Abstract
We report a case of immunoglobulin G4-related disease (IgG4-RD) presenting with a clinical course suggestive of fibrosing thyroiditis and endocrine ophthalmopathy associated with enlarged cervical lymph nodes. This clinical presentation should prompt a search for associated systemic disorders, including an IgG4-RD. The clue to the exact diagnosis of the underlying disease is histological examination showing an IgG4 plasmatocytic infiltrate in the inflammatory organs involved.
Key Words: Graves’-like orbitopathy, Thyroiditis, Immunoglobulin G4-related disease
What Is Known about This Topic?
• Immunoglobulin G4-related disease (IgG4-RD) is a newly recognized fibroinflammatory process defined by a dense lymphoplasmacytic infiltrate rich in IgG4. Riedel's thyroiditis and a subclass of sclerosing Hashimoto's thyroiditis are considered to be IgG4 related. The association with orbitopathy has rarely been documented in patients with sclerosing Hashimoto's thyroiditis and Riedel's thyroiditis. The treatment of IgG4-RD aims to reduce the inflammatory process and prevent an irreversible fibrotic transformation.
What Does This Article Add?
• The current case report highlights that IgG4-RD should be considered in the differential diagnosis of Graves' orbitopathy in the presence of cervical inflammatory disease, involving cervical lymph nodes and thyroid. Diagnosis relies on biopsy directed at the site with inflammatory involvement.
Introduction
Immunoglobulin G4-related disease (IgG4-RD) is a syndrome characterized by increased IgG4-positive plasmacytic cells in the involved organs. The main organs which can be affected are the pancreas, bile ducts, salivary glands, lymph nodes and thyroid. Recently, a subsection of Hashimoto's autoimmune thyroiditis was described, IgG4 thyroiditis, consisting of a fibrosing variant of the disease. An alternative is the possibility of Riedel's thyroiditis, considered to be a clinical presentation of an IgG4-RD.
We describe a case of an IgG4-RD in a 50-year-old Caucasian man presenting with symptoms suggestive of Hashimoto's thyroiditis with ophthalmopathy. The presence of thyroiditis with significant cervical lymph nodes prompted further investigation with FDG-PET scanning followed by tonsillar biopsy. The biopsy revealed IgG4-RD. After treatment with corticosteroids, the lymph nodes decreased in size and the orbitopathy clinical activity score improved, with a significant decrease in inflammatory disease demonstrated by MRI. Nevertheless, the firm thyroid enlargement persisted.
Case Report
A 50-year-old Caucasian man was referred by the ophthalmologist in January 2013 to exclude endocrine ophthalmopathy. The patient developed bilateral proptosis with intermittent diplopia over a period of 3 months associated with orbital pain and red and swollen eyelids. The clinical activity score was 3/7: eyelid swelling, redness and pain [1]. His past clinical history was unremarkable. He never smoked nor did he take medication. No allergies were reported. He noticed slowly developing throat discomfort and a diffuse firm swelling of the neck slowly evolving over a period of 7 months. Furthermore, he complained of chronic fatigue and weight loss. He denied fever, chills, night sweats, joint pain, jaw claudication, and abdominal pain. Physical examination showed significant cervical lymph node enlargement and swollen tonsils. Thyroid palpation revealed a diffuse firm and painless goiter.
In an additional blood analysis, an erythrocyte sedimentation rate of 8 mm/h (reference range, <15 mm/h) and C-reactive protein level of 0.1 mg/dl (reference range, <1.0 mg/dl) were within normal limits.
The thyroid function was as follows: serum-free triiodothyronine level, 5.3 pmol/l (reference range, 3.2-6.1 pmol/l); free thyroxine level, 14.1 pmol/l (reference range, 10.3-25.7 pmol/l); thyroid-stimulating hormone level, 4.95 mU/l (reference range, 0.3-4.0 mU/l), and normal serum calcium, 9.2 mg/dl (reference range, 9.1-10.2 mg/dl).
