Abstract
Problem
Physician scientists play a critical role in discovering new biological knowledge and translating their findings into medical practices that can improve clinical outcomes. Collectively, the National Institutes of Health (NIH) and its affiliated Medical Scientist Training Programs (MSTPs) invest upwards of $500,000 to fully train each of the 900+ MD/PhD students enrolled in these programs. Nevertheless, graduates face the challenges of navigating fragmented intervals of clinical training and research engagement, re-initiating research upon completing their residencies, managing financial pressures, and competing for funding following what is typically four or more years of research inactivity. Together, these barriers contribute to the high attrition rate of MSTP graduates from research careers.
Approach
The authors designed and implemented (2009–2014), for a single trainee, an alternative post-graduate training model characterized by early research engagement, strategic mentoring, unyoked clinical and research milestones, and dedicated financial support.
Outcomes
The pilot training experiment was so successful that the trainee secured an NIH project grant and completed his transition to research independence 3.5 years after starting the experimental training schedule—nearly 9 years earlier (based on age) than is typical for MD/PhDs transitioning from mentoredto independent research. This success has demonstrated that unyoking research engagement from conventional calendar-based clinical training milestones is a feasible, effective means of incubating the research independence in MSTP graduates.
Next Steps
The authors encourage the design and application of similar unconventional approaches that interweave residency training with ongoing research activity for appropriate candidates, especially in sub-specialties with increased MSTP graduate enrollment.
Problem
Physician scientists play a critical role in discovering new knowledge and translating their findings to medical practices that can improve clinical outcomes. Established in 1964 by the National Institutes of Health (NIH), the Medical Scientist Training Program (MSTP) is the preeminent model for training this unique cadre of scientists in the United States. While this program has a track record of placing nearly 95% of its graduates into residency programs for continued clinical training, more than 21% of these trainees do not pursue research following clinical training.1 Multiple factors likely contribute to this attrition. Most residency training programs preclude time for continued engagement with research during the first few years of clinical training, lengthening the hiatus from research begun during the clinically focused years of undergraduate medical MSTP training. Additionally, financial pressures resulting from the long post-graduate training sequence may influence some MSTP graduates’ decision to leave research. We suggest that unconventional residency training models should be developed and adopted to incubate the scientific growth of medical scientists and nurture their transition from supported to independent investigators.
The conventional model for clinical training is based on a framework whereby trainees work continuously in clinical service, acquiring a compulsory set of skills within a fixed timeframe. In contrast, the current model for PhD-level training for investigators in the scientific disciplines is based on a framework whereby an established committee of mentors evaluates each trainee’s individual progression towards a set of mutually-determinedmilestones over an unspecified time period (usually 3 to7 years). This graduate school training for research scientists is typically followed by further postdoctoral training which also continues for an unspecified length of time based on the individual trainee’s development. This PhD system recognizes that trainees differ in their capacities to master new knowledge and technical skills, and as such, allows trainees to progress at different rates. In certain circumstances, exceptional PhD graduates may forego traditional postdoctoral training to directly establish independent research laboratories.
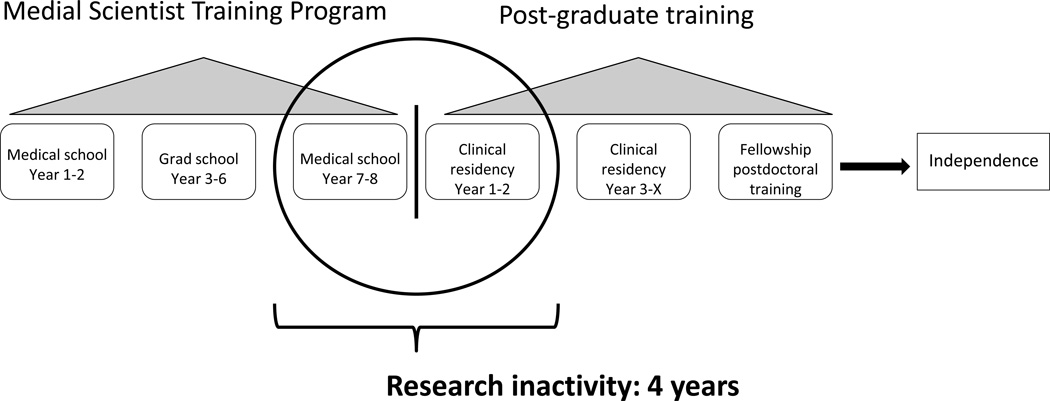
The MSTP is a sequential integration of these two otherwise independent training systems. In this model, research training occurs in successive, intermittent segments. An unintended consequence of this integration is that the development of trainees’ research skills becomes entrenched within and interrupted by a framework designed to optimize the delivery of clinical care (rather than the progression of junior supported researchers to independence). As illustrated in Figure 1, the current conventional model necessitates that trainees re-initiate research engagement after four or more years of inactivity. This model also prevents exceptional researchers from transitioning to scientific independence prior to completing their clinical training. Furthermore, physician-scientists serving as residents often face time demands and financial pressures when their development as an investigator is most fragile, which may cause some of them to abandon their research interests altogether.
