Abstract
Introduction
Numerous scales and assessments are available to assess sexual compulsivity (SC).
Aim
This study sought to conduct an Item Response Theory (IRT) analysis of the Sexual Compulsivity Scale (SCS) to provide evidence about its measurement precision at the various levels of the SC construct in a sample of highly sexually active gay and bisexual men (GBM).
Methods
SCS data from a sample of 202 GBM who are highly sexually active but who vary in their experiences of SC symptoms were modeled using Samejima's polytomous graded response IRT model. To describe the performance of the SCS relative to the HDSI, SCS scores were compared with participants’ corresponding HDSI results to determine sensitivity, specificity, positive and negative predictive values, and accuracy.
Main Outcome Measures
This study examined the correspondence between the SCS and the Hypersexual Disorder Screening Inventory (HDSI), a diagnostic instrument for the screening of hypersexuality.
Results
IRT analyses indicated that, although two of the SCS items had low reliability, the SCS as a whole was reliable across much of the SC continuum. Scores on the SCS and the HDSI were highly correlated; however, no potential cutoffs on the SCS corresponded strongly with the polythetic scoring criteria of the HDSI.
Conclusion
Comparisons of SCS scores with HDSI results indicated that the SCS itself could not serve as a substitute for the HDSI and would incorrectly classify a substantial number of individuals’ levels of hypersexuality. However, the SCS could be a useful screening tool to provide a preliminary screening of people at risk for meeting criteria on the HDSI. Combining the SCS and the HDSI may be an appropriate evaluation strategy in classifying GBM as negative on both (i.e., “non-hypersexual/non-SC”), positive on the SCS only (i.e., “at risk”), and positive on both the SCS and the HDSI (i.e., “problematic hypersexuality/SC”).
Keywords: gay and bisexual men, sexual compulsivity, hypersexuality, hypersexual disorder, item response theory, psychometrics
Introduction
Various theoretical frameworks have been proposed to describe sexual compulsivity (SC),1-8 which has been characterized as “sexual fantasies and behaviors that increase in intensity and frequency over time so as to interfere with personal, interpersonal, or vocational pursuits.”9-16 Driven by little consensus about its fundamental features, research has described SC as being a dysregulation of sexual desire or arousal,1,17,18 a behavioral addiction,3,4 a part of the OCD spectrum characterized by compulsive sexual behavior,2,11,19,20 and an impulse control disorder.21,22 Terminology has also varied widely in the literature with various descriptors used in attempts to delineate the fundamental features and unique aspects of the theoretical perspective.5,6 More recently, “hypersexuality” was proposed to synthesize the disparate and often competing perspectives and subsume the various elements of behavioral dysregulation, loss of control, and distress around excessive sexual thoughts and behaviors that result in clinically significant distress or problems in functioning.5
Numerous scales and instruments are available to assess theoretically different aspects of SC. Hook and colleagues conducted a review of measures of SC and identified over 17 instruments that have been developed and used across diverse samples, including gay and bisexual men (GBM), heterosexual men and women, psychotherapy patients, community samples, and college students.23 Currently, there are at least 10 self-report scales of SC symptoms and consequences, including the commonly used Sexual Compulsivity Scale (SCS),11,24-26 four self-report checklists, and three clinician-rated scales of SC symptoms (see Hook et al., 2010 for an in depth review).23 The SCS, the CSBI, and the SISSES have been found to be the most reliable and valid scales.5 Additionally, the Hypersexual Disorder Screening Inventory (HDSI) was developed for the clinical assessment of hypersexual disorder, which was proposed for inclusion in the DSM-5.5,27-29
Most of the available measures reviewed by Hook and colleagues were shown to have several limitations.23 Some of the measures were developed recently and therefore, have had limited research on their psychometric properties. Many of the studies investigating the psychometric properties of the scales have relied on small samples or specific populations (e.g., college students, individuals seeking treatment for sexual compulsivity). Internal consistency coefficients have been adequate, but little evidence exists about the temporal stability of instruments (i.e., test/re-test reliability), the factor structure of the scales, or convergent and discriminant validity. The most important limitation is a lack of evidence of the ability of some scales to discriminate between individuals with severe or less severe SC, an important factor to consider both, analytically and clinically.
While the need for consensus about its definition and operational criteria has been identified,5,6,18 particularly in light of the need for epidemiological data, there is also a need to identify which validated instruments are best for capturing data about SC symptomology.23 The SCS11,24-26 is a self-report, 10-item scale of SC symptoms that is widely used in research studies and the most widely used measure of SC among GBM.15 It has been to shown to be a correlate of sexual risk taking.10,15,24,30 Initially, higher SC was defined as the within-gender 80th-percentile score, which was subsequently demonstrated across a variety of studies to correspond to a score of approximately 24.31,32 With regard to its psychometric properties, the SCS has been used in studies with over 30 diverse samples and item-to-total correlations range from .46 to .68 and Cronbach alpha's range from .59 - .92 (almost all > .70).23 Additionally, there is a body of research providing evidence of its convergent and discriminant validity. Test-retest reliability over a period of two weeks was high (.95) and ranged from .64 to .80 when a longer period was tested (3 months). An early study suggested a 2-factor structure (social disruptiveness dimension & personal discomfort dimension) underlies the scale,24 but this factor structure has not been replicated.23
Aims
Given the demonstrated strengths of the SCS with regard to reliability and validity, our study sought to conduct an Item Response Theory (IRT) analysis of the SCS to provide evidence about its structure (i.e., its dimensionality) and its ability to discriminate among individuals with more or less severe SC, particularly when using the scale's commonly used cutoff score of 24. Previously published psychometric evaluations of the SCS have focused exclusively on classical test theory (CTT) statistics. In contrast to IRT, CTT statistics assume that a scale measures its purported construct consistently regardless of the level of the trait a person possesses.33,34 On the other hand, IRT modeling allows researchers to examine the extent to which a scale item is endorsed across varying levels of the underlying construct and, thereby, provides information about the measurement precision at all levels of the construct (i.e., does it measure equally well at low, average, and high levels of SC?) and about the utility of each item (i.e., do any items provide unique information at levels of SC not measured by other items?).35 We also sought to examine the correspondence between the SCS and the HDSI in screening highly sexually active GBM for evidence of SC/hypersexual symptomology. Given our prior work to establish the diagnostic precision of the HDSI in differentiating among GBM who engage in similar levels of sexual activity,29 it is critical to assess the utility of the SCS as a screening tool relative to the HDSI, in terms of cutoff scores on the SCS and how they corresponded with the diagnostic results of the HDSI.
