Abstract
Background & objectives:
The Indian Disability Evaluation and Assessment Scale (IDEAS) has been recommended for assessment and certification of disability by the Government of India (GOI). However, the psychometric properties of IDEAS as adopted by GOI remain understudied. Our aim, thus, was to study the internal consistency and validity of IDEAS in patients with schizophrenia.
Methods:
A total of 103 consenting patients with residual schizophrenia were assessed for disability, quality of life (QOL) and psychopathology using the IDEAS, WHO QOL-100 and Positive and Negative symptom scale (PANSS) respectively. Internal consistency was calculated using Cronbach's alpha. For construct validity, relations between IDEAS, and psychopathology and QOL were studied.
Results:
The inter-item correlations for IDEAS were significant with a Cronbach's alpha of 0.721. All item scores other than score on communication and understanding; total and global IDEAS scores correlated significantly with the positive, negative and general sub-scales, and total PANSS scores. Communication and understanding was significantly related to negative sub-scale score only. Total and global disability scores correlated negatively with all the domains of WHOQOL-100 (P<0.01). The individual IDEAS item scores correlated negatively with various WHOQOL-100 domains (P< 0.01).
Interpretation & conclusions:
This study findings showed that the GOI-modified IDEAS had good internal consistency and construct validity as tested in patients with residual schizophrenia. Similar studies need to be done with other groups of patients.
Keywords: Disability, IDEAS, internal consistency, mental illness, schizophrenia, validity
Disability is a complex bio-psycho-social phenomenon that results from interplay of illness-related factors and the overall socio-environmental context in which the person lives1. Amongst the different illnesses, mental illnesses are associated with significant disability, with major depression, alcohol dependence, schizophrenia, bipolar affective disorder and obsessive-compulsive disorder (OCD) among the ten leading causes of disability adjusted life years (DALYs) worldwide2. Neuropsychiatric disorders alone contribute to 14 per cent of DALYs lost to disability due to all causes3. Assessment and quantification of disability is important for the purposes of treatment, rehabilitation planning and effectiveness, policy making and providing governmental assistance and also for defining eligibility criteria for availing such benefits. However, it has been recognised that psychiatric disability is characterized by different patterns of disabilities when compared to that seen in patients with other chronic physical illnesses by virtue of their symptomatic presentations and pattern of associated socio-occupational dysfunction4.
In India, it is estimated that more than 2.27 million people are disabled due to mental illnesses and intellectual sub-normality5. However, till recently there was no standard government approved instrument for assessment of psychiatric disability, although there have been many attempts to design instruments for assessment of psychiatric disability in the Indian context, i.e., ‘PGI Disability Scale’6,7, and Schedule for Assessment of Psychiatric Disability (SAPD)8. In 2001, the task force of Rehabilitation Committee of the Indian Psychiatric Society (IPS) developed the instrument -Indian Disability Evaluation and Assessment Scale (IDEAS) for measuring and quantifying disability in patients with mental disorders9. The scale was field tested at eight centres across the country, involving 1,078 patients. It is found to have good internal consistency, face, content and criterion validities10. In 2001, a Committee was constituted by the Department of Health, Government of India (GOI) under the Chairmanship of Director General of Health Services on the basis of request made by the Ministry of Social Justice & Empowerment to prescribe guidelines for evaluation and assessment of disability associated with mental illnesses and procedure for certification under the provisions of Persons with Disabilities Act, 1995. The Committee approved IDEAS as developed by IPS with some modifications for the assessment and certification of disability associated with mental illnesses11.
In the last decade, about a dozen studies have employed IDEAS either in its original form or as modified by the GOI. Most of these studies have focused on prevalence and pattern of psychiatric disabilities in hospital-based and community samples12,13,14,15. A few studies16,17,18 have assessed the effect of pharmacological and psychological interventions on disability. Three studies19,20,21 have reported the distribution of disorders and pattern of disability in patients seeking certification. However, the reliability and validity of the instrument have not been reported. Thus, the present study was aimed to assess the internal consistency and construct validity of GOI modified IDEAS. It was hypothesized that the disability scores would have positive correlation with residual symptoms of schizophrenia (convergent validity) and negative correlation with quality of life (QOL) (divergent validity) and presence of such relations would provide evidence for construct validity of the scale.
