Abstract
Introduction
Urinary incontinence (UI) is defined as any complaint of involuntary urine leakage. A description is provided of our experience with the ATOMS® (Adjustable Transobturator Male System. Agency for Medical Innovations. A.M.I.) adjustable implant in patients with mild to moderate UI.
Material and methods
A retrospective study was made of the data referring to 13 patients treated with this adjustable system. Demographic and personal data were collected along with information on the etiology, severity, characteristics, duration of UI, complementary tests, surgery times, complications and results obtained.
Results
The full continence (no use of pad) recovery rate at the close of the study was 12/13 (92.3%). Three cases required a single filling during the mean 16 months of follow–up (range 4–32; median 14 months). A complication in the form of perineal hematoma was resolved with conservative treatment and a case of urinary retention was resolved by placing a bladder catheter for the duration of one week. Three patients experienced perineal–scrotal dysesthesias that disappeared spontaneously in the first three months.
Conclusions
The described adjustable continence system has been found to be very effective in males with mild to moderate UI. In our experience, the ATOMS® implant offers excellent results over the middle term with a very low rate of complications that were easily resolved in all cases.
Keywords: male, urinary, incontinence, prothesis, adjustable
INTRODUCTION
Urinary incontinence (UI) is defined as any complaint of involuntary urine leakage [1]. According to data from the National Incontinence Observatory (NIO), the overall prevalence of male UI in Spain is about 7% (range 3.6–17%). In individuals over 65 years of age, this percentage can reach 14–29% and exceeds 50% in those over 85 years of age or in institutionalized subjects. Urinary incontinence has a strong impact upon the quality of life of the patient producing stress, depression, limitations in social and professional life, altered interpersonal relations, diminished sexual function and an increased risk of falls or need for institutionalization. Treatment options are diverse: rehabilitation of pelvic floor muscles, pharmacologic treatment, transurethral injection of substances and slings and an artificial urinary sphincter.
To date in our hospital, the invasive technique of choice for the treatment of males with mild to moderate (defined as the need for 1–2 pads/day) stress urinary incontinence (SUI) has been the implantation of Pro Act (Adjustable Continence Therapy for the Prostate. Uromedica. Plymouth, USA) type paraurethral balloons regardless of the underlying cause, due to the good results obtained and low complications rate [2–4]. Nevertheless, we continue to evaluate new techniques such as the ATOMS® implant with a view of offering more individualized treatment. The present study describes and analyzes our experience with this system.
MATERIAL AND METHODS
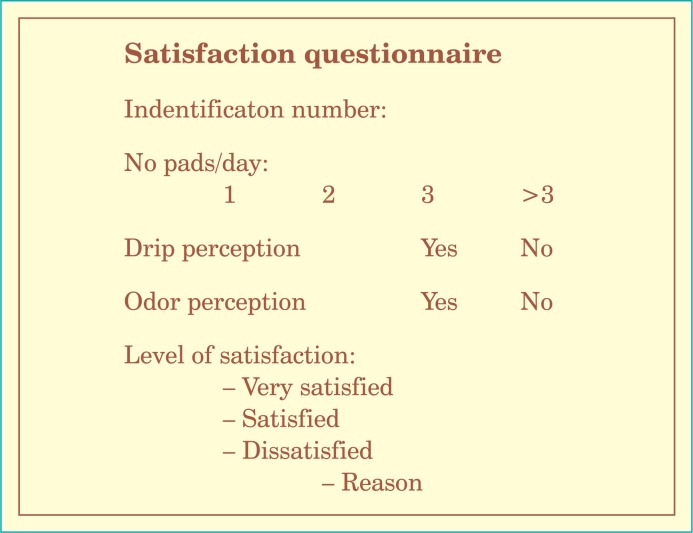
A retrospective cohort study was made based on the review of case histories and satisfaction questionnaires among patients subjected to surgical treatment for mild to moderate SUI diagnosed via urodynamic findings that persisted a year after surgery (Figure 2). The study involved patients subjected to serial micturition cystourethrography (MCU) without urethral stenosis, presenting good bladder capacity (300–550 milliliters) and who received an ATOMS® implant in the period 2010–2012.
