Abstract
Despite the co-occurrence and clinically significant relation between trauma exposure and smoking, there is little understanding of the mechanisms underlying the posttraumatic stress symptoms-smoking relation. The present study examined whether dysphoria (i.e., a psychopathologic symptom dimension that reflects depression’s core affective, cognitive, and psychomotor features) accounted for the covariance between posttraumatic stress symptom severity and an array of smoking processes among trauma-exposed daily smokers. Participants (n = 189; 47.6% female; Mage = 41.15; SD = 12.47) were trauma-exposed, treatment-seeking daily cigarette smokers who completed measures of posttraumatic stress symptom severity, dysphoria, and four cognitive-based smoking processes that interfere with smoking cessation: avoidance/inflexibility to smoking, perceived barriers to smoking cessation, negative affect reduction motivation for smoking, and negative affect reduction/negative reinforcement expectancies from smoking. Dysphoria indirectly and significantly accounted for the relation between posttraumatic stress symptom severity and smoking outcomes. The present results provide initial empirical support that dysphoria accounts for the covariance between posttraumatic symptom severity and a variety of clinically-relevant smoking variables in trauma-exposed, treatment-seeking smokers. The findings suggest the potential importance of targeting dysphoria during smoking cessation among trauma-exposed individuals.
Keywords: Posttraumatic Stress, Tobacco, Depression, Dysphoria, Trauma
Trauma exposure is alarmingly high among the general population (Breslau et al., 2003; Frans, et al., 2005). The majority of trauma-exposed individuals recover from the traumatic event exposure, but a small subset fail to do so and develop posttraumatic stress disorder (PTSD; Breslau et al., 2003). Trauma-exposed individuals without PTSD are not at as high of risk for drug abuse or dependence as those who develop PTSD (Breslau et al., 2003). Yet, trauma-exposed persons are at a greater risk for developing nicotine dependence relative to non-trauma exposed persons. Compared to individuals not exposed to a traumatic event, trauma-exposed individuals (with or without PTSD) are more likely to be smokers, tend to smoke more heavily, have higher levels of nicotine dependence, and show poorer outcomes during quit attempts (Feldner et al., 2007; Zvolensky et al., 2008). Trauma-exposed smokers are also particularly motivated to smoke to reduce negative affect and expect that smoking will reduce negative affect (Calhoun et al., 2011), perhaps owing to the fact that smoking appears to temporarily relieve distress among such persons (Beckham et al., 2005). Moreover, a cross-sectional study found that greater smoking rates and higher levels of nicotine dependence are related to PTSD and increased PTSD symptom severity (Beckham et al., 1997). Despite the documented co-occurrence and clinically significant relations between trauma exposure and smoking, there is little understanding of the mechanisms underlying the posttraumatic stress symptoms-smoking relation.
Depression may be one common, affect-relevant mechanism linking posttraumatic stress symptom severity and smoking. Moderate to severe levels of depressive symptoms prior to smoking cessation treatment are frequently associated with poorer cessation outcomes (Cinciripini et al., 2003; Niaura & Abrams, 2001). Some work suggests that dysphoria, a within-symptom cluster of depression, may be more related to smoking maintenance and relapse than other depressive symptoms (Leventhal et al., 2011). Greater dysphoria is also linked to higher rates of smoking over time (Helstrom et al., 2009), and smokers who endorse greater dysphoria are more vulnerable to dependent smoking and relapse as a means to attenuate dysphoria-related symptoms (Leventhal et al., 2011).
Depressive symptoms also often co-occur with PTSD (Kessler et al., 1995). For example, an extensive literature on early childhood trauma suggests that early exposure to stress is related to later symptoms of depression (Heim et al., 2008). Moreover, those who developed PTSD are at a markedly increased risk for major depression (Breslau et al., 2003). Trauma-exposed individuals without PTSD, however, were not at an increased risk for the onset of major depression. Indeed, recent work has linked posttraumatic stress symptom severity and dysphoria (Bernstein et al., 2011). Theoretically, among trauma-exposed smokers, dysphoria may contribute to perceived challenges in quitting smoking and mood-management, smoking motivation, and cognition. That is, among trauma-exposed smokers with posttraumatic stress symptoms, increased levels of dysphoria and negative cognition may contribute to greater (a) perceived obstacles to smoking cessation and (b) perceived mood regulation benefits of smoking. Thus, dysphoria may, at least partially, explain the association between posttraumatic stress and factors that contribute to poor smoking cessation outcomes.
