Abstract
Background
Many community dwelling individuals with schizophrenia do not take medications regularly and, thus, are prone to frequent relapses.
Aim
Evaluate the effectiveness of self-management training on adherence to medications and relapse among individuals with chronic schizophrenia living in the community.
Methods
A total of 201 individuals with chronic schizophrenia living in the urban and rural communities of Shanghai Municipality were randomized into a treatment as usual control group (n=98) or a selfmanagement intervention group (n=103) that received weekly self-management skills training for 6 months followed by 24 months of monthly group booster sessions in which a community health worker reviewed patients’ self-management checklists. Two psychiatrists blind to the treatment status of patients, assessed adherence to medications using the Morisky Medication Adherence Scale and patients’ insight into their illness using the Scale to Assess Unawareness of Mental Disorders (SAUMD) at baseline and 30 months after baseline. A total of 194 individuals (95.6%) completed the study.
Results
There were no differences between groups at baseline, but after 30 months the intervention group had significantly better medication compliance, significantly greater insight into their illness, and (by self-report) were using significantly higher dosages of antipsychotic medication. Only 2 (1.9%) of the 103 intervention group participants relapsed (i.e., experienced one or more re-hospitalizations) over the 30 months of follow-up, but 14 (14.3%) of the 98 control group subjects relapsed (X2=8.83, p=0.003).
Conclusions
Given the large sample size, relatively long follow-up, randomized design, and single-blind evaluation of outcomes the dramatic reduction in relapse and improvements in medication adherence and insight identified in this study are robust findings. These results extended our previous findings, which demonstrated the benefit of self-management training on improving the symptoms and social functioning of individuals with chronic schizophrenia living in the community. Cost-benefit studies are now needed to assess the feasibility of up-scaling this self-management intervention to a wide range of communities.
Keywords: schizophrenia, community mental health services, medication adherence, insight, relapse, re-hospitalization, randomized controlled trial, China
Abstract
背景
许多社区精神分裂症患者服药不规律因而很容易频繁复发。
目的
评估自我管理培训对社区慢性精神分裂症患者服药依从性和复发情况的影响。
方法
共纳入上海市城市和农村的社区慢性精神分裂症患者201例,随机分为常规治疗组(n=98)或自我管理干预组(n=103)。干预组接受为期6个月的每周一次自我管理技能培训,之后参加每月一次的加强小组会议,由社区卫生工作者检查患者的自我管理清单,共24个月。由两名单盲于患者治疗情况的精神科医生使用Morisky服药依从性量表评估患者服药依从性并采用自知力评估量表(Scale to Assess Unawareness of Mental Disorders,SAUMD)了解基线时和30个月后患者的自知力。总共194人(95.6%)完成研究。
结果
基线时两组间无显著差异,但在30个月后,干预组服药依从性比常规治疗组好,对疾病的自知力提高,自我报告使用抗精神病药物的剂量相对高。在随访30个月里,干预组103例患者中只有2例(1.9%)复发(即一次或多次住院),然而对照组98例患者中有14例(14.3%)复发(X2=8.83, p=0.003)。
结论
本研究样本量大、随访时间相对长、随机设计并采用单盲法评估,研究结果的说服力相对强。本研究发现自我管理干预后患者复发显著减少、服药依从性改善以及自知力提高。这些结果拓展了我们先前的研究发现,显示自我管理训练可以有效改善社区慢性精神分裂症患者的症状和社会功能。今后需要纳入成本效益分析研究,评估将自我管理干预扩大到其他更多社区的可行性。
1. Introduction
Schizophrenia is a mental disorder with a high relapse rate and high levels of disability. There are an estimated 16 million individuals with schizophrenia in China.[1] A previous study found that the symptoms of schizophrenia re-occurred in approximately 50% of individuals within one year after remission of the previous episode and 85% of individuals relapse within five years of the previous episode.[2] The prevention of relapse depends heavily on the proper use of antipsychotic medications, but the level of medication adherence among communitydwelling residents with mental disorders is only about 30%.[3] One reason for poor medication adherence in China is the underdeveloped state of the community mental health services, so many individuals with schizophrenia lack medical supervision.[4] Promotion of self-management strategies that stress the proactive participation of the affected individual themselves is one potential way to deal with this problem that, if effective, could cover a large proportion of community dwelling individuals with chronic mental illnesses.[5] Mental disorders share many features with chronic physical illnesses in terms of the course of disease and the rehabilitation process. Individuals with mental disorders that have remitted are usually able to carry out self-management activities.[6] A study in 2006 by Yuan and colleagues found better medication adherence after selfmanagement training among a group of inpatients with schizophrenia.[7] A follow-up study by Li and colleagues in 2009 found similar results one year after discharge.[8]
The current report is a secondary analysis of a previously reported randomized controlled trial[9] of self-management training for community dwelling individuals with chronic schizophrenia. The initial report demonstrated that self-management training can improve symptoms and social functioning over a 30-month follow-up period. The current paper reports on the effect of self-management training on medication adherence and relapse.
