.21 | ||||
| Sudden cardiac death | ||||||||
| Q2 | 0.92 (0.59 to 1.43) | 0.71 | 0.86 (0.55 to 1.34) | 0.50 | 0.60 (0.39 to 0.94) | 0.02 | 0.95 (0.60 to 1.50) | 0.82 |
| Q3 | 0.78 (0.49 to 1.25) | 0.30 | 0.99 (0.63 to 1.55) | 0.98 | 0.69 (0.44 to 1.07) | 0.10 | 1.23 (0.79 to 1.90) | 0.36 |
| Q4 | 1.13 (0.74 to 1.73) | 0.56 | 0.95 (0.61 to 1.47) | 0.82 | 0.61 (0.39 to 0.97) | 0.04 | 0.84 (0.52 to 1.35) | 0.46 |
| Overall | 0.43 | 0.91 | 0.09 | 0.36 | ||||
| Nonfatal MI | ||||||||
| Q2 | 1.16 (0.74 to 1.82) | 0.51 | 1.13 (0.73 to 1.75) | 0.58 | 0.82 (0.51 to 1.32) | 0.42 | 0.92 (0.57 to 1.47) | 0.72 |
| Q3 | 1.17 (0.75 to 1.83) | 0.49 | 1.01 (0.64 to 1.60) | 0.96 | 1.12 (0.71 to 1.76) | 0.64 | 1.01 (0.64 to 1.60) | 0.97 |
| Q4 | 1.11 (0.71 to 1.74) | 0.65 | 0.98 (0.63 to 1.52) | 0.91 | 0.84 (0.53 to 1.35) | 0.48 | 1.25 (0.81 to 1.93) | 0.32 |
| Overall | 0.90 | 0.91 | 0.42 | 0.54 | ||||
| All cardiac events | ||||||||
| Q2 | 1.21 (0.96 to 1.52) | 0.10 | 1.36 (1.09 to 1.71) | 0.01 | 0.83 (0.65 to 1.05) | 0.13 | 0.86 (0.68 to 1.10) | 0.24 |
| Q3 | 1.02 (0.80 to 1.30) | 0.89 | 1.07 (0.84 to 1.37) | 0.59 | 0.94 (0.74 to 1.19) | 0.61 | 1.06 (0.84 to 1.34) | 0.61 |
| Q4 | 1.10 (0.87 to 1.39) | 0.42 | 0.98 (0.77 to 1.25) | 0.88 | 0.73 (0.57 to 0.94) | 0.02 | 0.94 (0.74 to 1.19) | 0.60 |
| Overall | 0.33 | 0.01 | 0.01 | 0.34 | ||||
| All cerebrovascular events | ||||||||
| Q2 | 0.98 (0.63 to 1.52) | 0.91 | 0.96 (0.62 to 1.47) | 0.84 | 0.99 (0.64 to 1.53) | 0.95 | 0.86 (0.57 to 1.29) | 0.46 |
| Q3 | 1.05 (0.68 to 1.62) | 0.82 | 0.79 (0.50 to 1.24) | 0.31 | 0.83 (0.52 to 1.32) | 0.43 | 0.65 (0.42 to 1.07) | 0.05 |
| Q4 | 1.06 (0.69 to 1.62) | 0.80 | 1.01 (0.67 to 1.53) | 0.96 | 0.91 (0.58 to 1.42) | 0.68 | 0.76 (0.49 to 1.17) | 0.22 |
| Overall | 0.98 | 0.68 | 0.84 | 0.27 | ||||
| Death from all causes | ||||||||
| Q2 | 0.93 (0.74 to 1.16) | 0.50 | 0.97 (0.77 to 1.21) | 0.78 | 0.77 (0.62 to 0.96) | 0.02 | 0.84 (0.67 to 1.05) | 0.13 |
| Q3 | 0.79 (0.63 to 0.99) | 0.04 | 0.95 (0.76 to 1.20) | 0.68 | 0.75 (0.59 to 0.94) | 0.01 | 0.93 (0.74 to 1.16) | 0.50 |
| Q4 | 0.94 (0.76 to 1.17) | 0.60 | 0.89(0.71 to 1.20) | 0.32 | 0.63 (0.49 to 0.80) | <0.001 | 0.78 (0.61 to 0.98) | 0.04 |
| Overall | 0.23 | 0.80 | 0.002 | 0.15 | ||||
HR, hazard ratio; 95% CI, 95% confidence interval; Q, quartile; MI, myocardial infarction.