Figure 2.
Satisfaction questionnaire.
The ATOMS® implant consists of an urethral pad with a lateral mesh on either side, a titanium port for adjustments and a silicone connection for joining both elements.
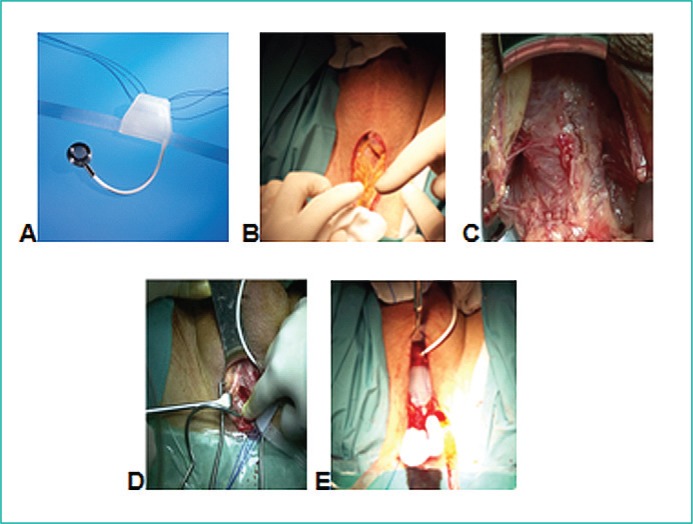
Our surgical technique is similar to that used by other groups, in all cases employing the suprapubic filling device instead of the recently marketed scrotal device [5–10]. Preoperative antibiotic prophylaxis is provided with a beta–lactam, following the recommendations of the current European guides [11]. With the patient in the lithotomy position, a longitudinal incision about 7–8 cm in length is made on the perineal midline, followed by dissection down to the bulbospongiosus muscle, which is preserved (Figure 1). Then, after identifying the ischiopubic rami, the left lateral mesh is inserted through the ipsilateral obturator orifice, emerging on the left lateral side of the bulbospongiosus muscle. The same procedure is carried out on the right side. Both bands are knotted, positioning the padding on the bulbospongiosus muscle at the urethral bulbar level, and anchored at four points by the lateral meshes. A transverse, left hypogastric incision about 2.5 cm in length is then made for housing the adjustable titanium port. The latter is fixed to the hypogastric subcutaneous tissue with Prolene 3/0 suture. Next, the subcutaneous tissue is dissected to form a superficial tunnel lateral to the spermatic cord (in the same way as for artificial sphincter preparation) extending to the implant site. A silicone connection is inserted through the tunnel joining the implant to the titanium port. Eight milliliters of saline solution is injected through the padding to achieve a degree of distension of the fixed implant, thereby applying slight compression upon the urethra. Layered closure of both incisions using loose Vicryl 3/0 stitches is then carried out. The bladder catheter is left in place for 24 hours and is removed before the patient is discharged. Oral antibiotic treatment is maintained up to 7 days after surgery. Subsequent follow–up comprises of a patient visit and micturition cystourethrography (MCU) four weeks after surgery to determine the objective and subjective implant results. Subsequent follow–ups depend on the primary pathology. An evolutive assessment is made of patient continence by administering as many fillings through the titanium port as needed to secure full urinary continence.
Figure 1.
The surgical technique. A. Components. B. Perineal incision. C. Bulbar Urethra Movilized. D. Tunneler application. E. ATOMS in place.
Demographic and personal data (age, gender, associated diseases) were collected along with information on the etiology, severity, characteristics, duration of UI, complementary tests, surgery times, complications and results obtained. The SPSS version 17.0 statistical package for MS Windows was used for descriptive analysis of the data with calculations of means, medians and percentages. Statistical comparisons were in turn made with the Pearson chi–squared test and the Fisher exact test, as applicable. Statistical significance was considered for p <0.05.
