Abstract
Rib fractures are one of main causes of chest or flank pain when related to an osteoporotic vertebral compression fracture (OVCF). The authors investigated the incidence and risk factors of rib fracture in 284 patients with OVCF using bone scans and evaluated the feasibility as to whether bone scans could be utilized as a useful screening tool. Hot uptake lesions on ribs were found in 122 cases (43.0%). The factors analyzed were age, sex, number and locations of fractured vertebrae, BMD, and compression rates as determined using initial radiography. However, no statistical significances were found. In 16 cases (5.6%), there were concurrent multiple fractures of both the thoracic and lumbar spines not detected by single site MRI. Sixty cases (21.1%) of OVCF with the a compression rate of less than 15% could not be identified definitely by initial plain radiography, but were confirmed by bone scans. It is concluded that a bone scan has outstanding ability for the screening of rib fractures associated with OVCF. Non-adjacent multiple fractures in both thoracic and lumbar spines and fractures not identified definitely by plain radiography were detected on bone scans, which provided a means for determining management strategies and predicting prognosis.
Graphical Abstract
Keywords: Osteoporosis, Spine, Compression Fracture, Rib Fracture, Osteoporotic Fracture
INTRODUCTION
Osteoporosis is a systemic musculoskeletal disease that gradually reduces bone mineral density (BMD) and changes bone microarchitectures (1). Vertebral compression fractures are one of the most common osteoporotic fractures with an incidence of 700,000 cases per year in the United States (2), and in South Korea the incidence of osteoporotic fractures is on the rise (3).
Regarding the treatment of an osteoporotic vertebral compression fracture (OVCF), conservative treatments like bed rest, medication, and braces used to be the norm. However, for persistent-painful OVCF resistant to conservative treatments, percutaneous vertebroplasty and kyphoplasty are now considered the treatments of choice, because both have been demonstrated to achieve satisfactory pain relief in the majority of OVCF patients (4). However, a significant proportion of OVCF patients complain of consistent chest or flank pain (5), and experience no meaningful pain relief even after percutaneous vertebroplasty or kyphoplasty, whereas others experience some relief of back pain, but still suffer from continuous chest or flank pain.
In a previous study, the authors found that rib fractures are one of main causes of persistent chest or flank pain (6). In fact, rib fractures are one of the most common osteoporotic non-vertebral fractures in the elderly (7). And it has been reported that the presence of a rib fracture is associated with an elevated risk of new osteoporotic fractures (8). Therefore, the authors sought to document the frequency of rib fractures in OVCF patients and to identify factors that affect their occurrence by conducting bone scans. In addition, the authors tried to confirm the efficacy of bone scan as a screening tool for OVCF. Therefore, we analyzed cases of non-adjacent multiple fractures unconfirmed by single-site MRI scans due to the co-occurrence of OVCF in the thoracic and lumbar spines. In addition, the authors investigated cases of fractures that might have been overlooked due to the indication of minute reductions in anterior height at initial plain radiography, noting the report that fracture diagnosis is delayed or neglected in about 25 to 50% of OVCF patients (9).
MATERIAL AND METHODS
Subjects
A total of 545 patients with acute OVCF confirmed by MRI or CT underwent percutaneous vertebroplasty or kyphoplasty at our hospital from January 2006 through March 2010 due to unresponsiveness to conservative management. Vertebral compression fractures with osteoporosis and those caused by minor external forces even though bone mineral density (T-score) was greater than -2.5 were considered to be OVCF. 134 of them with a pathologic fracture, prior experience of vertebroplasty or kyphoplasty, or in need of surgical treatment during follow-up were excluded. In addition, hot uptake on a bone scan can last up to 2 yr after fracture (10). Therefore 42 patients with a history of OVCF within the previous 2 yr were excluded to differentiate old fractures, and 85 patients ineligible for a bone scan were also excluded. The remaining 284 patients were subjected to this study.
