Abstract
Background and Objectives
Little information is available regarding adult patients with congenital heart disease (CHD) who needed unscheduled hospitalization (USH). This paper aims to elucidate the clinical features of adult patients with CHD requiring USH.
Subjects and Methods
Study subjects included patients with CHD aged 18 years or older who were hospitalized at our facility during a 5-year study period. Medical records were retrospectively reviewed and data regarding USH were collected. Patient's background, underlying heart disease, cause of hospitalization, and prognosis (second USH regardless of cause or death) were examined.
Results
Overall, 959 CHD patients underwent a total of 1761 hospitalizations, including 145 patients who were unexpectedly hospitalized 239 times. The median age at USH was 27 years old. Of the 959 patients, 54% were male. Underlying heart diseases included repaired tetralogy of Fallot (21%), single ventricular physiology after Fontan operation (17%), and Eisenmenger syndrome (12%). The causes of USH included arrhythmia (40%), heart failure (20%), infectious disease (13%), and hemorrhage or thrombus (13%). A total of 48 patients required readmission. In total, 13 patients died, including four hospital deaths. The USH-free survival rate was 77% for 1 year and 58% for 3 years.
Conclusion
The rate of USH was high for adults with complicated CHD. Common causes of USH included arrhythmia, heart failure, hemorrhage-related or thrombus-related conditions and infection. These data provide the current status of medical care for adult CHD patients in Japan and their therapeutic needs.
Keywords: Heart defects, congenital; Hospitalization; Aging
Introduction
Due to advancements in various noninvasive diagnostic methods, surgical treatments, and intensive care, many patients with congenital heart disease (CHD) can survive into adulthood. At present, the numbers of adult patients with CHD in the USA, Europe, and Japan are estimated to be 1 million,1) 1.2 million,2) and 400000,3) respectively. These figures are expected to increase in the future.4) Naturally, most CHD patients remain uncured, requiring lifelong follow-up because they often have residual lesions and/or sequelae after corrective surgery.1),5) In fact, mortality6) and morbidity7) in adult patients with CHD is high. Incidence of hospitalization in these patients has been shown to be higher4) than that in the general population. Therefore, the incidence of unscheduled hospitalization (USH) is also expected to be high in adult patients with CHD, although little information is available regarding adult patients with CHD who needed USH.8,9),10),11) The term USH referred to emergent hospitalization of patients who needed immediate diagnostic workup or therapy. Hospitalization to general ward and intensive care units were included in this study. However, overnight stays at emergency room were excluded. The objective of this study was to elucidate the clinical features of adult patients with CHD requiring USH.
Subjects and Methods
Subjects
Study subjects included CHD patients aged 18 years or older who were hospitalized at our facility during a 5-year study period from January 2005 to December 2009. Medical records were studied retrospectively. Data regarding USH were collected. Chronological trends in USH, patient background, underlying heart disease, cause of hospitalization, and prognosis (second USH regardless of cause or death) were examined. Scheduled hospital admissions and outpatient care cases were excluded. Because some patients required several USHs, the number of patients differed from the number of hospitalizations. Some patients had repeated USHs due to the same cause. For such cases, the initial USH during the study period was examined.
Heart disease
There were eight different underlying heart diseases according to morphological diagnosis (Table 1). Single ventricular physiology (SVP)-Fontan included patients who underwent Fontan operation, whereas SVP-non Fontan included SVP patients who did not undergo Fontan operation regardless of the reason. Underlying heart diseases were divided into simple or complex CHDs according to the type of heart disease, intervention, and residual lesion.1)
Table 1. Clinical characteristics of adult patients with congenital heart disease requiring unscheduled hospitalization.
