Abstract
Introduction
Ileal ureter is a suitable treatment option for patients with long ureteric strictures. Minimally invasive techniques have been shown to be as safe as open techniques but superior in terms of post–operative recovery. We report our experience using minimally invasive techniques for total intracorporeal ureteral replacement.
Material and methods
A chart review revealed five patients who underwent intracorporeal ileal ureter using minimally invasive techniques in the preceding 5 years. 4 patients underwent conventional laparoscopic surgery and 1 patient underwent robotic–assisted surgery. Patient's characteristics, perioperative data and functional outcomes as well as a detailed description of surgical technique are reported. In all 5 of these patients, the ileal ureter was performed completely intracorporeally.
Results
The median age of our patients is 61 (range 42–73). The median operative time was 250 minutes (range 150–320) and median blood loss was 100 ml (range 50–200). The median hospital stay was 8 days (range 6–10) and there were no major perioperative complications reported. At median follow up of 22 months (range 4–38), there were no recurrences of strictures or any other complications.
Conclusions
We have demonstrated the safety and feasibility of minimally invasive intracorporeal ileal ureter. Numbers are still small but its application is likely to grow further.
Keywords: ileal ureter, ileal interposition, minimally invasive, laparoscopy, intracorporeal, ureteric strictures, robotics
INTRODUCTION
Substitution of ureter using ileum is suitable in cases with long or multiple ureteric strictures. The usage of ileum as a replacement of ureter was first done by Shoemaker in 1906 and subsequently popularized by Goodwin in 1959 [1]. Historically, an ileal ureter replacement was done for ureteric strictures secondary to tuberculosis. However, its usage has increased with increased incidence of ureteric strictures secondary to endoscopic procedures as well as radiation strictures. Ileum is a suitable substitute of ureter due to its rich blood supply and mobility. The risk of uraemia and acidosis is low if the selected patients have good renal functions preoperatively [2].
The first case of laparoscopic ileal ureter replacement was reported in 2000 [3] and the same group has also shown clear benefits of laparoscopic over open surgery in terms of post–operative recovery [4]. Since then, there are various reports of ileal ureter using laparoendoscopic single site as well as a robotic approach.
In our study, we report 5 patients with long ureteric stricture of which 4 patients underwent conventional laparoscopic surgery and 1 patient underwent robotic–assisted intracorporeal ileal ureter. There is a recent publication on robotic intracorporeal ileal ureter [5]; however, our series is the first report of laparoscopic intracorporeal ileal ureter.
MATERIAL AND METHODS
A search of our database of patients who underwent minimally invasive surgery in the past 5 years revealed 5 patients who underwent minimally invasive intracorporeal ileal ureter. Out of which, 4 patients underwent laparoscopic surgery and 1 patient underwent robotic assisted ileal ureter. The database was reviewed to include the data on patient's characteristics, disease etiology, perioperative data, complications and follow up.
A detailed description of the surgical technique of laparoscopic and robotic ileal ureter will be included (Figure 1). Our previous publication with the accompanied video has also demonstrated the key steps involved in laparoscopic ileal ureter [8].
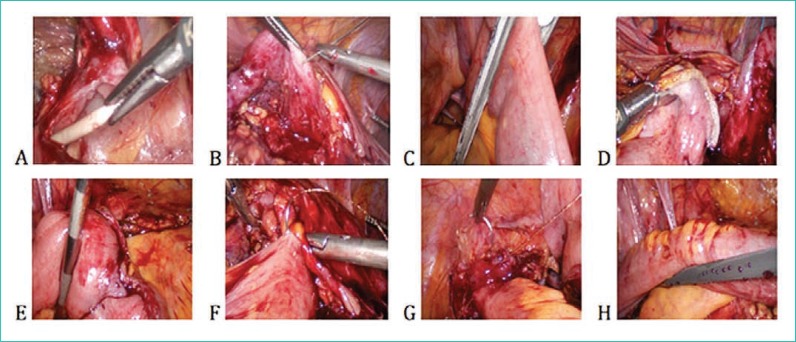
Figure 1.