Confirmatory factor analyses have identified dysphoria, intrusion, avoidance, and hyperarousal as defining symptom clusters of PTSD (Simms et al., 2002). These distinct clusters correlate differently with other psychiatric disorders. For example, the dysphoria cluster represents symptoms that are similar across depression and anxiety disorders, whereas the intrusion cluster includes phenotypically different symptoms across disorders (Simms et al., 2002). Recent work found greater endorsement of dysphoric symptoms, as assessed by an emotional numbing factor of PTSD, related to being a heavy smoker versus a nonsmoker (Cook et al., 2009). These data suggest exploring components of PTSD symptomology among a trauma-exposed population may offer unique insights into the posttraumatic stress symptoms-smoking comorbidity. Although research links posttraumatic stress symptoms, dysphoria, and smoking, no research has explored the explanatory value of dysphoria in the relation between PTSD symptom clusters (i.e., intrusion, avoidance, or hyperarousal) and cognitive-based smoking processes. This represents a clinically noteworthy gap in the literature given the important role cognitive-based processes play in addiction and mental health.
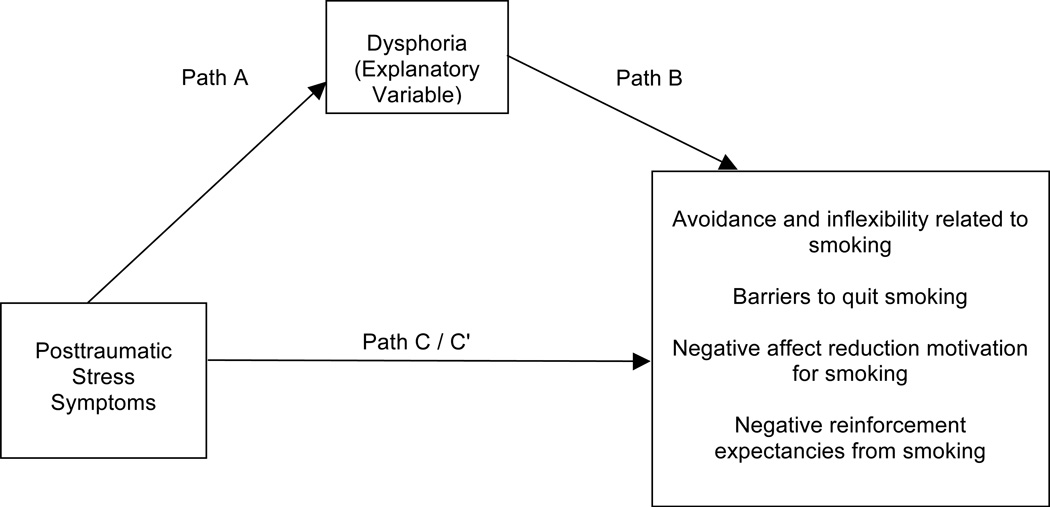
Taken together, the present study examined the potential explanatory role of dysphoria regarding the relation between posttraumatic stress symptom severity, only including items that load on the intrusion, avoidance, or hyperarousal factors, and cognitive-based smoking processes of smoking, including (1) the tendency to respond with avoidance/inflexibility in the presence of aversive smoking-related thoughts, feelings, or internal sensations; (2) perceived barriers to smoking cessation; (3) negative affect reduction motivation for smoking; and (4) negative affect reduction/negative reinforcement expectancies from smoking (see Figure 1). We hypothesized that dysphoria would explain the relation between posttraumatic symptom severity and these smoking processes, and that these effects would not be explained by gender, the trait-like propensity to experience negative affect, and time since traumatic event.
Figure 1.
Proposed model: Dysphoria as a potential explanatory variable of the association between intrusion, avoidance, and hyperarousal posttraumatic stress symptoms and cognitive-based processes of smoking.