| USH | Total hospitalization | |||
|---|---|---|---|---|
| Patients (n=145) | Admissions (n=239) | Patients (n=959) | Admissions (n=1761) | |
| Age at 1st admission (years) | 27 (18-82) | |||
| 18-19 | 15 (10) | |||
| 20-29 | 69 (48) | |||
| 30-39 | 26 (18) | |||
| 40-49 | 11 (8) | |||
| 50-59 | 12 (8) | |||
| 60-69 | 10 (7) | |||
| 70- | 2 (1) | |||
| Male gender | 79 (54) | |||
| CHD diagnosis | ||||
| SVP-Fontan | 24 (17) | 43 (18) | 78 (8) | 180 (10) |
| SVP-non fontan | 8 (6) | 12 (5) | 24 (3) | 57 (3) |
| TOF | 31 (21) | 42 (18) | 99 (10) | 193 (11) |
| TGA | 11 (8) | 22 (9) | 42 (4) | 92 (5) |
| VSD | 11 (8) | 17 (7) | 47 (5) | 63 (4) |
| ASD | 14 (10) | 23 (10) | 389 (41) | 686 (39) |
| Eisenmenger syndrome | 18 (12) | 39 (16) | 48 (5) | 142 (8) |
| Others | 28 (19) | 41 (17) | 232 (24) | 348 (20) |
| Intervention | ||||
| Corrective surgery | 101 (79) | |||
| Palliative surgery | 9 (6) | |||
| CI | 3 (2) | |||
| No surgery/CI | 32 (22) | |||
Values are n (%). USH: unscheduled hospitalization, SVP: single bentricular physiology, TOF: tetralogy of Fallot, TGA: transposition of great arteries, VSD: ventricular septal defect, ASD: atrial septal defect, CI: catheter intervention
Cause of unscheduled hospitalization
Causes of USH were classified into arrhythmia, heart failure, infectious disease, hemorrhage or thrombus, neurological abnormality, and other causes. Arrhythmia included supraventricular tachycardia, ventricular tachycardia, junctional tachycardia, and atrioventricular block confirmed by 12-lead electrocardiography. Palpitations were not identified on 12-lead electrocardiography because the symptoms had disappeared by the time the patient was examined for palpitations. Heart failure included patients with acute decompensated heart failure (AHF), renal failure (RF), and protein-losing enteropathy (PLE). Patients with orthopnea, nocturnal dyspnea, pulmonary congestion, increased edema, or cardiac dilation were classified as AHF. However, deteriorated cardiac function due to arrhythmia was classified as arrhythmia. RF referred to a threefold or greater increase in serum creatinine levels above the baseline due to poor hemodynamics. Drug-induced RF {e.g., due to angiotensin-converting enzyme inhibitor (ACEI) administration} was excluded. PLE referred to the loss of proteins from the gastrointestinal tract which was confirmed by intestinal scintigraphy and the observation of edema and/or ascites and hypoalbuminemia. Infectious diseases were divided into infectious endocarditis (IE) and others (non-IE). According to Duke's criteria,12) both "definite IE" and "possible IE" were included as IE.
Prognosis
We investigated the duration of hospitalization for patients who survived up to the time they were discharged from hospital. We also reviewed the incidence of death, presence/absence of heart transplant or heart/lung transplant, and the incidence of second USH. We calculated post-discharge survival and USH-free survival rates. We also compared survival and USH-free survival rates between simple and complex CHD groups. An event was considered as either death or to a second USH regardless of the cause. The impact of clinical indicators in USH-free survival rate was examined. Clinical indicators included age, gender, hemodynamics (biventricular physiology vs. SVP), ventricular ejection fraction (ejection fraction ≥60% vs. <60%) on echocardiogram or ventriculography at the time of discharge, type B natriuretic peptide levels, and the presence of oral treatments (diuretic agents, β-blockers, ACEI/angiotensin receptor blockers, anticoagulants, digitalis, and antiarrhythmics).
Statistics
Data are expressed as n (%), median, and range. The survival rate was assessed using Kaplan-Meier method. Cox regression analysis was used to assess event predictive factors. Significant differences observed by univariate analysis were assessed by multivariate analysis. JMP 10 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. Statistically significant difference was considered when p was less than 0.05.
Results
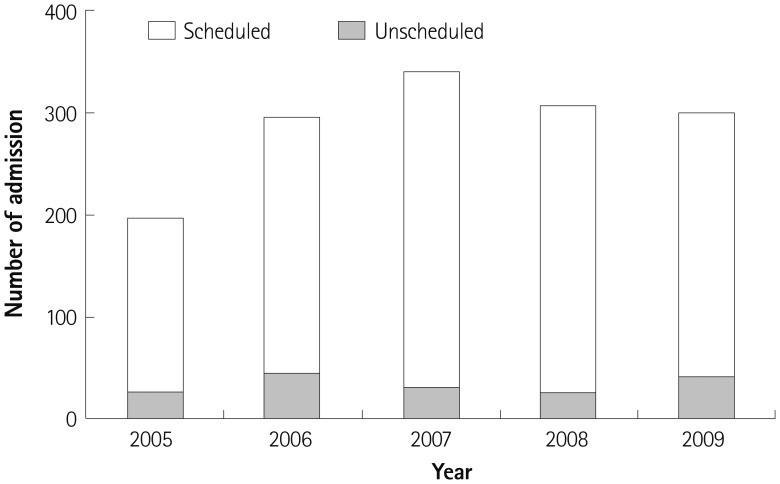
During the period of this study, 959 adult CHD patients were hospitalized a total of 1761 times. Of these, 145 patients were unexpectedly hospitalized 239 times (Table 1). No patient was newly diagnosed as CHD during index hospitalizations. The median age at USH was 27 years of age (range, 18-82 years). Of the 959 patients, 54% were male. Young people (18-29 years of age) comprised 58% of all subjects. No obvious increase in the total number of hospitalizations or in the number of USHs was observed during the study period (Fig. 1).