Evaluation and analysis methods
A single nuclear medicine specialist was in charge of reading bone scan images. Rib fracture occurrence was recorded regardless of how many hot uptakes were present in ribs (Fig. 1). In order to explore factors potentially affecting the presence of rib fracture, the factors analyzed were age, sex, number and locations of fractured vertebrae, the bone mineral density (T-score), and compression rates as determined using initial radiography. Regarding the influence of age, patients were divided into two groups of greater than 80 yr and less than 80 yr, and then into four groups of patients aged under 60 yr, 60-69 yr, 70 to 79 yr, and over 80 yr. In order to determine whether number of fractured vertebrae affected the occurrence of rib fracture, patients were divided into groups based on the presence of a single OVCF or multiple OVCF. Also, analyses were done for thoracic fractures, lumbar fractures, and combined fractures in thoracic & lumbar spines to determine the influence of OVCF site on the presence of rib fractures. To confirm the influence of the bone mineral density, patients with BMD (L1-L4, T-scores) of greater than -2.5 and less than -2.5 were compared. Regarding the initial amount of anterior height loss, patients were divided into two groups of anterior height loss greater than and less than 15%. Pearson's chi-square test was conducted to investigate the correlation between the prevalence of rib fracture and each of the above-mentioned factors. Statistical analysis was performed using SPSS ver. 21.0.
Fig. 1.

Simultaneous rib fractures in patients with OVCF.
The authors then tried to determine the efficacy of a bone scan as a screening test on approaching for OVCF by investigating cases of non-adjacent multiple fractures and minimal height loss fractures. Fractures of non-adjacent sites on the thoracic and lumbar spine were not detected in single site MRI images taken just after trauma, but were detected by a bone scan (Fig. 2). Also, in order to confirm the usefulness of a bone scan for identifying fractures that could be missed by plain radiography, frequencies of compression fracture with less than 15% anterior height loss were investigated among patients with a single OVCF (Fig. 3). Amounts of anterior height loss were assessed by calculating the difference between estimated anterior height of vertebra before fracture occurrence and anterior height determined by initial plain radiography. The mean heights of vertebrae superior and inferior to fractured vertebrae were used to estimate anterior heights of fractured vertebrae before fracture occurrence.
Fig. 2.
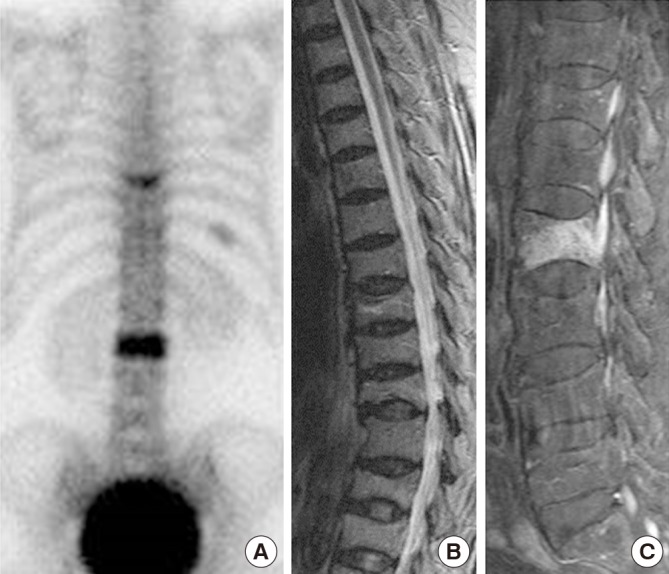
Two-site fractures. (A) Thoracic and lumbar vertebral fractures (hot uptake) in a bone scan. Thoracic (B) and lumbar (C) MRI depicting only one vertebral fracture in the same patient.
Fig. 3.
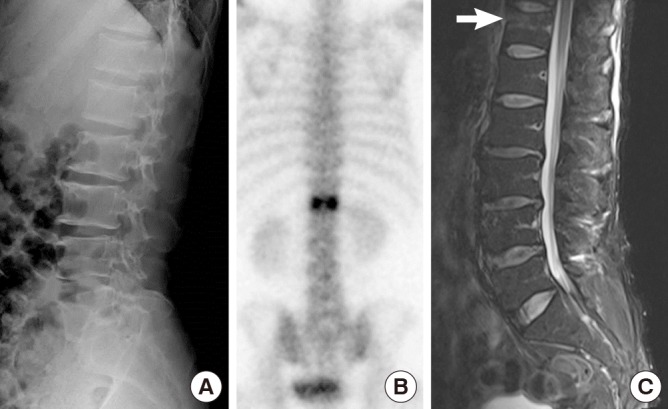
Mild compression fracture by plane radiography. When the amount of anterior height loss associated with a fractured vertebra is less than 15%, the fracture may be overlooked on plane radiographs (A). Vertebral fracture was confirmed by a bone scan (B) and by MRI (C, white arrow).