HR calculated with multivariate Andersen–Gill model; group of patients within the first quarter of the distribution used as the reference group; atorvastatin and placebo group pooled; multiple events considered.
P value of the Wald test statistic.
Combined vascular end point consisting of MI, cardiac death, and stroke.
P value of the multivariate Wald test statistic investigating whether there was any difference between any two quartiles.
Figure 1.
No association of HDL cholesterol with end points. Spline fit of the association between HDL cholesterol and the primary end point (A) and all-cause death (B). HR, hazard ratio. CB, confidence band.
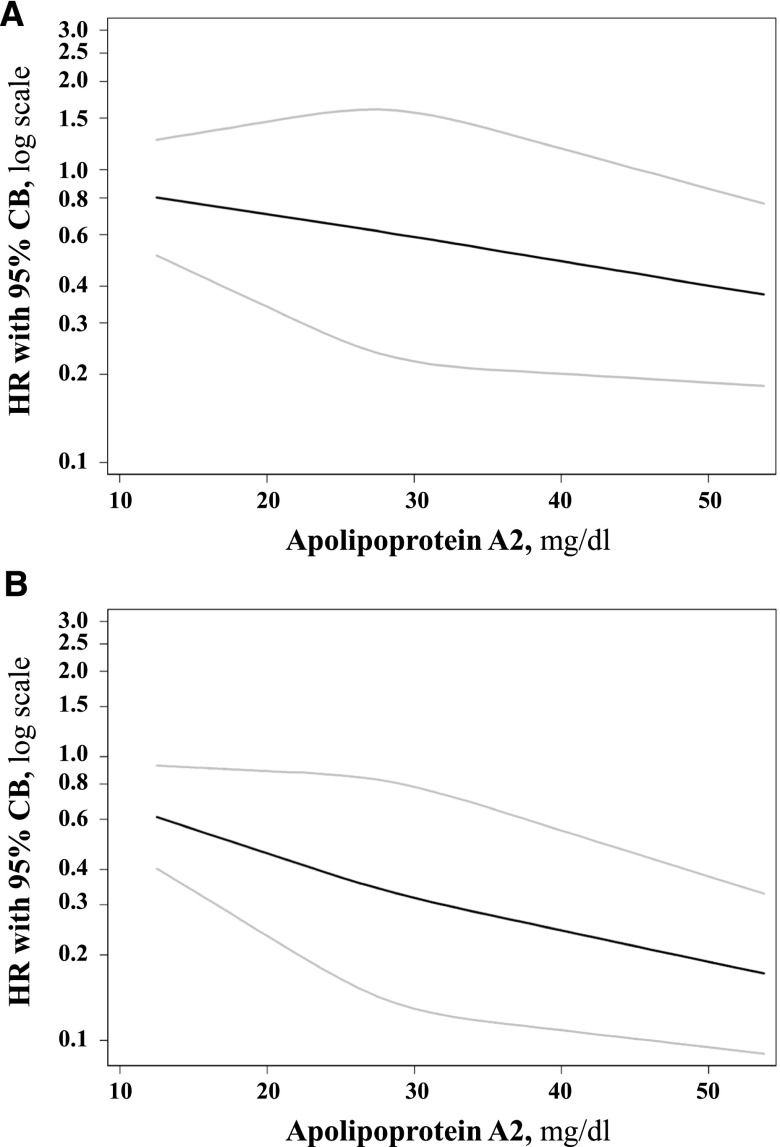
The quartiles of apoA1 and apoC3 were not associated with end points (Table 5). By contrast, the multivariate adjusted analyses conducted in the entire cohort showed that participants in the fourth versus first quartile of apoA2 had decreased the risk of death from any cause (Table 5). The cubic spline model corroborated the inverse association between apoA2 and the risk of death from any cause (P<0.001) (Figure 2). In the propensity score–matched subgroup, the hazard ratios for all-cause mortality comparing the fourth, third, and second with the first apoA2 quartile were similar to those obtained in the entire cohort (see Supplemental Table 9). Because of the lower sample size, the P value comparing the fourth with the first apoA2 quartile did not reach statistical significance after Bonferroni correction in the subgroup analysis. The association of apoA2 with the risk of death from any cause did not reach statistical significance when apoA2 was included in the Cox model as a standardized continuous variable either (hazard ratio, 0.91; 95% confidence interval, 0.82 to 1.01; P=0.09).