Fig. 1. The number of scheduled and unexpected hospitalizations from 2005 to 2009.
Underlying heart disease
Clinical characteristics of adult patients with CHD requiring USH are summarized in Table 1. There were 31 (21%) cases of repaired Tetralogy of Fallot (TOF), 24 (17%) cases of SVP-Fontan, and 18 (12%) cases of Eisenmenger syndrome. Complex heart diseases comprised 79% of the underlying heart disease. Corrective operations were performed in 101 (70%) cases. Palliative operations were performed in 9 (6%) cases. Three (2%) cases underwent catheter intervention. Surgical or catheter intervention was performed at least once in 113 (78%) patients.
Cause of unscheduled hospitalization
Causes of USH are summarized in Table 2. Arrhythmia was the most frequent cause at 40%. Arrhythmia was further classified into supraventricular arrhythmia (79%) and ventricular tachycardia (14%). Heart failure accounted for 20% of all UEH. AHF, PLE, and RF accounted for 83%, 14%, and 3% of USH, respectively. Infectious disease made up 13% of USH cases, of which IE made up 42%. Hemorrhage or thrombus accounted for 13% of USH. Hemoptysis, warfarin-related hemorrhage/bleeding tendency, and thrombus accounted for 58%, 26%, and 11%, respectively, of all hemorrhage or thrombus cases.
Table 2. Causes for unscheduled hospitalization.
| Patients (n=145) | |
|---|---|
| Arrhythmia | 60 (41) |
| Supraventricular tachycardia | 48 |
| Ventricular tachycardia | 8 |
| Junctional tachycardia | 2 |
| Complete atrioventricular block | 1 |
| Palpitation | 1 |
| Heart failure | 29 (20) |
| Acute decompensated heart failure | 24 |
| Protein loosing enteropathy | 4 |
| Renal failure | 1 |
| Infection | 18 (12) |
| IE | 8 |
| Non-IE | 10 |
| Hemorrhage | 18 (12) |
| Hemoptysis | 11 |
| Bleeding tendency | 5 |
| Thrombus | 2 |
| Neurological problem | 5 (3) |
| Others | 15 (10) |
Values are n (%). IE: infectious endocarditis
Underlying disease and unscheduled hospitalization causes
Underlying CHDs as causes of USH are summarized in Table 3. Emergency hospitalization due to arrhythmia was the most common ones, of which TOF accounted for 30% of cases whereas SVP accounted for 26%, including 18% Fontan cases and 8% non-Fontan cases. In HF, over one-third cases were caused by SVP (Fontan 21%, non-Fontan 7%), followed by Eisenmenger syndrome at 17%. Hospitalizations for infectious diseases also included TOF cases (28%). Hemorrhage-related admissions included Eisenmenger syndrome (39%) and TOF (17%).
Table 3. Proportion of underlying congenital heart disease as cause of unscheduled hospitalization.
