Abstract
Background & objectives:
Small intestinal bacterial overgrowth (SIBO) leads to several gastrointestinal (GI) problems and complications leading to malabsorption. The effectiveness of probiotics in the treatment of SIBO syndrome has not been well studied. This pilot study was aimed to assess the efficacy of a probiotic consisting of lactobacilli in the treatment of SIBO.
Methods:
In this study, 30 cases suffering from chronic abdominal pain or diarrhoea and with a positive hydrogen breath test were randomized in a double-blind manner into two groups: probiotic drug user and control group. After an initial 3-week aggressive therapy with broad-spectrum antibiotics, a 15-day maintenance antibiotic therapy with lactol was administered for the study group and the same regimen without lactol for the control group. After six months the HBT result and the GI symptoms were analyzed and compared between the two groups.
Results:
The result of hydrogen breath test and the clinical symptoms in patients receiving the maintenance regimen with lactol probiotic showed a better response. The hydrogen breath test turned negative in 93.3 per cent of those receiving lactol compared to 66.7 per cent of the controls. In all the cases receiving lactol, the abdominal pain disappeared completely (P=0.002). In addition, other GI problems including flatulence, belching and diarrhoea significantly improved in the study group (P<0.05).
Interpretation & conclusions:
Based on the preliminary data it seems that adding lactol probiotic to the maintenance therapy of small intestinal bacterial overgrowth patients on routine antibiotic therapy will be beneficial in preventing the complications of this syndrome.
Keywords: Hydrogen breath test (HBT), lactol, small intestinal bacterial overgrowth (SIBO) syndrome
Excessive increase in the number of bacteria in the microbial flora in the stomach and small intestine is accompanied by the onset of gastrointestinal (GI) symptoms and can cause major problems1. Bacterial overgrowth can be the result of a change in the clinical condition which has altered the pH and the bowel movements. In addition, immune deficiency and malnutrition are the other risk factors accompanying this disorder1,2. Small intestinal bacterial overgrowth (SIBO) leads to steatorrhoea, vitamin B12 absorptive impairment and also injury to the small intestinal microvilli which itself causes malabsorption. On the other hand, this SIBO can lead to coma, neurological deficit and acidosis- induced shock2. SIBO has also been proposed to be a common causative factor in the pathogenesis of irritable bowel syndrome (IBS)3. The diagnosis of this syndrome is made by hydrogen breath test (HBT)3,4.
Probiotics are live microorganism which are beneficial for their hosts and prevent certain diseases such as antibiotic-associated diarrhoea, and inflammatory bowel disease (IBD)5. These bacteria act by enhancing the epithelial barrier function, modulating the immune system and by competitive binding and adherence to the intestinal epithelium and mucosa6,7. Probiotics containing lactobacilli have shown beneficial effects on many gastrointestinal disorders, vaginal infections, hypercholesterolaemia, etc8,9. Moreover, these can also improve the digestive metabolism and also the immune process10.
This preliminary study was aimed to investigate the effect of lactol probiotic in treating or reducing the complications in patients suffered from SIBO.
Material & Methods
This study which registered in IRCT (2013061313662N1) was performed on the patients with chronic stomach pain and discomfort or changes in their defaecation with no other anatomical or functional diagnosis other than small intestinal bacterial overgrowth (SIBO), who were referred to the Infectious and Internal Diseases Clinics of Quaem Hospital, Mashhad University of Medical Sciences (MUMS), Mashhad, Iran, from May 2010 to October 2011. Hydrogen breath test (HBT) was performed after obtaining informed written consent. The study protocol was approved by the Research Council Ethics Committee of Mashhad University of Medical Sciences. The consumption of all types of antibiotics, proton-pump inhibitors (PPI), Bismuth or other digestive drugs was ceased since one month before the test; it was performed following 12 h of fasting and three hours after using a mouth wash solution. The amount of released respiratory hydrogen following each deep breath in and breath out was recorded. The production of 20 ppm of hydrogen at each time point was defined as its consumption by the bacteria and, therefore, was considered as a positive test result11.
Thirty consecutive cases with a positive HBT result were included in the study. Their GI symptoms were recorded. They were randomized in a double-blind, manner into two groups: probiotic drug user and control group. Following three week of aggressive therapy with broad-spectrum antibiotics, a monthly maintenance therapeutic regimen including 15 days of antibiotic therapy with minocycline, 100 mg twice a day, and 15 days with lactol probiotic (Bioplus Life Sciences Pvt. Ltd., India) (Bacillus coagulan spores and Fructo-oligosaccharides), twice a day after meals, was administered for the study group. The control group received 15 days of antibiotic therapy with minocycline, 100mg twice a day, during first half of each month and received no other drug during the rest of the month. After the treatment period (6 months), the HBT was performed once again and GI symptoms were recorded again, the HBT test result and also rate of GI symptoms improvement were compared between the two groups.