Figure 2.
Trend toward inverse relationship of apoA2 with death from any cause. Spline fit of the association between apoA2 and the primary end point (A) and all-cause death (B). HR, hazard ratio; CB, confidence band.
Discussion
The main finding of this study was that the baseline concentrations of HDL cholesterol were not predictive of all-cause mortality and cardiovascular end points. The baseline concentrations of apoA1 and apoC3 were also not associated with outcomes. However, there was a trend toward an inverse association between baseline apoA2 concentrations and death from any cause.
LDL lowering was demonstrated to reduce cardiovascular risk and mortality in the Study of Heart and Renal Protection study and in a post hoc analysis of the 4D study.15,16 Yet lipid lowering does not seem to be as effective in preventing cardiovascular events in hemodialysis patients as in the general population.14,17 However, patients on maintenance hemodialysis treatment carry a very high cardiovascular risk.18 Raising low levels of HDL cholesterol may reduce this risk.19 The aforementioned hypothesis is also based on the consistent relationship between low HDL cholesterol and increased cardiovascular risk in the general population.5,20,21 However, this association did not hold true in these analyses. Few studies have previously investigated the association between HDL cholesterol and apolipoproteins with outcomes in patients with ESRD.22–24 Consistent with our results, HDL cholesterol was not associated with survival in a cohort of 15,859 hemodialysis patients from the DaVita dialysis clinics in the United States.22 Oxidized HDL cholesterol was even demonstrated to positively correlate with future cardiovascular events in 412 hemodialysis patients.23 By contrast, HDL cholesterol was inversely related to prevalent cardiovascular disease in another cohort of 607 hemodialysis patients.24 In summary, the association of HDL cholesterol with outcomes is at least weakened in ESRD. The data may therefore support the idea that HDL become dysfunctional in chronic hemodialysis.25
Surprisingly, high apoA2, unlike apoA1, tended to be associated with a lower risk of death from any cause in the 4D study. This observation may reflect differences in the metabolism of apoA1 and apoA2 in ESRD.26 Moreover, the associations of apoA2 with death from any cause may suggest potentially protective effects of this protein.7–9 In contrast with the lack of an association between apoA1 and end points in our study, a previous study showed that induction of apoA1 may improve HDL functionality in hemodialysis patients.27 Hence, future studies are needed to further elucidate the relationships of apoA1 and apoA2 with cardiovascular end points in ESRD.
This study has several strengths. First, the study participants underwent very detailed clinical and laboratory examinations. Second, there was a precise follow-up for all-cause mortality and various vascular end points. Third, laboratory testing was repeated after 4 weeks and then every 6 months. In contrast with previous studies, this enabled us to control for longitudinal measurements of HDL cholesterol during the follow-up. Fourth, we performed very detailed statistical analyses of the associations of HDL cholesterol and apolipoproteins with outcomes including stratified analyses, cubic spline modeling, and propensity score–matched subgroup analyses for apoA2. Fifth, the sample size of the cohort including >1000 patients on maintenance hemodialysis treatment was very large.
