Abstract
An association between atherosclerosis and osteoporosis has been reported in several studies. This association could result from local intraosseous atherosclerosis and ischemia, which is shown by limb osteoporosis in patients with peripheral artery disease (PAD), but also could result from bidirectional communication between the skeleton and blood vessels. Systemic bone disorders and PAD are frequent in ESRD. Here, we investigated the possible interaction of these disorders. For 65 prevalent nondiabetic patients on hemodialysis, we measured ankle-brachial pressure index (ABix) and evaluated mineral and bone disorders with bone histomorphometry. In prevalent patients on hemodialysis, PAD (ABix<0.9 or >1.4/incompressible) was associated with low bone turnover and pronounced osteoblast resistance to parathyroid hormone (PTH), which is indicated by decreased double-labeled surface and osteoblast surface (P<0.001). Higher osteoblast resistance to PTH in patients with PAD was characterized by weaker correlation coefficients (slopes) between serum PTH and double-labeled surface (P=0.02) or osteoblast surface (P=0.03). The correlations between osteoclast number or eroded surface and serum mineral parameters, including PTH, did not differ for subjects with normal ABix and PAD. Common vascular risk factors (dyslipidemia, smoking, and sex) were similar for normal, low, and incompressible ABix. Patients with PAD were older and had high C-reactive protein levels and longer hemodialysis vintage. These results indicate that, in prevalent nondiabetic patients with ESRD, PAD associates with low bone turnover and pronounced osteoblast resistance to PTH.
Keywords: arteries, arteriosclerosis, end stage kidney disease, hemodialysis, hyperparathyroidism, parathyroid hormone
The bone–vascular axis concept emerged from clinical and experimental findings linking bone and arterial remodeling and changes.1 Observations in diverse populations have revealed associations between atherosclerosis and vascular calcifications with decreased bone mineral density (BMD), risk for vertebral or hip fracture, low bone turnover, and cardiovascular disease.2–8 The biologic link between vascular disease and bone changes is certainly part of the aging process, but in many studies, these bone–vessel associations remained significant after adjustment for age, suggesting an age-independent causal relationship. Nevertheless, the factors or mechanisms underlying these associations are not well understood and could result from common mechanisms acting on both systems (e.g., inflammation, hyperlipidemia, diabetes, smoking,9–12 or generalized arterial disease per se). Blood vessels play a major role in osteogenesis, and factors affecting the blood supply to bones could have major effects on bone remodeling and structure.13–15
Ischemia resulting from intraosseous atherosclerosis and arterial calcifications could explain the association between osteoporosis and decreased BMD. The link between compromised bone circulation and osteoporosis was documented by the observation linking lower limb bone mineral content and abnormal bone turnover with increased risk of fractures in men with ischemic atherosclerotic peripheral artery disease (PAD).16–19
Lower limb PAD is a frequent complication of ESRD, and low ankle-brachial pressure index (ABix) or incompressible arteries are associated with all-cause and cardiovascular mortality.20–23 In general populations, associations between PAD and BMD are observed at the local (lower limb) level and frequently, in the absence of overt mineral metabolism disorders; in patients with CKD and ESRD, those interactions coexist frequently with mineral and bone disorders, including perturbed parathyroid hormone (PTH) and vitamin D metabolisms. In this study, we had the opportunity to analyze the relationships between ABix-assessed subclinical PAD and mineral and bone abnormalities, including systemic bone, on the basis of histomorphometry of iliac crest biopsies. These results indicate that, in prevalent nondiabetic patients with ESRD, PAD was associated with low bone turnover and pronounced osteoblast resistance to PTH.
Results
Patient Characteristics
We studied 65 patients whose clinical characteristics, brachial and lower limb systolic BP (SBP), and ABix are summarized in Table 1. ABix was normal in 30 of 65 (46.2%) patients, ABix was low in 11 (16.9%) patients, and ABix>1.4 or incompressible arteries were present in 24 (36.9%) patients. Patients with abnormal ABix were older. Peripheral artery calcifications were present in all subjects with pathologic ABix and 25.7% of patients whose ABix was normal. Hemodialysis vintage, the proportion of patients with previous parathyroidectomy (PTX), and the calcium phosphate binders prescribed dose were higher in patients with low ABix or incompressible arteries.
Table 1.
Clinical characteristics of patients with ESRD
| Characteristic | ABix | ANOVA P Value | ||
|---|---|---|---|---|
| Normal (n=30) | Low (n=11) | >1.4 (n=24) | ||
| Age (yr) | 44 (29 to 50) | 59a (52 to 65) | 59a (52 to 64) | <0.001 |
| Body mass index (kg/m2) | 22.6 (21.3 to 24.1) | 20.9 (17.1 to 27.9) | 22.5 (20.3 to 23.5) | NS |
| Vintage (mo) | 48 (29 to 65) | 85a (36 to 104) | 144a (96 to 173) | <0.001 |
| Smoking (pack/yr) | 0 (0 to 3) | 0 (0 to 25) | 5.5 (0 to 16) | NS |
| PTX (no.) | 4/30 (13.3%) | 5/11a (45.5%) | 13/24a (54.2%) | 0.004 |
| CaCO3 (g/d) | 1.2 (0.8 to 1.2) | 1.8 (1.4 to 2.4) | 2.4b (2 to 2.4) | <0.001 |
| Brachial SBP (mmHg) | 147 (134 to 164) | 147 (131 to 156) | 156 (138 to 168) | NS |
| Lower limb SBP (mmHg) | 175 (164 to 185) | 126a (104 to 139) | 300a (250 to 300) | <0.001 |
| ABix | 1.14 (1.10 to 1.16) | 0.86a (0.65 to 0.89) | 1.76a (1.52 to 1.9) | <0.001 |
Values are medians (95% confidence intervals). Kruskal–Wallis one-way ANOVA on ranks.