A. Ureter identification and removal of Double J stent; B. Renal pelvis mobilization and suspension; C. Bowel transection using Endo_GIA stapler; D. Transected bowel temporarily fixed to renal pelvis; E. End–to–end anastomosis after distal transection; F – Pyeloileal anasotomosis; G – Ileovesical anastomosis; H – completed isoperistaltic ileal ureter.
Technique of laparoscopic intracorporeal ileal ureter
A conventional laparoscopy set and 30° telescope is used. The patient is placed in a lateral position. A transperitoneal approach is used in all of our patients. Ports were positioned as follows: 10 mm port at the level of the umbilicus for camera, two additional 12 mm ports 5 cm above and below the umbilicus, and one 5 mm port 1 cm below the xiphoid for liver retraction for right–sided surgery. All the ports are placed in the midline. An additional 12 mm port is placed in either right or left iliac fossa to facilitate the application of Endo–GIA stapler (Figure 2).
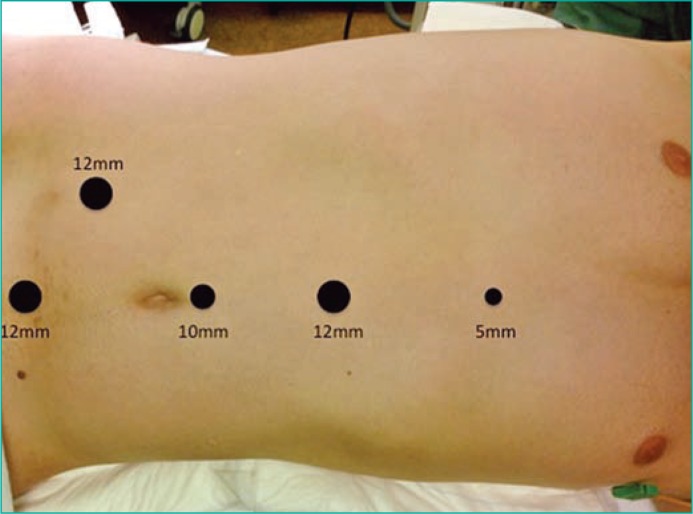
Figure 2.
Picture showing port placement for laparoscopic right ileal ureter: 10 mm port above umbilicus for camera; 12 m port x 2.5 cm above and below the umbilicus, 5 mm port 1 cm below the xiphoid for liver retraction and additional 12 mm port in right iliac fossa for Endo–GIA stapler.
The colon is medialised to expose the renal pelvis. A careful dissection of the renal pelvis was performed. After the ureter is identified, the ureter is transected and the double J stent is removed if it was inserted previously. Extensive mobilization of the renal pelvis is then performed and stay suturing using a straight needle is used to suspend the renal pelvis. A loop of terminal ileum 20 cm away from ilealcaecal valve is identified and suspended to the abdominal wall using a straight needle. The proximal end of terminal ileum is transected using an endo–GIA stapler. A bipolar cautery is used for haemostasis of the cut mesentery if bleeding occurs. The transected end of the ileum is brought up to the renal pelvis and temporarily fixed in that position using vicryl 3/0 sutures. The distal end of the ileum is brought down to the pelvis to ensure adequate length for the distal anastomosis and it is transected at this point using the Endo–GIA. Care is taken to ensure that it is an isoperistaltic segment. The bowel continuity is re–established by performing functional end–to–end anastomosis using the Endo–GIA stapler. The pyeloileal anastomosis can be performed using barbed sutures such as a V–lock or Stratafix suture. A 9fr double J stent was inserted before completion of the anastomosis. After completion of pyeloileal anasotomosis, the bladder is mobilized and a cystostomy is performed at the dome. The ileovesical anastomosis is performed in a similar fashion using a barbed suture. A surgical drain is placed.