Material & Methods
The study was conducted in the department of Psychiatry, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarth, a tertiary care multispecialty hospital catering to major part of north India during the period of January to December 2008. The study was approved by the Institutional Review Board (IRB). To be included in the study, patients were required to have a diagnosis of residual schizophrenia, aged 20-60 yr, with no other psychiatric co-morbidity including substance dependence (except nicotine) and no associated chronic physical illness. Those with organic brain syndrome and mental retardation were also excluded. The study followed a prospective design, in which 103 patients were recruited by using convenience sample and were evaluated cross-sectionally. The study was limited to patients of residual schizophrenia, because this group of patients had stable residual psychopathology and resultant disability and quality of life.
Each patient provided written informed consent. Initially, the patients were evaluated on Structured Clinical Interview for Axis-1 DSM-IV Disorders-Clinical Version (SCID-CV)22 to confirm the diagnosis of residual schizophrenia. Further, they were evaluated on the inclusion and exclusion criteria. After recording the socio-demographic and clinical profile, patients who fulfilled the study criteria were further assessed for residual psychopathology, disability and quality of life. Disability was assessed using the GOI-modified IDEAS11 and psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS)23 for schizophrenia on the basis of information provided by the patient, caregivers and the mental state examination. The assessments on these instruments were done by two separate assessors, i.e. PANSS was administered by a psychiatrist and evaluation on IDEAS was done by another psychiatrist or a vocational guidance instructor. The assessors were well versed with these instruments and were blind to the assessment findings of the other assessor. After completion of these evaluations, patients were invited to complete the Hindi version of WHOQOL-100, which is a validated instrument for assessment of QOL in north Indian population24. It generates scores on six domains of QOL, namely, physical, psychological, level of independence, social relationships, environment and spirituality.
The IDEAS, evaluates disability in four areas (termed items in the scale), namely, self care, interpersonal activities, communication and understanding, and work. Each item is scored on a 5 point scale with a range of 0-4, i.e. from no (0) to profound disability (4). To ease rating on each item, questions related to that area of functioning are given explicitly and a description for each score has been provided. The total disability score is obtained by summing up the ratings on each item. The global disability score is calculated by adding the ‘total disability score’ and Duration of Illness (DOI) score which has been operationalized for different duration of illness categories. Global disability score of 0 (i.e. 0%) corresponds to ‘no disability’, a score from 1 to 6 (i.e. <40%) corresponds to ‘mild disability’, a score of 7-13 (40 - 70%) corresponds to moderate disability, score of 14-19 (71-99%) to severe disability and a score of 20 (100%) corresponds to profound disability. In order to score this instrument, information from all possible sources is obtained including interview of patient, the caregiver and case notes wherever available. Further, it has provision and anchor point to rate the disability of all those on regular job and those involved in household work11. Two major modifications were done by the GOI in IDEAS. First, in contrast to the recommendation of IPS to use IDEAS only for patients with diagnoses of schizophrenia, OCD, bipolar disorder and dementia, the Committee recommended that the scale can be used for ‘mental illnesses’ as defined under the Persons with Disability Act; i.e. for any mental disorder other than mental retardation. Second, the IPS recommended the use of IDEAS for patients with total duration of illness of at least two years. Further, the recommendation for episodic illnesses was that the number of months the patient has been symptomatic in the last two years (MI 2Y-months of illness in the last two years) should be determined. On the other hand, the Committee recommended use of duration of illness without distinguishing between symptomatic and asymptomatic periods. In keeping with the decision of the Committee, in 2002, the Government of India issued a gazette notification for assessment and certification of disability associated with mental illnesses using the modified IDEAS13.
Statistical analysis: The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 14.0 Chicago, USA. Descriptive analysis (mean, standard deviation and frequency) was carried out for the socio-demographic, clinical variables, and PANSS scores. Mean scores of each item of IDEAS were computed. Student t-test was used to study differences in IDEAS item scores with regard to gender, marital status, education, occupation, religion, area of residence and family type. Pearson's Product Moment Correlation test was used to study the relationships between the items, total and global scores of the IDEAS and age, age at onset and duration of illness. Correlation matrix for the sub-scales of IDEAS and global score was generated to study inter-item relation and item-scale relation. In view of multiple correlations, P<0.01 was taken as significant. Internal consistency was calculated using Cronbach's alpha. Pearson's correlation matrix was computed to study correlations between IDEAS scores; and PANSS and WHO QOL scores.