Thyrotropin receptor antibodies, <1 IU/l (reference value, <1 IU/l) were negative and serum thyroid microsomal antibodies were positive with a titer of 568 IU/ml (reference range, <250 IU/ml). The patient was treated with levothyroxine 75 μg, q.d.
Serum antinuclear and antineutrophil cytoplasmic antibodies were negative.
Liver function (AST, 15 IU/l/ALT, 25 IU/l; reference range, 15-40/10-40 IU/l), pancreas enzymes (lipase, 25 IU/l; reference range, 10-60 IU/l) and kidney function (creatinine, 1.05 mg/dl; reference range 0.72-1.17 mg/dl) were within normal limits.
Hepatitis B and C serology were not in favor of chronic persistent infection and human immunodeficiency virus antibodies were negative.
Urinary collection did not show the presence of albuminuria or proteinuria.
An IgG4 plasma level was also performed and showed elevated levels: 139.2 mg/dl (reference range, 14-126 mg/dl).
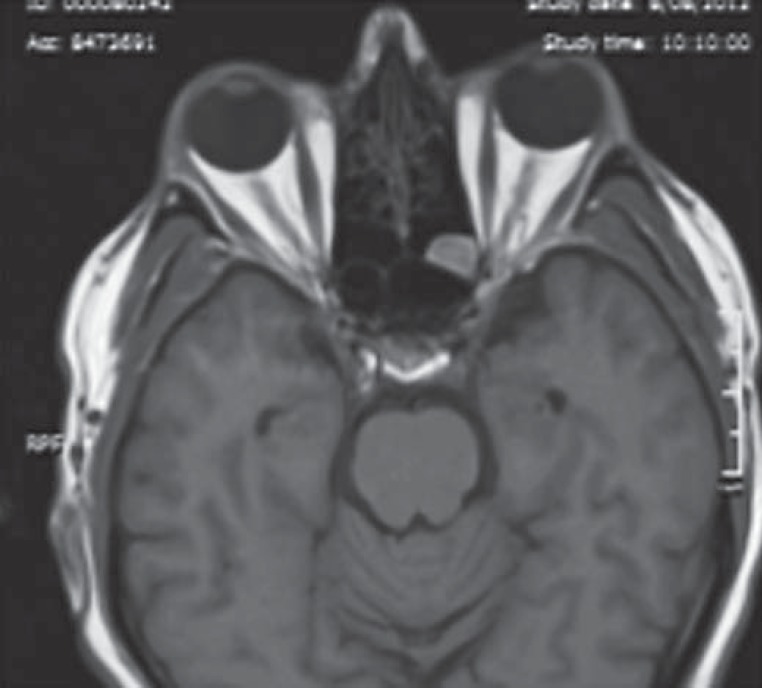
An orbital MRI (fig. 1) was performed on a 1.5-tesla magnet and revealed a bilateral enlargement of the lateral, medial and inferior rectus ocular muscles without any intraorbital mass. Signal intensities of extraocular muscles and orbital fat tissues were measured by short-time inversion recovery image and were in favor of an active intraorbital inflammatory process. The infraorbital optic nerve was also enlarged bilaterally. Inflammatory lesions were also seen in the maxillary sinus and in ethmoidal cells. Lacrimal glands were not enlarged on MRI images.
Fig. 1.
MRI of the orbit performed in January 2013. Axial T1-weighted postcontrast image showing bilateral proptosis, enlarged connective tissue, orbital fat, and extraocular muscle enlargement. The infraorbital optic nerve is enlarged bilaterally. Inflammatory lesions are also seen in the maxillary sinus and in ethmoidal cells.
The thyroid gland was enlarged with markedly hypoechoic and heterogeneous scattered hyperechoic areas on gray-scale ultrasound examination. It was also hypovascular compared with the background parenchyma.