One limitation of these analyses is that they were secondary, exploratory, and thus not predefined. Consequently, the results, especially those for apoA2, require confirmation in future studies. We also do not present data on HDL functionality. However, previous mechanistic studies addressed this issue in detail.10–12 HDL cholesterol levels were not considered for the decision to include or exclude a patient. Nevertheless, implicit confounding conferred by the use of exclusion criteria (e.g., exclusion of several outliers for LDL cholesterol) cannot be totally ruled out.13
In summary, HDL cholesterol does not predict all-cause mortality and vascular complications in patients on maintenance hemodialysis treatment. A possible beneficial effect of apoA2 on survival will require confirmation in future studies.
Concise Methods
Study Design, Setting, and Participants
The design of the 4D study was previously reported in detail.13,14 Briefly, the 4D study is a prospective, randomized, multicenter trial including 1255 patients with type 2 diabetes mellitus who were aged 18–80 years and were on hemodialysis for <2 years. Recruitment started in March 1998 and ended in October 2002. Patients were randomly assigned to receive double-blinded treatment with either 20 mg of atorvastatin (n= 619) or placebo (n=636) once daily. The participants were reexamined at 4 weeks and then every 6 months after randomization until March 2004. At each follow-up visit, a blood sample was taken and information about any suspected end point or serious adverse event was obtained. The study was approved by the local ethics committee and performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants.
Outcome Measures
The 4D study end points were centrally adjudicated by three members of the end point committee blinded to study treatment and according to predefined criteria. The primary end point of the 4D study was defined as a composite of cardiac death, nonfatal myocardial infarction, and stroke, whichever occurred first (combined cardiovascular events). Sudden cardiac death was considered as previously described.13,14 Myocardial infarction was diagnosed when at least two of three criteria were met, including typical symptoms, elevated levels of cardiac enzymes, or diagnostic changes in the electrocardiogram. Stroke was defined as a neurologic deficit lasting longer than 24 hours. Computed tomographic or magnetic resonance imaging results were available in all but 16 patients.
We evaluated the following end points in this analysis: combined primary end point, cardiac death, sudden cardiac death, nonfatal myocardial infarction, all cardiac events combined, all cerebrovascular events, and all-cause death.14
Laboratory Procedures
The standard laboratory procedures have been performed in identical fashion as previously described.13,14 HDL cholesterol was measured with the homogenous assay from Roche Diagnostics (Mannheim, Germany). Lipoproteins were separated by a combined ultracentrifugation-precipitation method (β quantification). Cholesterol was measured with enzymatic reagents from WAKO (Neuss, Germany) on a WAKO R30 or Olympus AU640 analyzer. We measured apoA1, apoA2, and apoC3 by turbidimetry with reagents from Greiner (Flacht, Germany).
Statistical Analyses
Quartiles of HDL (subgroup analyses within the fourth HDL quartile for patients with HDL cholesterol ≤50 mg/dl and >50 mg/dl) cholesterol and apoA1, apoA2, and apoC3 were formed. The baseline characteristics were presented for the quartiles of the aforementioned parameters. Means and SDs or medians with interquartile ranges were presented for continuous variables and frequencies with percentages for categorical variables. P values for differences in the baseline characteristics across the quartiles were calculated with analysis of covariance for continuous variables and logistic regression for categorical variables. All analyses were adjusted for age and sex. An extended Cox regression approach (Andersen–Gill model, which allows adjustment for multiple events) was used to evaluate the prognostic