2. Methods
2.1. Sample
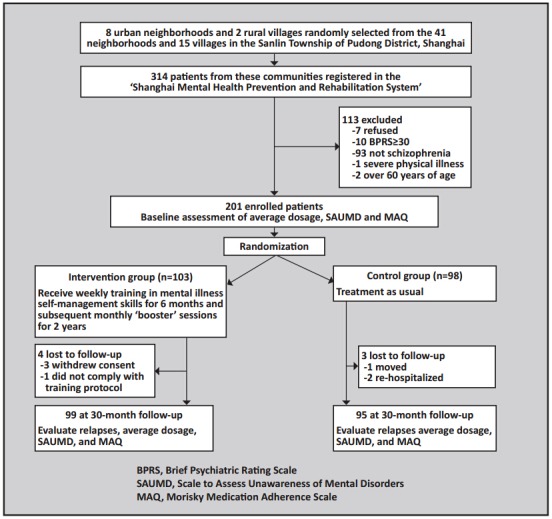
As shown in Figure 1, participants in this study were from 10 randomly selected communities, in the Sanlin Township of Pudong District in Shanghai. All 314 individuals in this township enrolled in the ‘Shanghai Mental Health Prevention and Rehabilitation System’ as of July 2011 were sent a letter with information about the aims and methods of the study inviting them to participate. Enrolled participants met the following inclusion and exclusion criteria: (a) met the diagnostic criteria for schizophrenia according to the Chinese Classification of Mental Disorders, 3rd edition (CCMD-3),[10] (b) 18 to 60 years of age, (c) had a middle school education or higher, (d) had relatively stable symptoms (Brief Psychiatric Rating Scale [BPRS][11] score <30), (e) had no severe physical diseases, and (f) provided written informed consent (signed by the participant and the guardian). After excluding the 113 individuals who refused or did not meet the inclusion criteria, the remaining 201 individuals were randomly assigned (by the toss of a coin) to the intervention group (n=103) or the control group (n=98). Among these participants, 99 (96.1%) in the intervention group and 95 (96.9%) in the control group completed the 30-month follow-up assessment. The 4 dropouts in the intervention group dropped out at the 2nd, 8th, 16th and 18th months of follow-up; the 3 dropouts in the control group dropped out at the 7th, 24th, and 28th months.
Figure 1. Flowchart of the study.
The study was approved by the Ethics Committee of the Pudong Yingbo Community Health Service Center.
2.2. Self-management training group
A previous report provided a detailed description of the training process.[9] In brief, the training manual included the Medication Management and Symptom Management modules of the ‘UCLA Social & Independent Living Skills program’[12] and information from other available sources. These modules focus on helping participants understand the importance of adhering to medications and of recognizing residual symptoms and early signs of relapse. Weekly 2-hour training sessions were provided to groups of 20 to 25 participants from the intervention group for six months. Skills were taught using a combination of didactic instruction, group interactions, role-played rehearsals, and group discussions. The 99 participants in the intervention group who completed the 30-month follow-up attended an average (sd) of 21.8 (2.0) of the 24 weekly sessions.
