Abstract
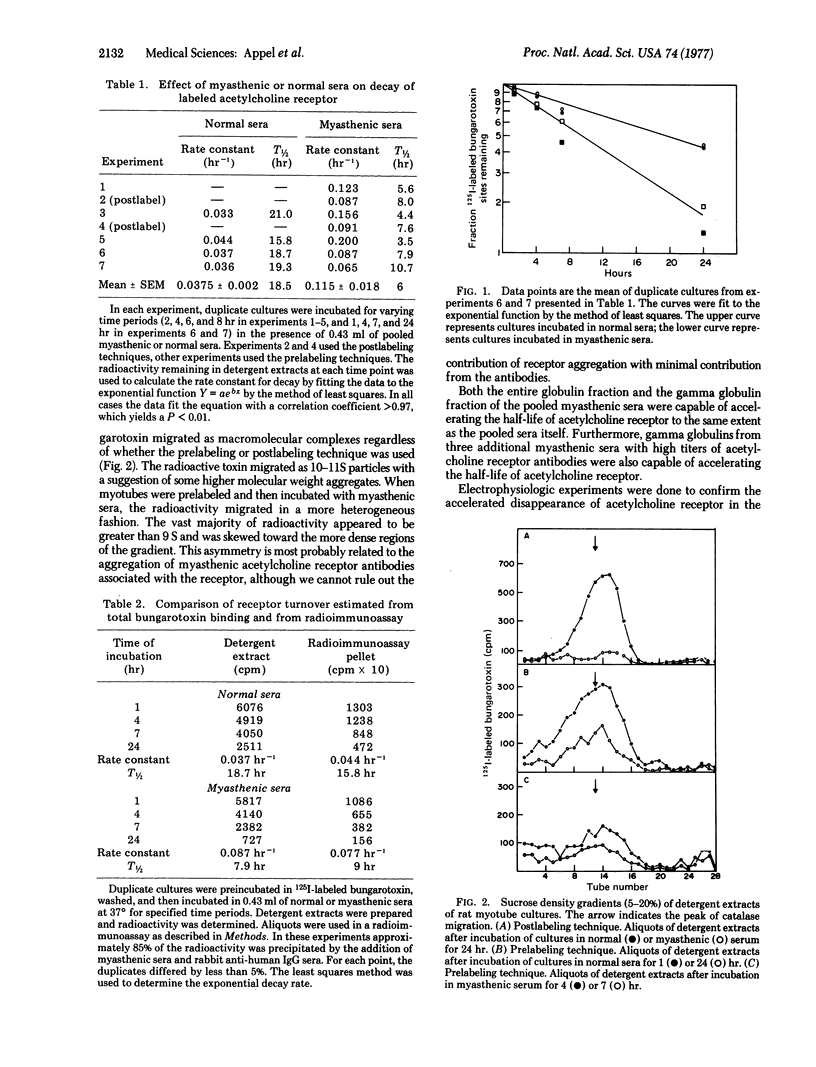
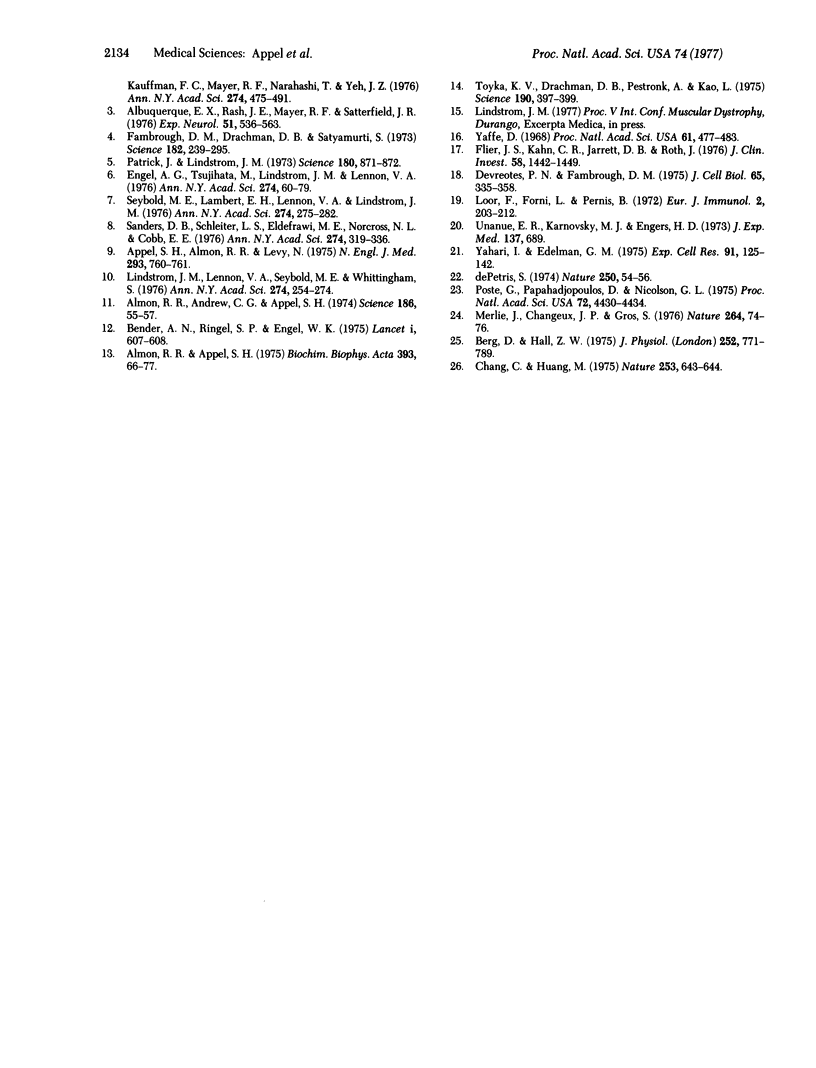
Altered geometry of the neuromuscular junction and a decreased number of acetylcholine receptors appear responsible for the defect of neuromuscular transmission in myasthenia gravis. We have used cultured rat myotubes as a model to study in vitro the potential role of myasthenic globulins in the pathological process. Acetylcholine receptor content was assayed by the extent of 125I-labeled alpha-bungarotoxin binding, and acetylcholine receptor function was assayed by the sensitivity to acetylcholine iontophoresis. The half-life of the acetylcholine receptor was 18.5 hr in the presence or absence of control sera. Myasthenic sera and globulins produced a gradual reduction in acetylcholine receptors, as assessed by biochemical and electrophysiological techniques. The half-life in the presence of myasthenic sera was 6 hr. The accelerated turnover was unaffected by puromycin but was slowed by lowered temperature (18-20 degrees), interference with energy metabolism (2,4-dinitrophenol), and interference with cytoskeletal structures (colchicine and cytochalasin B). We found no electrophysiological evidence to suggest globulin blockade of acetylcholine access to the acetylcholine receptor. Our observations suggest that circulating globulins in myasthenia gravis may contribute to the functional defects of neuromuscular transmission by accelerating the rate of internationalization and degradation of surface membrane acetylcholine receptors.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albuquerque E. X., Lebeda F. J., Appel S. H., Almon R., Kauffman F. C., Mayer R. F., Narahashi T., Yeh J. Z. Effects of normal and myasthenic serum factors on innervated and chronically denervated mammalian muscles. Ann N Y Acad Sci. 1976;274:475–492. doi: 10.1111/j.1749-6632.1976.tb47709.x. [DOI] [PubMed] [Google Scholar]
- Albuquerque E. X., Rash J. E., Mayer R. F., Satterfield J. R. An electrophysiological and morphological study of the neuromuscular junction in patients with myasthenia gravis. Exp Neurol. 1976 Jun;51(3):536–563. doi: 10.1016/0014-4886(76)90179-5. [DOI] [PubMed] [Google Scholar]
- Almon R. R., Andrew C. G., Appel S. H. Serum globulin in myasthenia gravis: inhibition of alpha-bungarotoxin binding to acetylcholine receptors. Science. 1974 Oct 4;186(4158):55–57. doi: 10.1126/science.186.4158.55. [DOI] [PubMed] [Google Scholar]
- Almon R. R., Appel S. H. Interaction of myasthenic serum globulin with the acetylcholine receptor. Biochim Biophys Acta. 1975 May 30;393(1):66–77. doi: 10.1016/0005-2795(75)90217-2. [DOI] [PubMed] [Google Scholar]
