Abstract
Background & objectives:
In Odisha, several cases of dengue virus infection were detected for the first time in 2010, the importance of dengue as a serious mosquito-borne viral infection was felt only in 2011 with the reporting of many more positive cases. This retrospective three year study was done to find out the seroprevalence of dengue IgM antibody and to know the predominant serotype of dengue virus among the patients suspected to have dengue virus infection in a tertiary care hospital in southern Odisha, India.
Methods:
Blood samples from clinically suspected dengue cases admitted in the Medicine and Paediatrics departments of a tertiary care hospital were collected. These were processed for detection of dengue specific IgM antibody, carried out by the ELISA method. Dengue IgM antibody positive serum samples were tested for serotypic identification.
Results:
Of the 5102 samples tested, 1074 (21.05 %) were positive for dengue IgM. Maximum numbers of cases were found in 2012. Majority (47.86 %) of cases were detected in the month of September. The most common affected age group was 11 to 20 yr. DENV1 and DENV2 were the detected serotypes.
Interpretation & conclusions:
Rapid increase in the dengue cases in 2012 became a public health concern as majority of cases were affecting the young adolescents. Most of the cases were reported in post-monsoon period indicating a need for acceleration of vector control programmes prior to arrival of monsoon.
Keywords: Dengue virus, IgM antibody, seroprevalence, serotype, vector control
Dengue virus belonging to the family “Flaviviridae”, consists of ten proteins, three of which are structural and seven non-structural, and it has four serotypes, namely DENV1, DENV2, DENV3 and DENV4. These arboviruses are transmitted by the mosquitoes; Aedes aegypti and Ae. albopictus1,2. Ae. albopictus breeds in a wide variety of natural and artificial habitats, though their resting occurs in outdoors and biting occurs both in outdoor as well as indoor3.
Although dengue has a global distribution, South-East Asian regions together with Western Pacific region bear nearly 75 per cent of the current global disease burden4. In India, with the occurence of first epidemic from Kolkata (1963), the disease was later reported from Vishkapattanam (1964), Vellore (1968), Ajmer (1969), Kanpur (1969), Jalore of Rajasthan (1985), Chandigarh (2002), Mumbai (2004), Ludhiana (2007), New Delhi (1996, 2003, 2006, 2010), Chennai (2006-2008) and Kerala (2008)4,5,6. Odisha State in 2010, enrolled its name for the first time in the list of States showing mortality due to dengue virus infection, with the reporting of 25 cases and five deaths7.
Early diagnosis of dengue virus infection is important for treatment and aversion of complications like dengue shock syndrome (DSS) and dengue haemorrhagic fever (DHF). Dengue virus specific IgM antibodies appear as early as three days of dengue viral fever and can persist for 30-60 days, whereas IgG antibodies appear at about seventh day, peak at 2-3 wk and persist for life8.
This retrospective study was done to analyze the trend of the disease during 2010-2012 and identification of circulating dengue virus serotypes among the patients admitted to a tertiary care hospital in south Odisha.
Material & Methods
This retrospective study was carried out among clinically suspected dengue patients admitted in the departments of Medicine and Paediatrics of Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha. The clinical diagnosis of dengue virus infection was based on the WHO definitions9. Probable dengue fever (DF) is defined as acute febrile illness with two or more of the following manifestations: headache, retro-orbital pain, myalgia, arthralgia, rash, haemorrhagic manifestations, and leucopenia. Confirmed DF is a case confirmed by laboratory criterion10.
Laboratory criterion for confirmation of DF included any one of the following: isolation of dengue virus from serum or autopsy samples; demonstration of a four-fold or greater change in reciprocal IgG or IgM to one or more dengue viral antigens in paired serum samples or demonstration of dengue virus antigen in autopsy tissue, serum, or cerebrospinal fluid samples by immunohistochemistry, immunofluorescence or ELISA; or detection of dengue virus genomic sequences in autopsy tissue, serum or cerebrospinal fluid samples by polymerase chain reaction10.
Although NS1 antigen can be detected from as early as one day post onset syndrome, it is positive only upto 18 days11. As this study was conducted in a tertiary care hospital, most cases were referred from the peripheral health centers, among whom some with fever of more than 2-3 wks duration were also noticed. On the other hand, dengue IgM antibody is a marker of recent infection, detection of which is easy, simple and less time-consuming as compared with other serological methods8. Moreover, it can be detected from as early three days to 60 days of infection. Though dengue IgM detection is a commonly performed test for diagnosis of dengue, it has limitations due to cross-reactivity between other circulating flaviviruses.