METHODS
Participants
The sample consisted of 189 treatment-seeking, trauma-exposed, adult daily smokers (47.6% female; Mage = 41.15; SD = 12.47) who endorsed at least one lifetime Criterion A traumatic event according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000). Only participants who reported smoking at least 8 cigarettes a day during the past year, as indexed by the Smoking History Questionnaire (Brown et al., 2002), were included. Exclusion criteria included suicidality and psychosis. Participants were primarily White (88.4%) adults, and married or living with someone (42.9%) or never married (32.8%). Nearly one-third (31.2%) of participants completed some college and 45.5% met criteria for at least one current (past year) psychological disorder. Participants reported an average daily smoking rate of 18.8 (SD = 8.97) cigarettes per day and daily smoking for an average of 23.0 years (SD = 12.69). The majority (67.2%) of participants reported that the traumatic event occurred more than 5 years ago.
Measures
Primary Predictors
Posttraumatic Diagnostic Scale (PDS)
The PDS (Foa, 1995) is a 49-item self-report instrument that assesses trauma exposure and the presence of posttraumatic stress symptoms based on DSM-IV criteria (American Psychiatric Association, 2000). Respondents report if they have experienced any of 13 traumatic events (e.g., “natural disaster“, “sexual or non sexual assault by a stranger”), including an “other” category, and then indicate which event was most disturbing. Participants report how long ago the traumatic event occurred on a 6-point scale from 1 “Less than one month [ago]” to 6 “More than 5 years [ago].” In the current study, only those participants indicating that they experienced, witnessed, or were confronted with a traumatic event that involved actual or threatened death or serious injury that was accompanied by a feeling of helplessness and terror (i.e., met DSM-IV-TR defined criterion A trauma; American Psychiatric Association, 2000) were included. The PDS also assesses the past-month frequency of the 17 DSM-IV-TR symptoms of PTSD for the most disturbing event endorsed from 0 “not at all/only once” to 3 “5 or more times a week/almost always.” For the present study, two summary scores were created. The first score (PDS-IAH) was the sum of items that load on the intrusion, avoidance, or hyperarousal symptom clusters in a four-factor confirmatory factor analysis (see Simms et al., 2002; Yufik & Simms, 2010); items that load on the dysphoria system cluster were excluded. The PDS-IAH included 9 items (i.e., items 22-28, 37, and 38). The second score (PDS-total) was the sum of all 17 items. The PDS has evidenced excellent psychometric properties (Foa et al., 1997), including high internal consistency (alpha = .92) and high test-retest reliability (kappa = .74). The PDS demonstrated excellent internal consistency (PDS-IAH: Cronbach's alpha .88; PDS-total: Cronbach's alpha .93).
Inventory of Depression and Anxiety Symptoms (IDAS)
The IDAS (Watson et al., 2007) is a 64-item self-report instrument that assesses distinct affect symptom dimensions within the past two weeks. Items are answered on a 5-point Likert scale ranging from “not at all” to “extremely.” The IDAS subscales show strong internal consistency, convergent and discriminant validity with psychiatric diagnoses and self-report measures; and short-term retest reliability (r = 0.79) with both community, and psychiatric patient samples (Watson et al., 2007). The present study used the dysphoria subscale (e.g. ‘‘I felt depressed;’’ 10 items). The dysphoria subscale demonstrated excellent internal consistency in the current sample (Cronbach’s alpha = .93).
Outcomes
Avoidance and Inflexibility Scale (AIS)
The AIS assesses avoidance and inflexibility related to smoking (Gifford & Lillis, 2009) on a Likert-type scale ranging from 1 “not at all” to 5 “very much.” Participants respond to 13 items, such as “How likely is it that these feelings will lead you to smoke?” and “To what degree must you reduce how often you have these thoughts in order not to smoke.” The AIS has demonstrated good internal consistency (Gifford & Lillis, 2009). Higher scores represent more smoking-based avoidance or inflexibility in the presence of uncomfortable or difficult sensations or thoughts, whereas lower scores suggest more ability to accept difficult feelings or thoughts without allowing them to trigger smoking. In the present study, the total score was used and the scale demonstrated high internal consistency (Cronbach’s alpha = .93).
Barriers to Cessation Scale (BCS)
The BCS assesses barriers associated with smoking cessation (Macnee & Talsma, 1995). Participants report the extent to which they identify with 19-items according to a 4-point Likert-type scale (0 = “not a barrier” to 3 = “large barrier”). Researchers report good internal consistency regarding the total score, and good content and predictive validity of the measure (Macnee & Talsma, 1995). As with previous research, the total score summary statistic was utilized. This scale demonstrated high internal consistency (Cronbach’s alpha = .89).