Upon completion of the six-months of training, participants received a ‘self-management checklist journal’ to record their daily adherence to medications, quality of sleep, occurrence of side effects, occurrence of residual symptoms and early signs of relapse, daily activities, and general mood. In most cases completion of this journal was monitored by a co-resident family member. Participants also attended monthly selfmanagement group meetings (‘booster sessions’). The 99 participants who completed the 30-month follow-up attended an average (sd) of 22.4 (1.5) of the 24 monthly sessions.
2.3. Treatment-as-usual control group
Individuals assigned to the control condition received regular outpatient treatment with medication and routine monitoring of medication adherence and clinical status by community mental health workers.
2.4. Assessments
Medication adherence refers to the degree to which an individual correctly follows medical advice. The revised version of the 4-item Morisky Medication Adherence Scale (MAQ)[13] was used to assess the adherence to medications. The four items are (1) “Do you ever forget to take your medicine?” (2) Are you careless at times about taking your medicine?” (3) When you feel better do you sometimes stop taking your medicine?” (4) “Sometimes if you feel worse when you take your medicine, do you stop taking it?” Items of the original western scale were binary (yes or no); we revised the items to be rated on a 0-4 Likert scale representing five levels varying from ‘never’ to ‘always’. The theoretical range in score of the four items is 0 to 16, with higher scores representing poorer adherence. This revised Chinese scale has previously been used to assess compliance in chronic physical illness[14] and in mental illness.[15] The internal consistency of the four items is good (Cronbach α=0.76).[14]
The 20-item Scale to Assess Unawareness of Mental Disorders (SAUMD)[16] was used to assess the insight of the participant. There are four subscales of the SAUMD assessing the awareness of current symptoms, awareness of past symptoms, attribution of current symptoms, and attribution of past symptoms. Every item is rated on a 1-5 Likert scale with higher scores indicating poorer insight. A previous study in China[17] reported that the scale has good test-retest reliability: intraclass correlation coefficient ICC for the total score was 0.81 and that for the four subscale scores ranged from 0.70 to 0.89.
Average dosage of antipsychotics was based on the participants’ self-report information and presented as chlorpromazine-equivalent dosage in milligrams per day. Relapse is defined as one or more hospital admissions for treatment of schizophrenia during the 30-month follow-up period.
The MAQ, SAUMD and average daily dosage of medication were assessed at baseline and the end of the study (2.5 years after enrollment) by two trained psychiatrists who were blind to the treatment status of participants. The agreement between the two psychiatrists was good: the ICC for the independent evaluation of 30 patients by thetwo coders was 0.79 for the total SAUMD score and 0.73 of the total MAQ score. To maintain the blinding throughout the study treating clinicians were not present during the evaluations, the two evaluators did not participate in any of the training sessions, and the two evaluators were specifically instructed not to ask participants about their participation in the study.
To limit measurement errors, whenever an evaluation resulted in a score for the MAQ or SAUMD that was more than 3 standard deviations above or below the group mean, a re-assessment by the second evaluator was conducted; if the difference between the two assessments was small, the first score was retained, if the difference was large, expert opinion was sought to arrive at a final score. Scores by the first evaluator were outside these 3 standard deviation limits only 5 times during the study (0.63% of all evaluations). In three of these cases the original score was retained and in two cases a revised score was used.
2.4. Analysis
Intention-to-treat analysis was conducted using the last observation value carried forward method. Means and standard deviations were used to describe continuous variables; repeated measures analysis of variance with adjustment for post-hoc comparisons using the least significant difference (LSD) method to estimate the overall and between-group effects. Paired t-tests were used for within-group comparisons. Categorical variables were compared using χ2 tests. The level of statistical significance was set at 0.05. All tests were two-tailed.