| Arrhythmia (n=60) | Heart failure (n=29) | Infection (n=18) | Hemorrhage (n=18) | Neurological (n=5) | Others (n=15) | |
|---|---|---|---|---|---|---|
| SVP-Fontan | 11 (18) | 6 (21) | 1 (6) | 2 (11) | 0 (0) | 3 (20) |
| SVP-non fontan | 5 (8) | 2 (7) | 0 (0) | 0 (0) | 1 (20) | 0 (0) |
| TOF | 18 (30) | 2 (7) | 5 (28) | 3 (17) | 1 (20) | 2 (13) |
| TGA | 5 (8) | 2 (7) | 0 (0) | 1 (6) | 1 (20) | 2 (13) |
| VSD | 3 (5) | 1 (3) | 3 (17) | 2 (11) | 0 (0) | 2 (13) |
| ASD | 6 (10) | 3 (10) | 3 (17) | 1 (6) | 1 (20) | 0 (0) |
| Eisenmenger | 0 (0) | 5 (17) | 3 (17) | 7 (39) | 1 (20) | 2 (13) |
| Others | 12 (20) | 8 (28) | 3 (17) | 2 (11) | 0 (0) | 4 (27) |
Values are n (%). SVP: single ventricular physiology, TOF: tetralogy of Fallot, TGA: transposition of great arteries, VSD: ventricular septal defect, ASD: atrial septal defect
Prognosis
Four individuals died during their first hospitalization, and three admitted in hospital at the time of final evaluation. The characteristics of 139 individuals who were discharged with survival are summarized in Table 4. The median duration of hospitalization was 23 days. A total of 48 individuals required second USH. In total, 13 patients died during the study period. No patients underwent heart transplant or heart/lung transplant. Analysis of the length of hospitalization for each different cause of hospitalization revealed that subjects admitted for HF required longer hospital stays (35 days). There were high rates of hospital readmission (59%) and mortality (30%) among these subjects (Table 5). For subjects admitted due to arrhythmia and those with hemorrhage-related admissions, readmission rates (32% and 39%, respectively) were also high, but the mortalities (5% and 6%, respectively) were not.
Table 4. Clinical characteristics of patients at discharge.
| All patients (n=138) | Patients with USH (n=51) | Patients without USH (n=87) | |
|---|---|---|---|
| NYHA class | |||
| 1 | 72 (52) | 17 (33) | 55 (63) |
| 2 | 44 (32) | 23 (45) | 21 (24) |
| 3 | 21 (15) | 10 (20) | 11 (13) |
| 4 | 1 (1) | 1 (2) | 0 (0) |
| Ejection fraction (n=125) | |||
| ≥0.6 | 83 (66) | 32 (70) | 51 (65) |