Results
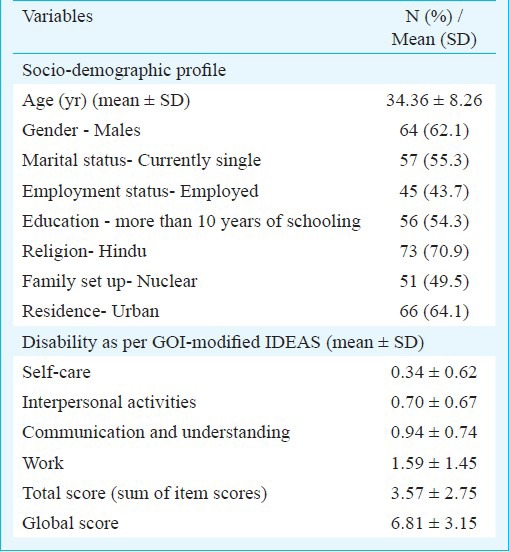
Socio-demographic and clinical characteristics: The mean age of the study sample (n=103) was 34.36 ± 8.26 yr; males (62.1%) outnumbered the females. More than half of the patients were currently single (N=57; 55.3%), unemployed/homemakers (58; 56.3%) and had received more than 10 years of education (N=56; 54.3%). There was nearly equal representation of patients from nuclear and non-nuclear families. About two-third of the patients were from urban background and more than two-third of the patients were following Hindu religion (Table I).
Table I.
Socio-demographic profile of the study sample (N=103)
The mean age at onset was 22.76 ± 5.64 yr and the mean total duration of illness was 138.96 ± 86.76 months. A majority of the patients were on atypical antipsychotics (78.6%) and were never hospitalized (74.3%). The mean PANSS positive subscale score was 9.19 ± 2.95, negative subscale score was 17.09 ± 5.37, general psychopathology subscale score was 23.16 ± 5.76 and total PANSS score was 49.45 ± 11.31.
Measures of disability and QOL: The mean scores on different items of GOI modified IDEAS are shown in Table I. Maximum disability was seen in the area of work, followed by the areas of communication and understanding, and interpersonal activities. The least disability was seen in the area of self care. The mean domain scores on WHOQOL-100 were: physical - 13.57 ± 2.92, psychological - 13.22 ± 2.40, level of independence- 13.47 ± 2.83, social relationships - 13.29 ± 2.66, environment - 13.53 ± 2.57 and spirituality- 3.23 ± 0.91.
Relationship of disability with socio-demographic and clinical variables: Males had significantly greater disability in the domains of self care P<0.001 and work P<0.001 as compared to females. Total duration of illness correlated with the IDEAS global score (r=0.406, P<0.001). None of the other socio-demographic and clinical variables had any association with disability.
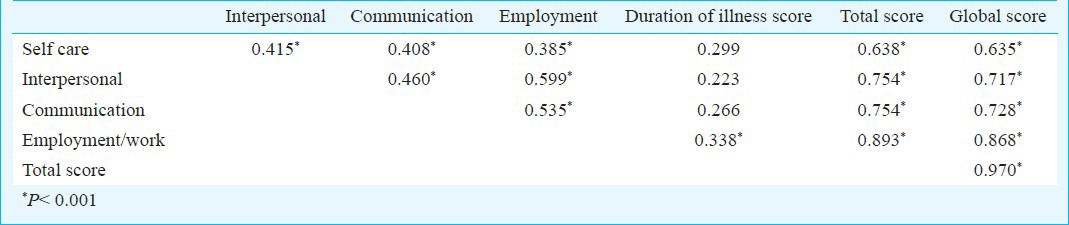
Internal consistency of GOI modified IDEAS: Scores on all the four items correlated significantly with each other and the total and global scores (Table II). The inter-item correlations varied from 0.385 to 0.599. The duration of illness had significant positive correlation with employment/work. The Cronbach's alpha which is a measure of internal consistency was 0.721 (4 items) and 0.708 (if DOI score was included for assessment of disability).
Table II.