Significantly different from normal ABix.
Significantly different from low ABix and ABix>1.4.
Blood chemistries are reported in Table 2 according to ABix. Patients with PAD had significantly higher serum high-sensitivity C-reactive protein (hCRP) and lower serum albumin. All others biochemical parameters, including PTH, were not significantly different among the three groups.
Table 2.
Blood chemistries of patients with ESRD according to ABix
| Parameter | ABix | ANOVA P Value | ||
|---|---|---|---|---|
| Normal (n=30) | Low (n=11) | >1.4 (n=24) | ||
| Cholesterol (mmol/L) | 5.03 (4.32 to 5.5) | 5.8 (5.06 to 7.75) | 4.97 (4.7 to 6) | NS |
| Triglycerides (mmol/L) | 1.52 (1.37 to 1.87) | 1.7 (1.5 to 2.68) | 1.63 (1.16 to 2.02) | NS |
| Uric acid (mmol/L) | 309 (260 to 339) | 313 (141 to 410) | 340 (285 to 369) | NS |
| Glycemia (mmol/L) | 4.88 (4.61 to 4.98) | 5.03 (4.61 to 5.74) | 5.02 (4.73 to 5.29) | NS |
| Serum Ca (mmol/L) | 2.45 (2.36 to 2.49) | 2.43 (2.34 to 2.52) | 2.46 (2.35 to 2.48) | NS |
| Serum ionized Ca (mmol/L) | 1.23 (1.19 to 1.26) | 1.23 (1.17 to 1.24) | 1.22 (1.18 to 1.24) | NS |
| Serum phosphate (mmol/L) | 1.84 (1.62 to 2.0) | 1.79 (1.25 to 2.84) | 1.98 (1.76 to 2.08) | NS |
| Serum Mg (mmol/L) | 1.15 (1.07 to 1.2) | 1.19 (1 to 1.31) | 1.17 (1.08 to 1.21) | NS |
| Serum PTH (pg/mL) | 322 (227 to 406) | 215 (121 to 467) | 212 (94 to 345) | NS |
| Serum 25(OH) cholecalciferol (µg/L) | 21.35 (15.4 to 30.45) | 17.85 (11.9 to 28.7) | 19.8 (12.2 to 24.2) | NS |
| Serum 1,25 (OH)2D3 (ng/L) | 18 (13 to 20) | 12.8 (8 to 18) | 16 (11.4 to 20.6) | NS (0.07) |
| Bone alkaline phosphatase (µg/L) | 25 (20 to 30) | 17 (12 to 25) | 18.5 (14 to 25) | NS (0.06) |
| Serum albumin (g/L) | 39.9 (38.6 to 41) | 37a (35 to 38.8) | 37a (36 to 38.6) | <0.001 |
| Hemoglobin (mmol/L) | 10 (9.5 to 10.5) | 9.7 (8.2 to 10.2) | 10.9 (8.9 to 11.4) | NS |
| hCRP (mg/L) | 3 (3 to 5) | 10a (7 to 12) | 8a (7 to 11) | <0.001 |
Values are medians (95% confidence intervals). Kruskal–Wallis one-way ANOVA on ranks.
Statistically different from normal ABix.
Bone Histomorphometry
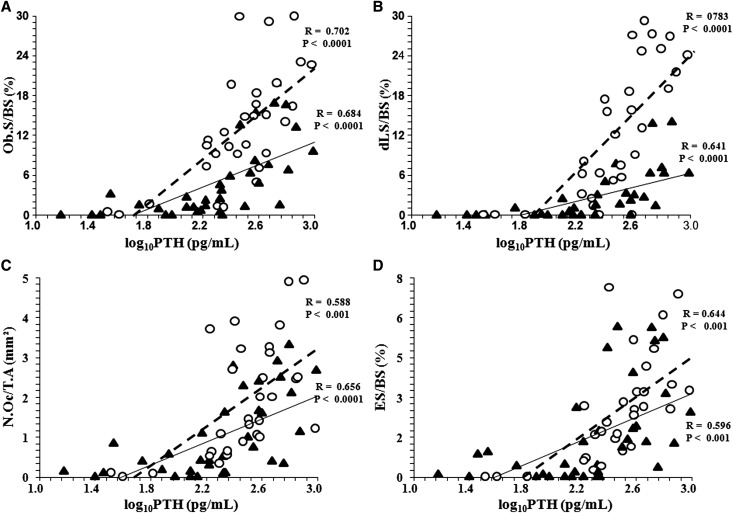
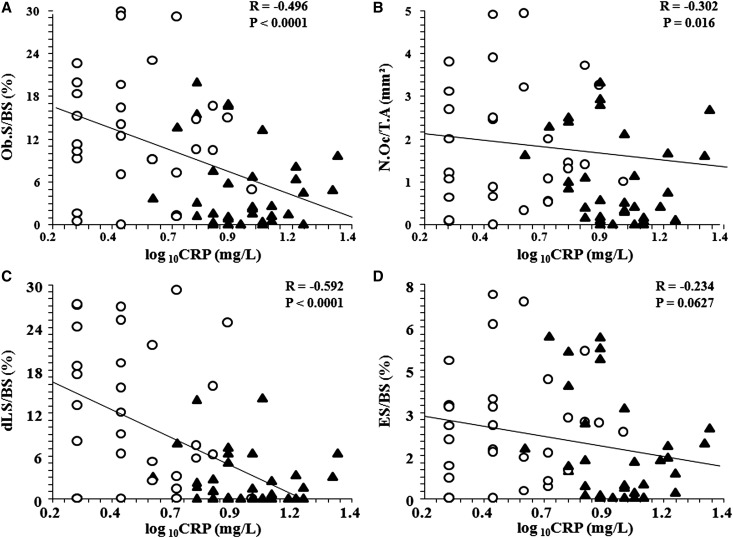
Bone histomorphometry parameters are given in Table 3. Osteoblast surface per bone surface (Ob.S/BS) and double-labeled surface (dLS/BS) were significantly lower in patients with PAD. Patients with PAD had higher aluminum-stained surface but similar bone volume and osteoid volume. In multiple regression analyses, dLS/BS was positively associated with serum PTH (P<0.001), and it was negatively associated with serum hCRP (P<0.001) but not negatively associated with aluminum-stained surfaces (P=0.27). As shown in Figure 1 in pooled abnormal ABix, after adjustment for age and serum hCRP, the correlations between serum PTH, dLS/BS, and Ob.S/BS were positive for normal and abnormal ABix (Figure 1). Upward shifts with significantly steeper slopes (β-coefficient) of the correlation between dLS/BS and PTH (mean β-coefficient±SD; 21±24.4 versus 5.12±30.3; T=2.34; P=0.03) and between Ob.S/BS and PTH (mean β-coefficient±SD; 17±18.6 versus 8.4±10.2; T=2.25; P=0.03) were observed for patients with normal ABix. Osteoclast number/per millimeter2 (N.Oc/T.A) and eroded surface (ES/BS) did not differ among the three groups (Figure 1). The correlations between circulating PTH, N.Oc/T.A, and ES/BS, were positive and similar for normal and abnormal ABix. Significant negative serum PTH-adjusted correlations were observed between serum hCRP, Ob.S/BS, and dLS/BS (Figure 2).