| <0.6 | 42 (34) | 14 (30) | 28 (35) |
| BNP (n=122) | 64 (5.8-1300) | 96 (5.8-1300) | 51 (11-636) |
| Medication | |||
| Diuretics | 88 (64) | 42 (82) | 46 (53) |
| Beta blocker | 39 (28) | 15 (29) | 24 (28) |
| ACEI/ARB | 39 (28) | 16 (31) | 23 (26) |
| Anticoagulant | 65 (47) | 26 (51) | 39 (45) |
| Digitalis | 43 (31) | 22 (43) | 21 (24) |
| Antiarrhythmic | 45 (32) | 15 (29) | 30 (34) |
Values are n (%), or median (range). NYHA: New York Heart Association, BNP: B type natriuretic peptide, ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin II receptor blocker
Table 5. Prognosis of ACHD requiring USH.
| Total (n=145) | Arrhythmia (n=60) | Heart failure (n=29) | Infection (n=18) | Hemorrhage (n=18) | Neurological (n=5) | Others (n=15) | |
|---|---|---|---|---|---|---|---|
| Hospital stay (days) | 23 | 24 | 35 | 27 | 16 | 19 | 11 |
| Death during hospital stay, n (%) | 4 (3) | 2 (3) | 2 (7) | ||||
| Follow up period after discharge (years) | 2.6 | 2 | 2.4 | 2.2 | 2.9 | 3.7 | 3.3 |
| Readmission, n (%) | 48 (35) | 18 (32) | 16 (59) | 3 (17) | 7 (39) | 1 (20) | 3 (20) |
| Death during study period, n (%) | 13 (9) | 3 (5) | 8 (30) | 1 (6) | 1 (7) |
ACHD: adult patients with congenital heart disease, UEH: unexpected hospitalization
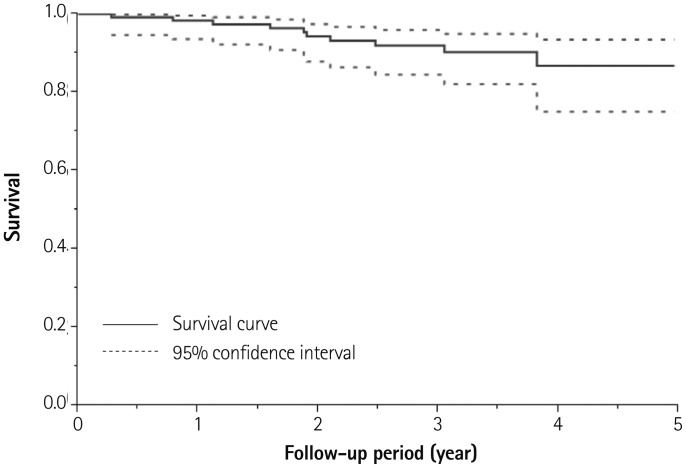
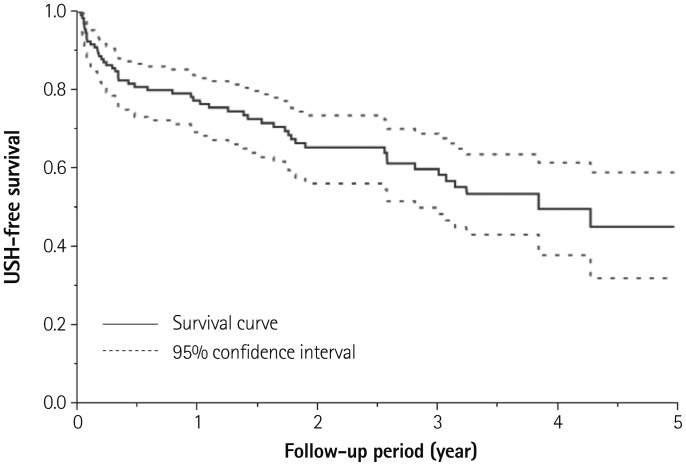
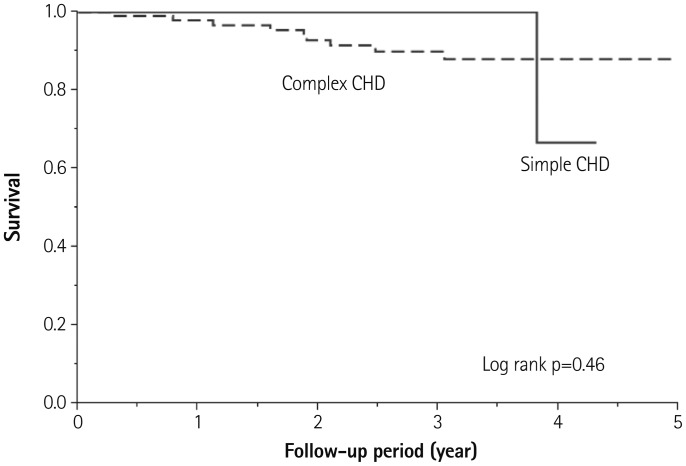
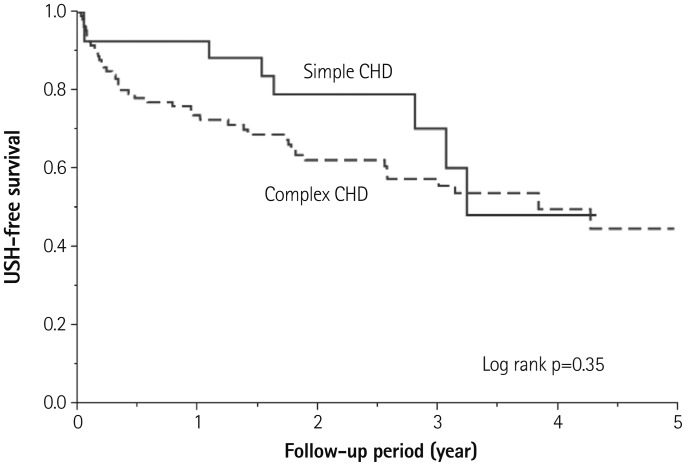
The survival rate calculated by the Kaplan-Meier method was 98% at 1 year and 91% at 3 years (Fig. 2). The rate of USH-free survival was 77% at 1 year and 58% at 3 years (Fig. 3). Survival and USH-free survival rate were comparable between simple and complex CHDs (Figs. 4 and 5). Multivariate Cox regression analysis revealed that diuretics use at discharge was an independent predictor of USH (hazard ratio: 2.59; 95% confidence interval: 1.19-6.23; p< 0.05) (Table 6).
Fig. 2. Kaplan-Meier curve of survival after discharge.
Fig. 3. Kaplan-Meier curve of USH-free survival after discharge. USH: unscheduled hospitalization.
Fig. 4. Kaplan-Meier survival estimates for survival between simple CHD and complex CHD. CHD: congenital heart disease.