Correlations between different items of GOI modified IDEAS
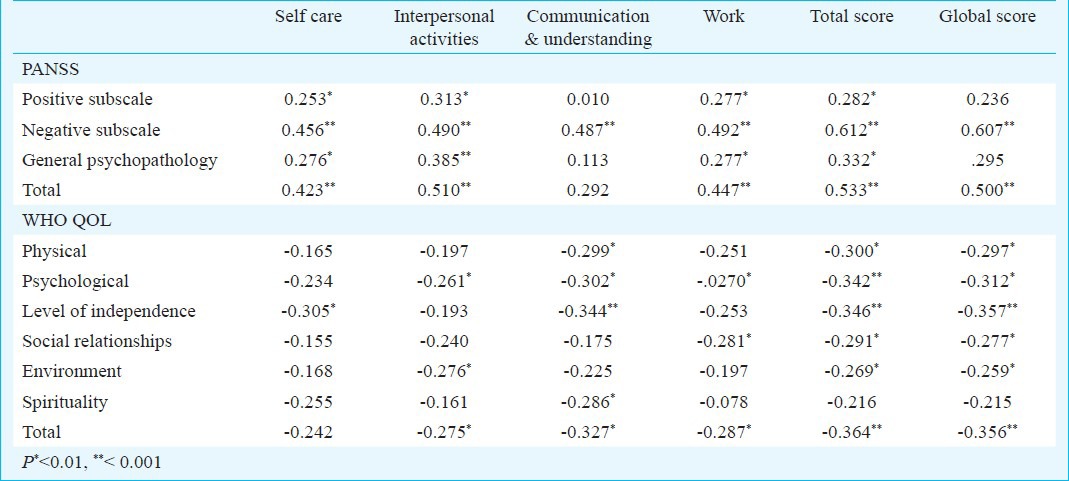
Construct validity: The results of the correlation matrix for studying convergent validity between IDEAS and PANSS scores; and divergent validity between IDEAS and WHOQOL-100 scores are shown in Table III. All item of IDEAS, total score and global IDEAS scores had significant positive correlation with all subscales of residual psychopathology as assessed on PANSS except communication item of IDEAS which correlated only with negative subscale of PANSS and global disability score which correlated only with negative subscale score and total PANSS scores. Significant negative correlations also emerged between various domains of QOL and various disability items. However, total disability and global disability correlated with all the domains of QOL.
Table III.
Relation between IDEAS scores and, PANSS and WHO QOL 100 scores for studying constructvalidity
Discussion
IDEAS is a scale approved by the GOI for assessment of disability in patients with psychiatric illnesses. We evaluated the construct validity of the scale by exploring its relationship with level of psychopathology and quality of life. Besides this, we also evaluated the internal consistency of the scale.
On IDEAS, maximum level of disability was seen in the domain of work, followed by communication and understanding, interpersonal activities and self-care. These findings were similar to other studies from India which had evaluated patients with schizophrenia using IDEAS13,19. The high level of disability in the domain of work possibly reflects the attitude of the society towards employability of people with mental illnesses. Studies from other parts of India suggest that people with schizophrenia face a lot of stigma and discrimination25 and have difficulty in getting jobs.
We also found that males had significantly higher disability in the domain of work as compared to females. This finding can be understood from the cultural aspect i.e. in Indian society as such males are expected to work and hence not being on a paid job is considered to be equal to non-productivity, whereas females are expected to do household work and even if they do not contribute to the desirable level, families accept them without much difficulties. In addition, patients of male gender also had higher disability in the area of self-care. These findings were similar to an earlier study which suggested that male gender predicted higher level of disability amongst those suffering from schizophrenia26.
Internal consistency is the extent to which all the items of a test measure the same latent variable, based on the degree of within-scale item correlations. The item inter-relations should ideally be greater than 0.3 and less than 0.7 to ensure item homogeneity but avoid significant item redundancy. In the present study, all the inter-item correlations of IDEAS fell within this range. The Cronbach's alpha, which is another measure of internal consistency, was found to be 0.721, which was also in the acceptable range (>0.7). These findings thus, show that IDEAS has good internal consistency.
Findings of the present study also showed that three out of the four items of the disability, the total and global disability score correlated with positive, negative and general psychopathology scores of PANSS, though the relation was strongest with negative symptom score. The item of communication correlated significantly only with negative subscale of PANSS. The present study was limited to patients with residual schizophrenia who had relatively higher scores in the negative domain of PANSS and it was assumed that whatever disability the patients had could be largely due to negative symptoms. Hence, strong correlation between negative symptoms and all the items of IDEAS indicated a good level of convergent validity of IDEAS. Other studies which have also looked at the relationship of disability and psychopathology have also reported similar findings27,28. In addition, studies done in naturalistic settings, which have evaluated the effect of treatment on disability, have also shown that with treatment, disability reduces29,30.