Ethics statement
The present study was approved by the institutional review board of Gil Medical Center, Gachon University (IRB No. GCIRB2014-349). Informed consent was waived by the board.
RESULTS
Analysis of subjects
Mean patient age was 71.3 (±8.6). The number of patients aged under 60 was 24 (8.5%), while that of patients in their 60s was 82 (28.9%). Patients in their 70s accounted for the largest proportion (129/45.4%) of the study subjects, and 49 patients were over 80 (17.3%). There were 63 (22.2%) males and 221(77.8%) females of mean age 70.1 (±9.2) and 71.4 (±8.4) yr respectively. Average bone mineral density (T-score) was -2.54 (±1.49). Vertebroplasty was performed on 43 of them and kyphoplasty on 241 patients. There were 114 cases of thoracic fracture, 133 cases of lumbar fracture, and 37 cases of both thoracic and lumbar fracture. And there were 204 cases of single fracture (71.8%), 52 cases of two-vertebral fractures (18.3%), and 28 cases of three or more vertebral fractures (9.9%).
Analysis of the frequency of rib fracture and its risk factors
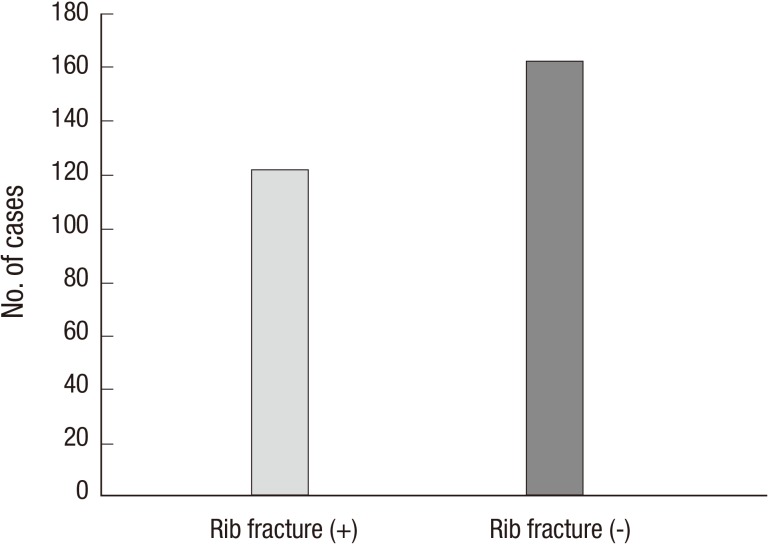
A total of 122 patients (43%) showed hot uptakes in ribs (Fig. 4). When patients were divided into two groups by age, 18 of 49 (36.7%) patients aged over 80 yr and 104 of 235 (44.3%) patients aged under 80 yr had hot uptakes in ribs. When patients were classified into the four groups by age like above, hot uptake in ribs was observed in 9 of 24 (37.5%) in the under 60 yr, in 31 of 82 (37.8%) in the 60-69 yr, in 64 of 129 (49.6%) in the 70-79 yr, and in 18 of 49 (36.7%) in the over 80 yr. In the analysis by sex, 29 of 63 (46.3%) male patients and 93 of 221 (42.1%) females showed hot uptakes in ribs. 85 of 204 (41.7%) in the single vertebral fracture group and 37 of 80 (46.3%) in the multiple vertebral fracture group showed hot uptakes in ribs. When patients were divided into thoracic, lumbar, and both thoracic and lumbar groups by the site of fracture, 51 of 114 (44.7%), 54 of 133 (40.6%), and 17 of 37 (46.0%) had rib fractures. Regarding the bone mineral density, 44.4% (72/162) of those with T-scores (≤-2.5) and 42.6% (52/122) of those with T-scores (>-2.5) showed hot uptakes in the ribs. For initial amounts of anterior height loss, 30 of 60 (50.0%) of those with an anterior height loss of under 15%, and 107 of 224 (47.7%) of those with an anterior height loss of over 15% had rib fractures.
Fig. 4.
Frequency of simultaneous rib fracture.
The above-mentioned analyses showed differences in rib fracture frequencies, but no statistically significant differences were found (Table 1).