Reasons for Smoking (RFS)
The RFS assesses smoking motives (Ikard et al., 1969). The psychometric properties of this scale have been well-established (Shiffman, 1993). The version of the RFS used consisted of 23 items and items are rated on a 1 (“never”) to 5 (“always”) scale. Previous research lends support for a unique relation among psychological vulnerabilities and the RFS-Negative Affect Reduction (RFS-NA; 6 items) subscale (Brown et al., 2001); thus, we utilized the RFS-NA subscale in this study, which demonstrated high levels of internal consistency (Cronbach’s alpha = .89).
Smoking Consequences Questionnaire (SCQ)
The SCQ (Brandon & Baker, 1991) is a 50-item self-report measure that assesses tobacco use outcome expectancies believed to underlie smoking motivation on a Likert-type scale, ranging from 0 (“completely unlikely”) to 9 (“completely likely”). Based on previous research (Gonzalez et al., 2009), we utilized the SCQ-Negative Reinforcement/Negative Affect Reduction subscale (SCQ-NR; 12 items). The SCQ-NR demonstrated high internal consistency (Cronbach’s alpha = .92).
Additional Measures used as Covariates or Sample Descriptors
Demographics Questionnaire
Demographic information collected included gender, age, race, educational level, and marital status.
Smoking History Questionnaire (SHQ)
The SHQ assesses smoking rate, years of daily smoking, number of years a daily smoker, and other characteristics (Brown et al., 2002). To describe the sample, smoking rate was obtained from the question, “Since you started regular daily smoking, what is the average number of cigarettes you smoked per day?” Number of years a daily smoker was also derived from this questionnaire.
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-I/NP)
Diagnostic assessments of past year Axis I psychopathology were conducted using the SCID-I/NP (First et al., 1994). All SCID-I/NP interviews were administered by trained research assistants or doctoral level staff and supervised by independent doctoral-level professionals. Interviews were audio-taped and the reliability of a random selection of 12.5% of interviews was checked (MJZ) for accuracy; no cases of (diagnostic coding) disagreement were noted.
Positive and Negative Affect Scale (PANAS)
The PANAS (Watson et al., 1988) is a self-report measure that requires participants to rate the extent to which they experience 20 different feelings and emotions (e.g., nervous, interested) based on a Likert scale ranging from 1 (“very slightly or not at all”) to 5 (“extremely”). The measure yields two factors, negative and positive affect, and has strong documented psychometric properties (Watson et al., 1988). The PANAS negative affectivity subscale (PANAS-NA; 10 items) was utilized in the present study. The PANAS-NA internal consistency was excellent (Cronbach’s alpha = .92).
Procedure
A community sample of adult daily smokers was recruited to participate in a randomized controlled dual-site clinical trial examining the efficacy of two smoking cessation interventions. Individuals responding to study advertisements were scheduled for an in-person, baseline assessment to evaluate study inclusion and exclusion criteria. After providing written informed consent, participants completed an interview and a computerized battery of self-report questionnaires. The Institutional Review Board at each study site approved the study protocol and all study procedures were conducted in compliance with ethical standards of the American Psychological Association. The current cross-sectional study is based on secondary analyses of baseline (pre-treatment) data for a subset of the sample.
Analytic Strategy
First, outliers and descriptive data were examined. Second, analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). Bootstrapping is the recommended approach when data distribution is nonnormal or unknown (Kelley, 2005; Kirby & Gerlanc, 2013); thus, nonnormality was not a principal concern. Models included PDS-IAH as the predictor and dysphoria as the explanatory variable. Based on previous research (see Gonzalez et al., 2008; Zvolensky et al., 2007), relevant variables that also correlated with study variables were entered as covariates, and included gender, PANAS-NA, and time since trauma. Four independent models were run with AIS (Model 1), BCS (Model 2), RFS-NA (Model 3), and SCQ-NR (Model 4) as criterion variables. See Figure 1. All models were subjected to 10,000 bootstrap re-samplings and a 95-percentile confidence interval (CI) was estimated (see Hayes, 2009; Preacher & Hayes, 2004, 2008). Finally, we performed analyses reversing PDS-IAH and dysphoria to further strengthen results (Preacher & Hayes, 2004). Given the cross-sectional nature of the study, we included these analyses to disprove alternative hypotheses and to further lend support to the explanatory priority of PDS-IAH and dysphoria. Finally, to further strengthen interpretation of results, all models and reverse models were run using PDS-total.