Method
Analyses for this paper were conducted on data from The Pillow Talk Project,29 a study of highly sexually active GBM in New York City (NYC). The primary goal of the study was to enroll GBM who are similar with regard to number of casual sexual partners but who differ in the extent to which their sexual thoughts and behaviors are causing problems in their lives – the defining feature of SC. Project enrollment was ongoing at the time of the analyses for this manuscript, which includes the first 202 men enrolled in the project.
Participants and Procedures
Beginning in February of 2011, we enrolled participants utilizing the following recruitment strategies: 1) respondent-driven sampling; 2) Internet-based advertisements on social and sexual networking websites; 3) email blasts through NYC sex party listservs; and 4) active recruitment in NYC venues such as gay bars/clubs and sex parties. Potential participants completed a phone-based screening interview to assess preliminary eligibility, which was defined as: 1) at least 18 years of age; 2) biologically male and self-identified as male; 3) nine or more male sexual partners in the prior 90 days; 4) self-identification as gay, bisexual, or some other non-heterosexual identity (e.g., queer); and 5) daily access to the Internet in order to complete Internet-based assessments. We operationalized highly sexually active as having at least nine male sexual partners in the 90 days prior to enrollment based on prior research with both community-based and probability-based samples of MSM which showed this to be 2-3 times higher than the average number of partners for GBM.10,14,16,36,37 Sexual partners were defined as any partner with whom the participant engaged in any physical sexual activity that had the potential to lead to orgasm.
Participants who met preliminary eligibility were emailed a link to an Internet-based computer-assisted self-interview (CASI), which included informed consent procedures. Men completed this one-hour survey at home via the Internet before completing an in-person baseline appointment, during which the sex eligibility criterion was confirmed using a timeline followback (TLFB) interview. This paper focuses exclusively on the Internet-based CASI data. All procedures were reviewed and approved by the Institutional Review Board of the City University of New York.
Measures
Demographics
Participants were asked to report several demographic characteristics including sexual identity, age, race/ethnicity, educational background, and relationship status. Participants self-reported their HIV status in the Internet survey. Men who reported being HIV-positive were asked to provide proof of their HIV status during their in-person baseline appointment, and men who reported being HIV-negative or unsure of their HIV status received a rapid HIV test as part of their baseline appointment. Three participants received a preliminary HIV-positive result and were referred for confirmatory testing and linkage to care – data from these three men were not included in these analyses.
Sexual compulsivity
Participants completed the Sexual Compulsivity Scale (SCS),25,26,38 the most widely used measure of SC among GBM.23 Participants responded to 10 items on a Likert-type scale from 1 (not at all like me) to 4 (very much like me), and responses to the ten items were summed to get an overall score ranging from 10 to 40. A score of 24 or higher has been found to distinguish those with the highest levels of SC across multiple studies. 10,14,31,32,39
Hypersexual disorder
Participants completed the Hypersexual Disorder Screening Inventory (HDSI), a measure developed by the DSM-5 Workgroup committee27 that consists of a total of 7 items split into two sections which have shown evidence of reliability and validity29,40 in measuring recurrent and intense sexual fantasies, urges, and behaviors and distress and impairment as a result of those sexual fantasies, urges, and behaviors in the prior 6 months. Responses were scored from 0 (Never true) to 4 (Almost always true) and were summed to provide a dimensional severity index score ranging from 0 to 28. Polythetic diagnostic criteria have been proposed that require recoding responses into dichotomies whereby responses of 3 or 4 are coded as endorsement and all others are coded as non-endorsement. Following the recoding, a preliminary positive screening for hypersexual disorder (HD) has been operationalized as the endorsement of at least four items in section A and at least one item in section B.
Data Analysis Plan
After examining demographic distribution of the sample and demographic differences in SCS scores using analysis of variance (ANOVA) techniques, we utilized three broad analytic procedures: (1) factor analyses to assess the underlying structure of the SCS; (2) IRT analyses to examine the reliability of the SCS; and (3) a comparison of the SCS with the HDSI screening result to examine the validity of the SCS.
Examination of factor structure
Factor analysis was used to test the two primary assumptions of unidimensional IRT models. Specifically, the assumption is that a single latent construct is responsible for the patterns of responses to the scale items and, after adjusting for the variance resulting from the latent construct, the responses to the scale items are independent of each other (i.e., the assumption of local independence). In other words, these assumptions are that the items are all measuring the same construct, and that this construct is the only construct they share in common. An examination of the assumption of unidimensionality was done based on the results of a CFA in which a single factor was specified and an exploratory factor analysis (EFA). Within the CFA, we examined standard indicators of model fit,41-49 which included root mean square error of approximation (RMSEA) less than 0.06, comparative fit index (CFI) greater than 0.95, Tucker Lewis index (TLI) greater than 0.95, and weighted root mean square residual (WRMR) less than 1.0. We next conducted an EFA in order to obtain estimates of the factor eigenvalues and percent of variance accounted for by each factor and compared models ranging from one to three factors. The first factor having an eigenvalue that is at least 4 times greater than that of the second factor and accounting for at least 20% of the variance were considered evidence for unidimensionality.50 To examine the assumption of local independence, we calculated the residual correlation matrix from the CFA. Any residual correlations between two items that exceed the absolute value of .20 were considered indicative of local dependence.
All factor analyses were conducted using Mplus software version 6.12 using weighted least squares estimation.51 All factor indicators (SCS items) were specified as ordered categorical (i.e., ordinal) variables. Modification indices were requested for CFA models. Comparisons of nested models were conducted using the DIFFTEST option which produces chi-square statistics of change in model fit in which a statistically significant result suggests the more restricted model (that with higher degrees of freedom) is a significantly worse fit to the data, while a non-significant result suggests improvement in model fit with the added restrictions.
Item response theory analyses
We modeled participants’ responses to the ten SCS items using Samejima's polytomous graded response model.52 In classical approaches to reliability, a single reliability estimate is made across levels of the trait being measured. This approach obscures the fact that scales often are more reliable at some levels of trait than others. In contrast, IRT methods estimate the precision of individual items and the scale as a whole across all levels of the trait being measured. We conducted IRT analyses using IRTPRO version 2.1.53 Fit statistics provided from this software package are S-χ2, which are Pearson χ2-based fit statistics that express the degree of fit or misfit between observed and expected values in the data. We also converted raw SCS scores into their theta values and corresponding test information statistics to examine the reliability of the scale across the continuum of sexual compulsivity.