3. Results
3.1. Comparisons at baseline
As shown in Table 1, there were no differences in demographic characteristics between participants in the intervention and control groups. There were also no differences between groups in terms of age of onset, duration of illness and number of hospitalizations. Most of the participants were chronically ill, with a mean duration of illness of 17.4 years, and had had multiple hospitalizations.
Table 1.
Comparison of demographic characteristics of the individuals in the self-management (intervention) group and treatment as usual (control) group
| intervention group (n=103) |
control group (n=98) |
statistics | p | |
|---|---|---|---|---|
| Male, n (%) | 55 (53.4%) | 51 (52%) | χ2=0.03 | 0.825 |
| Age, mean (sd) | 35.3 (9.6) | 34.7 (9.9) | t=0.92 | 0.334 |
| Years of schooling, mean (sd) | 9.7 (2.6) | 9.7 (2.8) | t=0.06 | 0.978 |
| Marital status, n (%) | ||||
| currently married | 55 (53.4%) | 50 (51.0%) | ||
| never married | 41 (39.8%) | 43 (43.9%) | χ2=0.96 | 0.591 |
| no longer married | 7 (8.0%) | 5 (5.1%) | ||
| Age of onset, mean (sd) | 22 (5.4) | 23 (6.1) | t=1.29 | 0.162 |
| Duration of illness in years, median (IQR) | 17 (9-24) | 18 (0-24) | Za=1.64 | 0.314 |
| Number of hospitalizations, mean (sd) | 2.2 (0.9) | 2.1 (0.9) | t=1.57 | 0.179 |
aMann-Whitney rank test was used for the comparison
Table 2 shows that the baseline scores on MAQ and the total and subscale scores on SAUMD were not significantly different between the intervention and control groups. Table 3 shows that the mean chlorpromazine-equivalent dosage of medication at baseline was not significantly different between the two groups.
Table 2.
Comparisons of mean (sd) SAUMD and MAQ scores between the intervention and control groups
| Baseline | 30-month follow-upa | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| intervention (n=103) |
control (n=98) |
Fb | p | intervention (n=103) |
control (n=98) |
Fb | p | ||
| SAUMD | |||||||||
| awareness of current symptoms | 11.2 (6.1) | 10.6 (5.4) | 0.53 | 0.462 | 8.7 (5.4) | 11.14 (5.7) | 11.34 | <0.001 | |
| awareness of past symptoms | 10.3 (7.6) | 11.8 (6.8) | 2.16 | 0.143 | 8.3 (5.6) | 10.35 (6.7) | 11.54 | <0.001 | |
| attribution of current symptoms | 12.4 (8.4) | 12.5 (6.4) | 1.25 | 0.262 | 11.1 (6.7) | 12.39 (7.2) | 6.14 | 0.014 | |
| attribution of past symptoms | 12.6 (7.6) | 11.2 (7.2) | 1.80 | 0.182 | 10.4 (6.1) | 11.67 (6.8) | 4.35 | 0.038 | |
| total score | 45.5 (21.1) | 44.2 (23.2) | 1.88 | 0.172 | 38.4 (23.1) | 45.6 (18.6) | 39.87 | <0.001 | |
| MAQ | |||||||||
| total score | 11.4 (2.7) | 11.1 (3.1) | 1.15 | 0.251 | 10.7 (2.1) | 11.6 (2.4) | 7.69 | 0.006 | |
SAUMD, Scale to Assess Unawareness of Mental Disorders; MAQ, Morisky Medication Adherence Scale
aThis was an intention-to-treat analysis; the last observed value (i.e., the value at baseline) was carried forward and used as the 30-month follow-up value for the 4 subjects who dropped out of the intervention group and for three subjects who dropped out of the control group
bF-value of the post-hoc between-group differences. The overall repeated measures ANOVA models for each of the six measures considered were all statistically significant (p<0.05).