Table 3.
Bone histomorphometry
| Surfaces | ABix | ANOVA P Value | ||
|---|---|---|---|---|
| Normal (n=30) | Low (n=11) | >1.4 (n=24) | ||
| Ob.S/BS (%) | 11.81 (9.12 to 16.33) | 2.42a (0.89 to 7.5) | 2.66a (0.3 to 6.3) | 0.002 |
| dLS/BS (%) | 10.52 (5.6 to 18.5) | 1.33a (0 to 2.40) | 1a (0 to 3.20) | <0.001 |
| N.Oc/T.A (mm2) | 1.42 (1 to 2.50) | 0.40b (0.1 to 1) | 0.80 (0.15 to 1.62) | 0.01 |
| ES/BS (%) | 2.58 (1.52 to 3.40) | 0.48 (0 to 1.4) | 1.38 (0.1 to 2.61) | NS |
| BV/TV (%) | 21.01 (16 to 22.3) | 19.23 (11.2 to 23.9) | 15.8 (12.66 to 20.7) | NS |
| OV/BV (%) | 8.76 (5.8 to 11.4) | 7.80 (2.45 to 11.1) | 6.15 (2.7 to 10.8) | NS |
| Aluminum-stained surface (%) | 5 (7.5 to 28.4) | 48a (20 to 91) | 48a (5 to 75) | <0.01 |
Values are medians (95% confidence intervals). Kruskal–Wallis one-way ANOVA on ranks with multiple comparison Z-value test. BV/TV, bone volume; OV/BV, osteoid volume.
Significantly different from normal ABix.
Significantly different from low ABix and ABix>1.4.
Figure 1.
Correlations between serum PTH and bone histomorphometry parameters. (A) Ob.S/BS, (B) dLS/BS, (C) N.Oc/T.A, and (D) ES/BS for patients with normal ABix (white circles) and patients with abnormal ABix (black triangles). The correlations are adjusted to serum CRP.
Figure 2.
Correlations between serum hCRP and bone histomorphometry parameters. (A) Ob.S/BS, (B) dLS/BS, (C) N.Oc/T.A, and (D) ES/BS in patients with normal ABix (white circles) and patients with abnormal ABix (black triangles). The correlations are adjusted to serum PTH.
Corrected univariate correlations showed that PAD was positively associated with serum CRP, age, dialysis vintage, and calcium carbonate dose and inversely related to dLS/BS, Ob.S/BS, aluminum-stained surfaces, and PTX (Table 4). Because of multiple colinearities (for example, correlation between vintage and PTX: R=0.3615; P=0.004 or correlation between vintage and aluminum-stained surface: R=0.5365; P<0.001), multivariate stepwise correlation analysis identified only hCRP, vintage, and dLS/BS as significant cofactors associated with PAD (Table 5).
Table 4.
Univariate correlations between PAD status (0, normal; 1, PAD) and clinical and biochemistry parameters
| Parameter | R Value | P Value |
|---|---|---|
| Age (yr) | 0.5936 | <0.001 |
| Vintage (mo) | 0.4878 | <0.001 |
| CaCO3 (g/d) | 0.5230 | <0.001 |
| hCRP (log mg/L) | 0.7512 | <0.001 |
| Serum albumin (g/L) | −0.5920 | <0.001 |
| dLS/BS (%) | −0.5627 | <0.001 |
| Ob.S/BS (%) | −0.5054 | <0.001 |
| N.Oc/T.A (mm2) | −0.3855 | 0.002 |
| Aluminum-stained surface (%) | 0.3539 | 0.004 |
| PTX (no, 0; yes, 1) | 0.3570 | 0.004 |
Table 5.
Stepwise regression report for PAD status (0, normal; 1, PAD)
| Parameter | T Value | P Value | Partial R2 Adjusted for Rest |
|---|---|---|---|
| Vintage (mo) | 4.040 | <0.001 | 0.2111 |
| dLS/BS (%) | −2.877 | <0.01 | 0.1195 |
| Log hCRP (mg/L) | 6.087 | <0.001 | 0.3669 |
| Age (yr) | 0.850 | 0.40 | NA |
| CaCO3 (g/d) | 1.1935 | 0.24 | NA |
| N.Oc/T.A (mm2) | 0.6961 | 0.49 | NA |
| PTX (no, 0; yes, 1) | 0.5972 | 0.55 | NA |
| Aluminum-stained surfaces (%) | 0.0509 | 0.96 | NA |
R2=0.6843.