effect of HDL cholesterol (four quartiles and subgroup analysis within the fourth quartile) and apolipoproteins (four quartiles) on cardiovascular events and mortality.28 Hazard ratios (95% confidence intervals) and P values adjusted for all potential confounding variables were calculated across quartiles of HDL cholesterol and apolipoproteins. We conducted a pooled analysis (atorvastatin and placebo groups) assuming a difference in baseline risk and also considering the interaction between the parameter of interest and randomization group. Moreover, possible effect modification by randomization group was explored by analyzing both randomization groups separately (data not shown). Covariates were selected for each end point separately using a stepwise selection procedure (forward, P=0.05; backward, P=0.1) from the following set of variables: sex, age, phosphate, hemoglobin, glycated hemoglobin, ever smoking, systolic and diastolic BP, body mass index, ultrafiltration volume, duration of dialysis, history of stroke/transitory ischemic attack, coronary artery disease (myocardial infarction, coronary artery bypass grafting, coronary intervention, and angiographically documented coronary artery disease), peripheral vascular disease, and congestive heart failure. We also calculated Cox regression models with HDL cholesterol as a time-varying variable. In addition, we calculated multivariate cubic spline models for the associations of HDL cholesterol and apoA2 with the primary end point and all-cause mortality and plotted the spline fits (Figures 1 and 2). We next performed a subgroup analysis in a propensity score–matched cohort. Propensity scores for apoA2 quartiles were calculated based on all potential confounding variables shown in Table 2. Individuals with similar propensity scores were matched by a nearest neighbor-matching algorithm without Caliper implemented in the STATA modul psmatch2. Nonmatched individuals were excluded from the reanalysis. Finally, we calculated a Cox model for the association of apoA2 as a standardized continuous variable with all-cause mortality (hazard ratio refers to the change in hazard per 1-SD increase of apoA2). All statistical tests were two sided. P values were corrected for multiple testing (4 parameters×7 end points=28) according to the Bonferroni correction. Thus, P values <0.002 (0.05/28) were considered significant. All statistical analyses were conducted using the Stata Statistical Software package (release 12; StataCorp., College Station, TX).
Disclosures
W.M. received consulting fees, lecture fees, and research grants from Pfizer. B.G. received grant support from Pfizer for post hoc analyses of the original 4D study. Synlab offers testing for HDL cholesterol and apolipoproteins.
Supplementary Material
Acknowledgments
The 4D study was supported by Pfizer Inc. This work was also supported by the German Federal Ministry of Education and Research (BMBF01 EO1004).
Parts of this article were orally presented in the late-breaking clinical trials session at the 50th European Renal Association–European Dialysis and Transplant Association Congress, held May 18–21, 2013, in Istanbul, Turkey.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013080816/-/DCSupplemental.
References
- 1.Vergeer M, Holleboom AG, Kastelein JJ, Kuivenhoven JA: The HDL hypothesis: Does high-density lipoprotein protect from atherosclerosis? J Lipid Res 51: 2058–2073, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher EA, Feig JE, Hewing B, Hazen SL, Smith JD: High-density lipoprotein function, dysfunction, and reverse cholesterol transport. Arterioscler Thromb Vasc Biol 32: 2813–2820, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen MK, Rimm EB, Furtado JD, Sacks FM: Apolipoprotein C-III as a potential modulator of the association between HDL-cholesterol and incident coronary heart disease. J Am Heart Assoc 1: jah3-e000232, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riwanto M, Rohrer L, Roschitzki B, Besler C, Mocharla P, Mueller M, Perisa D, Heinrich K, Altwegg L, von Eckardstein A, Lüscher TF, Landmesser U: Altered activation of endothelial anti- and proapoptotic pathways by high-density lipoprotein from patients with coronary artery disease: Role of high-density lipoprotein-proteome remodeling. Circulation 127: 891–904, 2013 [DOI] [PubMed] [Google Scholar]