Patients presenting as probable DF having fever for more than three days were included in the study group. A total of 5102 blood samples were reviewed over a period of three years from January 2010 to November 2012. Using strict aseptic precautions, about 3 ml blood was collected from each patient. This study was approved by the Institutional Ethical Committee. In the department of Microbiology, serum was separated using the standard methods and subjected to IgM antibody testing by dengue IgM antibody capture ELISA test kit supplied by the National Institute of Virology, Pune.
Due to lack of facility for genotypic study, serotypic characterization could not be done in 2010 and 2011. But in 2012, 35 of the randomly selected dengue IgM positive serum samples were sent to Regional Medical Research Centre (RMRC), Bhubaneswar, for serotypic identification.
Statistical analysis: Fisher's exact test and (GraphPad Software Inc.) was used for data analysis.
Results
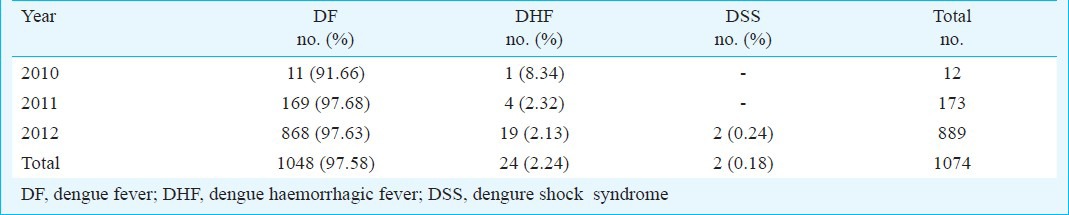
In this three year study, a total 5102 serum samples were analyzed, among which dengue IgM antibodies were detected in 1074 (21.05%) cases. Year-wise distribution of dengue IgM positive cases over the three year period is shown in Table I. Highest number of cases (889), were seen in 2012, whereas lowest number (12) was seen in 2010. Seasonal trend in each year showed that there were almost no positive cases from January to June; the infection started spreading in August, reaching its peak in September and October and slowly declined by December. Majority of the cases 514 (47.86%) were found in the month of September (Figure). In our study, 21.2 per cent of dengue IgM seropositivity was noticed among females while 20.9 per cent among males. Though majority of the patients belonged to 11-20 yr age group followed by 21-30 yr age group (Table II). Among the 1074 detected cases, 1048 (97.58%) presented with dengue fever (DF), 24 (2.24%) with dengue haemorrhagic fever (DHF) and two (0.18%) with dengue shock syndrome (DSS) (Table III).
Table I.
Year-wise distribution of dengue cases
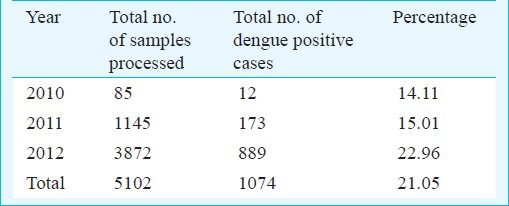
Fig.
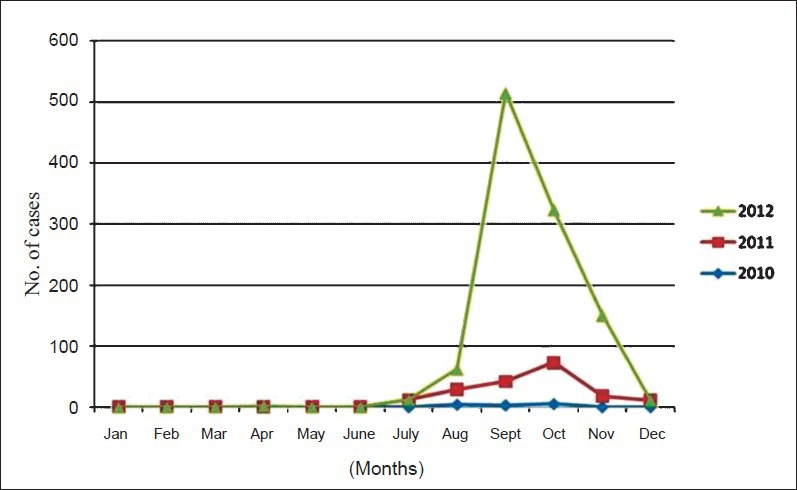
Seasonal variation of dengue cases during the study period.