Results
Descriptive Analyses
No outliers were observed and four cases were removed due to missing data; thus, 189 cases comprised the sample included in the analyses. The removal of these cases did not influence the overall pattern or statistical significance of the results. Means, standard deviations, and bivariate correlations are presented in Table 1.
Table 1.
Descriptive statistics and correlations for study variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gendera | -- | ||||||||
| 2. PANAS-NAa | 0.17* | -- | |||||||
| 3. Time Since Traumaa | −0.07 | −0.16* | -- | ||||||
| 4. PDS-IAHb | 0.21** | 0.48*** | −0.16* | -- | |||||
| 5. IDAS-Dysphoriac | 0.16* | 0.79*** | −0.09 | 0.49*** | -- | ||||
| 6. Avoidance & Inflexibilityd | 0.20** | 0.24** | 0.10 | 0.12 | 0.34*** | -- | |||
| 7. Barriers to Cessationd | 0.23** | 0.31*** | −0.05 | 0.21** | 0.46*** | 0.61*** | -- | ||
| 8. RFS-Negative Affectd | 0.30*** | 0.45*** | −0.10 | 0.33*** | 0.51*** | 0.54*** | 0.56*** | -- | |
| 9. SCQ-Negative Reinforcementd | 0.21** | 0.40*** | −0.10 | 0.22** | 0.42*** | 0.48*** | 0.56*** | 0.72*** | -- |
| Mean (or %) | 47.6% | 19.06 | 5.40 | 4.61 | 19.67 | 46.12 | 24.52 | 3.51 | 5.91 |
| Standard Deviation | -- | 7.57 | 0.98 | 5.36 | 8.29 | 10.77 | 11.07 | 0.79 | 1.67 |
Note. N = 189
p < .001,
p < .01,
p < .05.
Covariates;
Predictor;
Explanatory Variable;
Criterion Variables
Gender = % listed as females (coded 1 = male; 2 = female); PANAS-NA = Positive and Negative Affect Scale-Negative Affect subscale; PDS-IAH = Posttraumatic Diagnostic Scale (including Intrusion, Avoidance, and Hyperarousal symptom clusters); RFS = Reasons for Smoking; SCQ = Smoking Consequences Questionnaire.
Main Analyses
Regression results for paths a, b, c, and c’ are presented in Table 2. Model 1 with AIS as the criterion revealed a significant total effect model (R2 = .104, F[4, 184] = 5.356, p < .001) with PDS-IAH as the predictor and all covariates entered. The model was significant after adding dysphoria and accounted for greater variance (R2 = .163, F[5, 183] = 7.145, p < .001). The direct effect of PDS-IAH on AIS after entering dysphoria was non-significant. Regarding the test of the indirect effect, higher rating of PDS-IAH predicted greater AIS indirectly through dysphoria (effect a*b).
Table 2.
Results from regression models
| Y | Model | b | SE | t | p | CI (lower) | CI (upper) |
|---|---|---|---|---|---|---|---|
| 1 | PDS-IAH → IDAS (a) | .218 | .079 | 2.764 | .006 | .062 | .373 |
| IDAS → AIS (b) | .529 | .147 | 3.593 | < .001 | .239 | .820 | |
| PDS-IAH → AIS (c’) | −.138 | .161 | −0.858 | .392 | −.455 | .179 | |
| PDS-IAH → AIS (c) | −.023 | .162 | −0.139 | .889 | −.343 | .298 | |
| PDS-IAH → IDAS → AIS (a*b) | .115 | .057 | .028 | .264 | |||
| 2 | IDAS → BCS (b) | .605 | .144 | 4.198 | < .001 | .321 | .890 |
| PDS-IAH → BCS (c’) | −.107 | .157 | −0.683 | .495 | −.418 | .203 | |
| PDS-IAH → BCS (c) | .024 | .161 | 0.151 | .880 | −.293 | .342 | |
| PDS-IAH → IDAS → BCS (a*b) | .132 | .066 | .029 | .298 | |||
| 3 | IDAS → RFS-NA (b) | .037 | .010 | 3.805 | < .001 | .018 | .057 |
| PDS-IAH → RFS-NA (c’) | .008 | .011 | 0.724 | .470 | −.013 | .029 | |
| PDS-IAH → RFS-NA (c) | .016 | .011 | 1.461 | .146 | −.001 | .037 | |
| PDS-IAH → IDAS → RFS-NA (a*b) | .008 | .004 | .002 | .018 | |||