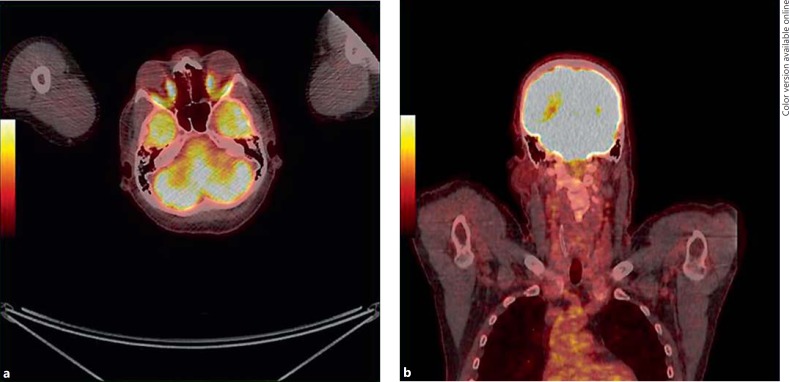
An FDG-PET (fig. 2a, b) was performed because of the presence of enlarged cervical lymph nodes. A high uptake of FDG was observed in the orbital areas and the tonsils, with a relatively increased uptake of FDG in the cervical lymph nodes. There was no increased uptake in the thyroid bed.
Fig. 2.
a A high glucose uptake is present in orbital areas. b A high glucose uptake is present in bilateral tonsils and cervical lymphadenopathies. Surprisingly, there is no increased uptake in the thyroid bed.
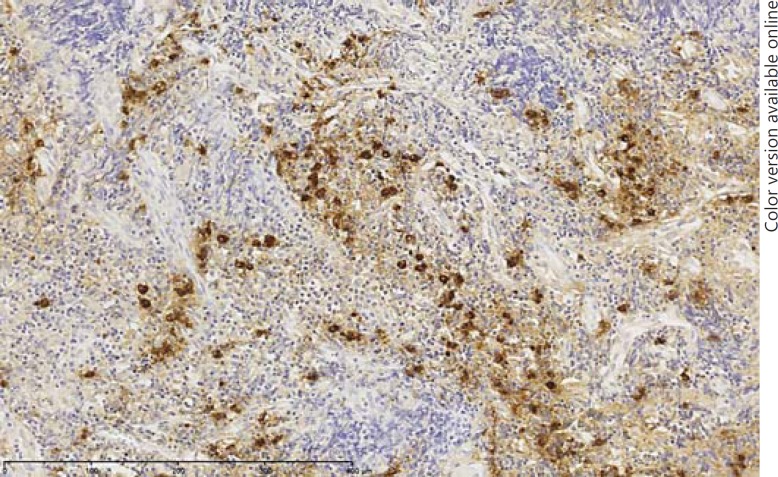
As a rule of thumb, a tonsil biopsy was performed as it was the best accessible site and with the primary aim of excluding a primary lymphoma. Histology demonstrated a dense lymphoplasmacytic infiltrate, lymphoid aggregates and focal storiform fibrosis (fig. 3). The eosinophils were low (1-2 eosinophils/10 high-power fields), without granulomas. No thyroid biopsy was performed because FDG-PET did not show any uptake.
Fig. 3.
IgG4-RD in the tonsils. Immunostaining for IgG4, demonstrating ample numbers of plasma cells that stain for IgG4. Comparison with the total number of plasma cells indicates a high IgG4/IgG ratio. Plasmatocytic anti-IgG4 (50 µm).
We evaluated the proportion of IgG4-positive plasma cells by direct counting of plasma cells stained with anti-CD138 (dilution 1:100; Dako), antitotal IgG (dilution 1:5,000; ICN Biomedicals) and anti-IgG4 monoclonal antibodies on 10 consecutive high-power fields. The staining procedure involved the Bond-Max device (Bond; Leica Microsystems and A. Menarini Diagnostics) with peroxidase and diaminobenzidine after antigen retrieval by heat with an appropriate buffer. Immunostaining for IgG and IgG4 revealed an elevated IgG4-positive plasma cell count of 289/10 high-power fields with an IgG4/IgG ratio of 0.87. Stains for infectious disease and cultures were negative. HHV-8 staining was negative, ruling out multicentric Castleman's disease.