Comparisons of the SCS with the HDSI
The last set of analyses were intended to examine the correspondence of the SCS with the screening result of the HDSI and examine potential cutoffs on the SCS that may correspond to the results of the HDSI screening. To examine this, we calculated a series of psychometric statistics for each possible cutoff (i.e., the point at which someone is considered to have received a “positive” classification) on the SCS: (1) sensitivity or true positive rate (number of positive results on both the SCS and HDSI divided by the number of positive results on the HDSI); (2) specificity or true negative rate (number of negative results on both the SCS and HDSI divided by the number of negative results on the HDSI); (3) positive predictive value (number of positive results on both the SCS and HDSI divided by the number of positive results on the SCS); (4) negative predictive value (number of negative results on both the SCS and HDSI divided by the number of negative results on the SCS); and (5) accuracy (number of results that were negative or positive on both the SCS and HDSI divided by the total sample size). These analyses take each point on a scale as a potential cutoff and compare them with a dichotomous outcome (in this case, the HDSI classification) in order to produce the relevant statistics for each – in this case, we were comparing each point on the SCS scale with screening results from the HDSI. A cutoff score that maximizes each possible statistic (i.e., close to 1.0) would suggest that the cutoff had strong correspondence with the outcome (i.e., the HDSI classification).
Results
As can be seen in Table 1, the sample was demographically diverse with regards to several factors, with more than half the sample being men of color and 40% HIV-positive. We compared demographic groups on their SCS scores and found only two significant differences. Men who were HIV-positive had significantly higher scores than those who were HIV-negative, and those who had a high school diploma, GED, or less had significantly higher scores than those with a bachelor's degree or a graduate degree (they were also marginally higher than those with some college or an associate's degree).
Table 1.
Demographic characteristics and comparisons with SCS scores
| SCS Score |
|||||
|---|---|---|---|---|---|
| Variable | n | % | M | SD | Test Statistic |
| Race/Ethnicity | F(5, 196) = 1.86 | ||||
| Black | 33 | 16.3 | 24.42 | 6.82 | |
| Latino | 30 | 14.9 | 26.90 | 8.17 | |
| White | 114 | 56.4 | 23.25 | 6.92 | |
| Asian/Native Haw./Pac. Islander | 4 | 2.0 | 21.75 | 6.40 | |
| Multiracial/Other | 16 | 7.9 | 26.13 | 6.28 | |
| Other/Unknown | 5 | 2.5 | 27.40 | 5.18 | |
| HIV Status (confirmed) | t(200) = −2.32* | ||||
| Negative | 121 | 59.9 | 23.35 | 6.82 | |
| Positive | 81 | 40.1 | 25.68 | 7.31 | |
| Sexual Orientation | F(2, 198) = 1.31 | ||||
| Gay, queer, or homosexual | 172 | 85.6 | 24.06 | 7.09 | |
| Bisexual | 24 | 11.9 | 26.29 | 7.42 | |
| Other non-heterosexual identity | 6 | 2.5 | 22.00 | 2.51 | |
| Employment Status | F(4, 197) = 1.54 | ||||
| Full-time | 70 | 34.7 | 23.76 | 7.07 | |
| Part-time | 50 | 24.8 | 24.02 | 6.53 | |
| On disability | 23 | 11.4 | 24.39 | 7.17 | |
| Student (unemployed) | 18 | 8.9 | 22.00 | 7.86 | |
| Unemployed | 41 | 20.3 | 26.44 | 7.23 | |
| Highest Educational Attainment | F(3, 198) = 3.83* | ||||
| High school diploma/GED or less | 23 | 11.4 | 28.22a | 8.17 | |
| Some college or Associate's degree | 61 | 30.2 | 24.95a, b | 7.13 | |
| Bachelor's or other 4-year degree | 66 | 32.7 | 23.58b | 6.80 | |
| Graduate degree | 52 | 25.7 | 22.65b | 6.32 | |
| Relationship Status | t(200) = −0.72 | ||||
| Single | 159 | 78.7 | 24.09 | 7.12 | |
| Partnered | 43 | 21.3 | 24.98 | 7.05 | |
| M | SD | ||||
| Age | 37.03 | 11.35 | |||
Note. N = 202. Results of LSD post-hoc analyses are indicated using superscripts – means followed by different letters are significantly different from each other.
Examination of factor structure
We began by testing a single-factor model of the SCS using CFA and found mixed results regarding its fit, with some indices (χ2[35] = 110.44, p < 0.001; RMSEA = 0.10) suggesting adequate to poor fit and others (CFI = 0.98, TLI = 0.97, WRMR = 0.86) suggesting good fit. Upon examining modification indices, there was evidence of residual covariance between several items. After allowing residual covariance between items 1, 2, and 5 as well as 4 and 6, model fit improved and all indicators suggested good model fit, χ2(31) = 41.66, p = 0.10; RMSEA = 0.04; CFI = 0.996; TLI = 0.995; WRMR = 0.48). These results suggest that the association between these items was greater than the covariance estimated through a single latent factor. Given that residual covariation between items provides evidence that local independence was violated for the each pair of items, we explored this issue further within the IRT analyses.
We conducted EFA using Mplus to confirm that the assumption of unidimensionality had been adequately met for IRT analyses. The first factor extracted had an eigenvalue of 5.81, which was more than six times as large as the eigenvalue of 0.93 for the second factor. In all, the first factor accounted for 58.1% of the total variation. The results of the EFA supported the notion that sufficient unidimensionality was present within the scale to conduct IRT analyses.50 It is worth noting, however, that the three-factor solution extracted by the EFA had better fit to the data than the single factor solution, despite the single factor solution meeting standard EFA criteria for selection. Within the three-factor solution, all items loaded significantly onto only one factor – the first factor included items 1, 2, and 5; the second factor consisted of items 3, 7, 8, 9, and 10; the third factor consisted of items 4 and 6.