3.2. Comparisons at the end of the 30-month study
As shown in Table 2, at the end of the study the overall medication adherence score (MAQ), the overall insight score (SAUMD), and each of the four insight subscale scores were all significantly better in the intervention group than in the control group. The drop in the scores of two SAUMD subscales about awareness of current and past symptoms was greater than the drop in the scores of the two SAUMD subscales about the attribution of current and past symptoms.
Table 3.
Comparisons of mean (sd) chlorpromazine-equivalent daily dosages (in mg) of antipsychotic medication between the intervention and control groupsa at baseline and at the 30-month follow-up
| Intervention group (n=103) | Control group (n=98) | t | p | ||
|---|---|---|---|---|---|
| daily dose in mg mean (sd) |
daily dose in mg mean (sd) |
||||
| baseline | 184 (27) | 192 (31) | 1.34 | 0.181 | |
| follow-upb | 203 (28) | 187 (30) | 3.91 | 0.001 |
aBefore and after comparison of the intervention group, paired-t=4.15, p<0.001; before and after comparison of the control group, paired-t=0.66, p=0.255; for the overall repeated measures analysis of variance F=9.54, p=0.002
bThis was an intention-to-treat analysis; the last observed value (i.e., the value at baseline) was carried forward and used as the 30-month follow-up value for the 4 subjects who dropped out of the intervention group and for three subjects who dropped out of the control group
As shown in Table 3, by the end of the study, the intervention group reported taking a higher average chlorpromazine-equivalent dosage of antipsychotic medication than the control group. The reported dosage had increased significantly from baseline in the intervention group but not in the control group.
Over the 30-month follow-up period 2 of the 103 individuals (1.9%) in the intervention group relapsed (1 was re-hospitalized once and one was re-hospitalized twice) and 14 of the 98 individuals (14.3%) in the control group relapsed (each of them was re-hospitalized once). This difference in relapse rate was statistically significant ( χ2=8.83, p=0.003).
4. Discussion
4.1. Main findings
This randomized controlled trial in a large sample of individuals with schizophrenia living in both urban and rural communities that used a rigorously blinded evaluation of outcomes found that weekly training in self-management skills for six months followed by monthly booster sessions can significantly decrease relapse rates and substantially improve medication adherence and insight into the illness. Many studies have convincingly demonstrated that low medication adherence is the main reason for high rates of relapse in individuals with chronic schizophrenia.[18],[19],[20] Thus any intervention than can convincingly improve medication adherence is quite important. The large size, long follow-up, randomized design, and blind assessment of outcomes employed in this study make the identified improvement in medication compliance all the more important. In combination with the findings of the first report from this study[9] – showing improved symptoms and social functioning with self-management training – this is a dramatic finding that merits widespread promulgation.
The mechanism underlying these improvements remains unclear. The self-management intervention is associated with at least four distinct but inter-related outcomes – decreased symptoms, improved social functioning, enhanced insight about the illness, and increased adherence to medications. At this point it is not possible (and may never be possible) to determine which of these four outcomes are primary and which are secondary. It is also not possible to deconstruct the intervention to identify the active component that directly stimulates change. In addition to the social support network engendered by the weekly group meetings in the first 6 months and monthly meetings thereafter, patients’ daily use of a detailed ‘self-management journal’ can serve as a long-term, self-directed support system that encourages them to adhere to their regimen. The daily records in the journal also help patients recognize their prodromal symptoms, negative moods, and sleeping problems, which presumably improves their insight about the illness.