Discussion
Our results indicated that, in patients with prevalent hemodialysis, subclinical PAD was associated with low bone turnover and more pronounced osteoblast resistance to PTH, which was assessed by decreased dLS/BS and Ob.S/BS and lower correlation β-coefficients (slopes) between serum PTH and dLS/BS or Ob.S/BS (Figure 1, A and B). The correlations between PAD and N.Oc/T.A or ES/BS did not differ from subjects with normal ABix. These bone–artery associations remained significant after adjustment for age, serum hCRP, and hemodialysis vintage. Although hemodialysis vintage and serum hCRP were independently associated with PAD, serum mineral parameters, including PTH, did not differ significantly between groups. Unlike the published association between the calcium phosphate binders doses and aortic calcifications,8 in multivariate analyses, this association was not observed in peripheral arteries with abnormal ABix.
Decreased femoral neck or total hip BMD and increased risk of fractures were reported to be associated with PAD,16,18,19 and bone perfusion was reduced in osteoporotic patients compared with normal and osteopenic subjects.15 In a study on patients with unilateral PAD, Laroche et al.16 reported that BMD was significantly lower in the affected limb compared with the unaffected limb. Unlike the reported association between PAD and local femoral BMD, our results indicated an association between PAD and systemic bone changes in nonweight-bearing anterior iliac crest.
Our study population did not include patients with diabetes, and the only common bone–artery risk factor was higher hCRP in patients with abnormal ABix (Tables 2 and 5). In an experimental in vivo study, Hjortnaes et al.24 showed the role of inflammation in the inverse relationship between osteoporotic bone remodeling and arterial and aortic valve calcifications. Inflammation is associated with atherosclerosis, a strong inductor of vascular calcifications,25,26 and a modulator of osteoblast activity.27 Independent of serum PTH, high serum hCRP was positively associated with abnormal ABix and inversely correlated with dLS/BS and Ob.S/BS (Figure 2).
However, the correlations between PTH and bone turnover markers were independent (Figure 1) of hCRP, suggesting that the resistance to PTH could be associated with arterial changes. As shown in Figure 1 and Table 5, an abnormal ABix was associated with low bone turnover, principally affecting osteoblasts. In contrast, N.Oc/T.A and resorption activity did not differ significantly between patient groups. In a study on the general population, Pennisi et al.17 showed that peripheral vessels atherosclerosis was associated with biochemistry parameters suggestive of reduced bone formation and abnormal bone turnover. PTH resistance in patients with ESRD is well known28 and multifactorial, including abnormal PTH signaling. Downregulation of PTH/PTH-related protein-receptor type 1 (PTHrP1) gene expression and mRNA in osteoblasts,29–31 presence of antagonistic C-terminal PTH fragments,32 hyperlipidemia-induced oxidant stress,33 uremic milieu,34 uremic toxins,35 inflammation,36 and aging37 are all mechanisms accounting for skeletal resistance to PTH and adynamic bone.
Could defective PTH signaling play a role in the development of bone–vascular axis abnormalities? Arterial calcifications are highly prevalent in subjects with low bone turnover8 and abnormal ABix.22 Experimental data showed that, by signaling through the PTH/PTHrP receptor (PTH1R), parathyroid PTH1–34 inhibited bovine vascular smooth muscle cell (VSMC) calcification38 and blocked the calcifying action of calcitriol.39 Shao et al.40 showed that teriparatide (human PTH1–34) inhibited osteogenic vascular calcification in diabetic LDL receptor-deficient mice. Cheng et al.41 showed that activation of VSMC PTH1R inhibited the Wnt/2-Catenin signaling pathway and prevented aortic calcifications and fibrosis in diabetic arteriosclerosis. The role of PTH1R signaling through PTH or PTHrP in arterial remodeling remains the subject of investigations, but experimental data indicate that PTHrP inhibited VSMC migration and proliferation42,43 and neointimal formation.44 PTH1R signaling plays an important role in the skeletal response to PTH through the control of osteocyte activation of SOST/sclerostin. In the presence of PTH resistance and impaired signaling, the transcriptional suppression of sclerostin production might be impaired.45,46 Resulting from experimental data, these hypotheses were not tested in this population, but serum sclerostin is increased in patients with ESRD47,48 and associated with cardiovascular calcifications.49
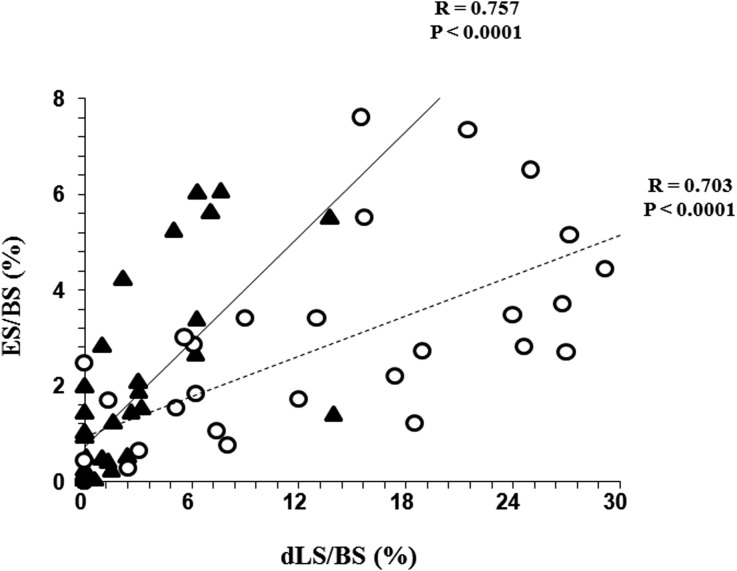