Item response theory analyses
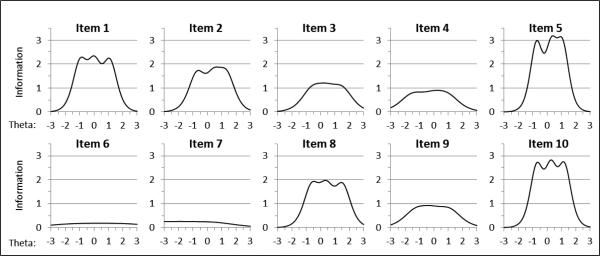
Each of the ten SCS items performed adequately in the analyses using an alpha threshold of .01. The p-values associated with the S-χ2 fit statistics ranged from 0.02 to 0.45, with an average p-value of 0.17 (See Table 2). However, as suggested by the range of p-values, the items performed at differing levels. A visual of each item's precision is presented in Figure 1. As can be seen, items 5 and 10 had excellent precision across much of the range of theta scores, while items 6 and 7 had poor precision across the entire range of theta. Although items 4 and 9 had less precision than others, they were the only two that had evidence of any precision at levels of theta less than -2. The final model itself had adequate fit, with a RMSEA statistic of 0.04. The software also provided some classical test theory statistics, such as the Cronbach's alpha, which was calculated to be 0.89 for the full scale. Results indicated that this estimate of internal consistency would not be substantially improved by the removal of any scale items. With regards to the assumption of local independence, the previously conducted CFA had indicated a significant residual correlation between several items. The IRT analyses, however, produced LD (i.e., local dependence) statistics54 of 4.1 for items 1 and 2, −0.8 for items 1 and 5, −0.3 for items 2 and 5, and 0.5 for items 4 and 6, all of which fell well below the threshold of 10 used to indicate some violation of local independence and were low enough to assume that the assumptions of IRT analyses were adequately met.
Table 2.
List of Sexual Compulsivity Scale Items with Corresponding Parameter Estimates and Fit Statistics
| Parameter Estimates |
S-χ2 |
|||||
|---|---|---|---|---|---|---|
| Item | Slope | Threshold 1 | Threshold 2 | Threshold 3 | χ 2 | χ2 p |
| 1. My desires to have sex have disrupted my daily life | 2.94 | −0.96 | 0.01 | 1.09 | 42.35 | 0.10 |
| 2. I sometimes fail to meet my commitments and responsibilities because of sex | 5.27 | −0.71 | 0.46 | 1.31 | 44.35 | 0.13 |
| 3. I sometimes get so horny I could lose control | 2.02 | −0.54 | 0.38 | 1.45 | 49.34 | 0.17 |
| 4. My sexual appetite has gotten in the way of my relationships | 1.74 | −1.45 | −0.08 | 0.85 | 51.00 | 0.16 |
| 5. My sexual thoughts and behaviors are causing problems in my life | 3.41 | −0.73 | 0.31 | 1.06 | 45.80 | 0.02 |
| 6. It has been difficult for me to find sex partners who desire having sex as much as I want | 0.77 | −1.45 | 0.40 | 2.20 | 67.15 | 0.22 |
| 7. I find myself thinking about sex while doing other things | 0.93 | −3.83 | −1.79 | 0.32 | 61.00 | 0.03 |
| 8. I feel my sexual thoughts and feelings are stronger than I am | 2.68 | −0.61 | 0.39 | 1.53 | 45.77 | 0.05 |
| 9. I think about sex more than I would like to | 1.76 | −1.20 | −0.20 | 1.03 | 43.76 | 0.40 |
| 10. I have to struggle to control my sexual thoughts and behavior | 3.24 | −0.72 | 0.27 | 1.20 | 29.42 | 0.45 |
Figure 1.
Above are the 10 IRT-based item information curves for the Sexual Compulsivity Scale. The horizontal axes display the values of theta (the value of the latent construct) ranging from −3 to 3. The vertical axes display the range of item information from 0 to 3.5, which indicates how precisely each item measures the construct (SC). Each individual plot shows how much information each item contributes to the scale across the possible values of theta.
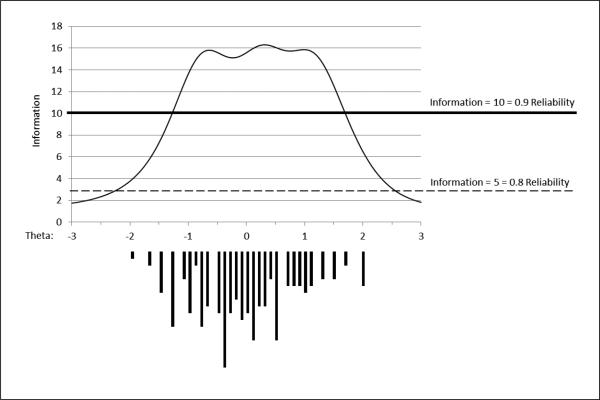
In addition to providing information regarding the contribution of each item on a scale, the IRT analyses provide useful diagnostics for the SCS scale on the whole. Table 3 provides the information values for the test as a whole across the continuum of the latent construct and Figure 2 displays the corresponding test information curve in the upper portion of the plot. Test information is the sum of information across all items and the curve displays the full scale's information function across the range of the latent construct. The test information curve is shown with two reference lines through it – a test information value of 5 corresponds with a reliability estimate of 0.80 demonstrating good reliability, and a value of 10 corresponds with a reliability estimate of 0.90 suggesting excellent reliability. As can be seen in the plot, the scale measured SC with at least 90% reliability from theta values of −1.2 to 1.8, which can be converted to corresponding SCS raw scores of 14 through 37. Similarly, the scale measured SC with at least 80% reliability across the range of theta values from −1.7 to 2.1, corresponding with SCS raw scores above 12 and less than 40 and covering virtually the entire range of possible scores. This suggests that the SCS has less than 80% reliability at only the lowest and highest possible values on the severity index (i.e., 10, 11, 12, and 40). It is worth noting that the often-used cutoff score of 24 for evidence of SC symptomology corresponded to a theta value of nearly 0 in this sample (i.e., the average value), and the scale well exceeded the threshold for 90% reliability at this score. This suggests the SCS is well suited for making distinctions between those with slightly lower and slightly higher levels of SC in this region of the construct (as it is along much of the continuum). The lower portion of Figure 3 shows that the distribution of scores across the latent construct was relatively normal and was well distributed from values of theta from −2.0 to 2.0.
Table 3.
