Abstract
We present our experience with intratesticular hematoma (ITH) without rupture of the tunica albuginea following blunt scrotal trauma and present an algorithm for management. We reviewed the charts of 3 patients who presented between 2006 and 2013 with this finding. Time from the incident to presentation ranged from 5 hours to 4 days. All patients underwent at least one scrotal ultrasound reviewed by the same urologist. Two patients underwent surgical exploration and all patients had resolution of pain within one to two days. Management of ITH should be centered on the patient's pain severity as well as serial ultrasound findings.
Keywords: intratesticular hematoma, blunt scrotal trauma, scrotal ultrasound
INTRODUCTION
Clinical management for acute blunt scrotal trauma includes prompt exploration if testicular rupture is identified on physical exam or ultrasound, which is known to decrease orchiectomy rates versus delayed repair [1–3]. To our knowledge, however, there are few reviews that include the specific management of intratesticular hematoma (ITH) without testicular rupture. Current recommendations advise conservative management if the tunica is intact and there is a small ITH, while a “significant” ITH should be explored [2–6]. The aim of this paper is to describe the outcomes of three cases of ITH without testis rupture and propose a management algorithm for this rare clinical scenario based on our experience as well as on a review of the literature.
METHODS
We reviewed the charts and images of three patients who presented between 2006 and 2013 with an ITH and intact tunica albuginea (TA) following blunt scrotal trauma. We then conducted PubMed and MEDLINE searches for “intratesticular hematoma” and “blunt scrotal trauma”.
Case 1
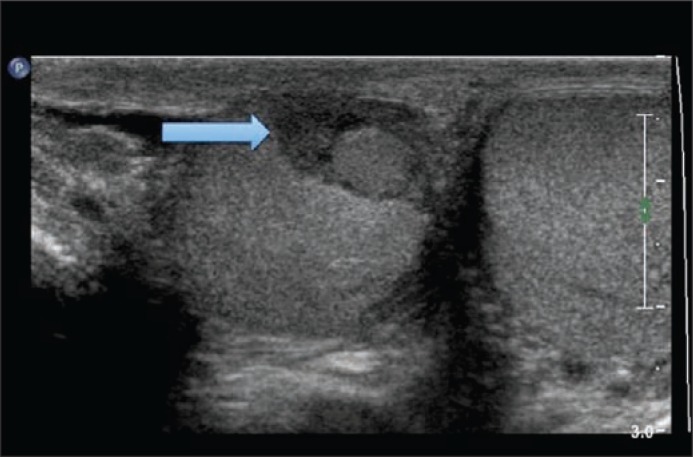
A 29–year old baseball player presented to the emergency department 6 hours after he was hit in the scrotum with a baseball. He exited the game due to 10/10 pain radiating to the inguinal area with mild nausea. Physical exam was notable for a non–displaced right testis that was indurated and tender to palpation with no discernible rupture. Ultrasound showed an intact TA with an area of heterogeneous echotexture measuring 2.0 x 0.8 x 1.6 cm with no flow (Figure 1). He was observed in the emergency department and an ultrasound was repeated 1 hour later. The hypoechoic area was noted to have expanded thus he was taken to the operating room where an ITH with an intact TA was found. The clot was evacuated and the nonviable seminiferous tubules were debrided. He had an unremarkable postoperative course.
Figure 1.
Scrotal ultrasound of 29 year old baseball player found to have ITH with intact tunica albuginea. Arrow = ITH.
Case 2
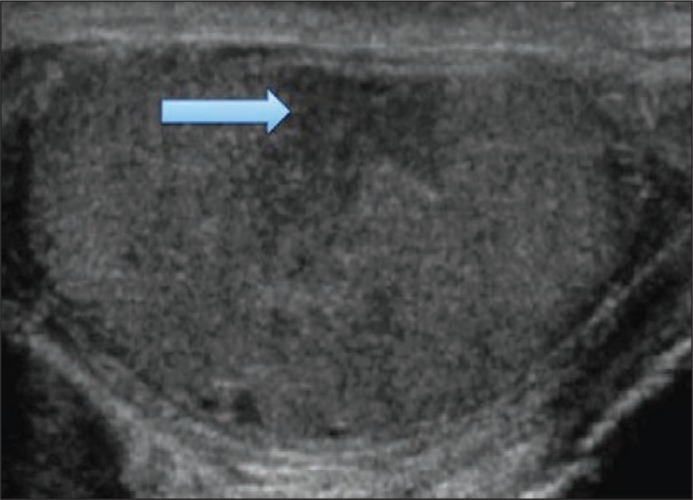
A 27–year old hockey player presented to the emergency department 5 hours after he was struck in the scrotum by a puck. He had moderate pain and his left hemi–scrotum was mildly swollen and tender with no palpable scrotal hematoma or testicular rupture. His scrotal ultrasound showed an intact left TA, good flow to the parenchyma, and a heterogeneous hypoechoic well–circumscribed region measuring 2.6 x 1.5 x 2.3 cm with no internal flow. Within this region there was a smaller round nodule with a hyperechoic rim, believed to represent an epidermoid cyst (Figure 2). Given that his scrotal exam was relatively benign and his pain could be controlled with oral narcotics, he was managed conservatively. An ultrasound the following day showed no interval expansion, and on ultrasound 3 weeks later, resolution of the small nodule within the ITH was noted, as well as continued good blood flow to the testis. He returned to the line–up and played one week after the injury.
Figure 2.
Scrotal ultrasound of 27 year old hockey player with ITH and incidental epidermoid cyst. Large Arrow = ITH. Small Arrow = Epidermoid Cyst.