- Appel S. H., Almon R. R., Levy N. Acetylcholine receptor antibodies in myasthenia gravis. N Engl J Med. 1975 Oct 9;293(15):760–761. doi: 10.1056/NEJM197510092931508. [DOI] [PubMed] [Google Scholar]
- Bender A. N., Ringel S. P., Engel W. K., Daniels M. P., Vogel Z. Myasthenia gravis: a serum factor blocking acetylcholine receptors of the human neuromuscular junction. Lancet. 1975 Mar 15;1(7907):607–609. doi: 10.1016/s0140-6736(75)91886-3. [DOI] [PubMed] [Google Scholar]
- Berg D. K., Hall Z. W. Loss of alpha-bungarotoxin from junctional and extrajunctional acetylcholine receptors in rat diaphragm muscle in vivo and in organ culture. J Physiol. 1975 Nov;252(3):771–789. doi: 10.1113/jphysiol.1975.sp011169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C. C., Huang M. C. Turnover of junctional and extrajunctional acetylcholine receptors of the rat diaphragm. Nature. 1975 Feb 20;253(5493):643–644. doi: 10.1038/253643a0. [DOI] [PubMed] [Google Scholar]
- De Petris S. Inhibition and reversal of capping by cytochalasin B, vinblastine and colchicine. Nature. 1974 Jul 5;250(461):54–56. doi: 10.1038/250054a0. [DOI] [PubMed] [Google Scholar]
- Devreotes P. N., Fambrough D. M. Acetylcholine receptor turnover in membranes of developing muscle fibers. J Cell Biol. 1975 May;65(2):335–358. doi: 10.1083/jcb.65.2.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel A. G., Santa T. Histometric analysis of the ultrastructure of the neuromuscular junction in myasthenia gravis and in the myasthenic syndrome. Ann N Y Acad Sci. 1971 Sep 15;183:46–63. doi: 10.1111/j.1749-6632.1971.tb30741.x. [DOI] [PubMed] [Google Scholar]
- Engel A. G., Tsujihata M., Lindstrom J. M., Lennon V. A. The motor end plate in myasthenia gravis and in experimental autoimmune myasthenia gravis. A quantitative ultrastructural study. Ann N Y Acad Sci. 1976;274:60–79. doi: 10.1111/j.1749-6632.1976.tb47676.x. [DOI] [PubMed] [Google Scholar]
- Fambrough D. M., Drachman D. B., Satyamurti S. Neuromuscular junction in myasthenia gravis: decreased acetylcholine receptors. Science. 1973 Oct 19;182(4109):293–295. doi: 10.1126/science.182.4109.293. [DOI] [PubMed] [Google Scholar]
- Flier J. S., Kahn C. R., Jarrett D. B., Roth J. Characterization of antibodies to the insulin receptor: a cause of insulin-resistant diabetes in man. J Clin Invest. 1976 Dec;58(6):1442–1449. doi: 10.1172/JCI108600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom J. M., Lennon V. A., Seybold M. E., Whittingham S. Experimental autoimmune myasthenia gravis and myasthenia gravis: biochemical and immunochemical aspects. Ann N Y Acad Sci. 1976;274:254–274. doi: 10.1111/j.1749-6632.1976.tb47691.x. [DOI] [PubMed] [Google Scholar]