An IgG4-RD was diagnosed with an inflammatory process involving the cervical lymph nodes, tonsils and orbits. Based on a consensus statement from 17 referral centers in Japan, the patient was treated by prednisolone using a dosage of 0.6 mg per kilogram of body weight per day for 4 weeks with subsequent tapering of 10% every 2 weeks.
Corticosteroid treatment improved the clinical activity score of ophthalmopathy dramatically with the disappearance of the swelling of the eyelids and the diplopia, and the disappearance of bilateral enlarged tonsils and enlarged lymph nodes. Thyroid function did not normalize, necessitating continued substitution therapy with thyroxin. The proptosis persisted 10 months after the initiation of treatment, although the signs of inflammation in the orbits disappeared.
Discussion
This case reports is of a patient with an IgG4-RD, with clinical manifestations of inflammatory involvement of cervical lymph nodes, orbital tissues and the thyroid. Although biopsy of the thyroid was not performed, the clinical and histological data suggested the presence of Riedel's thyroiditis or a fibrosing variant of Hashimoto's thyroiditis.
IgG4-related sclerosing disease has recently been recognized as a fibroinflammatory condition characterized by lymphoplasmacytic infiltration. Plasma cells bear high titers of IgG4 and this constitutes the basis of the diagnosis. Virtually all tissues may be involved and the affected organs may ultimately show fibrotic changes [2]. The term ‘IgG4-RD’ encompasses several disorders described many years ago under various designations depending on the organ and/or system involved (e.g. Mikulicz's syndrome, Riedel's thyroiditis and retroperitoneal fibrosis).
This entity was not described as a systemic disease until 2003 [2]. It was first reported in Japanese patients with autoimmune pancreatitis, in whom similar histological findings were observed in other organs, suggesting a systemic inflammatory process such as seen in sarcoidosis [3]. The condition is rare and epidemiological data are very limited. The majority of patients are male and older than 50 years at clinical presentation [4]. In Japan, the estimated incidence is 0.2-1 per 100,000 [5].
The pathogenesis of this disease remains ill-defined. Nevertheless, the serum IgG4 level is elevated in 44-100% of patients in a recently published series [6]. Diagnosis cannot be made based solely on a single measurement of IgG4 plasma levels. The gold standard for diagnosis is histology, with a documented dense lymphoplasmacytic infiltrate in a storiform pattern. The immunostaining must demonstrate an elevated absolute number of IgG4-positive plasma cells associated with a high ratio of IgG4 to IgG (>40%) [7,8].
This case report illustrates a rather unusual presentation of an IgG4-RD, with initial symptoms suggesting autoimmune thyroiditis with ophthalmopathy. The presence of significant enlarged lymph nodes and tonsils and an indurated goiter prompted further investigation with an FDG-PET scan followed by tonsil biopsy to rule out a primary lymphoma. Also, the swollen painful and firm thyroid associated with an inflammatory process in the surrounding cervical lymph nodes raised the possibility of an IgG4-RD, which was subsequently confirmed on histology [9].
In the differential diagnosis, we considered other systemic disorders such as sarcoidosis, Castleman's disease, microangiitis with granulomatosis, lymphoma, myositis, and cancer.