Case 3
A 56–year old veteran presented to the emergency room 4 days after he fell and struck his scrotum. He complained of worsening pain and nausea with one episode of emesis. His scrotum was not significantly swollen and there was no evidence of rupture, however, he had significant tenderness on exam. His scrotal ultrasound showed blood flow to the testis and a 1.1 x 1.2 x 1.3 cm ITH (Figure 3). Due to his significant pain and extreme tenderness on exam, he was taken to the operating room. Scrotal exploration revealed an intact TA however nearly 50% of the seminiferous tubules were nonviable and required debridement (Figure 4). His pain resolved on post–operative day 2 and at five–month follow–up his testis size remained stable with no scrotal pain.
Figure 3.
Scrotal ultrasound of 56 year old Veteran four days after a fall. Arrow = ITH.
Figure 4.
Bivalved testis showing non-viable semniferous tubules that were subsequently debrided.
DISCUSSION
The goals of surgical exploration for blunt trauma are salvage of the testis for endocrine and fertility preservation, pain control, and a shorter recovery time [7]. The pathophysiology of an ITH without TA rupture appears to involve a compartment syndrome within the affected testis [7]. There is a paucity of literature regarding the diagnosis and management of ITH, and current recommendations are based on descriptions from over two decades ago [1–3].
Chandra et al. developed an algorithm for blunt scrotal trauma based off of 44 patients with blunt scrotal trauma, of which 6 were diagnosed with ITH on ultrasound. Five of the six were managed conservatively and one with surgery due to incomplete visualization of the TA. However, no size parameters or specifics of the ITH were given for these patients and only one patient was followed up. The authors concluded that most cases of ITH can be treated conservatively and advocated a 6–week follow–up ultrasound to rule out a mass [8]. A study of 33 patients including 7 with ITH who all underwent ultrasound followed by surgical exploration revealed a 71% sensitivity and 77% specificity for ultrasound diagnosis of ITH (5 of 7 cases). Their rationale for intervention was based off of Cass’ original work aimed at decreasing morbidity, delayed orchiectomy rates, and long term testis atrophy. Twenty–four patients (73%) had follow–up within one month of surgery, though none of the explored cases of ITH were specifically reported [9].
In our series, surgical exploration was pursued in cases of extreme pain or tenderness on exam and with evidence of an expanding ITH on ultrasound. Case 2 was observed successfully given moderate symptoms and a stable appearance of the ITH on serial ultrasound. Unfortunately, as with other studies, the size parameters of a “significant” versus an “insignificant” ITH remain undetermined. Our study is limited as a case series and by its retrospective nature, however, due to the paucity of literature in this area we feel it will aid in the management strategy of these patients.
Based on our experience and on a review of the literature, we propose a clinical algorithm for ITH without TA rupture (Figure 5). A patient with mild to moderate pain and a stable ITH on serial ultrasound can be safely observed. Serial scrotal ultrasound should be performed within the first 72 hours following blunt trauma. However, if a patient has significant pain or evidence of a large and/or expanding ITH on serial ultrasound, scrotal exploration should be considered.
Figure 5.
Algorithm for Management of ITH.
References
- 1.Cass AS. Testicular trauma. J Urol. 1983;129:299–300. doi: 10.1016/s0022-5347(17)52062-5. [DOI] [PubMed] [Google Scholar]
- 2.Cass AS, Luxenberg M. Value of early operation in blunt testicular contusion with hematocele. J Urol. 1988;139:746–747. doi: 10.1016/s0022-5347(17)42620-6. [DOI] [PubMed] [Google Scholar]
- 3.Cass AS, Luxenberg M. Testicular injuries. Urology. 1991;37:528–530. doi: 10.1016/0090-4295(91)80317-z. [DOI] [PubMed] [Google Scholar]
- 4.Morey AF, Metro MJ, Carney KS, Miller KS, McAninch JW. Consensus on genitourinary trauma: external genitalia. Br J Urol. 2004;94:507–515. doi: 10.1111/j.1464-410X.2004.04993.x. [DOI] [PubMed] [Google Scholar]
- 5.Morey AF, Dugi DD., III . Genital and Lower Urinary Tract Trauma. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell–Walsh Urology. 10th ed. Philadelphia: Saunders; 2012. pp. 2512–2514. Chapt 88. [Google Scholar]
- 6.Lynch TH, Martínez–Piñeiro L, Plas E, Serafetinides E, Türkeri L, Santucci R. EAU Guidelines on Urological Trauma. Eur Urol. 2005;47:1–15. doi: 10.1016/j.eururo.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 7.Kukadia AN, Ercole CJ, Gleich P, Hensleigh H, Pryor JL. Testicular trauma: potential impact on reproductive function. J Urol. 1996;156:1643–1646. doi: 10.1016/s0022-5347(01)65472-7. [DOI] [PubMed] [Google Scholar]
- 8.Chandra RV, Dowling RJ, Ulubasoglu M, Haxhimolla H, Costello AJ. Rational Approach to Diagnosis and Management of Blunt Scrotal Trauma. Urology. 2007;70:230–234. doi: 10.1016/j.urology.2007.03.064. [DOI] [PubMed] [Google Scholar]
- 9.Guichard G, El Ammari J, Del Coro C, Cellarier D, Loock PY, Chabannes E, et al. Accuracy of Ultrasonography in Diagnosis of Testicular Rupture after Blunt Scrotal Trauma. Urology. 2008;71:52–56. doi: 10.1016/j.urology.2007.09.014. [DOI] [PubMed] [Google Scholar]