Abstract
Introduction
Arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) is a genetic cardiomyopathy that most commonly affects young adults. The most commonly observed reason of death in patients suffering from ARVC/D is sudden cardiac death (SCD). On the other hand, idiopathic right ventricular outflow tract tachycardia (RVOT VT) usually has a benign course. Both of the entities may have ventricular tachycardia (VT) with left bundle branch block (LBBB) pattern and inferior axis. We tried to propose new discriminating electrocardiographic indices for differentiation of foretold entities.
Material and method
This was a retrospective study. We reviewed records of patients admitted between 2003 and 2012 with the diagnosis of either ARVC/D or RVOT VT that presented with VT (LBBB morphology).
Result
A total of fifty nine patients (30 RVOT VT and 29 ARVC/D) were enrolled. In ARVC/D group, men were dominant while the reverse was true of RVOT VT. Palpitation was more common in the RVOT VT group (90% vs. 66.7%), but aborted SCD and sustained VT were more common in ARVC/D group. The new ECG criteria proposed by us mean QRS duration in V1–V3, QRS difference in right and left precordial leads, S wave upstroke duration, JT interval dispersion, QRS and JT interval of right to left precordial leads were all significantly longer in ARVC/D when compared to RVOT VT patients (p < 0.001).
Conclusion
The proposed ECG criteria can be used for non-invasive diagnosis of ARVC/D and incorporation in the future updates of ARVC/D task force criteria.
Keywords: Ventricular tachycardia, Outflow tract, Arrhythmogenic right ventricular cardiomyopathy
1. Introduction
Arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) is characterized by progressive replacement of ventricular myocytes with variable amounts of fibrous and adipose tissue. This patchy involvement is mostly located in right ventricular (RV) inflow–outflow tract and apex, which predisposes patients to ventricular premature depolarization, non-sustained or sustained ventricular tachycardia (VT) and even ventricular fibrillation leading to sudden cardiac death (SCD).1 Accordingly, this condition may lead to superior or inferior axis and left bundle branch block (LBBB) ventricular arrhythmias, which have recently been considered as major and minor criteria respectively.2 On the other hand, idiopathic right ventricular outflow tract (RVOT) arrhythmia occurs with LBBB and inferior axis in the absence of overt structural heart disease and has a more favorable outcome.3
Considering several similarities between the two entities (namely LBBB, inferior axis VT, precipitation of symptoms by exercise and presentation predominantly in young otherwise healthy individuals), but with the strict differences in prognoses and therapeutic options, several diagnostic tools are proposed to differentiate between these two.4–7
However, despite the task force criteria proposed for distinguishing between these two conditions,2 there still exists room for new discriminators. Herein we took this challenge to identify such electrocardiographic discriminators between the two entities.
2. Materials & methods
2.1. Study population
Clinical and electrocardiographic data of all consecutive patients admitted in our hospital from 2003 through 2012 and with a diagnosis of either ARVC/D (classified as affected according to 1994 task force8) or RVOT VT was collected in a preformed data sheet. Twelve-lead electrocardiogram (ECG) recordings taken with Twelve-channel MAC ECG machine in double voltage 20 mm/1 mv and 25 mm/s speed were analyzed by two specialists unaware of patients' history and clinical diagnosis.
Considering the revision made on ARVC/D definition in 2010,2 all patients were re-evaluated after data collection and entered in the study only if they were classified as definite ARVC/D (two major or, one major and two minor criteria) cases as per the new definition. Considering that all these patients were labeled as “definite ARVC/D” as per revised definition of the 2010 task force, no change in number of studied patients happened. Patients with LBBB pattern and inferior axis ventricular arrhythmia were grouped in RVOT VT if they did not have any structural abnormality evident in echocardiography or cine-angiography, and nor could they be classified as ARVC/D. Majority of patients were admitted in hospital electively and were clinically stable.