Conversion Table to Transform Sexual Compulsivity Scale Scores to 6 Scores Along with the Scale's IRT-estimated Measurement Precision for Each Score
| Sum Score | θ Score | Test Information | S.E. | Sum Score | θ Score | Test Information | S.E. |
|---|---|---|---|---|---|---|---|
| 10 | −2.27 | 2.77 | 0.60 | 26 | 0.21 | 16.19 | 0.25 |
| 11 | −2.03 | 3.77 | 0.51 | 27 | 0.32 | 16.30 | 0.25 |
| 12 | −1.80 | 4.83 | 0.45 | 28 | 0.43 | 16.24 | 0.25 |
| 13 | −1.58 | 6.35 | 0.40 | 29 | 0.54 | 16.06 | 0.25 |
| 14 | −1.38 | 8.44 | 0.34 | 30 | 0.66 | 15.74 | 0.25 |
| 15 | −1.20 | 11.02 | 0.30 | 31 | 0.77 | 15.74 | 0.25 |
| 16 | −1.03 | 13.62 | 0.27 | 32 | 0.89 | 15.81 | 0.25 |
| 17 | −0.88 | 14.66 | 0.26 | 33 | 1.01 | 15.86 | 0.25 |
| 18 | −0.74 | 15.76 | 0.25 | 34 | 1.15 | 15.36 | 0.26 |
| 19 | −0.60 | 15.79 | 0.25 | 35 | 1.29 | 14.68 | 0.26 |
| 20 | −0.48 | 15.60 | 0.25 | 36 | 1.45 | 12.55 | 0.28 |
| 21 | −0.36 | 15.34 | 0.26 | 37 | 1.63 | 11.27 | 0.30 |
| 22 | −0.24 | 15.12 | 0.26 | 38 | 1.82 | 8.71 | 0.34 |
| 23 | −0.13 | 15.28 | 0.26 | 39 | 2.04 | 6.49 | 0.39 |
| 24 | −0.02 | 15.58 | 0.25 | 40 | 2.34 | 4.12 | 0.49 |
| 25 | 0.09 | 15.92 | 0.25 | ||||
Note: S.E. = Standard Error. Test information and standard error values are based on θ score values rounded to the nearest tenth decimal point.3.
Figure 2.
Above is the IRT-based test information curve for the Sexual Compulsivity Scale. The horizontal axis displays the values of theta (the value of the latent construct) ranging from −3 to 3. The vertical axis for the upper portion of the plot displays the range of test information from 0 to 18, which indicates how precisely the test measures the latent construct (SC). For values of theta between −1.8 and 2.1, the scale measures with at least 80% reliability; for values of theta between −1.2 and 1.8, the scale measures with at least 90% reliability (corresponding to raw scores of 15 to 38). The lower portion of the plot is a histogram of sample that shows the observed distribution of scores within the sample across the continuum of sexual compulsivity; this shows that the sample had adequate variability across much of the continuum from −2.0 to 2.0.
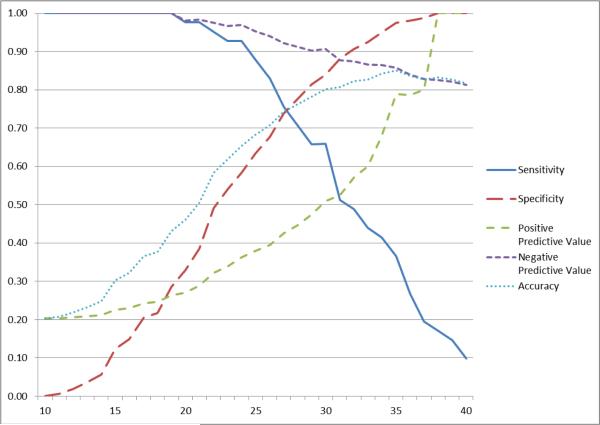
Figure 3.
Above is a plot of the psychometric statistics calculated for each possible cutoff on the SCS and their correspondence with the screening results of the HDSI. The formulas used to calculate each statistic are reported in the Method section of the text.
Alternative scoring analyses
The final analysis compared participants’ scores on the SCS with their corresponding screening results using the HDSI by comparing potential cutoff points on SCS raw score with the screening results of the HDSI. The results of these analyses are displayed in Figure 3 and suggested that there are several potential cutoffs on the SCS that correspond moderately well to the screening results of the HDSI. The commonly used cutoff of 24 displayed evidence of high sensitivity and reasonable specificity, suggesting a 7% rate of false-negatives (i.e., 1 minus sensitivity) and 42% rate of false-positives (i.e., 1 minus specificity). Higher cutoffs could be used to maximize specificity (i.e., reduce the rate of false-positives), but this would come with a corresponding decrease in sensitivity (i.e., the rate of false-negatives) as cutoff scores are increased. Sensitivity remained perfect through SCS cutoff scores of 19, suggesting that nobody who scored below a 20 on the SCS was classified as negative on the SCS but positive on the HDSI (on the other hand, between 71-100% of individuals were classified as positive on the SCS but negative on the HDSI in this range of scores). Two scores – 27 and 28 – had sensitivity and specificity rates that both exceeded 70%. Depending on the reason for using the SCS, it may be more desirable to maximize sensitivity, specificity, or both, but these results suggest that there were no cutoffs on the SCS that perfectly corresponded with the results of the HDSI. It is worth noting that, while the scale's overall accuracy was maximized at the highest scores on the SCS, this result was strongly influenced by the low number of individuals who screened positive relative to negative on the HDSI.
Discussion
The purpose of this study was to provide the first IRT-based analysis of the SCS in a sample of highly sexually active GBM. We examined the factor structure of the SCS, conducted IRT analyses to provide insight into its reliability of measurement at differing levels of SC, and finally examined its correspondence with the HDSI, a newly developed measure designed to unify investigations into problematic sexual thoughts and behavior. Overall, we found partial support for a unidimensional view of SC, found that the scale overall is reliable across much of the continuum of SC, and found that it is highly related to hypersexuality as measured by the HDSI, though no potential cutoffs on the SCS correspond directly with the diagnostic criteria designed for use within the HDSI.