Previous studies have also evaluated the relation of disability as measured by different disability scales with QOL31. Findings of the present study also showed significant inverse correlations between the items of IDEAS and different domains of QOL as assessed by WHO QOL-100. It was observed that among the various domains of QOL, the psychological QOL and level of independence had higher number of correlations and stronger correlations with disability. However, total and global disability scores correlated with all the domains of QOL, and this suggests that disability as assessed on IDEAS has negative correlation with QOL and provides further evidence of construct validity of the scale.
The present study had few limitations. It was conducted in a small sample. Moreover, the study was conducted in a homogenous sample of patients suffering from schizophrenia, and any physical illness that can potentially contribute to disability was ruled out. Thus, the results cannot be generalized to other group of patients. Further the study involved cross-sectional evaluation of the relationship between disability, psychopathology and QOL. Future studies should attempt to overcome these limitations.
To conclude, the present study showed that GOI modified IDEAS had good internal consistency and construct validity. These psychometric properties enhance the credibility of the instrument for assessment of psychiatric disability.
References
- 1.World Health Organization. Geneva: World Health Organization; 2001. International classification of functioning, disability and health: ICF. [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization; 2008. The global burden of disease: 2004 update. [Google Scholar]
- 3.Seattle, WA, USA: IHME; 2013. Institute for Health Metrics and Evaluation (IHME). The global burden of disease: Generating evidence, guiding policy. [Google Scholar]
- 4.Kasthuri P, Chandrashekar H, Kumar CN, Prashanth NR. Disabilities research in India. Indian J Psychiatry. 2010;52:281–5. doi: 10.4103/0019-5545.69252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Census of India, 2001. New Delhi (India): Ministry of Home Affairs, Government of India; 2001. [accessed on June 16, 2012]. Registrar General of India. Available from: http://www.censusindia.net . [Google Scholar]
- 6.Murthy RS, Anuradha D, Pershad D, Wig NN. Psychiatric disability Scale. Preliminary report. Indian J Clin Psychol. 1975;2:183. [Google Scholar]
- 7.Wig NN, Murthy RS, Pershad D. Relationship of disability with psychiatric diagnosis and treatment acceptance patterns. Indian J Psychiatry. 1979;21:355–8. [Google Scholar]
- 8.Thara R, Rajkumar S, Valecha V. The schedule for assessment of psychiatric disability - A modification of the DAS-II. Indian J Psychiatry. 1988;30:47–55. [PMC free article] [PubMed] [Google Scholar]
- 9.Gurgaon: Indian Psychiatric Society; 2002. The Rehabilitation Committee of the Indian Psychiatric Society. IDEAS (Indian Disability Evaluation and Assessment Scale) - A scale for measuring and quantifying disability in mental disorders. [Google Scholar]
- 10.Thara R. Measurement of psychiatric disability. Indian J Med Res. 2005;121:723–4. [PubMed] [Google Scholar]
- 11.Ministry of Social Justice and Empowerment, Government of India. Guidelines for evaluation and assessment of mental illness and procedure for certification. (No. 16-18/97-NI) 2002. [accessed on June 16, 2012]. Available from: http://www.ccdisabilities.nic.in/page.php?s=reg'p=guide_mental't=pb#maincont .