The rational expression behind these new criteria is based on localized fibrosis in right ventricle in ARVC/D patients compared to RVOT VT patients. Thus, we thought that depolarization or repolarization differences may be important. Specific ECG criteria to be compared in the two groups during normal sinus rhythm were:
-
1)
Mean QRS duration in V1–V3
-
2)
S wave upstroke duration from nadir of S to end of QRS
-
3)
Difference in sum of QRS duration in left and right precordial leads: (QRS duration in V1+V2+V3)–(QRS duration in V4+V5+V6)
-
4)
Ratio of sum of QRS duration in right to left precordial leads: (QRS duration in V1+V2+V3)/(QRS duration in V4+V5+V6)
-
5)
JT interval dispersion: JT interval is measured from the beginning of J point to the end of T wave. For each patient, the difference between maximum and minimum JT intervals was calculated as the JT interval dispersion
-
6)
Ratio of sum of JT interval segment in right to left precordial leads: (JT INTERVAL segment in V1+V2+V3)/(JT INTERVAL segment in V4+V5+V6)
-
7)
Presence of T wave inversion in V1 throughV3.
All stages of study were conducted according to Helsinki declaration.
2.2. Data management and statistical analyses
All data was entered and statistical analyses were performed using SPSS version 16 for windows. A univariate analysis was conducted to compare clinical and electrocardiographic variables of patients with ARVC/D and RVOT VT, using student's T-test for continuous variable and chi-square test for categorical variables. Using a 2 tailed distribution, a p value ≤0.05 was considered significant. For continuous ECG indices, various cut-offs were used and sensitivity and specificity for diagnosing ARVC/D were computed using the 2010 definition of ARVC/D as gold standard.
Based on the computations, we have reported the cut-off that had the highest specificity above 50% and both positive as well as negative predictive values have been reported. Similarly, various cut-offs for ECG indices were used and sensitivity and specificity for diagnosing RVOT VT were computed by considering absence of any structural abnormality in echocardiography or cine-angiography and ruling out of ARVC/D using the 2010 definition,2 as the gold standard filtering criteria. Here also we have reported the cut-off that had the highest specificity above 50% and again both positive as well as negative predictive values have been reported.
3. Results
Fifty nine patients fulfilled criteria for entering the study that included 29 patients with ARVC/D and 30 with RVOT VT. Baseline characteristics of the patients are presented in Table 1. Male predominance, Aborted SCD and sustained VT were more frequent in ARVC/D group (70.4% vs. 23.3%, p < 0.001; 37% vs. 6.7% p = 0.005; 55.6% vs. 13.3%, p < 0.001 respectively), while palpitation was more prevalent among the RVOT VT patients (90% vs. 66.7% p = 0.03).
Table 1.
Baseline characteristics of the study population.
| Characteristics | ARVC/D |
RVOT VT |
p value |
|---|---|---|---|
| n = 29 | n = 30 | ||
| Age (years) Mean ± SD | 41.7 ± 14.4 | 42.7 ± 12.7 | 0.21 |
| Male n (%) | 19 (70.4) | 7 (23.3) | <0.001 |
| Palpitation n (%) | 18 (66.7) | 28 (90) | 0.03 |
| Syncope n (%) | 14 (48.1) | 10 (33.3) | 0.51 |
| Aborted SCD n (%) | 11 (37) | 2 (6.7) | 0.005 |
| Sustained VT n (%) | 16 (55.6) | 4 (13.3) | <0.001 |
Abbreviation: SCD = Sudden cardiac death.
Electrocardiographic (ECG) findings in the two groups are summarized in Table 2. One example of ECG findings is depicted in Fig. 1. As is obvious, electrocardiographic indicators of localized delayed depolarization during normal sinus rhythm (Mean QRS duration in V1–V3, S wave upstroke duration, Difference in sum of QRS duration and JT interval in left and right precordial leads, ratio of sum of QRS duration in right to left precordial leads) have significant differences between the two groups (p value < 0.001). T wave inversion was more common in ARVC/D than in RVOT patients (59.3% vs. 33.3% p = 0.05).
Table 2.