Table II.
Age and sex wise distribution of cases
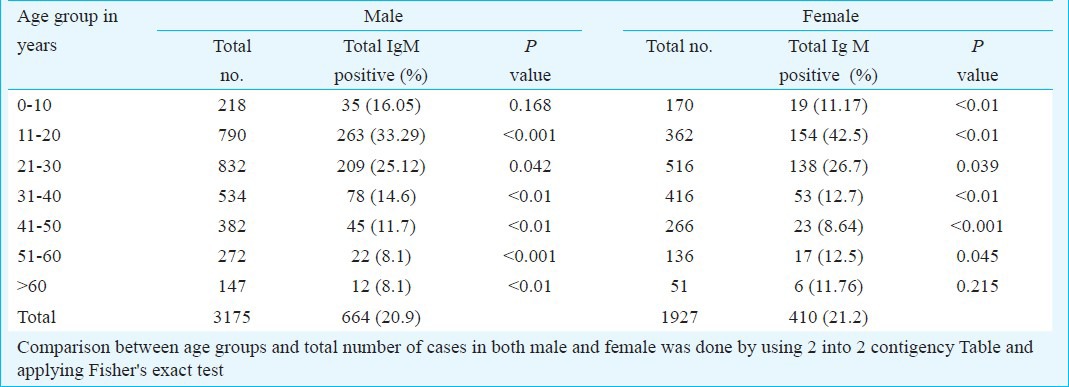
Table III.
Clinical presentation of cases
Thirty five serum samples were tested by reverse transcription polymerase chain reaction (RT-PCR) at RMRC, Bhubaneswar. Of these, two cases with co-infection with DENV1 and DENV2, and one case of DENV2 infection were noticed.
Discussion
In this three year study, a sudden and rapid increase in number of dengue cases was observed in 2012 compared to the previous two years. Increased travel among people to neighbouring States for the purpose of jobs and trades might be responsible for the spread of the disease. Also, rapid unplanned urbanization with heavy construction activities and poor sanitation facilities contribute to fertile breeding grounds for the mosquitoes.
The maximum number of dengue cases seen in the month of September indicated an active viral transmission during monsoon and post-monsoon period as reported earlier12,13. A higher occurrence of dengue infection was noted among females which is similar to a study conducted in Chennai5. However, this was discordant with other studies where a male predominance was noticed4,14. More number of patients belonged to the age group of 11 to 20 yr followed by 21 to 30 year which was consistent with studies conducted in different parts of India15,16. In a study conducted in Delhi 21 to 30 yr age group was most commonly affected and another study conducted in Kanpur, showed 0 to 15 yr age group to be commonly affected4,17. In this retrospective study, DF was found to be the most common presentation which was similar to a study conducted in Delhi10. It is an established fact that complications like DHF and DSS occur mainly in cases with secondary infections due to antibody mediated immune enhancement, cross reactive T – cell response with activation of TH-2 lineage cell and stimulation of soluble factors18.
Both the DENV1 and DENV2 serotypes were found to be circulating in this region. Though DENV1 was found in 1997 outbreak in New Delhi, all the four types were responsible for 2003 outbreak. DENV3 was the predominant one in 2005 outbreak19. DENV2 was associated with the outbreaks in Jammu, Haryana, Delhi, Luckhnow and epidemic in Gujarat20.
This study reported an increasing trend in seroprevalence of dengue virus infection affecting the young children and late adolescents. Both DENV1 and DENV2 serotypes were found. There is a need to develop vaccines that can protect against all the four serotypes. As most cases were reported during post monsoon period, continued and coordinated efforts should be made to control the transmitting vectors to prevent dengue outbreaks.