Fig. 5. Kaplan-Meier survival estimates for USH-free survival between simple CHD and complex CHD. USH: unscheduled hospitalization, CHD: congenital heart disease.
Table 6. Univariate and multivariate analysis for predictors of USH-free survival.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| Age | 1.02 | 1.00-1.03 | 0.09 | |||
| Male gender | 0.97 | 0.56-1.69 | 0.91 | |||
| SVP | 1.64 | 0.87-2.94 | 0.12 | |||
| Reduced EF | 0.78 | 0.40-1.43 | 0.43 | |||
| BNP per 10 pg/mL | 1.01 | 1.00-1.02 | 0.05 | 1.01 | 1.00-1.02 | 0.20 |
| Diuretics | 3.05 | 1.55-6.71 | <0.01 | 2.59 | 1.19-6.23 | <0.05 |
| Beta blocker | 1.18 | 0.62-2.12 | 0.6 | |||
| ACEI/ARB | 1.04 | 0.56-1.85 | 0.9 | |||
| Anticoagulation | 1.52 | 0.87-2.66 | 0.14 | |||
| Antiarrhythmics | 0.98 | 0.52-1.76 | 0.95 | |||
| Digitalis | 2.32 | 1.31-4.05 | <0.01 | 1.53 | 0.82-2.85 | 0.18 |
USH: unscheduled hospitalization, HR: hazard ratio, CI: confidence interval, SVP: single ventricular physiology, EF: ejection fraction, BNP: B type atriuretic peptide, ACEI: angiotensin converting enzyme, ARB: angiotensin II receptor blocker
Discussion
This study revealed the clinical characteristics of adult patients with CHD requiring USH at a single Japanese facility. USH constituted 14% of all hospital admissions. Young patients (median age, 26 years) with complex heart malformations were unexpectedly hospitalized emergently due to various cardiovascular diseases (e.g., arrhythmia or heart failure) and noncardiovascular diseases (e.g., infection or hemorrhage/thrombus). The median duration of hospital stay was 23 days. The mortality rate was not high despite a high incidence of readmission.
Compared to reports from Europe,9),10) the rate of USH in our study was low. Although a long period of hospital stay was required for patients in this study, there were only a few hospital deaths (3%). The age, underlying heart disease, and causes of USH were similar. The relatively low USH rate may have been a reflection of the fact that there were many scheduled hospitalizations for regular hemodynamic evaluation by cardiac catheterization at this facility. These hospitalizations occurred mainly in complex heart disease cases, especially after a Fontan operation.13) For asymptomatic cases, the effect of intervention based on hemodynamic evaluations needs to be examined further. The differences observed in the duration of hospital stay and mortality rate might have been influenced by differences in health care and insurance systems as well as being related to treatment policies.
In terms of cardiovascular disease-related causes of USH, arrhythmia and heart failure were common. In terms of noncardiovascular disease-related causes of USH, infection and hemorrhage/thrombus were common. These findings were consistent with earlier reports.9),10)
The most common USH were related to arrhythmia. In addition, TOF and SVP were frequently observed in these patients. Initial treatments were mostly similar to those in patients having other heart diseases. However, arrhythmia in CHD patients may occur due to postoperative incision line, residua, or complications in addition to underlying heart disease.5),14),15) Information on hemodynamic characteristics of the condition is required for the long-term management of CHD. In this study, readmission to hospital was observed in one-third of adult CHD cases requiring USH. The cause of readmission was often a relapse of arrhythmia (data not shown). To avoid readmission to the hospital due to arrhythmia, in addition to drug therapy, electrophysiological studies and catheter ablation, interventions for hemodynamic abnormalities, such as pulmonary valve replacement in TOF16) and total cavopulmonary connection conversion with concomitant arrhythmia surgery17) in atriopulmonary connection Fontan should be actively considered.
In USH for heart failure, SVP and Eisenmenger were often observed. Readmission and death were common. The main pathology observed in AHF in acquired heart disease is left ventricular failure.18) However, AHF in adult patients with CHD differed greatly, i.e., in addition to left ventricular failure, right ventricular failure and failed Fontan circulation were the main pathological conditions.19) The affected right ventricle may be in the subpulmonary or systemic position. Therefore, appropriate management is required after accurately understanding the hemodynamic characteristics of CHD, similar to that in the management of arrhythmia. Following standard practices for acquired heart disease, we administered pharmacological therapy such as β-blocker and renin-angiotensin-based inhibitor administration, and nonpharmacological therapy such as cardiac resynchronization therapy in adult CHD patients with heart failure;14),20) however, the effects of these therapies were limited, suggesting that an evidence-based treatment strategy needs to be constructed for adult CHD patients with specific hemodynamics.