Figure 1.
Standard clinical training schedule for Medical Scientist Training Program (MSTP) trainees. The training schedule is characterized by a sequence of 2 years of medical school training, 3 to 6 years of PhD training, and then the 2 final years of medical school. MSTP trainees then engage in post-graduate clinical training, which consists of 3 to 7 years (depending on the specialty) of immersive clinical training. There are limited opportunities for research engagement during the early stages of clinical training; more opportunities exist during later stages. Trainees interested in receiving advanced clinical training and furthering their research development then, post residency, engage in fellowship for an additional 1 to 4 years. At the conclusion of this 13- to 20-year training process, research-minded trainees have established their independent research laboratories.
In 2009, in our respective roles as dean of a medical school (R.S.W.), chair of a clinical department (R.R.K.), and physician-scientist in training (K.D.), we collectively designed and implemented an unconventional residency training model characterized by early and intensive research engagement, strategic mentoring, unyoked clinical and research milestones, and dedicated financial support with the intent of accelerating the independence of a physician scientist (K.D.). Our goal was to test a scalable model that other medical-scientist training leaders could apply for suitable candidates.
Approach
Experimental training schedule
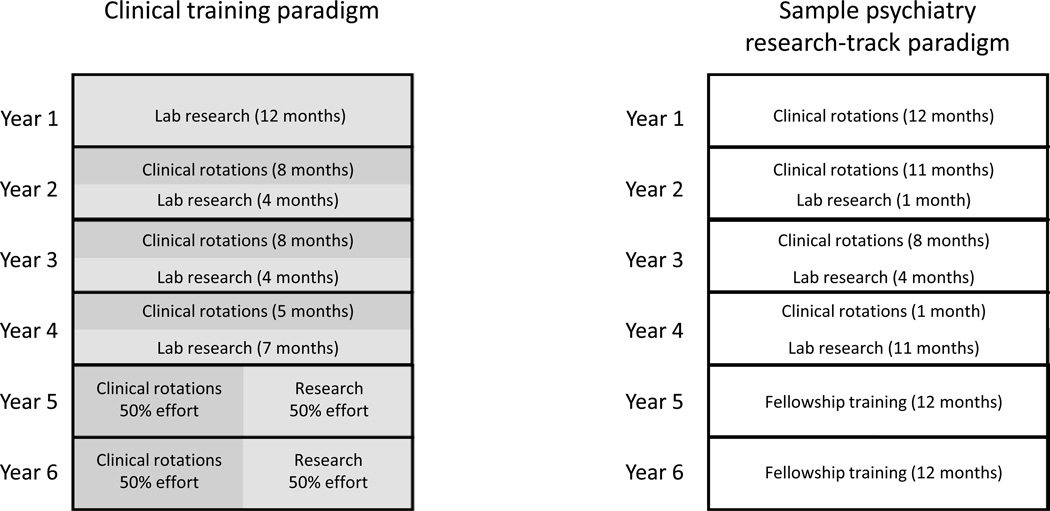
Our pilot experiment occurred from 2009 – 2014. The experiment was designed for an MSTP graduate (K.D.) pursuing clinical training in psychiatry through the Duke University medical center residency program. The graduate had earned his MD and his PhD, and he had completed two years of postdoctoral training while concurrently completing his medical school electives (i.e., years 7–8 of his MSTP training sequence). He had not yet begun clinical residency training. The three of us designed the experimental training schedule reported here, and the American Board of Psychiatry and Neurology approved the schedule.To address the loss of research momentum usually experienced by physician scientists due to research inactivity during clinical training, the program allowed for 100% research effort during the first post-graduate year. The trainee also received dedicated research space, financial resources to cover research supplies, and salary support (at the level of a full-time technician). The allotted research space was housed within the laboratory of a senior research mentor, and the trainee met one-on-one with the senior research mentor bi-weekly to track research milestones. The objective of this initial research year was for the trainee to identify a research focus and to establish a productive working relationship with a skilled research technician (i.e., the senior research mentor). During the next three years, the clinical schedule was designed such that the trainee engaged in research at one-third effort (see Figure 2). Specifically, the schedule allowed the trainee to engage in repeated intervals of 8 to 10 weeks of full-time clinical rotations followed by 4 to 6 weeks of full-time research. Over these 3 years, the research trainee completed the clinical requirements established for the first two years of typical post-graduate residency training in psychiatry. The research objectives established for the trainee during this time included collecting sufficient preliminary data for an NIH career development (K) award proposal, publishing a minimum of two first/senior author manuscripts, and participating in grant writing workshops.