4.2. Limitations
Several issues need to be considered when assessing the importance of these rather dramatic findings. (a) Participants in the intervention group had substantially more contact with medical staff (as they participated in the training) than those in the control group so it is not possible to definitively attribute the improved outcomes to the training, it could also be due to the ‘placebo effect’ of increased contact with staff members. (b) Assessment of medication adherence and the dosage of medication were dependent on patients’ self-reports (not on objective measures). Participants in the intervention group may have been more motivated to appear at interview as if they were compliant. (c) The relapse measure, defined as one or more hospitalizations, was fairly objective, but it is possible that the increased contact with staff in the intervention group – not patients’ self-management – allowed for earlier recognition and intervention to avert re-hospitalization. (d) The cross-sectional outcome at 30 months following-baseline may not reflect the average level of adherence and insight over the entire followup period. (e) The higher self-reported medication dosage at 30 months in the intervention group may not necessarily represent higher adherence because we did not assess the prescribed level of medication in the two groups. (f) Finally, as we pointed out in the previous report on this study,[9] the sample only included individuals with chronic schizophrenia who were registered in the municipal monitoring system of persons with severe mental disorder and who did not have acute symptoms (i.e., BPRS total score <30). The very low attrition seen in the study (3.5% over 30 months) is likely related to their registration in the program. Future studies with less selective samples are needed to determine the effectiveness of this selfmanagement training in the larger population of all community dwelling individuals with schizophrenia.
Some follow-up research will be need to address these limitations, but we believe that the very robust main finding of the study will remain intact even after full consideration of these potentially confounding factors.
4.3. Implications
Given the generally poor outcomes and frequent relapses of individuals with chronic schizophrenia, this self-management intervention could potentially result in a major improvement in the quality of life of individuals living with schizophrenia. We believe that the success of this program in the Chinese environment (where almost all patients live with family members) depends on the willingness of patients to make the effort to learn self-management skills, the support of co-resident family members, and the enthusiastic participation of mental health professionals and other medical staff. The next step is to develop mechanisms to up-scale this intervention and to conduct cost-effectiveness studies to demonstrate the benefits of the intervention to individuals with schizophrenia, their families, and the community at large.
Biography

Bin Zhou obtained an associate degree in Preventive Medicine from Tongji University in 2003 and a bachelor’s degree in Family Medicine from Fudan University in 2010. He is an attending public health doctor at the Department of Preventive Health Care of Yingbo Community Health Service Center where he has been working since 2010. His main research interest is the community rehabilitation of mental disorders.
Funding Statement
This study was funded by the Shanghai Municipal Health Bureau Young Investigator Grant (20114y028).
Conflict of interest: The authors declare no conflict of interest related to this manuscript.
Ethical review: The study was approved by the Ethics Committee of the Pudong Yingbo Community Health Service Center.
Informed consent: All participants or their guardians provided written informed consent to participate in this study.
References
- 1.Qi L. [Sociological analysis of the mental disorders].. 2006; 12(1): 84-86. Chinese. Lin Chuang Xin Shen Ji Bing Za Zhi. 2006;12(1):84–86. Chinese. [Google Scholar]
- 2.Mao PX, Tang YL, Chen Q, Wang Y, Luo J, Xu Y, et al. [The analysis of the Schizophrenia patients’ awareness on disease recurrence and its related factors] Zhongguo Xin Li Wei Sheng Za Zhi. 2004;18(4):264–268. Chinese. [Google Scholar]
- 3.Hu XL, Ou Yang DX, Li XH. [The situation and analysis of medication compliance on mental illness] Yi Yao Dao Bao. 2011;30(5):685–688. Chinese. [Google Scholar]
- 4.Zhang SJ, Wang JG. [The survey on Shanghai community mental health services] Lin Chuang Jing Shen Yi Xue Za Zhi. 2010;20(2):138–139. Chinese. [Google Scholar]
- 5.Zhang LL, Dong JQ. [Progress in the self-management in patients with chronic diseases] Zhongguo Man Xing Bing Yu Fang Yu Kong Zhi. 2010;8(8):207–211. Chinese. [Google Scholar]
- 6.Bilsker D. Self-management in the mental health field. Visions: British Columbia’s Mental Health Journal. 2003;18:4–5. [Google Scholar]
- 7.Yuan JL. [Effect of medicine self-control skill training on firstepisode female schizophrenic patients] Jian Yan Yi Xue Yu Lin Chuang. 2009;6(6):5–7. Chinese. [Google Scholar]
- 8.Li HW, Su XF. [Impact of self-management training for the rehabilitation of patients with schizophrenia] Qi Lu Hu Li Za Zhi. 2012;18(4):101–102. doi: 10.3969/j.issn.1006-7256.2012.04.068. Chinese. [DOI] [Google Scholar]
- 9.Zhou B, Zhang P, Gu YW. Effectiveness of self-management training in community residents with chronic schizophrenia: a single-blind randomized controlled trial in Shanghai, China. Shanghai Arch Psychiatry. 2014;26(2):81–87. doi: 10.3969/j.issn.1002-0829.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinese Society of Psychiatry. [The Chinese Classification and Diagnostic Criteria of Mental Disorders Version 3 (CCMD-3)] Jinan: Chinese Society of Psychiatry. 2001 Chinese.