Our findings support, in a human ESRD population, the common role of inflammation in bone and cardiovascular remodeling, which was shown experimentally by Hjortnaes et al.,24 but the association between low bone turnover and arterial remodeling is not new.8,50 Hjortnaes et al.24 confirm the dissociation between serum PTH concentrations and bone histology and PTH concentration with clinical disease. Herein, the presence of subclinical PAD was not associated with any differences in serum PTH but was associated with a different clinical effect, which was characterized by skeletal resistance to PTH involving, more importantly, osteoblast function and number compared with osteoclast and bone erosion (Figure 3). Bone remodeling is maintained by a balance between bone erosion and bone formation and dependent on bidirectional communication between osteoblasts and osteoclasts through paracrine factors (receptor activator of NF-κB [RANK] ligand, osteoprotegerin, and ephrinB2 ligand), cell–cell contact, and cell–bone matrix interactions.50 Lesser coupling between bone erosion and bone formation with decreased number and activity of osteoblasts was observed in several conditions, such as skeletal unloading during prolonged bed rest,51 aluminum-related osteodystrophy in patients on dialysis,52 and chronic inflammation.53,54 In this study, the PTH- and CRP-adjusted correlation between aluminum-stained surfaces and dLS/BS was not significant, but patients with PAD had microinflammation and increased serum CRP. We can speculate that the microinflammation could play a role in bone erosioformation uncoupling. As shown on Figure 2, serum CRP was inversely correlated with dLS/BS and Ob.S/BS but less correlated or not correlated with N.Oc/T.A and ES/BS. Inflammation and proinflammatory cytokines, such as TNF-α and IL-1, could cause an imbalance in bone remodeling by downregulation of PTH/PTHrP136 and activation of osteoclasts through classic or alternative RANK/RANK ligand pathways favoring bone erosion.53,54
Figure 3.
Correlation between bone histomorphometry parameters. dLS/BS and ES/BS in patients with normal ABix (white circles) and patients with abnormal ABix (black triangles).
The possible role of abnormal PTH signaling in arterial remodeling and vascular pathology remains hypothetical, because observational studies on the basis of correlations studies and associations are not proof of causality. This limitation is an important limitation of this study. Another limitation concerns the limited number of patients and clinical characteristics of the population, which included relatively young subjects with primary kidney disease, excluding diabetes, treated in the 1990s. This population differs markedly from the population treated today, which includes higher percentages of patients with diabetes and older patients with overt cardiovascular comorbidities and shorter vintage. The treatment modalities have evolved with withdrawal of aluminum-containing phosphate binders and the use of noncalcium-containing phosphate binders, the wider use of vitamin D receptor agonists and cholecalciferol supplementation, the prescription of calcimimetics, and the improvement of hemodialysis techniques.
In summary, our results showed that, in prevalent nondiabetic patients with ESRD, the PAD was associated with low bone turnover and low bone formation with pronounced osteoblast resistance to PTH.
Concise Methods
Patients
With the exception of 1 patient, the population of 65 prevalent nondiabetic patients on hemodialysis was previously detailed.55 Inclusion criteria were (1) hemodialysis vintage ≥12 months and (2) absence of clinical history of cardiovascular disease, including history of lower limb arteries angioplasty, stenting, amputation, or trophic disorders (ulcerations or gangrene). Dialysis duration was individually tailored (4–6 hours three times per week) to control body fluids and blood chemistries. The bicarbonate dialysate was prepared using double reverse osmosis-treated water with 1.5 or 1.75 mmol/L Ca according to the serum Ca-PO4 equilibrium and the need for active vitamin D3 (1α-OH-D3 prescribed in eight patients). Although CaCO3 was used exclusively as a PO4 binder at the time of the study, 28 patients had taken aluminum hydroxide in the past; 12 patients underwent subtotal PTX, and 10 patients underwent total PTX with heterotopic autotransplantation into the forearm. PTX had been performed 20–70 months before the study. Erythropoietin was administered to maintain hemoglobin≥100 g/L when necessary. All subjects gave informed written consent to participate in the study, which was approved by our Institutional Review Board in accordance with the Declaration of Helsinki.
ABix
Lower limb artery status was on the basis of ABix measurement and the ratio between SBP in the ankle (arteria tibialis posterior or dorsalis pedis) and the arm (arteria brachialis). SBPs were measured in a supine position after 15 minutes of rest. Brachial artery SBP was measured two times in the arm without arteriovenous shunt and averaged. Ankle SBP was measured two times in each foot and averaged. SBPs were measured with a Doppler SEGA M842 8-MHz Unit (Société Electronique Générale et Appliquée, Paris, France) during cuff deflation. Patients were divided in three groups according to their ABix values: normal ABix, 0.9–1.3; low ABix, <0.9; >1.4 (i.e., incompressible).
Bone Histomorphometry
Diagnostic anterior iliac crest bone biopsies were obtained after dLS/BS according to the schedule of 2 days on tetracycline, 10 days off tetracycline, and 2 days on tetracycline as previously detailed.55 The extent of the dLS/BS (percent) was measured on two unstained 10-µm-thick sections. On three Toluidine blue-stained 5-µm-thick sections, bone volume (percent), Ob.S/BS (percent), ES/BS (percent), and N.Oc/T.A were assessed. Bone Al staining was expressed as the percentage of the trabecular surface stained. All measurements were made using an eyepiece reticle (Carl Zeiss Integral Plate II, Oberkochen, Germany).