Confirmatory and exploratory factor analyses suggested that the scale had sufficient unidimensionality and local independence to proceed with IRT analyses. However, they also revealed substantial overlap in the content of items 1, 2, and 5 as well as items 4 and 6 that was above that expected of a scale measuring a single underlying construct. Moreover, although typical criteria used to judge the number of factors within the exploratory factor analysis suggested that a single factor was a reasonable fit to the data, model fit indices suggested that a three-factor model significantly improved overall model fit. Not surprisingly, the additional factors consisted of those items which showed evidence of residual correlation in the confirmatory factor analysis – a factor for items 1, 2, and 5 and another for items 4 and 6. While the other items on the scale deal with the general frequency or strength of sexual thoughts and behaviors, items 1, 2, and 5 deal with the extent to which they are leading to problems in one's life and items 4 and 6 deal with difficulties finding and maintaining sexual and romantic relationships as a result of one's sexual thoughts, feelings, and behaviors. These findings suggest the possibility that, were more items designed to tap into each of these distinct clusters, SC might be characterized by three dimensions: (1) frequent and intense sexual thoughts, feelings, and behaviors, (2) general problems and difficulties resulting from these thoughts, feelings, and behaviors, and (3) social, sexual, and intimacy problems and difficulties resulting from these thoughts, feelings, and behaviors. Although these three characteristics are common within SC conceptualizations, they have yet to be measured as distinct but related symptom clusters which, theoretically, all measure a common underlying trait of SC. Developing a scale that measures each of these with at least 3-4 items would allow for such an investigation.
Having determined that the SCS had sufficient unidimensionality for IRT analyses, we proceeded with treating it as such. In doing so, we found that the scale overall had very strong reliability – above a reliability of 0.9 across more than half of the continuum, and a reliability of at least 0.8 across all but one-tenth of the continuum. Despite these high reliability statistics for the scale as a whole, we found several items that performed poorly. Items 3, 4, and 9 did not perform as well as some of the others, but provided more precision and information at extreme low or high levels of SC than some of the better items, and thus added unique information to the overall scale. Items 6 and 7, however, performed poorly across the entire continuum of SC. Examining their content, this is somewhat unsurprising – item 6 asks about difficulty finding sex partners who desire sex as much as the participant wants and item 7 asks about whether participants think about sex while doing other things. It stands to reason that item 6 may have more to do with external forces rather than internal SC. Moreover, in this sample of highly sexually active GBM, it is not surprising that, unlike the other items, item 7 was highly skewed, with a majority of participants highly endorsing this item, and this most likely undermined its ability to provide useful information (though the item may very well provide information in a sample with lower overall levels of SC symptomology).
Finally, when examining its correspondence with the HDSI, we found that the continuous scores from each shared much in common and the theoretically related constructs of SC and hypersexuality had substantial overlap. However, when examining the SCS in relation to the diagnostic screening results of the HDSI, we found the opposite. Results indicated that there is no cutoff on the SCS that corresponds well (i.e., simultaneously maximizes its sensitivity, specificity, positive predictive value, and negative predictive value) with the screening results of the HDSI. One might think that the commonly used cutoff of 24 on the SCS to indicate problematic levels of SC might simply be too low to correspond with the more stringent criteria of the HDSI. However, we found that no matter how high the SCS score, there was no higher cutoff that corresponded substantially better with the HDSI. Rather, researchers would have to choose whether to maximize sensitivity or specificity should they want to use the SCS to predict HDSI screening results. The commonly used cutoff of 24 on the SCS – which was the 50th percentile in this sample – would produce a 7% rate of false-negatives, correctly “flagging” most probable cases for further screening, while also producing a 42% rate of false-positives. As such, the SCS might be a useful tool to provide a preliminary screening of people at high risk for meeting criteria on the HDSI, similar to screening tests utilized to identify individuals at risk for alcohol-use disorders or drinking problems prior to more extensive interviews or diagnostic evaluations.55,56 The SCS itself could not serve as a substitute for the HDSI and would incorrectly label a substantial number of individuals as hypersexual. It is worth considering the possibility that researchers and practitioners may wish to combine the results of the commonly used SCS cutoff of 24 with the diagnostic screening criteria for the HDSI, thus classifying individuals as negative on both (i.e., “non-hypersexual/non-SC”), positive on the SCS only (i.e., “at risk”), and positive on both the SCS and the HDSI (i.e., “problematic hypersexuality/SC”). Given the sensitivity of the cutoff of 24 on the SCS, it is unlikely that many individuals would trigger a positive screening result on the HDSI and not score above 24 on the SCS, and this may be particularly true among less sexually active samples. Future research is needed to determine the utility of such a three-category system of classification.
Limitations
Although this study had numerous strengths, including an at-risk sample of behaviorally similar men and a novel analytic approach that has rarely been used in the literature on SC, it was not without its limitations. Neither the SCS nor the HDSI were administered by a clinician in this study and, as such, both are subject to self-report biases and a lack of clinical decision-making. Moreover, the field lacks a relevant “gold standard” for diagnosing hypersexuality-related conditions, and as such, we relied on the HDSI as proposed for the DSM-5. Future research should examine the differences that result from treating each scale as a diagnostic, clinician-administered interview. This sample is also qualitatively different from other samples of GBM – although this is a strength of the study in many regards given that they are a sample most at risk for experiencing problems with SC and hypersexuality, it also limits the generalizability of these findings. For example, a score of 24 on the SCS has typically been found to be the 80-85th percentile in most samples, but it was 50th percentile in the current sample. As such, it is possible that scale responses and, thus, scale reliability would differ in less highly sexually active samples. Additionally, this sample of GBM was recruited in NYC and may be different from other samples and not representative of all GBM in the US.
Conclusions
Despite these limitations, our findings indicate that the SCS is a reliable measure for use in a non-treatment seeking sample of GBM who are highly sexually active. More work is needed to replicate the current findings with clinical and other community-based samples, including women and heterosexual men. Future research in this area could also benefit from examining whether the combined utility of both the SCS and the HDSI in classifying individuals into three groups that differentiate SC severity (i.e., non-hypersexual/non-SC; at-risk; and problematic hypersexuality/SC). Such research would allow more accurate estimates of the prevalence of each group and in distinguishing what psychiatric and substance use comorbidities 3,5,8,12,57 and other health risks that have been found to be associated with SC, such as HIV and other sexually transmitted infections (STIs),10,14,15,31,58-63 may exist among the groups. Finally, these data shed light on the cross-sectional association between these two scales but future research should carefully consider the development of both SC and HD over time to more carefully understand the ways in which these constructs develop and can best be measured.