Chi-square test, Fisher's exact test were used for data analysis (P<0.05 was considered as significant).
Results & Discussion
The patients’ demographic data and GI symptoms at the initiation and termination points of the study are presented in Tables I and II. Of the 30 cases, 15 (50%) were females. The age ranged from 21 to 80 yr. The mean age of the study group which received Lactol probiotic was 34.60 ± 10.68 yr whereas the control group for which a non-probiotic therapeutic regimen was administered had a mean age of 42.86 ± 16.61 yr. No significant difference was detected between the two groups regarding age and sex. At the end of the treatment course, pain had completely disappeared in the probiotic group whereas it was resolved in only seven of the 15 cases (46.7%) of the control group; the difference was significant (P=0.002). The number of patients with complaints of bloating, belching and diarrhoea was remarkably less in the patients receiving lactol probiotic in comparison to controls (Table II). In this study the presence of nausea, vomiting, constipation and feeling loss of appetite was similar in both groups. The post-treatment HBT results were negative in 93.3 per cent patients of the study group in comparison to 66.7 per cent of the controls.
Table I.
Clinical characteristics of subjects at baseline
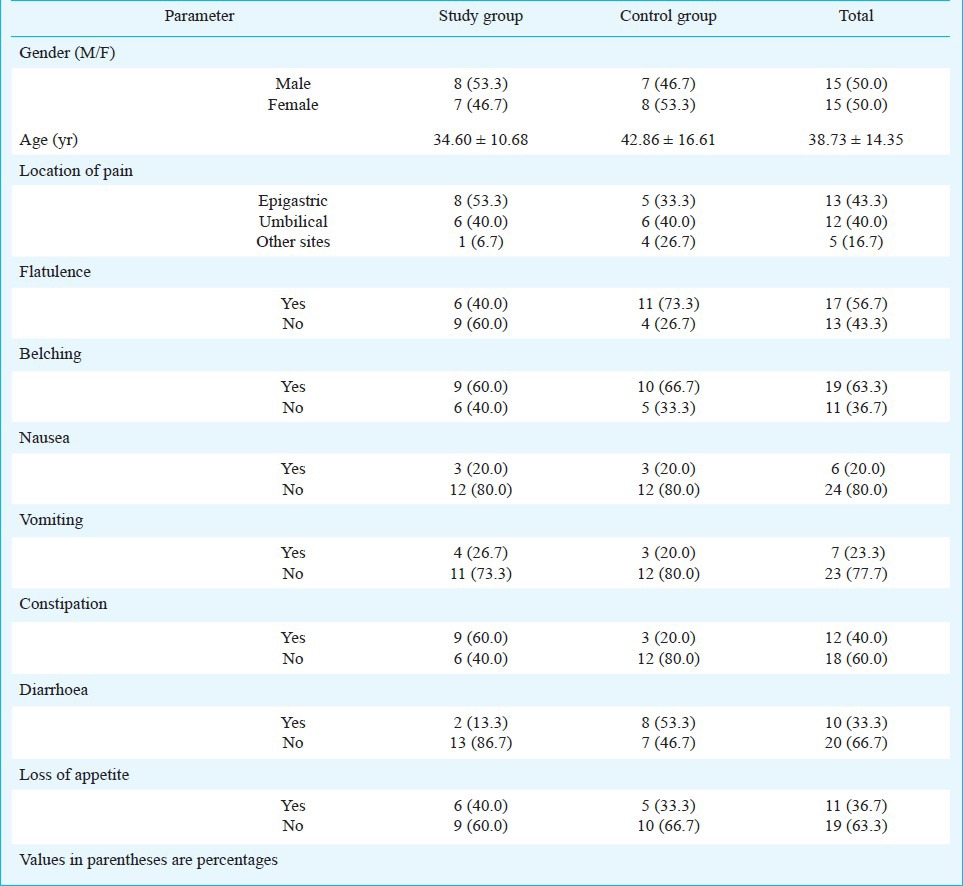
Table II.
Clinical characteristics data of subjects after six months of treatment

The main goal of this study was to assess the effectiveness of a maintenance therapy with lactol probiotic in the treatment of patients suffering from SIBO who had a positive HBT. Also the improvement in the gastrointestinal symptoms in the study and control groups was compared.
In our study, 33.3 per cent patients of the study group and 53.3 per cent of the controls had a Bachelor degree or higher education but no significant difference was observed when the two groups were compared based on the patients’ educational status. Other studies performed on the efficacy of probiotics have only focused on the gastrointestinal symptoms of disorders such as antibiotic-induced diarrhoea, IBD, and other inflammatory and allergic diseases12,13,14,15,16.