Blood Chemistries
Blood chemistries, including serum Ca and PO4, blood lipids, blood glucose, uric acid, and serum albumin, are the mean values of all measurements in the 6 months preceding the ABix measurements. Routine biochemical parameters were determined by standard methods using autoanalyzers. Blood samples for measurement of bone alkaline phosphatase serum levels (Quidel MicroVue BAP EIA), 25(OH) cholecalciferol, and 1,25(OH)2D3 were taken the day of the bone biopsy. Intact PTH (N-IRMA; Nichols Institute) was determined every 3 months, and the reported values are the average of two measurements done during the 6 months preceding the bone biopsy. Bone biopsy and measurement of ABix were done the same month.
Statistical Analyses
Data are expressed as medians and 95% confidence intervals. The primary analysis concerned ABix subgroup normal, low, or >1.4 comparison with Kruskal–Wallis one-way ANOVA on ranks and Bonferroni multiple comparison Z-test value. For the univariate (Pearson or Spearman correlation coefficient), and multivariate regression studies, low and incompressible ABix groups were pooled and considered to have PAD. The correlations slopes are expressed as β-coefficients±SD and compared by t test. For these correlations, artery disease status was used as a dummy variable (0, normal ABix; 1, PAD). Multiple regression analyses were performed using the subset of univariate analysis-selected independent variables (after Bonferroni correction for the number of correlations studied). All analyses were calculated using NCSS 2000 (Gerry Hintze, Kaysville, UT).
Disclosures
None.
Acknowledgments
We thank Ms. Janet Jacobson for editorial assistance.
The study was supported by Groupe d’Étude de la Pathophysiologie de l’Insuffisance Rénale (GEPIR).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Arteriosclerosis, Bone Biology, and Calciotropic Hormone Signaling: Learning the ABCs of Disease in the Bone-Vascular Axis,” on pages 243–245.
References
- 1.Thompson B, Towler DA: Arterial calcification and bone physiology: Role of the bone-vascular axis. Nat Rev Endocrinol 8: 529–543, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schulz E, Arfai K, Liu X, Sayre J, Gilsanz V: Aortic calcification and the risk of osteoporosis and fractures. J Clin Endocrinol Metab 89: 4246–4253, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Tankó LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR: Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res 20: 1912–1920, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Szulc P, Kiel DP, Delmas PD: Calcifications in the abdominal aorta predict fractures in men: MINOS study. J Bone Miner Res 23: 95–102, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Naves M, Rodríguez-García M, Díaz-López JB, Gómez-Alonso C, Cannata-Andía JB: Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 19: 1161–1166, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Hyder JA, Allison MA, Wong N, Papa A, Lang TF, Sirlin C, Gapstur SM, Ouyang P, Carr JJ, Criqui MH: Association of coronary artery and aortic calcium with lumbar bone density: The MESA Abdominal Aortic Calcium Study. Am J Epidemiol 169: 186–194, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pennisi P, Russo E, Gaudio A, Veca R, D’Amico F, Mangiafico RA, Laspina M, Tringali G, Signorelli SS, Fiore CE: The association between carotid or femoral atherosclerosis and low bone mass in postmenopausal women referred for osteoporosis screening. Does osteoprotegerin play a role? Maturitas 67: 358–362, 2010 [DOI] [PubMed] [Google Scholar]
- 8.London GM, Marty C, Marchais SJ, Guérin AP, Métivier F, de Vernejoul MC: Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15: 1943–1951, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Parhami F, Garfinkel A, Demer LL: Role of lipids in osteoporosis. Arterioscler Thromb Vasc Biol 20: 2346–2348, 2000 [DOI] [PubMed] [Google Scholar]
- 10.Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS: Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: Evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int 16: 1263–1271, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Gerdhem P, Obrant KJ: Effects of cigarette-smoking on bone mass as assessed by dual-energy X-ray absorptiometry and ultrasound. Osteoporos Int 13: 932–936, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Mody N, Parhami F, Sarafian TA, Demer LL: Oxidative stress modulates osteoblastic differentiation of vascular and bone cells. Free Radic Biol Med 31: 509–519, 2001 [DOI] [PubMed] [Google Scholar]
- 13.Bridgeman G, Brookes M: Blood supply to the human femoral diaphysis in youth and senescence. J Anat 188: 611–621, 1996 [PMC free article] [PubMed] [Google Scholar]
- 14.Alagiakrishnan K, Juby A, Hanley D, Tymchak W, Sclater A: Role of vascular factors in osteoporosis. J Gerontol A Biol Sci Med Sci 58: 362–366, 2003 [DOI] [PubMed] [Google Scholar]
- 15.Griffith JF, Yeung DKW, Tsang PH, Choi KC, Kwok TCY, Ahuja AT, Leung KS, Leung PC: Compromised bone marrow perfusion in osteoporosis. J Bone Miner Res 23: 1068–1075, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Laroche M, Pouilles JM, Ribot C, Bendayan P, Bernard J, Boccalon H, Mazieres B: Comparison of the bone mineral content of the lower limbs in men with ischaemic atherosclerotic disease. Clin Rheumatol 13: 611–614, 1994 [DOI] [PubMed] [Google Scholar]