In the one patient who underwent the robotic–assisted intracorporeal ileal ureter, the surgical steps are similar to above. The 12 mm ports placed 5 cm above and below the umbilicus are replaced by the 8 mm robotic port in this case. We started off the surgery in the same lateral position as the laparoscopic approach. After completion of the pyeloileal anastomosis, the robot was undocked and the patient was repositioned to the supine position. The ileovesical ansatomosis was then completed in a similar fashion as described above.
RESULTS
The median age of our 5 patients is 61 (range 42–73). The etiology of the ureteric strictures in our patients is retroperitoneal fibrosis, radiation stricture, ureteric avulsion and idiopathic fibrosis in 2 patients (Table 1). All of our patients had a normal preoperative glomerular filtration rate (GFR). The median operative time was 250 minutes (range 150–320) and median blood loss was 100 ml (range 50–200). All of our patients have a double J stent and drain inserted intra–operatively. The median hospital stay was 8 days (range 6–10). One patient developed post–operative fever with no obvious source and responded to an antibiotic treatment. The patient who underwent robotic ileal ureter was noted to have proximal migration of double J stent during routine stent removal at 6 weeks post–operatively. The stent was removed under general anesthesia and there were no further complications. All patients underwent double J stent removal at 6 weeks post surgery. At median follow up of 22 months (range 4–38), there were no recurrence of stricture on post–operative IVU or any other complications (Figure 3).
Table 1.
Patients’ biodata and perioperative data
| No. | Age | Sex | Etiology | Technique | Op time (min) | Blood loss (ml) | Hospital stay (days) | Complications | Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1. | 65 | Male | Ureteric avulsion | Robotic intracorporeal ileal ureter | 320 | 50 | 8 | Migrated stent | 33 |
| 2. | 58 | Male | Idiopathic stricture | Laparoscopic intracorporeal ileal ureter | 225 | 200 | 10 | No | 20 |
| 3. | 42 | Female | Radiation stricture | Laparoscopic intracorporeal ileal ureter | 250 | 100 | 8 | No | 35 |
| 4. | 61 | Female | Idiopathic stricture | Laparoscopic intracorporeal ileal ureter | 270 | 100 | 7 | Fever | 12 |
| 5. | 73 | Female | Retroperitoneal fibrosis | Laparoscopic intracorporeal ileal ureter | 150 | 50 | 6 | No | 2 |
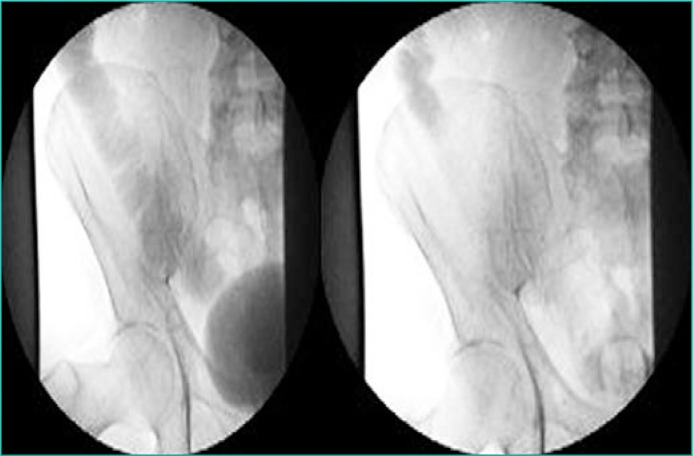
Figure 3.
Post–operative IVP showing no contrast extravasation and prompt emptying of contrast from the ileal ureter segment.