At the initiation of the study the pain was mostly located in the epigastric and umbilical areas which fully disappeared in the lactol receiving group at the end of the treatment course. The symptoms of diarrhoea, flatulence and belching improved significantly in the lactol group in comparison to the controls.
In spite of the aggressive and maintenance treatments administered for all the cases, 93.3 per cent patients showed negative result of the HBT at the end of treatment in the study group compared to 66.7 per cent in the control group, showing the effectiveness of the probiotic treatment. These results need to be confirmed in a study with a larger sample size.
In conclusion, the results of this pilot study show that adding a probiotic drug such as lactol to the maintenance regimen may improve the GI symptoms and prevent the probable complications in patients with SIBO.
References
- 1.Binder HJ. Disorders of Absorption. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, editors. Harrison's principles of internal medicine. 18th ed. New York: McGraw Hill; 2012. pp. 2460–76. [Google Scholar]
- 2.Kleigman RM, Behrman RE, Jenson HB, Stanton BF. 19th ed. Philadelphia: PA: Saunders; 2011. Nelson textbook of pediatrics. [Google Scholar]
- 3.Quigley EM. Bacteria: a new player in gastrointestinal motility disorders - infections, bacterial overgrowth, and probiotics. Gastroenterol Clin North Am. 2007;36:735–48. doi: 10.1016/j.gtc.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 4.O’Mahony S, Shanhan F. Enteric microbiota and small intestinal bacterial overgrowth. In: Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger & Fordtran's gastrointestinal & liver disease :pathophysiology, diagnosis, management. 9th ed. Philadelphia: Saunders Elsevier; 2010. pp. 1772–7. [Google Scholar]
- 5.Scherezenmeir J, De Verse M. Probiotics, and synbiotics-approaching a definition. Am J Clin Nutr. 2001;73:361S–64S. doi: 10.1093/ajcn/73.2.361s. [DOI] [PubMed] [Google Scholar]
- 6.De Simone C, Ciardi A, Grassi A. Effect of Bifidobacterium bifidum and Lactobacillus on gut mucosa peripheral blood B lymphocytes. Immunopharmacol Immunotoxicol. 1992;14:331–40. doi: 10.3109/08923979209009228. [DOI] [PubMed] [Google Scholar]
- 7.Fuller R. Probiotics in human medicine. Gut. 1991;32:439–42. doi: 10.1136/gut.32.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freter R. Factors affecting the microecology of the gut. In: Fuller R, editor. Probiotics, the scientific basis. London: Champan & Hall; 1992. pp. 111–44. [Google Scholar]
- 9.Reid G. Probiotics for urogenital health. Nutri Clin Care. 2002;5:3–8. doi: 10.1046/j.1523-5408.2002.00512.x. [DOI] [PubMed] [Google Scholar]
- 10.Rowland IR, Grasso P. Degradation of N-nitrosamines by intestinal bacteria. Appl Microbiol. 1975;29:7–12. doi: 10.1128/am.29.1.7-12.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Semard CA, Powell DW. Approach to the patient with diarrhea and malabsorption. In: Goldman L, Ausiello DA, editors. Cecil medicine. 23th ed. Philadelphia: PA: Saunders Elsevier; 2008. p. 1029. [Google Scholar]
- 12.Soifer LO, Peralta D, Dima G, Besasso H. Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study. Acta Gastroenterol Latinoam. 2010;40:323–7. [PubMed] [Google Scholar]
- 13.Barrett JS, Canale KE, Gearry RB, Irving PM, Gibson PR. Probiotic effects on intestinal fermentation patterns in patients with irritable bowel syndrome. World J Gstroenterol. 2008;14:5020–4. doi: 10.3748/wjg.14.5020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jonkers D, Penders J, Masclee A, Pierik M. Probiotics in the management of inflammatory bowel disease: a systematic review of intervention studies in adult patients. Drugs. 2012;72:803–23. doi: 10.2165/11632710-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Rohde CL, Bartolini V, Jones N. The use of probiotics in the prevention and treatment of antibiotic-associated diarrhea with special interest in Clostridium difficile-associated diarrhea. Nutr Clin Pract. 2009;24:33–40. doi: 10.1177/0884533608329297. [DOI] [PubMed] [Google Scholar]
- 16.Bixquert Jimenez M. Treatment of irritable bowel syndrome with probiotics. An etiopathogenic approach at last? Revista espanola de enfermedades digestivas. Rev Esp Enferm Dig. 2009;101:553–64. doi: 10.4321/s1130-01082009000800006. [DOI] [PubMed] [Google Scholar]