RESULTS
A total of 13 patients were included in the study. The mean age was 63 years (range 59–87).
Urinary incontinence developed following radical prostatectomy in 12 patients (92.3%) and following transurethral resection of the prostate in the remaining subject (7.2%). One patient had received radiotherapy (7.2%). Two patients (14.4%) had received another device for UI in the form of a Pro Act type paraurethral balloon; in both cases it had been removed due to spontaneous rupture of some element of the device more than 10 years after implantation. The clinical and demographic characteristics are shown in Table 1. The mean surgery time was 86.6 minutes (range 65–115). There were no intraoperative complications. Likewise, there were no added difficulties in performing the operation in those patients who had previously received a Pro Act implant, nor in the patient subjected to radiotherapy. In the immediate postoperative period, we observed one complication in the form of a perineal hematoma which resolved with conservative treatment, and one case of urinary retention which was resolved by placing a bladder catheter for the duration of one week. Three patients (23.1%) experienced postoperative perineal–scrotal dysesthesias which disappeared spontaneously in the first three months after surgery.
Table 1.
Demographic and clinical characteristics
| Age | 63 years (59–87) |
|---|---|
| Etiology | |
| Laparoscopic radical Prostatectomy | 92.3% (12) |
| Transurethral resection prostate | 7.7% (1) |
| Medical history | |
| Smoker | 15.4% (2) |
| High blood pressure | 30.8% (4) |
| Diabetes Mellitus | 7.7% (1) |
| Dyslipidemia | 38.5% (5) |
| Pelvic radiotherapy | 15.4% (2) |
| Previous implants surgery | 2 patients Pro–Act system. 100% removal after more than ten years of use for deterioration. |
| Type of incontinence | |
| Stress | 92.3% (12) |
| Mixed | 7.7% (1) |
| N° pads/day | |
| 1 | 30.8% (4) |
| 2 | 69.2% (9) |
| ASA | |
| I | 38.5% (5) |
| II | 46.2% (6) |
| III | 15.4% (2) |
| IV | 0% (0) |
| Follow–up (months) | 16 months (4–32) |
All complications were grade 1 and 2 using the Clavien Classification of Surgical Complications [12]. The full continence (no use of pad) recovery rate at the close of the study was 12/13 (92.3%). Three cases required a single filling (about two milliliters of saline solution) during the follow–up period. Following surgery, one patient who previously required two pads was able to use a single pad, which he did not wet each day; he expressed satisfaction with the operation. The results were not significantly different among the patients who had received previous implant surgery for UI. Likewise, the antecedent of radiotherapy in one patient did not affect the good results obtained with the device. No differences were found in surgical time or complications. All of the patients claimed to be satisfied with the results obtained. The mean duration of follow–up was 16 months (median 14; range 4–32).
DISCUSSION
Urinary incontinence (UI) can be classified according to whether it is caused by an alteration in the filling phase (hyperactive detrusor muscle, sphincter incompetence) or in the voiding phase (acontractile detrusor muscle, lower urinary tract obstruction) [13]. The present study focuses on incontinence secondary to sphincter incompetence, since this was the presentation in all of our patients. This type of UI can manifest after pelvic radiotherapy or after prostate gland surgery, including transurethral resection (1–3%), laser vaporization (0–3.3%), adenectomy (1–3%) or radical prostatectomy (1–40%). Radical prostatectomy is by far the most frequent cause, since the determination of prostate–specific antigen (PSA), prostate biopsies and advances in imaging techniques have produced a growing number of patients in which an early diagnosis is established, allowing radical prostatectomy with healing intent due to the existence of organ–confined malignancy [14–17]. Urinary incontinence following radical prostatectomy is fundamentally stress incontinence secondary to sphincter insufficiency (representing approximately 65% of all cases), though there are also cases of urge incontinence and even obstructive incontinence (stricture of the anastomosis) as a result of overflow [2, 18, 19]. The incidence of UI is decreasing thanks to the introduction and the expertise gained with new surgical techniques, which are much more precise and less invasive [20–25]. In general terms, the proportion of patients finally requiring surgery to resolve UI following radical prostatectomy is about 6–9% [26].