DISCUSSION
Previous studies have shown that laparoscopic ileal ureter is superior to open surgery in terms of shorter time to convalescence and shorter hospital stay [4]. A recent study has also demonstrated feasibility of complete intracorporeal ileal ureter using the robotic technique [5]. However, the operative time was 7 hours and this is partly attributed to the docking and undocking of the robot during different parts of surgery according to the author. In our series, the operative time of robotic assisted ileal ureter is longer than laparoscopic cases, though not clinically significant. In our series, a shorter operating time was observed in patients undergoing laparoscopic ileal ureter and we think this is attributed to the fact that the position of the patients can be adjusted whenever necessary without having to undock the robot, thus shortening the operative time. The additional 12 mm port inserted to right or left iliac fossa provides a better angle for manipulation of Endo–GIA to aid in the bowel resection and reconstruction. The pyeloileal and ileovesical anastomosis can be performed efficiently with the aid of a barbed suture such as stratafix or V–Lock. The conclusion of superiority of a laparoscopic approach over robotic in terms of operating time can only be drawn with larger prospective series to reach any clinical significance.
In terms of hospital stay, our series show a longer hospital stay in comparison to previous minimally invasive series which could be due to the subsidy system whereby the patients have to stay for 1 week in order to receive full subsidies.
Various previous literature on open ileal ureter reported about 10% of long–term complications such as anastomotic leak, strictures and fistula [6, 7]. In our series, there are no reported long–term complications. We attributed this to the fact that the minimally invasive technique allows for better visualization, which results in a more meticulous dissection and better pyeloileal and ileovesical anastomosis.
Currently, minimally invasive ileal ureter is shown to be advantageous over conventional open repair. However, there have been no comparison trials amongst the different minimally invasive techniques. We recognize the main limitation of our paper in view of its retrospective nature and small numbers of patients to allow us to draw any conclusions of clinical significance. A prospective trial with adequate numbers in the future will better compare the different techniques of minimally invasive ileal ureter.
CONCLUSIONS
In conclusion, minimally invasive intracorporeal ileal ureter is a safe and feasible procedure and it is a good alternative technique in patients undergoing this surgery.
References
- 1.Abrams HJ, Buchbinder MI. Experience with ileal ureters. Bulletin of The New York Academy of Medicine. 1977;53:329–337. [PMC free article] [PubMed] [Google Scholar]
- 2.Armatys SA, Mellon MJ, Beck SDW, Koch MO, Foster RS, Bihrle R. Use of Ileum as Ureteral Replacemnet in Urological Recostruction. J Urol. 2009;181:177–181. doi: 10.1016/j.juro.2008.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill IS, Savage SJ, Senagore AJ, Sung GT. Laparoscopic ileal ureter. J Urol. 2000;163:1199–1202. [PubMed] [Google Scholar]
- 4.Stein RJ, Turna B, Patel NS, Weight CJ, Nguyen MM, Shah G, et al. Laparoscopic assisted ileal ureter: technique, outcomes and comparism to open procedure. J Urol. 2009;182:1032–1039. doi: 10.1016/j.juro.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Brandao LF, Autorino R, Zargar H, Laydner H, Krishnan J, Samarasekera D, et al. Robotic ileal ureter: a completely intracorporeal technique. Urology. 2014;83:951–954. doi: 10.1016/j.urology.2013.11.035. [DOI] [PubMed] [Google Scholar]
- 6.Armatys SA, Mellon MJ, Beck SD, Koch MO, Foster RS, Bihrle R, et al. Use of ileum as urteral replacement in urological reconstruction. J Urol. 2009;181:177–181. doi: 10.1016/j.juro.2008.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung BI, Hamawy KJ, Zinman LN, Libertino JA. The use of bowel for ureteral replacement for complex ureteral reconstruction: long term results. J Urol. 2006;175:179–183. doi: 10.1016/S0022-5347(05)00061-3. [DOI] [PubMed] [Google Scholar]
- 8.Sim A, Todenhöfer T, Mischinger J, Halalsheh O, Boettge J, Rausch S, et al. Totally intracorporeal replacement of the ureter using whole–mount ileum. J Endourol. 2014 doi: 10.1089/end.2014.0169. [DOI] [PubMed] [Google Scholar]