- Loor F., Forni L., Pernis B. The dynamic state of the lymphocyte membrane. Factors affecting the distribution and turnover of surface immunoglobulins. Eur J Immunol. 1972 Jun;2(3):203–212. doi: 10.1002/eji.1830020304. [DOI] [PubMed] [Google Scholar]
- Merlie J. P., Changeux J. P., Gros F. Acetylcholine receptor degradation measured by pulse chase labelling. Nature. 1976 Nov 4;264(5581):74–76. doi: 10.1038/264074a0. [DOI] [PubMed] [Google Scholar]
- Patrick J., Lindstrom J. Autoimmune response to acetylcholine receptor. Science. 1973 May 25;180(4088):871–872. doi: 10.1126/science.180.4088.871. [DOI] [PubMed] [Google Scholar]
- Poste G., Papahadjopoulos D., Nicolson G. L. Local anesthetics affect transmembrane cytoskeletal control of mobility and distribution of cell surface receptors. Proc Natl Acad Sci U S A. 1975 Nov;72(11):4430–4434. doi: 10.1073/pnas.72.11.4430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders D. B., Schleifer L. S., Eldefrawi M. E., Norcross N. L., Cobb E. E. An immunologically induced defect of neuromuscular transmission in rats and rabbits. Ann N Y Acad Sci. 1976;274:319–336. doi: 10.1111/j.1749-6632.1976.tb47695.x. [DOI] [PubMed] [Google Scholar]
- Seybold M. E., Lambert E. H., Lennon V. A., Lindstrom J. M. Experimental autoimmune myasthenia: clinical, neurophysiologic, and pharmacologic aspects. Ann N Y Acad Sci. 1976;274:275–282. doi: 10.1111/j.1749-6632.1976.tb47692.x. [DOI] [PubMed] [Google Scholar]
- Toyka K. V., Brachman D. B., Pestronk A., Kao I. Myasthenia gravis: passive transfer from man to mouse. Science. 1975 Oct 24;190(4212):397–399. doi: 10.1126/science.1179220. [DOI] [PubMed] [Google Scholar]
- Unanue E. R., Karnovsky M. J., Engers H. D. Ligand-induced movement of lymphocyte membrane macromolecules. 3. Relationship between the formation and fate of anti-Ig-surface Ig complexes and cell metabolism. J Exp Med. 1973 Mar 1;137(3):675–689. doi: 10.1084/jem.137.3.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe D. Retention of differentiation potentialities during prolonged cultivation of myogenic cells. Proc Natl Acad Sci U S A. 1968 Oct;61(2):477–483. doi: 10.1073/pnas.61.2.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yahara I., Edelman G. M. Electron microscopic analysis of the modulation of lymphocyte receptor mobility. Exp Cell Res. 1975 Mar 1;91(1):125–142. doi: 10.1016/0014-4827(75)90150-0. [DOI] [PubMed] [Google Scholar]