ECG findings during normal sinus rhythm and tachycardia.
| ECG finding | ARVC/D |
RVOT VT |
p Value |
|---|---|---|---|
| n = 29 | n = 30 | ||
| Mean QRS duration in V1–V3 Mean ± SD, Median (range) |
120.7 ± 20.7, 120 (100–120) |
94.3 ± 18.7, 90 (80–100) |
<0.001 |
| S wave upstroke duration in V1 Mean ± SD, Median (range) |
50.7 ± 20.9, 40 (40–60) |
35.6 ± 5, 40 (30–40) |
<0.001 |
| QRS difference in right/left precordial leads Mean ± SD, Median (range) |
48.5 ± 49.2, 30 (0–90) |
8 ± 22.6, 0 |
<0.001 |
| QRS duration in right/left precordial leads Mean ± SD, Median (range) |
1.3 ± 0.7, 1.2 (1.0–1.4) |
1 ± 0.05, 1.0 |
<0.001 |
| JT interval dispersion Mean ± SD, Median (range) |
33.3 ± 34.3, 40 (0–40) |
16 ± 19.9, 0 (0–40) |
0.086 |
| JT interval duration in right/left precordial leads Mean ± SD, Median (range) |
2.2 ± 5.5, 1.1 (1.0–1.5) |
0.9 ± 0.1, 1.0 (1.0–1.0) |
<0.001 |
| T wave inversion in V1–V3 n (%) | 16 (59.3) | 10 (33.3) | 0.05 |
Results are illustrated in number (and percentage in parentheses).
NS = Non significant.
Fig. 1.
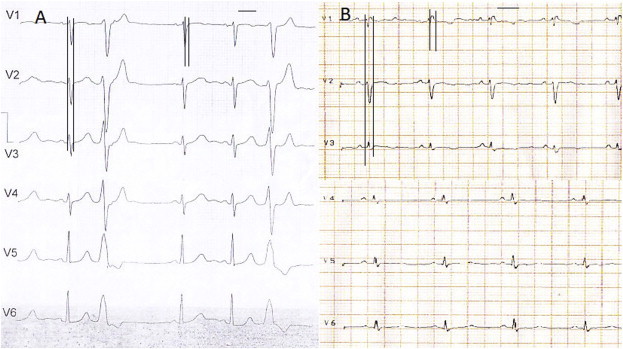
Sample ECG of a patient with RVOT ventricular arrhythmia (A) and ARVC/D patient (B). Mean QRS duration is measured in the first sinus beat which is 90 and 110 ms respectively. In the second sinus beat, S wave upstroke duration from nadir of S to end of QRS is measured which is 40 and 60 ms respectively. In the 3rd sinus beat, JT interval is shown. JT interval duration in right precordial/left precordial leads is 1.16 and 1. Pay attention also to T wave inversion in V1 throughV3 in the second patient.
Out of all the baseline clinical characteristics presented in Table 1, only age and sex could have influenced the outcomes listed in Tables 2 and 3 . Age distribution was similar for both the groups in our study. On the other hand, although women exhibited more repolarization changes than men, gender of the patient wasn't found to have any impact on the outcome in multivariate analysis. Sensitivity, specificity and positive and negative predictive values of indices are summarized in Tables 3 and 4 and Fig. 1.
Table 3.
Statistical accuracy using new depolarization and repolarization indices in normal sinus rhythm for differentiating ARVC/D from RVOT VT patients.
| ECG finding | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Mean QRS duration in V1-3 ≥105 ms | 72 | 78 |
| S wave upstroke duration in V1 ≥55 ms | 30 | 100 |
| QRS difference in right and left precordial leads ≥35 | 52 | 85 |
| QRS duration in right precordial/left precordial ≥1.17 | 63 | 94 |
| JT interval duration in right precordial/left precordial ≥1.15 | 48 | 97 |
| T wave inversion in V1 through V3 | 59.3 | 65.6 |
Table 4.
Statistical accuracy for diagnosis of ARVC/D using new indices.
| ECG variable | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| QRS difference in right and left precordial leads >35 & QRS duration in right precordial/left precordial >1.17 | 51.9 | 93.8 | 87.5 | 69.5 |
| QRS duration in right precordial/left precordial >1.17 & JT interval duration in right precordial/left precordial >1.15 | 37 | 100 | 100 | 64 |
NPV = Negative predictive value, PPV = positive predictive value.
4. Discussion
Despite the road map illustrated by revised task force in 2010,2 absence of overt abnormalities on imaging leads to difficulties in diagnosis of ARVC/D. This becomes more challenging because good imaging modalities are still not available in all the institutions. Considering fibro fatty deposition of RV and resultant depolarization and repolarization abnormalities, our objective was to investigate if ECG criteria could be used to differentiate RVOT VT from ARVC/D patients.