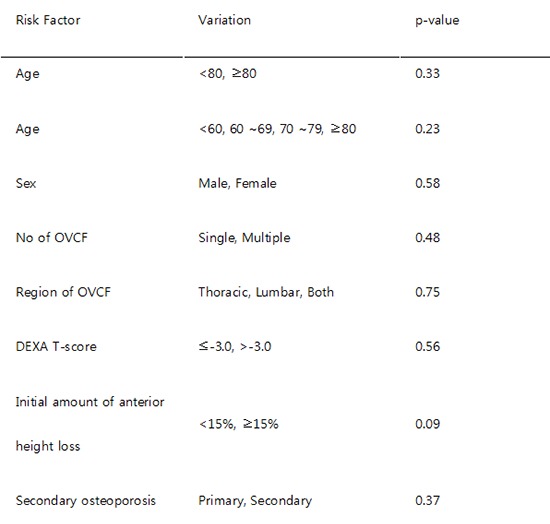
Table 1.
Analysis of risk factors
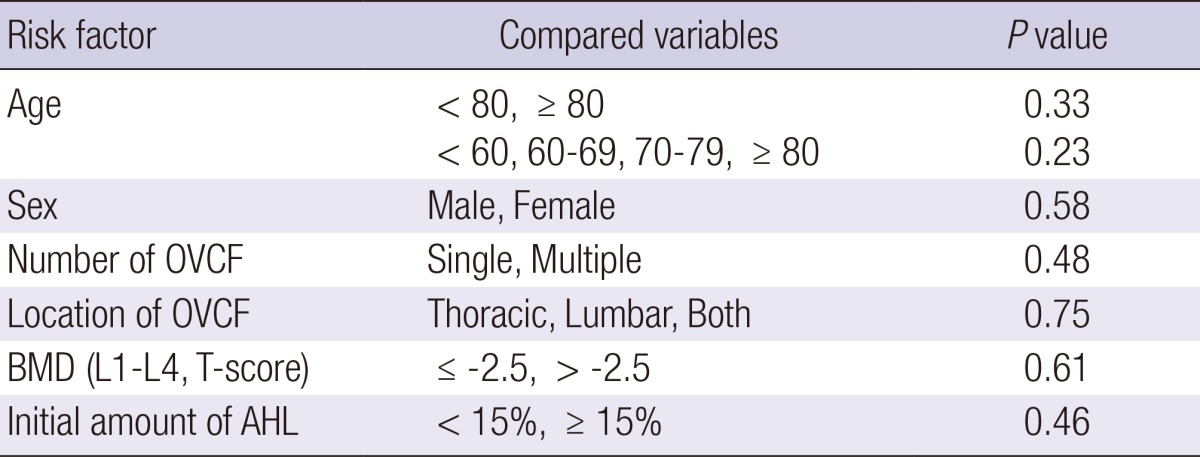
OVCF, osteoporotic vertebral compression fracture; BMD, bone mineral density; AHL, anterior height loss.
Effectiveness of bone scan as a screening test
At our center, thoracic MRI is used to examine C7 to L1 and lumbar MRI to examine T11 to S1. Sixteen (5.6%) patients were scheduled to undergo vertebroplasty or kyphoplasty under the diagnosis of a single site OVCF based on thoracic or lumbar MRI scans. However, hot uptakes in multiple spinal locations were found later by bone scans, and so their treatment plans were changed. In addition, 60 cases (21.2%) not cleared because anterior height losses of under 15% were not recognized definitely by initial plain radiography were confirmed later to have OVCF on bone scan images.