The involvement of the orbits in IgG4-RD has recently been described [10]. This may be associated with IgG4-related changes such as the thyroid, thereby mimicking autoimmune thyroid disease and Graves' ophthalmopathy. A sclerosing variant of Hashimoto's thyroiditis with histopathological features resembling the IgG4-related variant of the disease was reported by Li et al. [11]. Immunostaining of IgG4 in Hashimoto's disease is very important in classifying towards a sclerosing pathway of IgG4-RD [11]. Although a proportion of cases of Hashimoto's thyroiditis show elevated numbers of IgG4-positive plasma cells, these cases lack the histological features typically associated with IgG4-RD [12]. It is suggested that a subgroup of IgG4 thyroiditis might have a close relationship with IgG4-related sclerosing disease. However, in 17 cases of IgG4 Hashimoto's thyroiditis no IgG4-related sclerosing disease was detected in other organs. IgG4 Hashimoto's thyroiditis is significantly associated with male gender, shorter disease duration of Hashimoto's thyroiditis before surgery than that of non-IgG4 thyroiditis and more severe symptoms such as tracheal stenosis, leading patients to undergo operations more rapidly [13]. Riedel's thyroiditis is another rare form of infiltrative and inflammatory disease of the thyroid gland and can be associated with systemic fibrotic disease. Research has shown that IgG4-RD is likely to be involved. Riedel's thyroiditis can occur in conjunction with other autoimmune diseases such as Hashimoto's thyroiditis. Although we did not obtain histopathological confirmation, the clinical data support the presence of Riedel's thyroiditis or a sclerosing type of Hashimoto's thyroiditis in our patient.
To our knowledge, the association of an IgG4-related inflammation in the orbits with Riedel's thyroiditis has rarely been described [14]. The pathophysiological mechanisms of IgG4-RD have begun to be elucidated. The physiological production of IgG4 can be induced by prolonged or repeated antigen exposure [15]. Via a Th2 cell-mediated response, IgG4 and IgE are produced primarily by the immune system [16]. In the present case report a subacute thyroiditis cannot be excluded as an initial trigger for the immune-mediated response. The absence of fever and clinical signs of subacute thyroiditis, however, are not in favor of the hypothesis of subacute thyroiditis as a trigger of IgG4-RD and Riedel's thyroiditis, as previously reported. Next, the preferential shift towards IgG4 production rather than IgE production will ultimately be determined by other environmental factors. In the presence of interleukin (IL)-10, IL-12 and IL-21, IgG4 secretion is favored [16,17]. In IgG4-RD, lymphocytes expressing IL-4 or IL-10 are identifiable in the affected organs by in situ hybridization. Peripheral blood T-cell phenotype is also shifted towards a Th2 response [18].
In contrast to classical autoimmune disorders, regulatory T (Treg) cells are activated and infiltrated tissues are characterized by a large number of CD4+CD25+ Treg cells. In addition, these Treg cells, as well as Th2 lymphocytes, are able to produce IL-10 but also TGF-β, which may ultimately play a primordial role favoring fibrosis over inflammation [18,19,20].
In the present case report, an FDG-PET scan was performed to evaluate the systemic involvement and to exclude lymphoproliferative disease. A high uptake of FDG in the tonsils and the orbital tissues and a relatively increased uptake of FDG in the cervical lymph nodes were observed. The absence of thyroid activity may reflect the fact that the thyroid inflammation resolved, whereas in the orbital tissue, FDG uptake probably indicated ongoing inflammation. Consequently, it was decided to biopsy the tonsils as the most direct and safest way to make a definitive diagnosis [21].
IgG4-RD is systemic and may affect different tissues sequentially. Therefore, in-depth evaluation of the organs affected by the disease should be part of the diagnostic evaluation. FDG-PET is a useful guide to target a biopsy and to further evaluate the systemic involvement of the IgG4-RD.
Indeed, histological analysis remains the diagnostic cornerstone of IgG4-RD since raised serum levels of IgG4 are neither sensitive nor specific to the diagnosis.
The biopsy in this patient complies with the gold standard of diagnosis, i.e. more than 40% of all infiltrating plasma cells were IgG4 positive, with very high IgG4-positive to IgG-positive plasma cell ratio of 0.87 [22]. There were no reasons to further extend the investigations, since liver tests were within the normal limits, biochemical data did not suggest the involvement of the gastrointestinal tract and the FDG-PET scan did not show a significant uptake in these sites.
Treatment with steroids decreased the size of the lymph nodes and tonsils. Also, the signs of inflammation of the eyes decreased and diplopia resolved. However, some degree of proptosis persisted. Thyroid enlargement and function were refractory to treatment, necessitating continuous substitution therapy.