Our finding of male predominance among ARVC/D patients compared to idiopathic RVOT counterparts (70% vs. 23.3%) was consistent with previous reports,9,10 although ARVC/D patients in our study were older than previously reported studies (41.7 vs. 34–38 years old).4,5,10 Palpitations were more frequent in RVOTVT patients, which was as expected owing to the benign nature of disease.9 Ventricular ectopy or non-sustained ventricular arrhythmia in ambulatory ECG holter monitoring was also seen very often.3,5
Syncope was more prevalent in ARVC/D patients with structurally abnormal heart, probably due to the limited cardiovascular reserve in these patients which makes them intolerant to tachycardia.5,10 The difference however wasn't statistically significant as the overall number of such patients was relatively small.5 Not unexpectedly, SCD, consequent of polymorphic VT or preceding ventricular fibrillation, was more common in ARVC/D group.1,10 Importantly, there were two patients with RVOT VT who had sudden cardiac death, which emphasizes that sudden death, though rare, can occur in these patients as well.5
In revised ARVC/D task force criteria, ECG of sinus rhythm and arrhythmia were incorporated.2 Except for the epsilon wave, prolonged S wave upstroke and T wave inversion, other ECG evidences of localized depolarization and repolarization were found to be lacking.
Stefan Peters et al11,12 described the prevalence and significance of localized indices of QRS prolongation in ARVC/D patients compared to general population. Using ROC curve, Mean QRS duration in right precordial leads ≥105 ms (milliseconds), was found to be present in 78% of ARVD patients in our study with specificity of 78%, which is in accordance with findings by Stefan Peters et al.12 Terminal activation duration of QRS ≥55 ms, was present in 30% of ARVC/D patients but had specificity of 100%, which leads to a good accuracy for differentiation them from a RVOTVT patient. Differential QRS duration in right and left precordial leads can be another discriminator favoring ARVC/D in patients with LBBB pattern and inferior axis VT. The quotient of (Mean QRS width in right precordial)/(Mean QRS width in left precordial leads) >1.17 had sensitivity of 63% and specificity of 94% while this was present in 98% of patients in a previous study. This was probably due to higher quality of their ECG acquisition and better delineation of the end of QRS.
Besides the previously addressed indices, we found two new indices in our study: QRS duration difference in right and left precordial leads & JT interval duration in right precordial/left precordial leads. We observed that these two had statistically significant difference (p < 0.001) and can be used as discriminating parameters. Cut-off point of 35 ms difference between right and left precordial leads had 85% specificity for ARVC/D. To the best of our knowledge, these parameters have not been mentioned before.
As could be anticipated, the inhomogeneity in RV texture leads to repolarization differences, which is manifested on ECG as JT interval differences along right and left precordial leads. The quotient of right over left precordial JT intervals ≥1.15 had 97% specificity for diagnosis of ARVC/D. May be this is another cause for electrical instability and is the harbinger of polymorphic VT and VF being more common in ARVC/D than RVOT VT patients.
Although JT dispersion was illustrated before in a variety of conditions,13 it has not been considered in ARVC/D. We thought that measuring cumulative localized JT interval in right compared to left precordial leads would be more pronounced as a differentiating criterion than just the difference of maximum from minimum JT interval (JT dispersion) which is subjected to more intra-observer and inter-observer errors.13 This may explain why JT interval dispersion >50 ms was not different between two studied groups but the JT interval duration in right precordial/left precordial ≥1.15 had the power for differentiation (Specificity = 97%).
We thought that combination of depolarization index (QRS duration) and repolarization index (JT interval) in right versus left ventricle, as evidenced by right versus left precordial, leads may be a significant difference between both the patient groups. Putting the evidences together, the significance of these variables is found to be higher for differentiation of ARVC/D from RVOT VT, as evidenced with high specificity and positive predictive value in Table 4. This would be more underscored when compared with invasive myocardial biopsy, which is 67% sensitive and 92% specific for ARVC/D.14
5. Conclusion
The findings of the present study corroborate the importance of ECG to differentiate ARVC/D from RVOT VT and could stimulate further analysis of ECG abnormalities, underlying localized right precordial ECG abnormalities and mechanisms of arrhythmogenesis.