Similar to acquired heart disease, transplantation is considered as a means to treat refractory heart failure in adult patients with CHD.21) However, transplantation for adult patients with CHD is very rarely performed in Japan due to extremely low number of donors. In fact, this study included no patient who underwent heart transplant or heart/lung transplant. Transplantation is expected to increasingly become a treatment choice for heart failure in adult patients who have CHD.
Adult CHD patients with complex hemodynamics and complications due to various underlying diseases and treatments were unexpectedly hospitalized. Therefore, a wide range of diagnostic and treatment approaches such as high-intensity echocardiography, catheterization intervention (angioplasty, valvuloplasty, and coil embolization), electrophysiological examinations, scintigraphy, and imaging modalities are needed.9) In order to manage the condition while bearing the quality of patient's life in mind, we need to understand the problems that have a significant effect in the lives of adult CHD patients, such as pregnancy, insurance, and employment. Therefore, the cooperation of adult CHD specialist-based medical team including echocardiographers, interventionists, electrophysiologists, radiologists, cardiac surgeons, and obstetricians is essential.
In Japan, specialists in pediatric cardiology are often responsible for the treatment of adult patients with CHD, whereas in North America and Europe, adult CHD cardiologists from the adult cardiovascular department often collaborate with specialists in pediatric cardiology to provide treatment.22) In particular, adult CHD with complex heart malformations affects extremely young population. Therefore, the number of adult patients with CHD will not only increase rapidly in future, but also will continue to age. The prevalence of age-related coronary heart disease, hypertension, and glucose-and lipid-related metabolic disorders as well as associated risk factors, is increasing. Consequently, Japan needs an adult CHD medical treatment system in which pediatric cardiologists specializing in CHD hemodynamics and adult cardiologists specializing in acquired heart disease can collaborate.
Limitations
This study has certain limitations. First, it was a retrospective study conducted at a single centre, including a small patient population. In addition, only patients admitted into the Department of Pediatric Cardiology and Cardiovascular Medicine were enrolled as subjects. Patients from the departments of internal medicine, neurology, surgery, or obstetrics and gynecology were not included. A larger-scale study that enrolls patients from other hospital departments is needed to clarify therapeutic issues in adult CHD patients.
Conclusions
This study revealed the clinical characteristics of adult patients with CHD requiring USH at a single institution in Japan. Young population with underlying complex heart malformations required USH for the following reasons: arrhythmia, heart failure, infection, hemorrhage, or thrombus-related problems. They showed a high rate of readmission to the hospital and, to a certain extent, mortality rate. These data revealed the current status of medical care for adult CHD patients. Our data also indicated future therapeutic needs for providing optimal medical care to such adult CHD patients in Japan.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Warnes CA, Liberthson R, Danielson GK, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–1175. doi: 10.1016/s0735-1097(01)01272-4. [DOI] [PubMed] [Google Scholar]
- 2.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–172. doi: 10.1161/CIRCULATIONAHA.106.627224. [DOI] [PubMed] [Google Scholar]
- 3.Shiina Y, Toyoda T, Kawasoe Y, et al. Prevalence of adult patients with congenital heart disease in Japan. Int J Cardiol. 2011;146:13–16. doi: 10.1016/j.ijcard.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 4.Verheugt CL, Uiterwaal CS, van der Velde ET, et al. The emerging burden of hospital admissions of adults with congenital heart disease. Heart. 2010;96:872–878. doi: 10.1136/hrt.2009.185595. [DOI] [PubMed] [Google Scholar]