- 17.Pennisi P, Signorelli SS, Riccobene S, Celotta G, Di Pino L, La Malfa T, Fiore CE: Low bone density and abnormal bone turnover in patients with atherosclerosis of peripheral vessels. Osteoporos Int 15: 389–395, 2004 [DOI] [PubMed] [Google Scholar]
- 18.von Mühlen D, Allison M, Jassal SK, Barrett-Connor E: Peripheral arterial disease and osteoporosis in older adults: The Rancho Bernardo Study. Osteoporos Int 20: 2071–2078, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collins TC, Ewing SK, Diem SJ, Taylor BC, Orwoll ES, Cummings SR, Strotmeyer ES, Ensrud KE, Osteoporotic Fractures in Men (MrOS) Study Group : Peripheral artery disease is associated with higher rates of hip bone loss and increased fracture risk in older men. Circulation 119: 2305–2312, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guerrero A, Montes R, Muñoz-Terol J, Gil-Peralta A, Toro J, Naranjo M, González-Pérez P, Martín-Herrera C, Ruiz-Fernández A: Peripheral arterial disease in patients with stages IV and V chronic renal failure. Nephrol Dial Transplant 21: 3525–3531, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Liu J-H, Lin H-H, Yang Y-F, Liu Y-L, Kuo H-L, Wang I-K, Chou C-Y, Huang C-C: Subclinical peripheral artery disease in patients undergoing peritoneal dialysis: Risk factors and outcome. Perit Dial Int 29: 64–71, 2009 [PubMed] [Google Scholar]
- 22.Adragao T, Pires A, Branco P, Castro R, Oliveira A, Nogueira C, Bordalo J, Curto JD, Prata MM: Ankle—brachial index, vascular calcifications and mortality in dialysis patients. Nephrol Dial Transplant 27: 318–325, 2012 [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Guo X, Li J, Hu D, Zhao D, Ma H, Mou Q, Liu J, Xu Y: Predictive value of ankle-brachial index to all-cause mortality and cardiovascular mortality in Chinese patients with chronic kidney disease. Vasa 41: 205–213, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Hjortnaes J, Butcher J, Figueiredo JL, Riccio M, Kohler RH, Kozloff KM, Weissleder R, Aikawa E: Arterial and aortic valve calcification inversely correlates with osteoporotic bone remodelling: A role for inflammation. Eur Heart J 31: 1975–1984, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aikawa E, Nahrendorf M, Figueiredo JL, Swirski FK, Shtatland T, Kohler RH, Jaffer FA, Aikawa M, Weissleder R: Osteogenesis associates with inflammation in early-stage atherosclerosis evaluated by molecular imaging in vivo. Circulation 116: 2841–2850, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Al-Aly Z, Shao J-S, Lai C-F, Huang E, Cai J, Behrmann A, Cheng S-L, Towler DA: Aortic Msx2-Wnt calcification cascade is regulated by TNF-α-dependent signals in diabetic Ldlr-/- mice. Arterioscler Thromb Vasc Biol 27: 2589–2596, 2007 [DOI] [PubMed] [Google Scholar]
- 27.Shapiro S, Tatakis DN, Dziak R: Effects of tumor necrosis factor alpha on parathyroid hormone-induced increases in osteoblastic cell cyclic AMP. Calcif Tissue Int 46: 60–62, 1990 [DOI] [PubMed] [Google Scholar]
- 28.Massry SG, Coburn JW, Lee DBM, Jowsey J, Kleeman CR: Skeletal resistance to parathyroid hormone in renal failure. Studies in 105 human subjects. Ann Intern Med 78: 357–364, 1973 [DOI] [PubMed] [Google Scholar]
- 29.Ureña P, Mannstadt M, Hruby M, Ferreira A, Schmitt F, Silve C, Ardaillou R, Lacour B, Abou-Samra AB, Segre GV, Drüeke T: Parathyroidectomy does not prevent the renal PTH/PTHrP receptor down-regulation in uremic rats. Kidney Int 47: 1797–1805, 1995 [DOI] [PubMed] [Google Scholar]
- 30.Picton ML, Moore PR, Mawer EB, Houghton D, Freemont AJ, Hutchison AJ, Gokal R, Hoyland JA: Down-regulation of human osteoblast PTH/PTHrP receptor mRNA in end-stage renal failure. Kidney Int 58: 1440–1449, 2000 [DOI] [PubMed] [Google Scholar]
- 31.Iwasaki-Ishizuka Y, Yamato H, Nii-Kono T, Kurokawa K, Fukagawa M: Downregulation of parathyroid hormone receptor gene expression and osteoblastic dysfunction associated with skeletal resistance to parathyroid hormone in a rat model of renal failure with low turnover bone. Nephrol Dial Transplant 20: 1904–1911, 2005 [DOI] [PubMed] [Google Scholar]
- 32.Slatopolsky E, Finch J, Clay P, Martin D, Sicard G, Singer G, Gao P, Cantor T, Dusso A: A novel mechanism for skeletal resistance in uremia. Kidney Int 58: 753–761, 2000 [DOI] [PubMed] [Google Scholar]
- 33.Sage AP, Lu J, Atti E, Tetradis S, Ascenzi M-G, Adams DJ, Demer LL, Tintut Y: Hyperlipidemia induces resistance to PTH bone anabolism in mice via oxidized lipids. J Bone Miner Res 26: 1197–1206, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Disthabanchong S, Hassan H, McConkey CL, Martin KJ, Gonzalez EA: Regulation of PTH1 receptor expression by uremic ultrafiltrate in UMR 106-01 osteoblast-like cells. Kidney Int 65: 897–903, 2004 [DOI] [PubMed] [Google Scholar]
- 35.Nii-Kono T, Iwasaki Y, Uchida M, Fujieda A, Hosokawa A, Motojima M, Yamato H, Kurokawa K, Fukagawa M: Indoxyl sulfate induces skeletal resistance to parathyroid hormone in cultured osteoblastic cells. Kidney Int 71: 738–743, 2007 [DOI] [PubMed] [Google Scholar]