We hypothesize that this observation is related to a fibrotic transformation of the thyroid gland, as seen in Riedel's thyroiditis and described in an IgG4-RD. This case report, therefore, highlights that IgG4-RD should be added to the differential diagnosis of Graves'-like orbitopathy, in the presence of cervical inflammatory lymph nodes. We acknowledge that doubts remain about the etiology of the thyroid involvement, since we were not able to confirm an IgG4-related involvement in the thyroid by biopsy. Arguments in favor of an IgG4-RD of the thyroid are that Hashimoto's thyroiditis is characterized by intense diffuse or focal uptake on FDG-PET and cervical involvement has never been reported [23,24]. There is no systematic report in the literature about the characteristics of FDG-PET scanning in Riedel's thyroiditis.
Possible explanations for the resistance of the thyroid to corticosteroid treatment may be the rather late diagnosis after initial symptomatology and the possibility of early fibrosis that occurs more often in conjunction with IgG4-RD compared with classical autoimmune thyroiditis. Therefore, this case report raises the importance of having a high index of suspicion for early diagnosis and appropriate treatment of an IgG4-RD before the occurrence of irreversible fibrosis.
Disclosure Statement
The authors declare that no financial or other conflict of interest exists in relation to the content of the article.
References
- 1.Bartalena L, Baldeschi L, Dickinson A, et al. Consensus statement of the European Group on Graves' Orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol. 2008;158:273–285. doi: 10.1530/EJE-07-0666. [DOI] [PubMed] [Google Scholar]
- 2.Stone JH, Zen Y, Deshpande V. Mechanisms of disease: IgG4-related disease. N Engl J Med. 2012;366:531–551. doi: 10.1056/NEJMra1104650. [DOI] [PubMed] [Google Scholar]
- 3.Fonte R, Pirali B, Chiovato L. Graves'-like orbitopathy in a patient with chronic autoimmune pancreatitis. Thyroid. 2011;21:1389–1392. doi: 10.1089/thy.2011.0191. [DOI] [PubMed] [Google Scholar]
- 4.Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–738. doi: 10.1056/NEJM200103083441005. [DOI] [PubMed] [Google Scholar]
- 5.Masaki Y, Kurose N, Umehara H. IgG4-related disease: a novel lymphoproliferative disorder discovered and established in Japan in the 21st century. J Clin Exp Hematop. 2011;51:13–20. doi: 10.3960/jslrt.51.13. [DOI] [PubMed] [Google Scholar]
- 6.Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol. 2011;23:108–113. doi: 10.1097/BOR.0b013e3283413469. [DOI] [PubMed] [Google Scholar]
- 7.Strehl ID, Hartmann A, Agaimy A. Numerous IgG4-positive plasma cells are ubiquitous in diverse localized non-specific chronic inflammatory conditions and need to be distinguished from IgG4-related systemic disorders. J Clin Pathol. 2011;64:237–243. doi: 10.1136/jcp.2010.085613. [DOI] [PubMed] [Google Scholar]
- 8.Dhall D, Suriawinata AA, Tang LH, et al. Use of immunohistochemistry for IgG4 in the distinction of autoimmune pancreatitis from peritumoral pancreatitis. Hum Pathol. 2010;41:643–652. doi: 10.1016/j.humpath.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 9.Hennessey JV. Riedel's thyroiditis: a clinical review. J Clin Endocrinol Metab. 2011;96:3031–3041. doi: 10.1210/jc.2011-0617. [DOI] [PubMed] [Google Scholar]