6. Study limitation
The current article is based on a retrospective study conducted for a relatively small sample size from a single center. Further studies that involve larger sample of patients selected prospectively are required to confirm the present findings. On the basis of this retrospective study, we could describe the ECG characteristics that appeared to be useful in distinguishing the RVOTVT/PVC from VT or PVC in the case of ARVD. The validity of these criteria arising from our cohort should be validated in a prospective study.
Conflicts of interest
All authors have none to declare.
References
- 1.Thiene G., Nava A., Corrado D. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med. 1988;318:129–133. doi: 10.1056/NEJM198801213180301. [DOI] [PubMed] [Google Scholar]
- 2.Marcus F., McKenna W.J., Sherrill D. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D): proposed modification of the task force criteria. Circulation. 2010 Apr 6;121:1533–1541. doi: 10.1161/CIRCULATIONAHA.108.840827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goy J.J., Tauxe F., Former M. Ten-year follow-up of 20 patients with idiopathic ventricular tachycardia. Pacing Clin Electrophysiol. 1990;13:1142–1147. doi: 10.1111/j.1540-8159.1990.tb02172.x. [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth C.D., Skanes A.C., Klein G.J., Gula L.J., Yee R., Krahn A.D. Differentiating arrhythmogenic right ventricular cardiomyopathy from right ventricular outflow tract ventricular tachycardia using multilead QRS duration and axis. Heart Rhythm. 2006;3:416–423. doi: 10.1016/j.hrthm.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 5.Niroomand F., Carbucicchio C., Tondo C. Electrophysiologic characteristics and outcome in patients with idiopathic right ventricular arrhythmia compared with arrhythmogenic right ventricular dysplasia. Heart. 2002;87:41–47. doi: 10.1136/heart.87.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morin D.P., Mauer A.C., Gear K. Usefulness of precordial T wave inversion to distinguish arrhythmogenic right ventricular cardiomyopathy from idiopathic ventricular tachycardia arising from the right ventricular outflow tract. Am J Cardiol. 2010;105:1821–1824. doi: 10.1016/j.amjcard.2010.01.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boulous M., Lashevsky I., Gespstein L. Usefulness of electroanatomical mapping to differentiate between right ventricular outflow tract tachycardia and arrhythmogenic right ventricular dysplasia. Am J Cardiol. 2005;95:935–940. doi: 10.1016/j.amjcard.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 8.McKenna W.J., Thiene G., Nava A., on behalf of the Task Force of the working group myocardial and pericardial disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology Diagnosis of arrhythmogenic right ventricular dysplasia cardiomyopathy. Br Heart J. 1994;71:215–218. doi: 10.1136/hrt.71.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwai S., Cantillon D.J., Kim R.J. Right and left ventricular outflow tract tachycardias: evidence for a common electrophysiologic mechanism. J Cardiovasc Electrophysiol. 2006 Oct;17:1052–1058. doi: 10.1111/j.1540-8167.2006.00539.x. [DOI] [PubMed] [Google Scholar]
- 10.Nava A., Bauce B., Basso C. Clinical profile and long-term follow-up of 37 families with arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2000 Dec;36:2226–2233. doi: 10.1016/s0735-1097(00)00997-9. [DOI] [PubMed] [Google Scholar]
- 11.Peters S., Trümmel M., Koehler B. QRS fragmentation in standard ECG as a diagnostic marker of arrhythmogenic right ventricular dysplasia-cardiomyopathy. Heart Rhythm. 2008 Oct;5:1417–1421. doi: 10.1016/j.hrthm.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Peters S., Trümmel M., Koehler B., Westermann K.U. The value of different electrocardiographic depolarization criteria in the diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Electrocardiol. 2007 Jan;40:34–37. doi: 10.1016/j.jelectrocard.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu H., Ohnishi Y., Inoue T., Yokoyama M. QT and JT dispersion in patients with monomorphic or polymorphic ventricular tachycardia/ventricular fibrillation. J Electrocardiol. 2001 Apr;34:119–125. doi: 10.1054/jelc.2001.23361. [DOI] [PubMed] [Google Scholar]
- 14.Angelini A., Basso C., Nava A. Endomyocardial biopsy in arrhythmogenic right ventricular cardiomyopathy. Am Heart J. 1996;132:203–206. doi: 10.1016/s0002-8703(96)90416-0. [DOI] [PubMed] [Google Scholar]