- 5.Di Angelantonio E, Gao P, Pennells L, Kaptoge S, Caslake M, Thompson A, Butterworth AS, Sarwar N, Wormser D, Saleheen D, Ballantyne CM, Psaty BM, Sundström J, Ridker PM, Nagel D, Gillum RF, Ford I, Ducimetiere P, Kiechl S, Koenig W, Dullaart RP, Assmann G, D’Agostino RB, Sr, Dagenais GR, Cooper JA, Kromhout D, Onat A, Tipping RW, Gómez-de-la-Cámara A, Rosengren A, Sutherland SE, Gallacher J, Fowkes FG, Casiglia E, Hofman A, Salomaa V, Barrett-Connor E, Clarke R, Brunner E, Jukema JW, Simons LA, Sandhu M, Wareham NJ, Khaw KT, Kauhanen J, Salonen JT, Howard WJ, Nordestgaard BG, Wood AM, Thompson SG, Boekholdt SM, Sattar N, Packard C, Gudnason V, Danesh J, Emerging Risk Factors Collaboration : Lipid-related markers and cardiovascular disease prediction. JAMA 307: 2499–2506, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Umemoto T, Han CY, Mitra P, Averill MM, Tang C, Goodspeed L, Omer M, Subramanian S, Wang S, Den Hartigh LJ, Wei H, Kim EJ, Kim J, O’Brien KD, Chait A: Apolipoprotein AI and high-density lipoprotein have anti-inflammatory effects on adipocytes via cholesterol transporters: ATP-binding cassette A-1, ATP-binding cassette G-1, and scavenger receptor B-1. Circ Res 112: 1345–1354, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Niimi M, Nishijima K, Waqar AB, Yu Y, Koike T, Kitajima S, Liu E, Inoue T, Kohashi M, Keyamura Y, Yoshikawa T, Zhang J, Ma L, Zha X, Watanabe T, Asada Y, Chen YE, Fan J: Human apolipoprotein A-II protects against diet-induced atherosclerosis in transgenic rabbits. Arterioscler Thromb Vasc Biol 33: 224–231, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winkler K, Hoffmann MM, Seelhorst U, Wellnitz B, Boehm BO, Winkelmann BR, März W, Scharnagl H: Apolipoprotein A-II is a negative risk indicator for cardiovascular and total mortality: Findings from the Ludwigshafen Risk and Cardiovascular Health Study. Clin Chem 54: 1405–1406, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Chan DC, Ng TW, Watts GF: Apolipoprotein A-II: Evaluating its significance in dyslipidaemia, insulin resistance, and atherosclerosis. Ann Med 44: 313–324, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Holzer M, Birner-Gruenberger R, Stojakovic T, El-Gamal D, Binder V, Wadsack C, Heinemann A, Marsche G: Uremia alters HDL composition and function. J Am Soc Nephrol 22: 1631–1641, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Speer T, Rohrer L, Blyszczuk P, Shroff R, Kuschnerus K, Kränkel N, Kania G, Zewinger S, Akhmedov A, Shi Y, Martin T, Perisa D, Winnik S, Müller MF, Sester U, Wernicke G, Jung A, Gutteck U, Eriksson U, Geisel J, Deanfield J, von Eckardstein A, Lüscher TF, Fliser D, Bahlmann FH, Landmesser U: Abnormal high-density lipoprotein induces endothelial dysfunction via activation of Toll-like receptor-2. Immunity 38: 754–768, 2013 [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto S, Yancey PG, Ikizler TA, Jerome WG, Kaseda R, Cox B, Bian A, Shintani A, Fogo AB, Linton MF, Fazio S, Kon V: Dysfunctional high-density lipoprotein in patients on chronic hemodialysis. J Am Coll Cardiol 60: 2372–2379, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wanner C, Krane V, März W, Olschewski M, Asmus HG, Krämer W, Kühn KW, Kütemeyer H, Mann JF, Ruf G, Ritz E, Deutsche Diabetes-Dialyse-Studie (4D) Study Group : Randomized controlled trial on the efficacy and safety of atorvastatin in patients with type 2 diabetes on hemodialysis (4D study): Demographic and baseline characteristics. Kidney Blood Press Res 27: 259–266, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Wanner C, Krane V, März W, Olschewski M, Mann JF, Ruf G, Ritz E, German Diabetes and Dialysis Study Investigators : Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 353: 238–248, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, Wanner C, Krane V, Cass