- 5.Perloff JK, Warnes CA. Challenges posed by adults with repaired congenital heart disease. Circulation. 2001;103:2637–2643. doi: 10.1161/01.cir.103.21.2637. [DOI] [PubMed] [Google Scholar]
- 6.Verheugt CL, Uiterwaal CS, van der Velde ET, et al. Mortality in adult congenital heart disease. Eur Heart J. 2010;31:1220–1229. doi: 10.1093/eurheartj/ehq032. [DOI] [PubMed] [Google Scholar]
- 7.Engelfriet P, Boersma E, Oechslin E, et al. The spectrum of adult congenital heart disease in Europe: morbidity and mortality in a 5 year follow-up period. The Euro Heart Survey on adult congenital heart disease. Eur Heart J. 2005;26:2325–2333. doi: 10.1093/eurheartj/ehi396. [DOI] [PubMed] [Google Scholar]
- 8.Opotowsky AR, Siddiqi OK, Webb GD. Trends in hospitalizations for adults with congenital heart disease in the U.S. J Am Coll Cardiol. 2009;54:460–467. doi: 10.1016/j.jacc.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 9.Kaemmerer H, Fratz S, Bauer U, et al. Emergency hospital admissions and three-year survival of adults with and without cardiovascular surgery for congenital cardiac disease. J Thorac Cardiovasc Surg. 2003;126:1048–1052. doi: 10.1016/s0022-5223(03)00737-2. [DOI] [PubMed] [Google Scholar]
- 10.Kaemmerer H, Bauer U, Pensl U, et al. Management of emergencies in adults with congenital cardiac disease. Am J Cardiol. 2008;101:521–525. doi: 10.1016/j.amjcard.2007.09.110. [DOI] [PubMed] [Google Scholar]
- 11.Gurvitz MZ, Inkelas M, Lee M, Stout K, Escarce J, Chang RK. Changes in hospitalization patterns among patients with congenital heart disease during the transition from adolescence to adulthood. J Am Coll Cardiol. 2007;49:875–882. doi: 10.1016/j.jacc.2006.09.051. [DOI] [PubMed] [Google Scholar]
- 12.Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96:200–209. doi: 10.1016/0002-9343(94)90143-0. [DOI] [PubMed] [Google Scholar]
- 13.Ohuchi H, Ono S, Tanabe Y, et al. Long-term serial aerobic exercise capacity and hemodynamic properties in clinically and hemodynamically good, "excellent", Fontan survivors. Circ J. 2012;76:195–203. doi: 10.1253/circj.cj-11-0540. [DOI] [PubMed] [Google Scholar]
- 14.Warnes CA. The adult with congenital heart disease: born to be bad? J Am Coll Cardiol. 2005;46:1–8. doi: 10.1016/j.jacc.2005.02.083. [DOI] [PubMed] [Google Scholar]
- 15.Ghai A, Harris L, Harrison DA, Webb GD, Siu SC. Outcomes of late atrial tachyarrhythmias in adults after the Fontan operation. J Am Coll Cardiol. 2001;37:585–592. doi: 10.1016/s0735-1097(00)01141-4. [DOI] [PubMed] [Google Scholar]
- 16.Miyazaki A, Sakaguchi H, Ohuchi H, et al. Efficacy of hemodynamicbased management of tachyarrhythmia after repair of tetralogy of Fallot. Circ J. 2012;76:2855–2862. doi: 10.1253/circj.cj-12-0208. [DOI] [PubMed] [Google Scholar]
- 17.Hiramatsu T, Iwata Y, Matsumura G, Konuma T, Yamazaki K. Impact of Fontan conversion with arrhythmia surgery and pacemaker therapy. Eur J Cardiothorac Surg. 2011;40:1007–1010. doi: 10.1016/j.ejcts.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 18.Sato N, Kajimoto K, Asai K, et al. Acute decompensated heart failure syndromes (ATTEND) registry. A prospective observational multicenter cohort study: rationale, design, and preliminary data. Am Heart J. 2010;159:949–955. doi: 10.1016/j.ahj.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 19.Trojnarska O. Heart failure in the adult patient with congenital heart disease. Cardiol J. 2007;14:127–136. [PubMed] [Google Scholar]
- 20.Shaddy RE, Webb G. Applying heart failure guidelines to adult congenital heart disease patients. Expert Rev Cardiovasc Ther. 2008;6:165–174. doi: 10.1586/14779072.6.2.165. [DOI] [PubMed] [Google Scholar]
- 21.Seddio F, Gorislavets N, Iacovoni A, et al. Is heart transplantation for complex congenital heart disease a good option? A 25-year single centre experience. Eur J Cardiothorac Surg. 2013;43:605–611. doi: 10.1093/ejcts/ezs350. discussion 611. [DOI] [PubMed] [Google Scholar]
- 22.Niwa K, Perloff JK, Webb GD, et al. Survey of specialized tertiary care facilities for adults with congenital heart disease. Int J Cardiol. 2004;96:211–216. doi: 10.1016/j.ijcard.2003.06.019. [DOI] [PubMed] [Google Scholar]