Figure 2.
A comparison of an experimental and conventional post-graduate training schedule for Medical Scientist Training Program (MSTP) participants. The experimental training model, outlined on the left, hastened research independence for one MSTP graduate. The program allowed for 100% research effort during the first post-graduate year. During the next three years, the clinical schedule allowed the trainee to engage in research at one-third effort and to complete the clinical requirements established for the first two years of typical post-graduate residency training in psychiatry. For the final two years of clinical training, leading to eligibility for board certification, the schedule afforded the trainee the time to engage in research and advanced clinical training concurrently (at 50% effort each). A standard training schedule, shown to the right, is characterized by 4 years of clinical training, with increased opportunities for research engagement during the later stages of residency training. Trainees interested in receiving advanced clinical training and furthering their research development then engage in fellowship for an additional 2 years.
For the final two years of clinical training leading to eligibility for board certification, the schedule was designed such that the trainee engaged in research and advanced clinical training concurrently (at 50% effort each; see Figure 2). The research objectives established for this time period included securing an NIH K award, collecting sufficient preliminary data to support a NIH Research Project Grant Program (R01) application, and publishing a minimum of three additional first/senior author manuscripts.
Financial support
The trainee’s initial research engagement (i.e., the first 3 years of the program) was supported by $300,000 from internal sources, and $176,000 direct costs through an NIH administrative supplement mechanism for the trainee’s senior research mentor. These funds (the $476,000) were earmarked to support the trainees’ scientific research (including, as mentioned, salary support at the level of a research technician, research supplies, and equipment). Separate internal funding mechanisms supported the trainee’s clinical effort in accordance with all other standard clinical trainees. The trainee received an initial salary of $75,000 to ameliorate the financial pressures associated with the long MSTP post-graduate training schedule (i.e., 6 to 12 years of post-graduate training). A portion of the initial salary was covered by funds from internal clinical sources (in accordance with the trainees clinical effort), and the remainder was covered by the awarded administrative supplement. Asecond National Institute of Mental Health (NIMH) MD/PhD administrative supplement provided an additional $237,864 to support the trainee’s final two years of transition to independence (nearly $200,000 of this support remainedunused and was later recovered by the NIMH).
Outcomes
During the initial three (2009–2012) years of training, the trainee published 5 first/senior author manuscripts. The trainee also completed all of the clinical objectives required for post-graduate year (PGY) 1 training and collected sufficient preliminary data to submit NIH R01 and NIH exploratory (R21) grant applications. During the next 18-month interval (2012–2014), the trainee received R01 and R21 research project grants, published 3 first/senior author manuscripts, and completed all of the clinical objectives required for PGY2 training. Further, the trainee received several major awards during his post-MSTP training, which signal the innovative model’s effectiveness. Finally, the trainee also successfully negotiated for additional internal resources (financial support, space allotment, and a tenure-track faculty appointment) commensurate with a startup package.
The pilot training experiment was so successful that the trainee secured the R01 grant, negotiated the tenure-track appointment, and completed his transition to independent researcher just 3.5 years after starting the experimental training schedule—nearly 9 years earlier (based on their average age [43 years2]) than is typical for MD/PhDs transitioning to research independence.
Notably, due to NIMH stipulations, the trainee could not hold an R01 and an MD/PhD administrative supplement concurrently. Thus, nearly $200,000 of unused funding garnered through the second administrative supplementwas recovered by the NIMH when the trainee received the R01 award. The trainee has completed 5 years of the training outline to date.
We observed – and addressed – several challenges during the early stages of the pilot program. First, we sought and achieved the necessary focused administrative support critical to creating and sustaining an environment wherein the trainee could concentrate exclusively on meeting the clinical and research milestones. Second, at the onset of clinical engagement (i.e., year 2), we began intensive monitoring to ensure that the trainee remained in compliance with the established clinical duty-hour regulations. Finally, the unique training model resulted in a mild degree of isolation from clinical peers on the part of the trainee (i.e., the trainee did not progress through clinical training with a fixed cohort of other residents). Notably, this final challenge could be addressed readily by creating programs in which multiple graduates engage concurrently in this novel training model.