References
- 1.Lambrechts L, Scott TW, Gubler DJ. Consequences of expanding global distribution of Aedes albopictus for dengue virus transmission. PLoS Negl Trop Dis. 2010;4:e646. doi: 10.1371/journal.pntd.0000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiter P. Aedes albopictus and the world trade in used tires, 1988-1995: the shape of things to come? J Am Mosq Control Assoc. 1998;14:83–94. [PubMed] [Google Scholar]
- 3.Tewari SC, Thenmojhi V, Katholi CR, Manavalan R, Munirathinam A, Gajanana A. Dengue vector prevalence and virus infection in a rural area in South India. Trop Med Int Health. 2004;9:499–507. doi: 10.1111/j.1365-3156.2004.01103.x. [DOI] [PubMed] [Google Scholar]
- 4.Garg A, Garg J, Rao YK, Upadhyay GC, Sakhuja S. Prevalence of dengue among clinically suspected febrile episodes at a teaching hospital in North India. J Infect Dis Immun. 2011;3:85–9. [Google Scholar]
- 5.Gunasekaran P, Kaveri K, Mohana S, Arunagiri K, Babu BVS, Priya PP, et al. Dengue disease status in Chennai (2006-2008): A retrospective analysis. Indian J Med Res. 2011;133:322–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Anoop M, Issac A, Mathew T, Philip S, Kareem NA, Unnikrishnan R, et al. Genetic characterization of dengue virus serotypes causing concurrent infection in an outbreak in Ernakulum, Kerala, South India. Indian J Biol. 2010;48:849–57. [PubMed] [Google Scholar]
- 7.Government of India, Health and Family Welfare Department, National Vector Borne Disease Control Programme, (NVBDCP): Dengue cases and deaths in the country since 2007. e2012. [accessed on December 5, 2012]. Available from: http://www.nvbdcp.gov.in/dencd.html .
- 8.Vijayakumar TS, Chandy S, Sathis N, Abraham M, Abraham P, Sridharan G. Is dengue emerging as a major public health problem? Indian J Med Res. 2005;121:100–7. [PubMed] [Google Scholar]
- 9.World Health Organization. Dengue hemorrhagic fever: Diagnosis, treatment and control. World Health Organization. 2nd ed. 1997. [accessed on December 2, 2012]. Available from: http://www.who.int/csr/resources/publications/dengue/Denguepublication/en/
- 10.Sharma Y, Kaur M, Singh S, Pant L, Kudesia M, Jain S. Seroprevalence and trend of dengue cases admitted to a Government hospital, Delhi- 5year Study (2006-2010): A look into the age shift. Int J Prev Med. 2012;3:537–43. [PMC free article] [PubMed] [Google Scholar]
- 11.Laboratory Guidance and Diagnostic Testing. Centers for Disease Control and Prevention. [accessed on July 20, 2013]. Available from: http://www.cdc.gov/dengue/clinicallab/laboratory.html .
- 12.Gupta E, Dar L, Narang P, Srivastava VK, Broor S. Serodiagnosis of dengue during an outbreak at a tertiary care hospital in Delhi. Indian J Med Res. 2005;121:36–8. [PubMed] [Google Scholar]
- 13.Ukey PM, Bondade SA, Paunipagar PV, Powar RM, Akulwar SL. Study of seroprevalence of dengue fever in central India. Indian J Community Med. 2010;35:517–9. doi: 10.4103/0970-0218.74366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar A, Rao R, Pandit V, Shetty S, Bamigatti C, Samaraging CM. Clinical manifestation and trend of dengue cases admitted in tertiary care hospital, Udupi, Karnataka. Indian J Community Med. 2010;35:386–91. doi: 10.4103/0970-0218.69253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kavita R. Dengue fever: The rise and establishment of a new disease in Kerala, India with special references to the capital, Thiruvananthapuram. J Acad Clin Microbiol. 2007;9:65–70. [Google Scholar]
- 16.Sukri NC, Laras K, Wandra T, Didi S, Larasati RP, Rachdyatmaka JR. Transmission of epidemic dengue hemorrhagic fever in easternmost Indonesia. Am J Trop Med Hyg. 2003;68:529–35. doi: 10.4269/ajtmh.2003.68.529. [DOI] [PubMed] [Google Scholar]
- 17.Chakravarti A, Kumaria R. Eco-epidemiological analysis of dengue infection during an outbreak of dengue fever, India. Virol J. 2005;2:32. doi: 10.1186/1743-422X-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martina BE, Koraka P, Osterhaus A. Dengue virus pathogenesis, an integrated view. Clin Microbiol Rev. 2009;22:564–81. doi: 10.1128/CMR.00035-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta E, Dar L, Kapoor G, Broor S. The changing epidemiology of dengue in Delhi, India. Virol J. 2006;3:1–5. doi: 10.1186/1743-422X-3-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raheel U, Faheem M, Riaz MN, Kanwal N, Javed F, Zaidi NSS, et al. Dengue fever in the Indian subcontinent: an overview. J Infect Dev Ctries. 2011;5:239–47. doi: 10.3855/jidc.1017. [DOI] [PubMed] [Google Scholar]