| 4 | IDAS → SCQ-NR (b) | .057 | .022 | 2.570 | .011 | .013 | .101 |
| PDS-IAH → SCQ-NR (c’) | −.013 | .024 | −0.531 | .596 | −.060 | .035 | |
| PDS-IAH → SCQ-NR (c) | < .001 | .024 | −0.018 | .986 | −.048 | .047 | |
| PDS-IAH → IDAS → SCQ-NR (a*b) | .012 | .007 | .003 | .030 | |||
Note. Path a is equal across all models; therefore, it presented only in the model with Y1 to avoid redundancies. N for analyses of models Y1-Y4 included 189 cases. The standard error and 95% CI for a*b are obtained by bootstrap with 10,000 re-samples. PDS-IAH (posttraumatic stress symptom severity [including Intrusion, Avoidance, and Hyperarousal symptom clusters]) is the predictor, IDAS (dysphoria subscale of IDAS measure) is the explanatory variable, and AIS (avoidance and inflexibility to smoking; Y1), BCS (barriers to smoking cessation; Y2), RFS-NA (reasons for smoking for negative affect reduction; Y3), and SCQ-NR (smoking expectancies for negative affect reduction; Y4) are the outcome variables. CI (lower) = lower bound of a 95% confidence interval; CI (upper) = upper bound; → = affects.
Model 2 with BCS as the criterion revealed a significant total effect model (R2 = .168, F[4, 184] = 9.305, p < .001) with PDS-IAH as the predictor and all covariates entered. The model was significant after adding dysphoria and accounted for greater variance (R2 = .241, F[5, 183] = 11.641, p < .001). The direct effect of PDS-IAH on BCS after entering dysphoria was non-significant. Regarding the test of the indirect effect, higher rating of PDS-IAH predicted greater BCS indirectly through dysphoria (effect a*b).
Model 3 with RFS-NA as the criterion revealed a significant total effect model (R2 = .260, F[4, 184] = 16.122, p < .001) with PDS-IAH as the predictor and all covariates entered. The model was significant after adding dysphoria and accounted for greater variance (R2 = .314, F[5, 183] = 16.737, p < .001). The direct effect of PDS-IAH on RFS-NA after entering dysphoria was non-significant. Regarding the test of the indirect effect, higher rating of PDS-IAH predicted greater RFS-NA indirectly through dysphoria (effect a*b).
Model 4 with SCQ-NR as the criterion revealed a significant total effect model (R2 = .184, F[4, 184] = 10.399, p < .001) with PDS-IAH as the predictor and all covariates entered. The model was significant after adding dysphoria and accounted for greater variance (R2 = .213, F[5, 183] = 9.893, p < .001). The direct effect of PDS-IAH on SCQ-NR after entering dysphoria was non-significant. Regarding the test of the indirect effect, higher rating of PDS-IAH predicted greater SCQ-NR indirectly through dysphoria (effect a*b).
Specificity Analyses
To further strengthen interpretation of results, the proposed predictor (PDS-IAH) and potential explanatory (dysphoria) variables were reversed for each of the four models tested previously. Tests of the indirect effects in these models were estimated based on 10,000 bootstrap re-samples and all results of the reversed models were non-significant.
Finally, PDS-total indirectly related to AIS (b = .108, CI95% = .034, .219), BCS (b = .122, CI95% = .042, .249), RFS-NA (b = .008, CI95% = .003, .015), and SCQ-NR (b = .012, CI95% = .004, .027) through dysphoria. Thus, the overall main findings did not differ when models were explored with PDS-total. All reverse models were non-significant.