- 11.Deng Y. Zhang JZ. [Psychiatry and Mental Health Research] p. Beijing: Beijing Publishing House: 1999. p. 59. Chinese. [Google Scholar]
- 12.Liberman RP. Dissemination and adoption of social skills training: Social validation of an evidence-based treatment for the mentally disabled. J Ment Health. 2007;16(5):595–623. [Google Scholar]
- 13.Wang X, Ma N, Zhang WF, Ma H. [Assessment of compliance with antipsychotic treatment in schizophrenic patients: a review] Zhongguo Xin Li Wei Sheng Za Zhi. 2014;28(1):45–50. doi: 10.3969/j.issn.1000-6729.2014.01.008. Chinese. [DOI] [Google Scholar]
- 14.Li K, Liang HY, Li X, Chen JP, Zhao L, Lv Y, et al. [Validity and reliability of the Morisky questionnaire in assessing antihypertensive therapy compliance of hypertension] Zhonghua Gao Xue Ya Za Zhi. 2010;18(11):1067–1070. doi: 10.3969/j.issn.1002-0829.2010.01.009. Chinese. [DOI] [Google Scholar]
- 15.Chen X, Wang RF, Wei JM, Qi SF, Chen XZ, Cao MY. [Efficacy and medication adherence of olanzapine, risperidone or clozapine combined with lithium in the treatment of acute mania in women] Shanghai Arch Psychiatry. 2010;22(1):37–40. doi: 10.3969/j.issn.1002-0829.2010.01.009. Chinese. [DOI] [Google Scholar]
- 16.Li YY, Ji JL, Weng SM. [The application of Insight Rating Scale in schizophrenia] Shanghai Arch Psychiatry. 1996;8(2):71–74. Chinese. [Google Scholar]
- 17.Song W, Song LS. [A comparative study of schizophrenia between two insight rating scales before and after treatment on schizophrenia] Zhong Yuan Jing Shen Yi Xue Xue Kan. 1999;5(4):205–206. Chinese. [Google Scholar]
- 18.Chen YF, Bu JM. [Risk factors of incompliance in schizophrenia patients discharge from hospital] Wu Jing Hou Qin Xue Yuan Xue Bao. 2013;22(3):182–184. Chinese. [Google Scholar]
- 19.Lin JR, Chen GZ, Guan BB, Huang YK, Huang JP, Li JY, et al. [The compliance of schizophrenic patients and factors that affect it] Zhongguo Shen Jing Jing Shen Ji Bing Za Zhi. 2000;221(3):152–688. doi: 10.3969/j.issn.1002-0152.2000.03.009. Chinese. [DOI] [Google Scholar]
- 20.Xu L, Jin T, Jiang GQ. [Re-admission in patients with schizophrenia analysis and countermeasures] Chongqing Yi Xue. 2010;39(4):413–414. Chinese. [Google Scholar]