Acknowledgements
This project was supported by a research grant from the National Institute of Mental Health (R01-MH087714; Jeffrey T. Parsons, Principal Investigator). H. Jonathon Rendina was supported in part by a National Institute of Mental Health Ruth L. Kirchstein Individual Predoctoral Fellowship (F31-MH095622). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to acknowledge the contributions of the Pillow Talk Research Team: John Pachankis, Ruben Jimenez, Demetria Cain, Sitaji Gurung, and Chris Cruz. We would also like to thank CHEST staff who played important roles in the implementation of the project: Chris Hietikko, Chloe Mirzayi, and Arjee Restar as well as our team of research assistants, recruiters, and interns. We would also like to thank Karon Cook for her guidance about the analyses for this paper. Finally, we thank Chris Ryan, Daniel Nardicio, and the participants who volunteered their time for this study.
References
- 1.Bancroft J, Vukadinovic Z. Sexual addiction, sexual compulsivity, sexual impulsivity, or what? Toward a theoretical model. Journal of Sex Research. 2004;41:225–234. doi: 10.1080/00224490409552230. [DOI] [PubMed] [Google Scholar]
- 2.Black DW. Compulsive Sexual Behavior: A Review. Journal of Practical Psychology and Behavioral Health. 1998;4:219–229. [Google Scholar]
- 3.Carnes PJ. Sexual Addiction and Compulsion: Recognition, Tretment, and Recovery. CNS Spectrums. 2000;5:63–72. doi: 10.1017/s1092852900007689. [DOI] [PubMed] [Google Scholar]
- 4.Goodman A. What's in a name? Terminology for designating a syndrome of driven sexual behavior. Sexual Addiction & Compulsivity. 2001;8:191–213. [Google Scholar]
- 5.Kafka MP. Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior. 2010;39(2):377–400. doi: 10.1007/s10508-009-9574-7. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan MS, Krueger RB. Diagnosis, assessment, and treatment of hypersexuality. Journal of Sex Research. 2010;47(2-3):181–198. doi: 10.1080/00224491003592863. [DOI] [PubMed] [Google Scholar]
- 7.Kuzma JM, Black DW. Epidemiology, prevalence, and natural history of compulsive sexual behavior. Psychiatr Clin North Am. 2008 Dec;31(4):603–611. doi: 10.1016/j.psc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Raymond NC, Coleman E, Miner MH. Psychiatric comorbidity and compulsive/impulsive traits in compulsive sexual behavior. Comprehensive Psychiatry. 2003;44:370–380. doi: 10.1016/S0010-440X(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 9.Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychology of Addictive Behaviors. 2010;24(3):487. doi: 10.1037/a0020527. [DOI] [PubMed] [Google Scholar]
- 10.Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior. 2010;39(4):940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: Validity, and predicting HIV risk behavior. Journal of personality assessment. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 12.Morgenstern J, Muench F, O'Leary A, et al. Non-paraphilic compulsive sexual behavior and psychiatric co-morbidities in gay and bisexual men. Sexual Addiction and Compulsivity. 2011;18:114–134. doi: 10.1080/10720162.2011.593420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muench F, Parsons JT. Sexual compulsivity and HIV: identification and treatment. Focus. 2004 Jul;19(6):1–5. [PubMed] [Google Scholar]
- 14.Parsons JT, Bimbi DS, Halkitis PN. Sexual compulsivity among gay/bisexual male escorts who advertise on the Internet. Sexual Addiction & Compulsivity. 2001;8:101–112. [Google Scholar]
- 15.Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. American Journal of Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Archives of Sexual Behavior. 2008;37(5):817–826. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- 17.Bancroft J, Graham CA, Janssen E, Sanders SA. The dual control model: Current status and future directions. Journal of Sex Research. 2009;46:121–142. doi: 10.1080/00224490902747222. [DOI] [PubMed] [Google Scholar]
- 18.Krueger RB, Kaplan MS. The paraphilic and hypersexual disorders. Journal of Psychiatric Practice. 2001;7:391–403. doi: 10.1097/00131746-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Coleman E. The obsessive–compulsive model for describing compulsive sexual behavior. American Journal of Preventive Psychiatry & Neurology. 1990;2:9–14. [Google Scholar]
- 20.Coleman E. Is your patient suffering from compulsive sexual behavior? Psychiatric Annals. 1992;22(6):320–325. [Google Scholar]
- 21.Barth RJ, Kinder BN. The mislabeling of sexual impulsivity. Journal of Sex and Marital Therapy. 1987;13:15–23. doi: 10.1080/00926238708403875. [DOI] [PubMed] [Google Scholar]
- 22.Mick TM, Hollander E. Impulsive–compulsive sexual behavior. CNS Spectrums. 2006;2006;11:944–955. doi: 10.1017/s1092852900015133. [DOI] [PubMed] [Google Scholar]
- 23.Hook JN, Hook JP, Davis DE, Worthington EL, Jr, Penberthy JK. Measuring sexual addiction and compulsivity: A critical review of instruments. Journal of Sex and Marital Therapy. 2010;36(3):227–260. doi: 10.1080/00926231003719673. [DOI] [PubMed] [Google Scholar]
- 24.Kalichman SC, Cain D. The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. Journal of Sex Research. 2004;41(3):235–241. doi: 10.1080/00224490409552231. [DOI] [PubMed] [Google Scholar]
- 25.Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994 Jun;62(3):385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- 26.Kalichman SC, Rompa D. The sexual compulsivity scale: Further development and use with HIV-Positive persons. Journal of Personality Assessment. 2001;76:379–395. doi: 10.1207/S15327752JPA7603_02. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association's DSM-5 Workgroup on Sexual and Gender Identity Disorders. [July 26, 2011];Hypersexual Disorder Screening Inventory. 2010 http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=415#.