Discussion
Posttraumatic stress symptom severity (i.e., intrusion, avoidance, or hyperarousal symptom clusters) was significantly related to the tendency to respond with inflexibility/avoidance in the presence of aversive smoking-related thoughts, feelings, or internal sensations, perceived barriers to smoking cessation, negative affect reduction motivation for smoking, and negative affect reduction/negative reinforcement expectancies from smoking through dysphoria. The observed effects were evident above and beyond the variance accounted for by gender, negative affectivity, and time since trauma. Results indicated that dysphoria at least partially explained the relation between posttraumatic stress symptom severity and the criterion variables. Although the present research design does not permit explication of the temporal ordering of the observed associations, we attempted to improve confidence in the observations by evaluating an alternative model in which the predictors (PDS-IAH and dysphoria) were reversed. All models emerged as non-significant, indicating that the studied smoking variables are not solely a set of 'interrelated constructs.' Rather, these variables may operate as part of a directional pathway leading from posttraumatic stress symptom severity to dysphoria to smoking processes. Additionally, we explored whether the inclusion of dysphoria items on the posttraumatic stress symptom severity measure would influence results. The inclusion of these items did not yield different results than when the items were excluded.
Clinically, the present findings suggest that it may be advisable to address dysphoria among trauma-exposed smokers seeking smoking cessation treatment. While additionally research is needed, it may be that smoking cessation programs for trauma-exposed individuals that incorporate depression management education and therapeutic training are more efficacious over standard smoking cessation programs. Although addressing PTSD may yield positive results for trauma-exposed smokers who seek clinical services, some trauma-exposed smokers may benefit by targeting dysphoric symptoms to facilitate changes in smoking processes. Thus, depression-oriented interventions may be a useful compliment or supplementary intervention tactic for trauma-exposed smokers, particularly those who may be less apt to 'engage' with therapeutic tactics oriented fully on PTSD symptoms.
There are a number of study limitations. First, the temporal relation between posttraumatic stress and dysphoria is unclear. The cross-sectional nature of the study design did not allow for testing of temporal sequencing. Based on the present results, future prospective studies are necessary to determine directional effects of these relations. Second, our sample consisted of primarily White, community-recruited, treatment-seeking, trauma-exposed daily cigarette smokers with a moderate smoking rate. This limitation restricts the generalizability of findings. Future studies may benefit by sampling ethnically diverse, lighter and heavier smokers to ensure the generalizability of the results to the general smoking population. Third, the current study relied on self-report measures. Future research could benefit by utilizing multi-method approaches and minimizing the role of method variance in the observed relations. Fourth, creating a summary score for PDS without including the dysphoria subscale may make it difficult to know exactly what was measured and how it applies to understanding the clinical presentation of PTSD. Although additional analyses explored the models utilizing the entire construct, future researchers should consider exploring explanatory pathways between each PTSD symptom clusters and cognitive-based processes of smoking. Finally, we did not have sufficient data to complete analyses on smokers with PTSD; thus, the degree to which study findings are specifically applicable to treatment seeking individuals with PTSD is uncertain. To further gauge the clinical significance of the current findings for smokers with PTSD, it would be important for future work to replicate this model with smokers who have PTSD.
Conclusions
Overall, the present study serves as an initial investigation into the nature of the association among posttraumatic stress, dysphoria, and a relatively wide range of clinically significant smoking processes with adult treatment-seeking, trauma-exposed smokers. The findings of the current study are a first step in informing possible underlying variables that may link intrusion, avoidance, and hyperarousal symptoms and cognitive process of smoking. Future work is needed to better understand the extent to which trauma-exposed smokers with symptoms of posttraumatic stress may benefit from addressing dysphoria during a smoking cessation program.