- 10.Masaki Y, Kurose N, Umehara H. IgG4-related disease: a novel lymphoproliferative disorder discovered and established in Japan in the 21st century. J Clin Exp Hematop. 2011;51:13–20. doi: 10.3960/jslrt.51.13. [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Bai Y, Liu Z, et al. Immunohistochemistry of IgG4 can help subclassify Hashimoto's autoimmune thyroiditis. Pathol Int. 2009;59:636–641. doi: 10.1111/j.1440-1827.2009.02419.x. [DOI] [PubMed] [Google Scholar]
- 12.Deshpande V, Huck A, Nielsen GP. Fibrosing variant of Hashimoto thyroiditis is an IgG4 related disease. J Clin Pathol. 2012;65:725–728. doi: 10.1136/jclinpath-2011-200485. [DOI] [PubMed] [Google Scholar]
- 13.Li Y, Nishihara E, Hirokawa M, Taniguchi E, Miyauchi A, Kakudo K. Distinct clinical, serological, and sonographic characteristics of Hashimoto's thyroiditis based with and without IgG4-positive plasma cells. J Clin Endocrinol Metab. 2010;95:1309–1317. doi: 10.1210/jc.2009-1794. [DOI] [PubMed] [Google Scholar]
- 14.Jakobiec FA, Stacy RC, Hatton MP. Clinical characterization and immunopathologic features of sclerosing dacryoadenitis and Riedel thyroiditis. Arch Ophthalmol. 2010;128:1626–1628. doi: 10.1001/archophthalmol.2010.299. [DOI] [PubMed] [Google Scholar]
- 15.Aalberse RC, Stapel SO, Schuurman J, et al. Immunoglobulin G4: an odd antibody. Clin Exp Allergy. 2009;39:469–477. doi: 10.1111/j.1365-2222.2009.03207.x. [DOI] [PubMed] [Google Scholar]
- 16.Wood N, Bourque K, Donaldson DD, et al. IL-21 effects on human IgE production in response to IL-4 or IL-13. Cell Immunol. 2004;231:133–145. doi: 10.1016/j.cellimm.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 17.De Broer BA, Kruize YC, Rotmans PJ, et al. Interleukin-12 suppresses immunoglobulin E production but enhances immunoglobulin G4 production by human peripheral blood mononuclear cells. Infect Immun. 1997;65:1122–1125. doi: 10.1128/iai.65.3.1122-1125.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Detlefsen S, Sipos B, Zhao J, et al. Autoimmune pancreatitis: expression and cellular source of profibrotic cytokines and their receptors. Am J Surg Pathol. 2008;32:986–995. doi: 10.1097/PAS.0b013e31815d2583. [DOI] [PubMed] [Google Scholar]
- 19.Detlefsen S, Bräsen JH, Zamboni G, et al. Deposition of complement C3c, immunoglobulin (Ig)G4 and IgG at the basement membrane of pancreatic ducts and acini in autoimmune pancreatitis. Histopathology. 2010;57:825–835. doi: 10.1111/j.1365-2559.2010.03717.x. [DOI] [PubMed] [Google Scholar]
- 20.Miyake K, Moriyama M, Aizawa K, et al. Peripheral CD4+ T cells showing a Th2 phenotype in a patient with Mikulicz's disease associated with lymphadenopathy and pleural effusion. Mod Rheumatol. 2008;18:86–90. doi: 10.1007/s10165-007-0010-3. [DOI] [PubMed] [Google Scholar]
- 21.Yasuda S1, Shohtsu A, Horiuchi M. Chronic thyroiditis: diffuse uptake of FDG at PET. Radiology. 1998;207:775–778. doi: 10.1148/radiology.207.3.9609903. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe T, Maruyama M, Ito T, et al. Clinical features of a new disease concept, IgG4-related thyroiditis. Scand J Rheumatol. 2013;42:325–330. doi: 10.3109/03009742.2012.761281. [DOI] [PubMed] [Google Scholar]
- 23.Yeo SH, Lee SK, Hwang I, Ahn EJ. Subacute thyroiditis presenting as a focal lesion on [18F]fluorodeoxyglucose whole-body positron-emission tomography/CT. AJNR Am J Neuroradiol. 2011;32:E58–E60. doi: 10.3174/ajnr.A2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akosman C, Selcuk NA, Ordu C, Ercan S, Ekici ID, Oyan B. Unicentric mixed variant Castleman disease associated with Hashimoto disease: the role of PET/CT in staging and evaluating response to the treatment. Cancer Imaging. 2011;11:52–55. doi: 10.1102/1470-7330.2011.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]