DISCUSSION
In general, the most common sites of osteoporotic fractures are vertebrae, proximal femur, and distal radius. Sontag et al. (11) reported that vertebral fractures and distal radius fractures accounted for 66% of initial osteoporotic fractures in their study on post-menopausal women. Also, proximal femur fractures accounted for a mere 2.2% of initial osteoporotic fractures, and the frequency of rib fracture was higher than that of proximal femur fracture. Barret-Connor et al. (8) in a prospective cohort study found that the rib is the most common site for osteoporotic non-vertebral fractures, and that rib fractures account for around 24% of total fractures. They also reported that a history of rib fracture increased the risks of an additional rib fracture, a hip fracture, or a distal radius fracture by more than two-fold, and thus, highlighted the significance of rib fracture. In a previous study conducted at our center, the frequency of rib fracture in OVCF patients was 57.7% and in the present study the frequency was 43%, which is reaffirming that the rib is a common site for osteoporotic fractures (6). The authors consider that the present study was conducted on patients who had undergone vertebroplasty or kyphoplasty, which is why the frequency rate of rib fracture at our center is high, compared to other studies. Regarding to factors that affect the occurrence of rib fractures, Siris et al. (12) in a cohort study of 170,083 women found that a low BMD increases the risks of all types of osteoporotic fractures, and reported that the risk of OVCF increases with age. Barrett-Connor et al. (8) proposed that an age over 80, a low BMD, a history of fracture before age 50, and injuries from falls are risk factors of rib fracture, but in the present study, no apparent correlation was found between age and rib fracture and no statistical relation was found between BMD and rib fracture. In addition, factors presumed to be correlated with the occurrence of rib fracture, that is, sex, number and locations of fractured vertebrae, and initial amount of anterior height loss, were not found to be statistically significant, but they were associated with rib fracture frequency. Accordingly, further studies are needed on larger number of patients.
To diagnose rib fractures, conventional methods, such as, history-taking, chest PA and rib series are employed, but these methods are considered nonspecific and comparatively inaccurate (13, 14). Diagnostic ultrasonography was introduced to increase the accuracy of recognizing rib fractures, but the technique remains controversial (15). On the other hand, a bone scan has high sensitivity for the diagnosis of occult fractures (16), and for detecting systemic skeletal diseases or metastatic bone tumors (17). Therefore, bone scan is useful for confirming the occurrence of associated diseases in older patients with OVCF. Manyard et al. (10) stressed the usefulness of bone scan as a means for predicting favorable clinical outcomes, based on the rationale that strong hot uptake by bone scan is highly predictive sign of clinical response to vertebroplasty.
MRI is highly sensitive at detecting bone edema induced by micro fracture, which difficult to be recognized on plain radiographs or CT scans (18), and MRI is indispensable for confirming degrees of soft tissue injury like injuries to the posterior ligament complex or an intervertebral disc. However, MRI is usually performed at a single-site due to its cost, which causes to be unable to detect unexpected additional lesions that were no adjacent to OVCF recognized by initial plain radiography. In this regard, bone scan is more useful for the detection of unexpected additional OVCF because it provides whole body images.
In most OVCF cases, fractures are triggered by minor trauma and degrees of vertebrae compression are slight, which makes fractures indistinct on plain radiographs. Delmas et al. (19) in a multi-center study reported that fractures were not diagnosed by initial plain radiography in 29.5-46.5% of patients with a vertebral fracture, and urged surgeons to be cautious when diagnosing OVCF. This is why most surgeons are now conducting imaging studies in addition to plain radiography when diagnosing OVCF. Accordingly, bone scans provide a powerful means of screening for OVCF, considering the shortcomings of MRI mentioned above.
In the present study, the authors were able to confirm the frequency rate of rib fractures radiologically, but clinical assessments based on treatment results and outcomes were not conducted, and thus, additional studies are considered necessary. Regarding problems associated with bone scan, there is a possibility that hot uptakes may be observed for 2 yr after fracture (10), which increases the risk of false positive findings. For this reason, patients with less than a 2-yr history of osteoporotic fractures were excluded from the present study. On the other hand, during the early stage, false negative results can be obtained (20).
Rib fractures do not infrequently accompany OVCF, and when accompanied, chest or flank pain can remain after vertebroplasty or kyphoplasty. Furthermore because rib fracture per se increases the risk of additional osteoporotic fracture, confirmation of its existence is necessary. The authors recommend that bone scans should be performed for the diagnosis of rib fracture accompanying OVCF. And bone scans have outstanding screening ability for patients with concurrent non-adjacent multiple fractures of the thoracic and lumbar spines or fractures not definitively detected by plain radiography.
Footnotes
All authors have no conflicts of interest.
Conception and design of the study: Jun DS, Yu CH. Data preparation: An BK, Yu CH, Hwang KH, Paik JW. Data analysis: Jun DS, An BK, Yu CH. Writing manuscript: Jun DS. Revision: Jun DS, An BK. Data visualization: An BK, Yu CH. Manuscript approval: all authors.