Acknowledgments
Grant Support: This work was supported by a National Institutes of Health (NIH) grant awarded to Drs. Michael J. Zvolensky and Norman B. Schmidt (R01-MH076629-01A1). Dr. Vujanovic acknowledges the support of a NIH/University of Texas Clinical and Translational Science Career Development Award (K12TR000370-07).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR®. Arlington, VA: American Psychiatric Publishing; 2000. [Google Scholar]
- Beckham JC, Feldman ME, Vrana SR, et al. Immediate antecedents of cigarette smoking in smokers with and without posttraumatic stress disorder: A preliminary study. Exp Clin Psychopharmacol. 2005;13(3):219. doi: 10.1037/1064-1297.13.3.219. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Kirby AC, Feldman ME, et al. Prevalence and correlates of heavy smoking in Vietnam veterans with chronic posttraumatic stress disorder. Addict Behav. 1997;22(5):637–647. doi: 10.1016/s0306-4603(96)00071-8. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Tanay G, Vujanovic AA. Concurrent relations between mindful attention and awareness and psychopathology among trauma-exposed adults: Preliminary evidence of transdiagnostic resilience. Journal of Cognitive Psychotherapy. 2011;25(2):99–113. [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. J Consult Clin Psychol. 1991;3(3):484. [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry. 2003;60(3):289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez C, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addict Behav. 2001;26(6):887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111(1):180. [PubMed] [Google Scholar]
- Calhoun PS, Levin HF, Dedert EA, Johnson Y, Beckham JC. The relationship between posttraumatic stress disorder and smoking outcome expectancies among US military veterans who served since September 11, 2001. J Trauma Stress. 2011;24(3):303–308. doi: 10.1002/jts.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinciripini PM, Wetter DW, Fouladi RT, et al. The effects of depressed mood on smoking cessation: mediation by postcessation self-efficacy. J Consult Clin Psychol. 2003;71(2):292. doi: 10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- Cook J, Jakupcak M, Rosenheck R, Fontana A, McFall M. Influence of PTSD symptom clusters on smoking status among help-seeking Iraq and Afghanistan veterans. Nicotine Tob Res. 2009;11:1189–1195. doi: 10.1093/ntr/ntp123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clin Psychol Rev. 2007;27(1):14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders - Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- Foa EB. Post-traumatic Stress Diagnostic Scale (PDS) Minneapolis: National Computer Systems. 1995 [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445. [Google Scholar]
- Frans Ö, Rimmö PA, Åberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatrica Scandinavica. 2005;111(4):291–290. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Lillis J. Avoidance and inflexibility as a common clinical pathway in obesity and smoking treatment. J Health Psychol. 2009;14(7):992–996. doi: 10.1177/1359105309342304. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Vujanovic AA, Johnson KA, Leyro TM, Zvolensky MJ. The role of mindful attention in regard to the relation between negative affect reduction outcome expectancies and emotional vulnerability among adult cigarette smokers. Cognitive Therapy and Research. 2009;33(6):645–656. doi: 10.1007/s10608-009-9246-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. J Psychiatr Res. 2008;43(2):138–147. doi: 10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. Methodology in the social sciences. New York, NY: The Guilford Press; 2013. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33(6):693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Helstrom AW, Bell ME, Pineles SL. Feeling better and smoking less: The relationship between trauma symptoms and smoking over time. Cognitive Therapy and Research. 2009;33(2):235–240. [Google Scholar]
- Ikard FF, Green DE, Horn D. A scale to differentiate between types of smoking as related to the management of affect. Substance Use & Misuse. 1969;4(4):649–659. [Google Scholar]
- Kelley K. The effects of nonnormal distributions on confidence intervals around the standardized mean difference: Bootstrap and parametric confidence intervals. Educational and Psychological Measurement. 2005;65(1):51–69. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Gerlanc D. BootES: An R package for bootstrap confidence intervals on effect sizes. Behavior Research Methods. 2013;45(4):905–927. doi: 10.3758/s13428-013-0330-5. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ, Schmidt NB. Smoking-related correlates of depressive symptom dimensions in treatment-seeking smokers. Nicotine Tob Res. 2011;13(8):668–676. doi: 10.1093/ntr/ntr056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macnee CL, Talsma A. Development and testing of the barriers to cessation scale. Nurs Res. 1995;44(4):214–219. [PubMed] [Google Scholar]
- Niaura R, Abrams DB. Stopping smoking: a hazard for people with a history of major depression? The Lancet. 2001;357(9272):1900–1901. doi: 10.1016/S0140-6736(00)05089-3. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Smoking cessation treatment: Any progress? J Consult Clin Psychol. 1993;61(5):718. doi: 10.1037//0022-006x.61.5.718. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbelling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. J Abnorm Psychol. 2002;111(4):637. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, O'Hara MW, Simms LJ, et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychol Assess. 2007;19(3):253. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. J Abnorm Psychol. 2010;119(4):764. doi: 10.1037/a0020981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Gibson LE, Vujanovic AA, et al. Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine Tob Res. 2008;10(8):1415–1427. doi: 10.1080/14622200802238951. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Miller MOB, et al. Incremental validity of anxiety sensitivity in terms of motivation to quit, reasons for quitting, and barriers to quitting among community-recruited daily smokers. Nicotine Tob Res. 2007;9(9):965–975. doi: 10.1080/14622200701540812. [DOI] [PubMed] [Google Scholar]