This pilot experiment demonstrated that a training paradigm that unyokes research engagement from conventional, calendar-based clinical training milestones can effectively and feasibly incubate the independent research of an MSTP graduate at an accelerated rate.
Next Steps
The training experiment we describe was performed with a single MSTP graduate pursuing clinical training in psychiatry through a single residency program. Nevertheless, we submit that the model may be scalable to other individuals (or cohorts) in diverse specialties in other residency programs. Further pilot programs and their evaluation will reveal the generalizability of this novel model.
Additional research will also reveal the best proportion of research engagement to clinical training. Some may argue that full-time clinical training may have advantages over meeting clinical milestones in a segmented manner. We contend that although current post-graduate clinical training models are indeed based on full immersion, trainees often acquire the core clinical learning milestones in a segmented manner. For example, a medical internship training sequence may include two months in the intensive care unit, two months on a general medicine unit, and then two months in an ambulatory care setting. Each trainee in a given program—though fully immersed in clinical training—may complete this 6-month sequence of rotations, but in a different order. Thus, we contend that many aspects of the predominant training model are already marked by segmented learning. As such, we believe that our proposed residency model, also characterized by month-to-month segmented clinical training and research engagement, is largely compatible with the training models currently in place for many clinical subspecialties. Notably, this approach may not be entirely feasible for surgical specialties that require refinement and maintenance of procedural skills.
The integrated model we describe results in two clear advantages over the current segmented model with respect to research training. First, our model provides support for a research technician during the first PGY of complete research immersion. This financial support allows trainees to establish a research enterprise that continues to drive scientific discovery even during subsequent periods when they are engaged in clinical training. Second, the pilot training sequence serves as a unique venue whereby trainees have the opportunity to create clear and informative links amongtheir clinical activities, research interests, and medical training.1,3Integration of this nature can occur during the latter stages of clinical training (i.e., fellowship), but in our model, we accelerate this integration to occur during the first two post-graduation years of research and clinical training. In fact, we believe that the early formation of links between clinical and research activities contributed directly to the rapid transition to scientific independence observed in our pilot study (i.e., the nine-year decrease in age to first R01) —a result the NIH has recently advocated.4 However, further experiments are required to test this hypothesis.
Overall, we demonstrate that an early and successful transition to independence for physician scientists can be supported with a post-graduate financial investment of approximately $720,000. This is in line with the $500,000 investment made by the NIH and its affiliated MSTPs to support the initialmedical and graduate training of each participating trainee. Thus, our findings support the development of novel federal support mechanisms and clinical training models that promote the early research engagement of selected MSTP graduates during residency.
Specifically, we encourage the design and application of similar unconventional approaches that interweave clinical training with ongoing research activity for appropriate candidates, especially in sub-specialties that demonstrate trends towards increased MSTP graduate enrollment.
Acknowledgments
The authors would like to thank National Institute of Mental Health staff for their helpful input on the initial design of the experimental training schedule. They would also like to thank M. G. Caron for graciously serving as the senior research mentor for the trainee.
Funding/Support: This work was supported by NIH supplement grants 3P50MH060451-09S1 to RRK/KD and 3R37MH073853-07S1 to M. G. Caron/KD.
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Disclaimers: None reported.
Contributor Information
Kafui Dzirasa, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, North Carolina.
Ranga R. Krishnan, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, North Carolina, and dean, Duke-NUS (National University of Singapore) Graduate Medical School, Singapore.
Sanders Williams, Gladstone Institutes, San Francisco, California.
References
- 1.Brass LF, Akabas MH, Burnley LD, Engman DM, Wiley CA, Andersen OS. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Academic Medicine. 2010;85:692–701. doi: 10.1097/ACM.0b013e3181d3ca17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institutes of Health Office of Extramural Research. Average age of principal investigators. [Accessed October 6, 2014]; Updated May 2008. http://www.report.nih.gov/NIH_Investment/PDF_sectionwise/NIH_Extramural_DataBook_PDF/NEDB_SPECIAL_TOPIC-AVERAGE_AGE.pdf.
- 3.Goldstein JL, Brown MS. The clinical investigator: bewitched, bothered, and bewildered—Butstill beloved. The Journal of clinical investigation. 1997;99:2803–2812. doi: 10.1172/JCI119470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institutes of Health. Office of Strategic Coordination—The Common Fund. NIH Directors Early Independence Award Program. [Accessed October 6, 2014]; http://commonfund.nih.gov/earlyindependence/.