An artificial sphincter is the gold standard of treatment in males with stress UI (SUI). In our department, we reserve such treatment for patients with severe SUI (defined as the need for ≥3 pads/day or the use of diapers), while mild to moderate presentations are treated with adjustable systems such as the Pro Act paraurethral balloons. This latter approach offers very good results, with advantages over the artificial sphincters, since they are less expensive and are quickly and easily placed. In addition, they do not produce compression over the entire urethral circumference, thereby ensuring improved preservation of the vascular supply and allow individualized pressure adjustment without the need for patient cooperation to ensure correct functioning. As a result, they are highly advisable as a passive continence system [3, 4].
On the past three years, supply problems have guided us to look for alternatives for the treatment of this type of incontinence. In this matter, our choice has been the ATOMS® adjustable implant system. The ATOMS® implant offers the same advantages as the adjustable Pro Act system. Its placement is easier and more reproducible, since most urologists are familiarized with this surgical field. Furthermore, radiological exposure is avoided and complete dissection and freeing of the urethra is not required – a condition that could complicate its use by some urologists.
The first results referring to the treatment of UI using this new implant system were introduced by Bauer in 2005 [5]. Seweryn et al. [7] in a series of 38 patients with a mean follow up duration of 16.9 months recorded a 60.5% continence rate (0–1 pad or <15 ml/24 h in the pad test), 23.7% of the patients used more than one pad or presented leakage between 16–100 ml/24 h and 15.8% used more than two pads or had leakage >100 ml/24 h following the introduction of the ATOMS® adjustable implant. According to these authors, the parameters with the greatest influence upon treatment outcome are the number of pads used or the volume of urine leakage before the operation. In 2012, Hoda et al. [9] published the results of a multicenter study in 124 patients, with a global success rate of 93.8% (61.6% continence, and with clear improvement in the rest of the patients). In a previous study of similar characteristics involving 99 patients, the same authors reported a 63% continence rate, while 29% of the patients showed improvement of UI after implanting the device [6]. Astorbieta et al., in a series of 22 patients, observed full continence or improvement in 90% of the cases [10]. In our study, 92.4% of the patients were fully continent after implantation of this system – this percentage is greater than the figures reported in the aforementioned series. This may be because we only use the ATOMS® adjustable implant in patients with mild to moderate UI, not in individuals with severe incontinence.
Regarding the complications of the technique, Seweryn et al. [7] reported a case of acute urinary retention after removing the bladder catheter (requiring a further 24 hours of catheterization), one case of urethral erosion and four cases of infection at the site of the titanium port (requiring replacement of the port in one case and of the entire system in the remaining three). A total of 52.6% of the patients experienced perineal–scrotal dysesthesias that were resolved with medical treatment. This percentage reached 60.5% and 68.7% in the European multicenter studies conducted by Hoda et al., commented above [8, 9]. In our series, this problem was detected in 23.1% of the patients and analgesic treatment proved effective in all cases. We consider that the production of perineal–scrotal dysesthesias may be related to sectioning of the nerve endings on performing the incision followed by tissue dissection.
We observed no significant differences in technical difficulty or in the outcomes of treatment according to whether or not previous radiotherapy had been provided. This observation is consistent with the data published in the literature [6, 7, 9].
We consider the adjustable systems to be the best option for patients with mild to moderate incontinence. However, considering the difficulties found in divulgating and consolidating widespread use of the Pro Act system, the new ATOMS® device – which is based on the same concept since it is adjustable and allows passive continence control with no patient skill of any kind at micturition – might prove more accessible to most urologists, since the surgical technique is easy and reproducible.