References
- 1.Riggs B, Melton LJ., 3rd Involutional osteoporosis. N Engl J Med. 1986;314:1676. doi: 10.1056/NEJM198606263142605. [DOI] [PubMed] [Google Scholar]
- 2.Melton LJ., 3rd Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976) 1997;22:2S. doi: 10.1097/00007632-199712151-00002. [DOI] [PubMed] [Google Scholar]
- 3.Rowe SM, Chung JY, Yoon TR, Lee JJ, BBae BH, Choi J. An epidomiological study of hip fracture: A comparison between 1991 and 2001. Korean J Bone Metab. 2003;10:109. [Google Scholar]
- 4.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976) 2000;25:923–928. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Patel U, Skingle S, Campbell GA, Crisp AJ, Boyle IT. Clinical profile of acute vertebral compression fractures in osteoporosis. Br J Rheumatol. 1991;30:418–421. doi: 10.1093/rheumatology/30.6.418. [DOI] [PubMed] [Google Scholar]
- 6.Jun DS, Shin WJ, Kim KH. The usefulness of bone scan in the osteoporotic vertebral compression fracture patients treated with kyphoplasty. J Korean Soc Spine Surg. 2008;15:18–22. [Google Scholar]
- 7.Jones G, Nguyen T, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA. Symptomatic fracture incidence in elderly men and women: the Dubbo Osteoporosis Epidemiology Study (DOES) Osteoporos Int. 1994;4:277–282. doi: 10.1007/BF01623352. [DOI] [PubMed] [Google Scholar]
- 8.Barrett-Connor E, Nielson CM, Orwoll E, Bauer DC, Cauley JA. Epidemiology of rib fractures in older men: Osteoporotic Fractures in Men (MrOS) prospective cohort study. BMJ. 2010;340:c1069. doi: 10.1136/bmj.c1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freedman BA, Potter BK, Nesti LJ, Giuliani JR, Hampton C, Kuklo TR. Osteoporosis and vertebral compression fractures-continued missed opportunities. Spine J. 2008;8:756–762. doi: 10.1016/j.spinee.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Maynard AS, Jensen ME, Schweickert PA, Marx WF, Short JG, Kallmes DF. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol. 2000;21:1807–1812. [PMC free article] [PubMed] [Google Scholar]
- 11.Sontag A, Krege JH. First fractures among postmenopausal women with osteoporosis. J Bone Miner Metab. 2010;28:485–488. doi: 10.1007/s00774-009-0144-9. [DOI] [PubMed] [Google Scholar]
- 12.Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, Chen YT. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA) Osteoporos Int. 2006;17:565–574. doi: 10.1007/s00198-005-0027-4. [DOI] [PubMed] [Google Scholar]
- 13.DeLuca SA, Rhea JT, O'Malley TO. Radiographic evaluation of rib fractures. AJR Am J Roentgenol. 1982;138:91–92. doi: 10.2214/ajr.138.1.91. [DOI] [PubMed] [Google Scholar]
- 14.Nevitt MC, Cummings SR, Browner WS, Seeley DG, Cauley JA, Vogt TM, Black DM. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992;135:490–499. doi: 10.1093/oxfordjournals.aje.a116315. [DOI] [PubMed] [Google Scholar]
- 15.Hurley ME, Keye GD, Hamilton S. Is ultrasound really helpful in the detection of rib fractures? Injury. 2004;35:562–566. doi: 10.1016/S0020-1383(03)00263-8. [DOI] [PubMed] [Google Scholar]
- 16.Batillas J, Vasilas A, Pizzi WF, Gokcebay T. Bone scanning in the detection of occult fractures. J Trauma. 1981;21:564–569. doi: 10.1097/00005373-198107000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig H, Kumpan W, Sinzinger H. Radiography and bone scintigraphy in multiple myeloma: a comparative analysis. Br J Radiol. 1982;55:173–181. doi: 10.1259/0007-1285-55-651-173. [DOI] [PubMed] [Google Scholar]
- 18.Spiegl UJ, Beisse R, Hauck S, Grillhösl A, Bühren V. Value of MRI imaging prior to a kyphoplasty for osteoporotic insufficiency fractures. Eur Spine J. 2009;18:1287–1292. doi: 10.1007/s00586-009-1045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557–563. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]
- 20.Sterling JC, Webb RF, Jr, Meyers MC, Calvo RD. False negative bone scan in a female runner. Med Sci Sports Exerc. 1993;25:179–185. [PubMed] [Google Scholar]