- 28.Kafka MP. What Happened to Hypersexual Disorder? Archives of Sexual Behavior. 2014:1–3. doi: 10.1007/s10508-014-0326-y. [DOI] [PubMed] [Google Scholar]
- 29.Parsons JT, Rendina HJ, Ventuneac A, Cook KF, Grov C, Mustanski B. A Psychometric Investigation of the Hypersexual Disorder Screening Inventory among Highly Sexually Active Gay and Bisexual Men: An Item Response Theory Analysis. Journal of Sexual Medicine. 2013 Dec;10(12):3088–3101. doi: 10.1111/jsm.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelly BC, Bimbi DS, Nanín JE, Izienicki H, Parsons JT. Sexual compulsivity and sexual behaviors among gay and bisexual men and lesbian and bisexual women. Journal of Sex Research. 2009;46:1–8. doi: 10.1080/00224490802666225. [DOI] [PubMed] [Google Scholar]
- 31.Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV seropositive men who have sex with men: Prevalence and predictors of high-risk behaviors. Addictive Behaviors. 1999;24(6):857–868. doi: 10.1016/s0306-4603(99)00056-8. [DOI] [PubMed] [Google Scholar]
- 32.Cooper A, Delmonico DL, Burg R. Cybersex users, abusers, and compulsives: New findings and implications. Sexual Addiction & Compulsivity. 2000;7:5–29. [Google Scholar]
- 33.Hays RD, Morales LS, Reise SP. Item response theory and health outcomes measurement in the 21st Century. Medical care. 2000;38(Suppl. 9):1128–1142. doi: 10.1097/00005650-200009002-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reeve BB, Fayers P. Fayers P, Hays RD, editors. Applying item response theory modeling for evaluating questionnaire item and scale properties. Assessing Quality of Life in Clinical Trials. (2nd ed) 2005 [Google Scholar]
- 35.Neal DJ, Corbin WR, Fromme K. Measurement of alcohol-related consequences among high school and college students: Application of item response models to the rutgers alcohol problem index. Psychological Assesment. 2006;18(4):402–414. doi: 10.1037/1040-3590.18.4.402. [DOI] [PubMed] [Google Scholar]
- 36.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of cooccurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stall R, Paul JP, Greenwood G, et al. Alcohol use, drug use and alcohol related problems among men who have sex with men: the Urban Men's Health Study. Addiction. 2001;96(11):1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- 38.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: Reliability, validity, and predicting HIV risk behavior. Journal of Personality Assessment. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 39.Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and Sexual Compulsivity in a Community-Based Sample of HIV-Positive Gay and Bisexual Men. AIDS and Behavior. 2012;16(3):741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reid RC, Carpenter BN, Hook JN, et al. Report of findings in a DSM-5 field trial for hypersexual disorder. Journal of Sexual Medicine. 2012;9(11):2868–2877. doi: 10.1111/j.1743-6109.2012.02936.x. [DOI] [PubMed] [Google Scholar]
- 41.Amtmann D, Bamer AM, Cook KF, Askew RL, Noonan VK, Brockway JA. University of Washington self-efficacy scale: A new self-efficacy scale for people with disabilities. Archives of Physical Medicine and Rehabilitation. 2012 doi: 10.1016/j.apmr.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 42.Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 44.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- 45.Kline RB. Principles and practice of structural equation modeling. The Guilford Press; 2010. [Google Scholar]
- 46.Reise SP, Haviland MG. Item response theory and the measurement of clinical change. Journal of Personality Assessment. 2005;84(3):228–238. doi: 10.1207/s15327752jpa8403_02. [DOI] [PubMed] [Google Scholar]
- 47.West SG, Finch JF, Curran PJ. Structural equation models with nonnormal variables: Problems and remedies. 1995 [Google Scholar]
- 48.Yu CY. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. University of California; Los Angeles: 2002. [Google Scholar]
- 49.Wang J, Wang X. Structural equation modeling: Applications using Mplus. Wiley; West Sussex, UK: 2012. [Google Scholar]
- 50.Reeve BB, Hays RD, Bjorner JB, et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical care. 2007;45(5):S22. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 51.Muthén LK, Muthén BO. Mplus user's guide. 7th Ed. Muthén & Muthén; Los Angeles, CA: 1998-2012. [Google Scholar]
- 52.Samejima F. Estimation of latent ability using a response pattern of graded scores. Psychometrika Monograph Supplement. 1969 [Google Scholar]
- 53.IRTPRO [computer program]. Version 2.1. Scientific Software International, Inc.; Skokie, IL: [Google Scholar]
- 54.Chen WH, Thissen D. Local dependence indexes for item pairs using item response theory. Journal of Educational and Behavioral Statistics. 1997;22(3):265–289. [Google Scholar]
- 55.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test. Guidelines for use in primary care. 2nd ed. World Health Organization; Geneva: 2001. [Google Scholar]
- 56.Stewart SH, Connors GJ. Screening for alcohol problems: What makes a test effective? Alcohol Research & Health. 2004/2005;28(1):5–16. [PMC free article] [PubMed] [Google Scholar]
- 57.Black DW, Kehrberg LLD, Flumerfelt DL, Schlosser SS. Characteristics of 36 subjects reporting compulsive sexual behavior. American Journal of Psychiatry. 1997;154(2):243–249. doi: 10.1176/ajp.154.2.243. [DOI] [PubMed] [Google Scholar]
- 58.Dodge B, Reece M, Cole SL, Sandfort TGM. Sexual compulsivity among heterosexual college students. Journal of Sex Research. 2004;41(4):343–350. doi: 10.1080/00224490409552241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dodge B, Reece M, Herbenick D, Fisher C, Satinsky S, Stupiansky N. Relations Between Sexually Transmitted Infection Diagnosis and Sexual Compulsivity in a Community-Based Sample of Men Who Have Sex with Men (MSM). Sex Transm Infect. 2007 Dec 20; doi: 10.1136/sti.2007.028696. [DOI] [PubMed] [Google Scholar]
- 60.Kalichman SC, Greenberg J, Abel GG. HIV-seropositive men who engage in high risk sexual behavior. Psychological characteristics and implications for prevention. AIDS Care. 1997;9(4):441–540. doi: 10.1080/09540129750124984. [DOI] [PubMed] [Google Scholar]
- 61.O'Leary A, Wolitski RJ, Remien RH, et al. Psychosocial correlates of transmission risk behavior among HIV-seropositive gay and bisexual men. AIDS. 2005;19:1–9. doi: 10.1097/01.aids.0000167353.02289.b9. [DOI] [PubMed] [Google Scholar]
- 62.Reece M. Sexual compulsivity and HIV serostatus disclosure among men who have sex with men. Sexual Addiction and Compulsivity. 2003;10:1–11. [Google Scholar]
- 63.Reece M, Plate PL, Daughtry M. HIV prevention and sexual compulsivity: The need for an integrated strategy of public health and mental health. Sexual Addiction & Compulsivity. 2001;8(2):157–167. [Google Scholar]