CONCLUSIONS
The ATOMS® adjustable implant offers very good results in treating mild to moderate UI in males. The device is passive and safe, and the implantation technique is easily reproducible. We consider that the implantation of an artificial sphincter in patients of this kind could be disproportionate, considering the degree of incontinence and the cost involved.
References
- 1.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, et al. The standardization of terminology of lower urinary tract function: report from the Standardisation Subcommitte of the International Continence Society. Urology. 2003;61:37–49. doi: 10.1016/s0090-4295(02)02243-4. [DOI] [PubMed] [Google Scholar]
- 2.Hübner WA, Schlarp OM. Treatment of incontinence after prostatectomy using a new minimally invasive device: adjustable continence therapy. BJU Int. 2005;96:587–594. doi: 10.1111/j.1464-410X.2005.05689.x. [DOI] [PubMed] [Google Scholar]
- 3.García Matres MJ, Cansino Alcaide JR, Monasterio S, Rodríguez de Bethencourt F, Hidalgo Togores L, de la Peña Barthel J. Balones parauretrales (Pro–ACTTM) en la incontinencia urinaria postquirúrgica del cáncer de próstata. Arch Esp Urol. 2009;62:871–881. doi: 10.4321/s0004-06142009001000012. [DOI] [PubMed] [Google Scholar]
- 4.Cansino Alcaide JR, Alvarez Maestro M, Martín Hernández M, Cabrera Castillo PM, Pérez–Utrilla Pérez M, Rodríguez de Bethencourt F, et al. Implante de balones parauretrales como tratamiento de la incontinencia urinaria masculina. Experiencia del Hospital Universitario La Paz. Arch Esp Urol. 2007;60:647–655. doi: 10.4321/s0004-06142007000600005. [DOI] [PubMed] [Google Scholar]
- 5.Bauer W, Karik M, Schramek P. The selfanchoring transobturator male sling to treat stress urinary incontinence in men: a new sling, a surgical approach and anatomical findings in a cadaveric study. BJU Int. 2005;95:1364–1366. doi: 10.1111/j.1464-410X.2005.05530.x. [DOI] [PubMed] [Google Scholar]
- 6.Hoda MR. Early results of a European multicentre experience with a new self–anchoring adjustable transobturator system for treatment of stress urinary incontinence in men. BJU Int. 2012;111:296–303. doi: 10.1111/j.1464-410X.2012.11482.x. [DOI] [PubMed] [Google Scholar]
- 7.Seweryn J, Bauer W, Ponholzer A, Schramek P. Initial Experience and Results With a New Adjustable Transobturator Male System for the Treatment of Stress Urinary Incontinence. J Urol. 2012;187:956–961. doi: 10.1016/j.juro.2011.10.138. [DOI] [PubMed] [Google Scholar]
- 8.Bauer W. Adjustable transobturator male system – ATOMS – for the treatment of post–prostatectomy urinary incontinence: The surgical technique. Pelviperineology. 2011;30:10–16. [Google Scholar]
- 9.Hoda MR, Primus G, Schumann A, Fischereder K, von Heyden B, Schmid N, et al. Behandlung der Belastungsinkontinenz nach radikaler Prostatektomie. Urologe. 2012;51:1576–1583. doi: 10.1007/s00120-012-2950-2. [DOI] [PubMed] [Google Scholar]
- 10.Astobieta Odriozola A, Gamarra Quintanilla M, Pereira Arias Jg, Leibar Tamayo A, Olaizola Fuertes G, et al. Nuestra experiencia con el sistema ajustable transobturador (Atoms®) para el tratamiento de la incontinencia urinaria masculina. Act Urol Esp. 2012;36:17. [Google Scholar]
- 11.Grabe M, Bartoletti R, Bjerklund–Johansen TE, Çek HM, Pickard RS, Tenke P. European Association of Urology Guidelines on urological infections. 2013 Chapt 15. [Google Scholar]