- 36.Katz MS, Gutierrez GE, Mundy GR, Hymer TK, Caulfield MP, McKee RL: Tumor necrosis factor and interleukin 1 inhibit parathyroid hormone-responsive adenylate cyclase in clonal osteoblast-like cells by down-regulating parathyroid hormone receptors. J Cell Physiol 153: 206–213, 1992 [DOI] [PubMed] [Google Scholar]
- 37.Zhou S, Bueno EM, Kim SW, Amato I, Shen L, Hahne J, Bleiberg I, Morley P, Glowacki J: Effects of age on parathyroid hormone signaling in human marrow stromal cells. Aging Cell 10: 780–788, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jono S, Nishizawa Y, Shioi A, Morii H: Parathyroid hormone-related peptide as a local regulator of vascular calcification. Its inhibitory action on in vitro calcification by bovine vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 17: 1135–1142, 1997 [DOI] [PubMed] [Google Scholar]
- 39.Jono S, Nishizawa Y, Shioi A, Morii H: 1,25-Dihydroxyvitamin D3 increases in vitro vascular calcification by modulating secretion of endogenous parathyroid hormone-related peptide. Circulation 98: 1302–1306, 1998 [DOI] [PubMed] [Google Scholar]
- 40.Shao J-S, Cheng S-L, Charlton-Kachigian N, Loewy AP, Towler DA: Teriparatide (human parathyroid hormone (1-34)) inhibits osteogenic vascular calcification in diabetic low density lipoprotein receptor-deficient mice. J Biol Chem 278: 50195–50202, 2003 [DOI] [PubMed] [Google Scholar]
- 41.Cheng S-L, Shao J-S, Halstead LR, Distelhorst K, Sierra O, Towler DA: Activation of vascular smooth muscle parathyroid hormone receptor inhibits Wnt/beta-catenin signaling and aortic fibrosis in diabetic arteriosclerosis. Circ Res 107: 271–282, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ishikawa M, Akishita M, Kozaki K, Toba K, Namiki A, Yamaguchi T, Orimo H, Ouchi Y: Amino-terminal fragment (1-34) of parathyroid hormone-related protein inhibits migration and proliferation of cultured vascular smooth muscle cells. Atherosclerosis 136: 59–66, 1998 [DOI] [PubMed] [Google Scholar]
- 43.Song GJ, Fiaschi-Taesch N, Bisello A: Endogenous parathyroid hormone-related protein regulates the expression of PTH type 1 receptor and proliferation of vascular smooth muscle cells. Mol Endocrinol 23: 1681–1690, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fiaschi-Taesch N, Sicari B, Ubriani K, Cozar-Castellano I, Takane KK, Stewart AF: Mutant parathyroid hormone-related protein, devoid of the nuclear localization signal, markedly inhibits arterial smooth muscle cell cycle and neointima formation by coordinate up-regulation of p15Ink4b and p27kip1. Endocrinology 150: 1429–1439, 2009 [DOI] [PubMed] [Google Scholar]
- 45.Saini V, Marengi DA, Barry KJ, Fulzele KS, Heiden E, Liu X, Dedic C, Maeda A, Lotinun S, Baron R, Pajevic PD: Parathyroid hormone (PTH)/PTH-related peptide type 1 receptor (PPR) signaling in osteocytes regulates anabolic and catabolic skeletal responses to PTH. J Biol Chem 288: 20122–20134, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Powell WF, Jr., Barry KJ, Tulum I, Kobayashi T, Harris SE, Bringhurst FR, Pajevic PD: Targeted ablation of the PTH/PTHrP receptor in osteocytes impairs bone structure and homeostatic calcemic responses. J Endocrinol 209: 21–32, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cejka D, Herberth J, Branscum AJ, Fardo DW, Monier-Faugere M-C, Diarra D, Haas M, Malluche HH: Sclerostin and Dickkopf-1 in renal osteodystrophy. Clin J Am Soc Nephrol 6: 877–882, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pelletier S, Dubourg L, Carlier M-C, Hadj-Aissa A, Fouque D: The relation between renal function and serum sclerostin in adult patients with CKD. Clin J Am Soc Nephrol 8: 819–823, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brandenburg VM, Kramann R, Koos R, Krüger T, Schurgers L, Mühlenbruch G, Hübner S, Gladziwa U, Drechsler C, Ketteler M: Relationship between sclerostin and cardiovascular calcification in hemodialysis patients: A cross-sectional study. BMC Nephrol 14: 219–228, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irie N, Takada Y, Watanabe Y, Matsuzaki Y, Naruse C, Asano M, Iwakura Y, Suda T, Matsuo K: Bidirectional signaling through ephrinA2-EphA2 enhances osteoclastogenesis and suppresses osteoblastogenesis. J Biol Chem 284: 14637–14644, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zerwekh JE, Ruml LA, Gottschalk F, Pak CYC: The effects of twelve weeks of bed rest on bone histology, biochemical markers of bone turnover, and calcium homeostasis in eleven normal subjects. J Bone Miner Res 13: 1594–1601, 1998 [DOI] [PubMed] [Google Scholar]
- 52.Faugere MC, Arnala IO, Ritz E, Malluche HH: Loss of bone resulting from accumulation of aluminum in bone of patients undergoing dialysis. J Lab Clin Med 107: 481–487, 1986 [PubMed] [Google Scholar]
- 53.Wei S, Siegal GP: Mechanisms modulating inflammatory osteolysis: A review with insights into therapeutic targets. Pathol Res Pract 204: 695–706, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schett G: Effects of inflammatory and anti-inflammatory cytokines on the bone. Eur J Clin Invest 41: 1361–1366, 2011 [DOI] [PubMed] [Google Scholar]
- 55.London GM, Marchais SJ, Guérin AP, Boutouyrie P, Métivier F, de Vernejoul MC: Association of bone activity, calcium load, aortic stiffness, and calcifications in ESRD. J Am Soc Nephrol 19: 1827–1835, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]