- 12.Chaudhury PK, Deka K, Chetia D. Disability associated with mental disorders. Indian J Psychiatry. 2006;48:95–101. doi: 10.4103/0019-5545.31597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohan I, Tandon R, Kalra H, Trivedi JK. Disability assessment in mental illnesses using Indian Disability Evaluation Assessment Scale (IDEAS) Indian J Med Res. 2005;121:759–63. [PubMed] [Google Scholar]
- 14.Ganesh Kumar S, Das A, Bhandary PV, Soans SJ, Harsha Kumar HN, Kotian MS. Prevalence and pattern of mental disability using Indian Disability Evaluation Assessment Scale in a rural community of Karnataka. Indian J Psychiatry. 2008;50:21–3. doi: 10.4103/0019-5545.39754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solanki RK, Singh P, Midha A, Chugh K, Swami MK. Disability and quality of life in schizophrenia and obsessive compulsive disorder: a cross-sectional comparative study. East Asian Arch Psychiatry. 2010;20:7–13. [PubMed] [Google Scholar]
- 16.Thirthalli J, Venkatesh BK, Naveen MN, Venkatasubramanian G, Arunachala U, Kishore Kumar KV, et al. Do antipsychotics limit disability in schizophrenia? A naturalistic comparative study in the community. Indian J Psychiatry. 2010;52:37–41. doi: 10.4103/0019-5545.58893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thirthalli J, Venkatesh BK, Kishorekumar KV, Arunachala U, Venkatasubramanian G, Subbakrishna DK, et al. Prospective comparison of course of disability in antipsychotic-treated and untreated schizophrenia patients. Acta Psychiatr Scand. 2009;119:209–17. doi: 10.1111/j.1600-0447.2008.01299.x. [DOI] [PubMed] [Google Scholar]
- 18.Ganesh Kumar S, Avinash S, Unnikrishnan B, Kotian MS. Effect of psychosocial intervention on quality of life and disability grading of mentally disabled adolescents. Curr Pediatr Res. 2011;15:127–31. [Google Scholar]
- 19.Kumar S, Kulhara P, Grover S, Malhotra R. Preliminary experiences with use of disability assessment scales at mental disability clinic, PGIMER, Chandigarh. J Mental Health Hum Behav. 2006;11:39–43. [Google Scholar]
- 20.Balhara YPS, Gauba D, Deshpande SN. Profile difference between male and female psychiatric patients seeking certificate of disability. Oman Med J. 2011;26:410–5. doi: 10.5001/omj.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kashyap K, Thunga R, Rao AK, Balamurali NP. Trends of utilization of government disability benefits among chronic mentally ill. Indian J Psychiatry. 2012;54:54–8. doi: 10.4103/0019-5545.94648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M. Washington, DC: American Psychiatric Press; 1997. Structural clinical interview for axis-1 DSM-IV disorders - Clinical version (SCID-CV) [Google Scholar]
- 23.Kay SR, Opler A, Fisbein A. Positive and Negative syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;2:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 24.Saxena S, Chandiramani A, Bhargava R. WHOQOL-Hindi: a questionnaire for assessing quality of life in health care settings in India. Natl Med J India. 1998;11:160–6. [PubMed] [Google Scholar]
- 25.Loganathan S, Murthy SR. Experiences of stigma and discrimination endured by people suffering from schizophrenia. Indian J Psychiatry. 2008;50:39–46. doi: 10.4103/0019-5545.39758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpiniello B, Carta MG. Disability in schizophrenia. Intrinsic factors and prediction of psychosocial outcome. An analysis of literature. Epidemiol Psichiatr Soc. 2002;11:45–58. doi: 10.1017/s1121189x00010149. [DOI] [PubMed] [Google Scholar]
- 27.McKibbin C, Patterson TL, Jeste DV. Assessing disability in older patients with schizophrenia: Results from the WHODAS-II. J Nerv Ment Dis. 2004;192:405–13. doi: 10.1097/01.nmd.0000130133.32276.83. [DOI] [PubMed] [Google Scholar]
- 28.Villalta-Gil V, Vilaplana M, Ochoa S, Haro JM, Dolz M, Usall J, et al. NEDENA Group. Neurocognitive performance and negative symptoms: are they equal in explaining disability in schizophrenia outpatients? Schizophr Res. 2006;87:246–53. doi: 10.1016/j.schres.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 29.Krishnadas R, Moore BP, Nayak A, Patel RR. Relationship of cognitive function in patients with schizophrenia in remission to disability: A cross-sectional study in an Indian sample. Ann Gen Psychiatry. 2007;30:6–19. doi: 10.1186/1744-859X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fenton WS, McGlashan TH. Natural history of schizophrenia subtypes II. Positive and negative symptoms and long-term course. Arch Gen Psychiatry. 1991;48:978–86. doi: 10.1001/archpsyc.1991.01810350018003. [DOI] [PubMed] [Google Scholar]
- 31.Mubarak A. Social functioning and quality of life of people with schizophrenia in the northern region of Malaysia. Adv Mental Health. 2005;4:200–9. [Google Scholar]