- 12.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 13.Moreno Sierra J. Atlas de incontinencia urinaria y suelo pélvico. :368. Chapt 24. [Google Scholar]
- 14.Welk BK, Herschorn S. The male sling for post–prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int. 2012;109:328–344. doi: 10.1111/j.1464-410X.2010.10502.x. [DOI] [PubMed] [Google Scholar]
- 15.Herschorn S, Bruschini H, Comiter C, Grise P, Hanus T, Kirschner–Hermanns R, et al. Surgical treatment of stress incontinence in men. Neurourol Urodyn. 2010;29:179–190. doi: 10.1002/nau.20844. [DOI] [PubMed] [Google Scholar]
- 16.Westenberg A, Gilling P, Kennett K, Frampton C, Fraundorfer M. Holmium laser resection of the prostate versus transurethral resection of the prostate: Results of a randomized trial with 4–year minimum long–term followup. J Urol. 2004;172:616–619. doi: 10.1097/01.ju.0000132739.57555.d8. [DOI] [PubMed] [Google Scholar]
- 17.Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol. 2008;53:382–389. doi: 10.1016/j.eururo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 18.Groutz A, Blaivas JG, Chaikin DC, Weiss JP, Verhaaren M. The pathophysiology of post–radical prostatectomy incontinence: a clinical and video urodynamic study. J Urol. 2000;163:1767–1670. [PubMed] [Google Scholar]
- 19.Porena M, Mearini E, Mearini L, Vianello A, Giannantoni A. Voiding dysfunction after radical retropubic prostatectomy: more than external urethral sphincter deficiency. Eur Urol. 2007;52:38–45. doi: 10.1016/j.eururo.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 20.Dalkin BL, Wessells H, Cui H. A national survey of urinary and health related quality of life outcomes in men with an artificial urinary sphincter for post–radical prostatectomy incontinence. J Urol. 2003;169:237–239. doi: 10.1016/S0022-5347(05)64076-1. [DOI] [PubMed] [Google Scholar]
- 21.Bauer RM, Mayer ME, Gratzke C, Soljanik I, Bastian PJ, Stief CG, Gozzi C. Urinary incontinence after radical prostatectomy. Urologe. 2009;48:1044–1049. doi: 10.1007/s00120-009-2081-6. [DOI] [PubMed] [Google Scholar]
- 22.Delgado Oliva FJ, Caballero Romeo JP, García Serrado D, Prieto Chaparro L, Carro Rubias C, Chillón Sempere S, et al. Incontinencia urinaria tras prostatectomía radical: evolución histórica de la técnica quirúrgica y estado actual del resultado funcional. Arch Esp Urol. 2009;62:809–818. doi: 10.4321/s0004-06142009001000005. [DOI] [PubMed] [Google Scholar]
- 23.Prieto L. Disfunción miccional en el cáncer de próstata. Arch Esp Urol. 2009;62:773–785. [PubMed] [Google Scholar]
- 24.Hollabaugh RS, Dmochowski RR, Kneib TB, Steiner MS. Preservation of putative continence nerves during radical retropubic prostatectomy leads to more rapid return of urinary continence. Urology. 1998;51:960–967. doi: 10.1016/s0090-4295(98)00128-9. [DOI] [PubMed] [Google Scholar]
- 25.Koppie TM, Guillonneau B. Predictors of Incontinence after Radical Prostatectomy: Where Do We Stand? Eur Urol. 2007;52:22–23. doi: 10.1016/j.eururo.2007.01.091. [DOI] [PubMed] [Google Scholar]
- 26.Bauer RM, Gozzi C, Hübner W, Nitti VW, Novara G, Peterson A, et al. Contemporary management of postprostatectomy incontinence. Eur Urol. 2011;59:985–996. doi: 10.1016/j.eururo.2011.03.020. [DOI] [PubMed] [Google Scholar]