A, Craig J, Neal B, Jiang L, Hooi LS, Levin A, Agodoa L, Gaziano M, Kasiske B, Walker R, Massy ZA, Feldt-Rasmussen B, Krairittichai U, Ophascharoensuk V, Fellström B, Holdaas H, Tesar V, Wiecek A, Grobbee D, de Zeeuw D, Grönhagen-Riska C, Dasgupta T, Lewis D, Herrington W, Mafham M, Majoni W, Wallendszus K, Grimm R, Pedersen T, Tobert J, Armitage J, Baxter A, Bray C, Chen Y, Chen Z, Hill M, Knott C, Parish S, Simpson D, Sleight P, Young A, Collins R, SHARP Investigators : The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet 377: 2181–2192, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.März W, Genser B, Drechsler C, Krane V, Grammer TB, Ritz E, Stojakovic T, Scharnagl H, Winkler K, Holme I, Holdaas H, Wanner C, German Diabetes and Dialysis Study Investigators : Atorvastatin and low-density lipoprotein cholesterol in type 2 diabetes mellitus patients on hemodialysis. Clin J Am Soc Nephrol 6: 1316–1325, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fellström BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, Chae DW, Chevaile A, Cobbe SM, Grönhagen-Riska C, De Lima JJ, Lins R, Mayer G, McMahon AW, Parving HH, Remuzzi G, Samuelsson O, Sonkodi S, Sci D, Süleymanlar G, Tsakiris D, Tesar V, Todorov V, Wiecek A, Wüthrich RP, Gottlow M, Johnsson E, Zannad F, AURORA Study Group : Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med 360: 1395–1407, 2009 [DOI] [PubMed] [Google Scholar]
- 18.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Chapman MJ, Le Goff W, Guerin M, Kontush A: Cholesteryl ester transfer protein: At the heart of the action of lipid-modulating therapy with statins, fibrates, niacin, and cholesteryl ester transfer protein inhibitors. Eur Heart J 31: 149–164, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, Jacobs DR, Jr, Bangdiwala S, Tyroler HA: High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 79: 8–15, 1989 [DOI] [PubMed] [Google Scholar]
- 21.Chapman MJ, Ginsberg HN, Amarenco P, Andreotti F, Borén J, Catapano AL, Descamps OS, Fisher E, Kovanen PT, Kuivenhoven JA, Lesnik P, Masana L, Nordestgaard BG, Ray KK, Reiner Z, Taskinen MR, Tokgözoglu L, Tybjærg-Hansen A, Watts GF, European Atherosclerosis Society Consensus Panel : Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: Evidence and guidance for management. Eur Heart J 32: 1345–1361, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilpatrick RD, McAllister CJ, Kovesdy CP, Derose SF, Kopple JD, Kalantar-Zadeh K: Association between serum lipids and survival in hemodialysis patients and impact of race. J Am Soc Nephrol 18: 293–303, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Honda H, Ueda M, Kojima S, Mashiba S, Michihata T, Takahashi K, Shishido K, Akizawa T: Oxidized high-density lipoprotein as a risk factor for cardiovascular events in prevalent hemodialysis patients. Atherosclerosis 220: 493–501, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Koch M, Kutkuhn B, Trenkwalder E, Bach D, Grabensee B, Dieplinger H, Kronenberg F: Apolipoprotein B, fibrinogen, HDL cholesterol, and apolipoprotein(a) phenotypes predict coronary artery disease in hemodialysis patients. J Am Soc Nephrol 8: 1889–1898, 1997 [DOI] [PubMed] [Google Scholar]
- 25.Zheng C, Aikawa M: High-density lipoproteins: From function to therapy. J Am Coll Cardiol 60: 2380–2383, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Okubo K, Ikewaki K, Sakai S, Tada N, Kawaguchi Y, Mochizuki S: Abnormal HDL apolipoprotein A-I and A-II kinetics in hemodialysis patients: A stable isotope study. J Am Soc Nephrol 15: 1008–1015, 2004 [DOI] [PubMed] [Google Scholar]
- 27.Vaziri ND, Moradi H, Pahl MV, Fogelman AM, Navab M: In vitro stimulation of HDL anti-inflammatory activity and inhibition of LDL pro-inflammatory activity in the plasma of patients with end-stage renal disease by an apoA-1 mimetic peptide. Kidney Int 76: 437–444, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andersen P, Gill R: Cox's regression model for counting processes: A large sample study. Ann Stat 10: 1100–1120, 1982 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.